The known: Aged care services face specific challenges in providing accessible, culturally safe, high quality care for Aboriginal and Torres Strait Islander people.
The new: Of 6209 Aboriginal and Torres Strait Islander people assessed for eligibility during 2017–2019, aged care was approved for 6114 (98.5%), of whom 3218 (52%) used these services. At least seven health conditions were recorded for 42% of assessed people, and almost all required assistance with at least one functional daily activity.
The implications: Despite their high care needs, only half the eligible applicants accessed approved aged care services. It is likely that the care needs of older Aboriginal and Torres Strait Islander people are not being met.
All older Australians, regardless of their cultural identity, should have access to high quality, safe aged care services. Over the past 20 years, the proportion of Aboriginal and Torres Strait Islander people aged 50 years or more has almost doubled from 9.9% (53 355 people) in 2001 to 17.6% (173 578 people) in 2021.1,2 This growth is despite continued health and social inequities across the lifespan that contribute to the earlier onset of many health conditions than for non‐Indigenous Australians, and the consequently higher prevalence of chronic physical and mental conditions and lower life expectancy.3,4 The 2021 final report of the Royal Commission into Aged Care Quality and Safety described an aged care system that is characterised by barriers to access and inflexibility that impede its ability to respond in a culturally appropriate manner to the specific needs of Aboriginal and Torres Strait Islander people.5
In 2022, 30 000 Aboriginal and Torres Strait Islander people were receiving aged care services, including 22 100 who received home and community support from the Commonwealth Home Support Programme, which provides episodic support for people with low level care needs, such as basic personal care and support. A further 5800 people, who required a higher level of care and long term support, received home care packages, and 2100 received residential aged care, both of which require an aged care eligibility assessment.6 In addition, the National Aboriginal and Torres Strait Islander Flexible Aged Care Program, which recognises the geographic diversity of older people (20% live in remote areas),4 provides flexible, culturally appropriate aged care services (including home and residential care), predominantly in rural and remote areas; it provided 1310 places in 2022.7
Aboriginal and Torres Strait Islander people face special challenges in accessing aged care services, including lack of services outside metropolitan areas, culturally inappropriate needs assessments and services, and the lack of Aboriginal health care workers.5,8 Aboriginal and Torres Strait Islander people who are assessed are less likely to obtain specific services and more likely to be enrolled in entry and lower level programs.9 Exacerbating these challenges is that few care service providers specialise in providing culturally appropriate care and service delivery.10
The Australian government announced a number of reforms in response to the findings of the Royal Commission, including expanding the Aboriginal and Torres Strait Islander aged care workforce and culturally appropriate services.11 However, information about the aged care needs of Aboriginal and Torres Strait Islander people is needed to appropriately support these reforms. We have therefore characterised the socio‐demographic characteristics, aged and health care needs, and aged care services used by older Aboriginal and Torres Strait Islander people who have undergone aged care eligibility assessments.
Methods
The Registry of Senior Australians (ROSA) is a linked national aged care and health data platform established in 2017.12 The ROSA Aboriginal and Torres Strait Islander Advisory Committee was established in 2020 to govern research based on Aboriginal and Torres Strait Islander data in ROSA according to terms of reference that prescribe processes for embedding the principles of Indigenous data sovereignty. It comprises Aboriginal and Torres Strait Islander leaders in aged care from all states and territories, and is chaired by the first author of this article (Odette Pearson).12
The ROSA Aboriginal and Torres Strait Islander Advisory Committee informed and defined the research question for the study reported in this article, using the ROSA data platform to characterise the socio‐demographic and aged care assessment characteristics and aged and health care needs and services used by Aboriginal and Torres Strait Islander people who received aged care eligibility assessments during 2017–2019.
We undertook a population‐based, retrospective cohort study using the ROSA National Historical Cohort, which includes de‐identified linked aged and health care data.12 We analysed data from the Australian Institute of Health and Welfare National Aged Care Data Clearinghouse Aged Care Assessment Program (aged care eligibility assessment), Aged Care Services records (aged care services used), the National Death Index (NDI), and Pharmaceutical Benefits Scheme (PBS) datasets included in ROSA.12 We report our study in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE),13 and also with the Consolidated criteria for strengthening the reporting of health research involving Indigenous peoples (CONSIDER)14 guidelines (Supporting Information, table 1).
Study cohort
We analysed data for Aboriginal and Torres Strait Islander people aged 50 years or older at the time of their first aged care eligibility assessment (study entry) by an aged care assessment team during 1 January 2017 – 31 December 2019. People assessed by regional assessment services were not included. Aboriginal and Torres Strait Islander status was determined from aged care assessment or service data.
Study variables
Socio‐demographic characteristics were identified in aged care assessments: sex, age, remoteness (Australian Statistical Geography Standard15) and socio‐economic status (Index of Relative Socio‐economic Disadvantage, IRSD16) by residential postcode, and accommodation and living arrangements. The professions of aged care assessors and reasons for assessment were also derived from aged care assessment records. Approvals for and use of aged care services (permanent residential aged care, home care packages, respite care, transition care) were respectively identified in aged care assessment and service records. Information on length of follow‐up and death were obtained from aged care service and NDI records.
The number and types of health conditions in the six months prior to study entry were ascertained in the PBS database using the Rx‐Risk‐V pharmaceutical‐based comorbidity index and health conditions at the time of the aged care assessment (Supporting Information, table 2).12 For people with the ten most frequent health conditions, the number of other medical conditions was also assessed. Geriatric syndromes and functional limitations were identified in aged care assessments, except dementia and incontinence, which were ascertained from Rx‐Risk‐V and aged care assessment data.12
Statistical analysis
We summarise socio‐demographic and aged care assessment characteristics by service type or whether any aged care was received after assessment as frequencies and proportions (categorical variables) or medians with interquartile ranges (IQRs; continuous variables). Median survival time and median follow‐up time were estimated in Kaplan–Meier survival analyses. Statistical analyses were undertaken in Stata 16.
Positionality
The study, together with the ROSA Aboriginal and Torres Strait Advisory Committee, was led by Odette Pearson, an Eastern Kuku‐Yalanji and Torres Strait Islander woman and co‐leader of the Wardliparingga Aboriginal health equity theme. Alex Brown, from the Yuin Nation and inaugural theme leader, is an established researcher, medical doctor, and mentor for Odette Pearson over the past decade. The partnership with the ROSA (authors Gillian Caughey, Maria Inacio, Steve Wesselingh) ensures that ROSA data on Aboriginal and Torres Strait Islander people are used to improve the aged care system so that Aboriginal and Torres Strait Islander people receive high quality, safe aged care. The non‐Indigenous authors of this article are experts in establishing and maintaining this unique national registry, epidemiology, pharmacoepidemiology, and statistics.
Ethics approval
The study was approved by the University of South Australia (200489) and Australian Institute of Health and Welfare (EO2018/1/418) human research ethics committees, and by the Aboriginal Health Research Ethics Committee (04‐20‐895).
Results
Median follow‐up time for the 6209 people included in our analysis (Supporting Information, figure 1) was 462 days (IQR, 190–777 days); 1129 people (18.2%) died during follow‐up (median time to death, 198 days; IQR, 66–470 days). Median age at eligibility assessment was 67 years (IQR, 60–75 years), 3626 people (58.4%) were women, 4043 (65.7%) lived in regional to very remote areas of Australia, and 2696 (43.8%) lived in areas in the lowest socio‐economic status quintile. Most people lived in public housing (2358, 38.7%) or their own residence (1439, 23.5%); 2249 (37%) lived alone, and 2112 (34.8%) lived with family other than partners (Box 1).
The median time from referral to aged care assessment was 12 days (IQR, 3–25 days); a median of three health professionals (IQR, 1–4) contributed to assessments. Health professionals most frequently involved in assessments were registered nurses (4301, 69.3%) and general practitioners (2385, 38.4%); Aboriginal health workers were involved in 655 aged care assessments (10.5%). Medical conditions (4691, 75.6%), changes in care needs (3477, 56%), and frailty (2873, 46.3%) were the most frequently recorded reasons for assessments. Hospital discharge was a reason for larger proportions of assessments leading to residential aged care (428, 42.6%) or respite care (319, 38.0%) than for assessments leading to home care packages (374, 20.7%) or no service (655, 21.9%). Change in cognitive status was a reason for larger proportions of assessments leading to residential aged care (391, 38.9%) or respite care (285, 34%) than for assessments leading to home care packages (272, 15%) (Box 1).
Aged care and health care needs: health conditions and functional limitations
The median number of health conditions recorded for 6208 people (data missing for one person) was six (IQR, 4–8), both overall and regardless of whether they received aged care services after assessment. Almost all people (6013, 96.9%) had two or more recorded health conditions, 4505 (72.6%) had five or more conditions, and 2592 (41.8%) had seven or more; the distributions by number of conditions were similar for people who did or did not access care (Box 2).
Among the most frequently recorded medical conditions were cardiovascular disease (5076 people, 82%), arthritis or pain (4257, 68.6%), diabetes (2939, 47.3%), and chronic respiratory disease (2933, 47.3%) (Box 3). Comorbidity was frequent among people with each of the ten most frequent medical conditions; 3332 of 5076 people with cardiovascular disease (65.6%) and 956 of 1136 of people with anxiety (84.2%) had five or more other recorded medical conditions. Comorbidity was most frequent among people with mental health conditions: 597 of 1136 people with anxiety (52.5%) and 1170 of 2416 people with depression (48.5%) had seven or more other medical conditions (Box 4).
Geriatric syndromes were recorded for 2265 people (36.5%); 747 had gait or mobility problems (12.0%), 630 had dementia (10.2%), 620 had histories of falls (10.0%), and 603 histories of incontinence (9.7%). The proportion of people with dementia was larger for those who accessed services (402, 12.5%) than for those who did not (228, 7.6%) (Box 2).
Assistance with at least one functional activity was required by 6190 of 6207 people (99.7%); more than 50% required at least some assistance with eight of ten activities assessed. The proportions of people completely unable to cope without assistance were largest for housework (2600 people, 41.9%), preparing meals (1735, 28.0%), and shopping (1704, 27.4%) (Box 5).
Aged care services used
A total of 6114 people (98.5%) were approved for at least one aged care service (permanent residential aged care, home care package, respite care, or transition care); 3218 (52.6% of approvals) received aged care services, including 891 (27.7%) who used more than one service (Box 1). The most frequently used services were home care packages (1806, 29.1%), permanent residential aged care (1005, 16.2%), and respite care (839, 13.5%). Home care packages were the first services used by 1660 people (51.6%), respite care by 686 (21.3%), transition care by 443 (13.7%), and permanent residential aged care by 429 (13.3%). The median time from assessment to service access ranged from six days (IQR, 3–14 days) for transition care to 286 days (IQR, 153–476 days) for home care packages. Of the 1005 people who entered residential aged care, 488 (48.6%) had previously used respite care (Box 1).
A total of 2896 people for whom services had been approved (47.4%) did not use an aged care service during the study period. Of all people who did not use aged care services (2991 people, including 95 people for whom they were not approved), 2486 (83.1%) had been approved for home care packages, 2282 (76.3%) for Commonwealth Home Support, 102 (3.4%) for National Aboriginal and Torres Strait Islander Flexible Aged Care, and eleven (0.4%) for multi‐purpose services (Supporting Information, table 3).
Discussion
Our large population‐based study provides a comprehensive assessment of the socio‐demographic characteristics, care needs, and aged care services used by older Aboriginal and Torres Strait Islander people following aged care eligibility assessments. We provide evidence that, despite the high prevalence of multimorbidity, geriatric syndromes, functional limitations, and social care needs identified during assessments, only half the people for whom services were approved (52%) subsequently used aged care services. Our findings indicate that access to and use of aged care services by Aboriginal and Torres Strait Islander people are not concordant with their assessed health and aged care needs.
It is likely that the 48% of people who did not access aged care services for which they were eligible instead used lower level, community‐based services, but we could not examine this possibility. However, as they had been assessed and recommended for more substantial care, these people did not receive the best support to meet their needs. Most people in our study lived in regional to very remote areas, and geographic distance and limited access may have contributed to not using aged care services. In a similar ROSA data‐based study of non‐Indigenous people, 72% had used aged care services within a year of being approved, most often transition care and permanent residential aged care.17 Home care packages were the most frequently used service type in our study, suggesting a preference for care that facilitates people staying on Country and closer to family, Elders, and community support for as long as possible.18,19 Family support and community are key components of healthy ageing for Aboriginal and Torres Strait Islander people.20 Two‐thirds of people in our study lived with family or in the community, and maintaining these living arrangements may have been preferred to formal aged care services that are not culturally appropriate.
Older Aboriginal and Torres Strait Islander people are knowledge keepers and protectors of cultural heritage. Their important roles, including mentoring through shared life experiences, are integral to raising healthy communities.21,22 Cultural factors, such as connection to Country, knowledge and beliefs, cultural expression and language, kinship and family, are important for the physical health, social, and emotional wellbeing of Aboriginal and Torres Strait Islander people.23 Providing all aged care services in a culturally respectful and safe manner, regardless of residential location was a key recommendation of the Royal Commission,5 and is essential for equitable access. Culturally safe aged care services for older Aboriginal and Torres Strait Islander people include maintaining cultural identity, culturally informed service delivery, a culturally competent workforce, culturally supportive environments, and partnerships within the aged care system.24 Most older Aboriginal and Torres Strait Islander people prefer health and aged care provided by Aboriginal‐controlled (ie, Aboriginal Community Controlled Health Services, ACCHS) or Aboriginal‐specific services.25 ACCHS aged care is associated with greater access to affordable, culturally safe and quality aged care, and stronger cultural identity and connection.26 Establishing relationships with ACCHS and employing Aboriginal staff may facilitate culturally safe aged care by mainstream aged care services.
The aged care workforce is also a key component of culturally appropriate services, and only 2% of the current workforce are of Aboriginal or Torres Strait Islander descent.27 There is a clear need to build an Aboriginal aged care workforce, and recognition that more training and employment of Aboriginal and Torres Strait Islander people across aged care services is required.5 Aboriginal health workers had been involved in the aged care assessments of only 10% of people in our study, and this proportion must be increased. Data collection must be informed by the holistic wellbeing needs of Aboriginal and Torres Strait Islander people if the effectiveness of aged care services is to be monitored and improved in an evidence‐based manner. The paucity of Aboriginal health worker aged care assessors and the absence of holistic Aboriginal wellbeing in aged care assessments has been recognised by the Australian Department of Health and Aged Care, which in May 2023 provided $8.2 million to increase the capacity of Aboriginal Community Controlled Organisations and of $4.2 million to establish a First Nations assessment workforce.28
Finally, a recent study identified problems in access to aged care services; more than half the Aboriginal and Torres Strait Islander people interviewed were unaware of government‐funded home care support and home care packages; identified barriers included inadequate availability of information and public awareness.8
Chronic diseases are major contributors to the disease burden for Aboriginal and Torres Strait Islander people.29 Comorbidity and multimorbidity are more evident at a younger age in Aboriginal and Torres Strait Islander people than in other Australians.3 The prevalence of physical and mental health conditions, comorbidity, and multimorbidity were higher in our study than previously reported.3,30 For example, the National Aboriginal Health Survey found that 36% of people over 55 years of age living in the community had diabetes and 56% cardiovascular disease;30 in our study, the figures were respectively 47% and 82%. The challenges for people with multiple medical conditions31 are exacerbated for older Aboriginal and Torres Strait Islander people by systematic barriers in access to care. A holistic tailored, integrated and collaborative approach to care is required for helping people with multiple medical conditions,31 but models of care for Aboriginal and Torres Strait Islander people also need to include family and community, and consideration of cultural needs, to achieve optimal health and wellbeing.
Limitations
Our data source did not include information on the 1310 National Aboriginal and Torres Strait Islander Flexible Aged Care Program places provided in remote and very remote areas during 2021–22,7 resulting in incomplete reporting of aged care service use in such areas. We examined only aged care service use following aged care assessments for permanent residential aged care, home care packages, or respite or transition care, not episodic community home support or informal care. The “Good Spirit, Good Life” quality of life framework identified twelve factors important to the quality of life and wellbeing of older Aboriginal Australians,32 but ROSA does not include data for such factors. Despite improvements in recent years, incomplete identification of Aboriginal and Torres Strait Islander people in aged and health care datasets is possible. It is likely that linkage of other aged care datasets within ROSA, including aged care assessments and service use, improves identification.
Conclusion
A key strength of our study was the population‐based cohort of older Aboriginal and Torres Strait Islander people assessed for aged care services, providing a comprehensive national overview, based on data from multiple aged and health care data sources. Our findings provide an important baseline for monitoring and evaluating service use, variation in access, and health outcomes. Our study provides greater understanding of the health care needs of older Aboriginal and Torres Strait Islander people as they enter the aged care system. This should be placed in the context of social, cultural, and spiritual wellbeing, to reduce disparities, improve access to care, and to develop community‐informed, culturally appropriate aged care and health care services. Further information about equity in access and the use of aged care service specific to geographic location is needed. Our findings can inform aged care policies regarding the ageing, care, and wellbeing needs of older Aboriginal and Torres Strait Islander people.
Box 1 – Socio‐demographic and aged care eligibility assessment characteristics of 6209 Aboriginal and Torres Strait Islander people assessed during 2017–2019, by subsequent aged care service type use
|
|
Services received |
||||||||||||||
|
Characteristic |
All assessed people |
Permanent residential aged care |
Home care package |
Respite care |
Transition care |
None* |
|||||||||
|
|
|||||||||||||||
|
Number of people |
6209 |
1005 |
1806 |
839 |
459 |
2991 |
|||||||||
|
Received as first service (of the 3218 people [52.6%] who used services) |
— |
429 [13.3%] |
1660 [51.6%] |
686 [21.3%] |
443 [13.7%] |
— |
|||||||||
|
Time to first service (days), median (IQR) |
160 (26–358) |
36 (11–124) |
286 (153–476) |
60 (14–196) |
6 (3–14) |
— |
|||||||||
|
Other aged care services accessed† |
|
|
|
|
|
|
|||||||||
|
Permanent residential aged care |
— |
— |
10 (0.6%) |
6 (0.7%) |
1 (0.2%) |
— |
|||||||||
|
Home care package |
— |
124 (12.3%) |
— |
114 (13.6%) |
10 (2.2%) |
— |
|||||||||
|
Respite |
— |
488 (48.6%) |
67 (3.7%) |
— |
6 (1.3%) |
— |
|||||||||
|
Transition |
— |
81 (8.1%) |
75 (4.2%) |
43 (5.1%) |
— |
— |
|||||||||
|
Age at first service (years), median (IQR)‡ |
67 (60–75) |
72 (63–80) |
68 (62–76) |
72 (63–79) |
68 (61–75) |
65 (59–74) |
|||||||||
|
Sex (women) |
3626 (58.4%) |
513 (51.0%) |
1123 (62.2%) |
444 (52.9%) |
259 (56.4%) |
1784 (59.7%) |
|||||||||
|
Remoteness§ |
|
|
|
|
|
|
|||||||||
|
Major city |
2115 (34.3%) |
395 (39.3%) |
658 (36.3%) |
270 (32.2%) |
190 (41.4%) |
934 (31.2%) |
|||||||||
|
Inner regional |
1732 (27.9%) |
240 (23.9%) |
606 (33.6%) |
202 (32.2%) |
149 (32.5%) |
777 (26.0%) |
|||||||||
|
Outer regional |
1347 (21.7%) |
234 (23.3%) |
342 (18.9%) |
208 (24.8%) |
85 (18.5%) |
678 (22.7%) |
|||||||||
|
Remote |
420 (6.8%) |
61 (6.1%) |
70 (3.9%) |
73 (8.7%) |
21 (4.6%) |
252 (8.4%) |
|||||||||
|
Very remote |
544 (8.8%) |
61 (6.1%) |
120 (6.6%) |
76 (9.1%) |
12 (2.6%) |
331 (11.1%) |
|||||||||
|
Socio‐economic status (IRSD)¶ |
|
|
|
|
|
|
|||||||||
|
1 (most disadvantage) |
2696 (43.8%) |
390 (39.4%) |
793 (44.2%) |
342 (41.2%) |
171 (37.7%) |
1353 (45.6%) |
|||||||||
|
2 |
1719(27.9%) |
261 (26.4%) |
514 (28.7%) |
210 (25.3%) |
142 (31.3%) |
835 (28.1%) |
|||||||||
|
3 |
1044 (17.0%) |
185 (18.7%) |
303 (16.9%) |
162 (19.5%) |
74 (16.3%) |
480 (16.2%) |
|||||||||
|
4 |
481 (7.8%) |
109 (11.0%) |
131 (7.3%) |
81 (9.8%) |
46 (10.1%) |
207 (7.0%) |
|||||||||
|
5 (least disadvantage) |
212 (3.5%) |
45 (4.6%) |
53 (3.0%) |
35 (4.2%) |
21 (4.6%) |
92 (3.1%) |
|||||||||
|
Usual accommodation** |
|
|
|
|
|
|
|||||||||
|
Public housing |
2358 (38.7%) |
315 (31.3%) |
732 (40.5%) |
290 (34.6%) |
158 (34.4%) |
1164 (38.9%) |
|||||||||
|
Own residence |
1439 (23.5%) |
233 (23.2%) |
414 (22.9%) |
230 (27.4%) |
133 (29.0%) |
680 (22.7%) |
|||||||||
|
Private rental |
1224 (20.1%) |
185 (18.4%) |
366 (20.3%) |
126 (15.0%) |
86 (18.7%) |
605 (20.2%) |
|||||||||
|
Family members residence |
380 (6.2%) |
89 (8.9%) |
105 (5.8%) |
55 (6.6%) |
39 (8.5%) |
164 (5.5%) |
|||||||||
|
Indigenous community |
324 (5.3%) |
24 (2.4%) |
101 (5.6%) |
39 (4.7%) |
12 (2.6%) |
175 (5.9%) |
|||||||||
|
Retirement village |
121 (2.0%) |
25 (2.5%) |
38 (2.1%) |
21 (2.5%) |
6 (1.3%) |
49 (1.6%) |
|||||||||
|
Other |
253 (4.2%) |
88 (8.8%) |
36 (2.0%) |
51 (6.1%) |
15 (3.3%) |
113 (3.8%) |
|||||||||
|
Living arrangements†† |
|
|
|
|
|
|
|||||||||
|
Alone |
2249 (37.0%) |
385 (38.3%) |
725 (40.1%) |
281 (33.5%) |
171 (37.3%) |
1012 (33.8%) |
|||||||||
|
With family (other than partner) |
2112 (34.8%) |
331 (32.9%) |
541 (30.0%) |
319 (38.0%) |
150 (32.7%) |
1082 (36.2%) |
|||||||||
|
With partner |
1429 (23.5%) |
176 (17.5%) |
454 (25.2%) |
174 (20.7%) |
114 (24.8%) |
696 (23.3%) |
|||||||||
|
With others/friends |
282 (4.6%) |
59 (5.9%) |
72 (4.0%) |
42 (5.0%) |
15 (3.3%) |
137 (4.6%) |
|||||||||
|
Aged care assessor†,‡‡ |
|
|
|
|
|
|
|||||||||
|
Registered nurse |
4301 (69.3%) |
772 (76.8%) |
1223 (67.7%) |
597 (71.2%) |
384 (83.7%) |
1981 (66.2%) |
|||||||||
|
General practitioner |
2385 (38.4%) |
330 (47.3%) |
866 (48.0%) |
302 (36.0%) |
95 (20.7%) |
1125 (37.6%) |
|||||||||
|
Occupational therapist |
1970 (31.7%) |
454 (45.2%) |
472 (26.1%) |
338 (40.3%) |
294 (64.1%) |
795 (26.6%) |
|||||||||
|
Social worker |
1889 (30.4%) |
471 (46.9%) |
451 (25.0%) |
311 (52.1%) |
230 (50.1%) |
783 (26.2%) |
|||||||||
|
Aboriginal health worker |
655 (10.5%) |
143 (14.2%) |
196 (10.9%) |
115 (13.7%) |
49 (10.7%) |
266 (8.9%) |
|||||||||
|
Other medical practitioner |
1417 (22.8%) |
342 (34.0%) |
411 (22.8%) |
228 (27.2%) |
184 (40.1%) |
519 (17.4%) |
|||||||||
|
Reasons for assessment† |
|
|
|
|
|
|
|||||||||
|
Medical conditions |
4691 (75.6%) |
732 (72.8%) |
1410 (78.1%) |
588 (70.1%) |
355 (77.3%) |
2259 (75.5%) |
|||||||||
|
Change in care needs |
3477 (56.0%) |
640 (63.7%) |
986 (54.6%) |
515 (61.4%) |
286 (62.3%) |
1600 (53.5%) |
|||||||||
|
Frailty |
2873 (46.3%) |
495 (49.3%) |
909 (50.3%) |
415 (49.5%) |
128 (27.9%) |
1362 (45.5%) |
|||||||||
|
Hospital discharge |
1723 (27.8%) |
428 (42.6%) |
374 (20.7%) |
319 (38.0%) |
328 (71.5%) |
655 (21.9%) |
|||||||||
|
Fall |
1278 (20.6%) |
256 (25.5%) |
371 (20.5%) |
200 (23.8%) |
122 (26.6%) |
566 (18.9%) |
|||||||||
|
Change in cognitive status |
1181 (19.0%) |
391 (38.9%) |
272 (15.1%) |
285 (34.0%) |
66 (14.4%) |
473 (15.8%) |
|||||||||
|
Change in caring arrangements |
579 (9.3%) |
131 (13.0%) |
154 (8.5%) |
110 (13.1%) |
36 (7.8%) |
247 (8.3%) |
|||||||||
|
Change in living arrangements |
534 (8.6%) |
158 (15.7%) |
95 (5.3%) |
107 (12.8%) |
31 (6.8%) |
237 (7.9%) |
|||||||||
|
Other |
996 (15.6%) |
198 (19.7%) |
241 (13.3%) |
162 (19.3%) |
45 (9.8%) |
501 (8.1%) |
|||||||||
|
|
|||||||||||||||
|
IQR = interquartile range; IRSD = Index of Relative Socioeconomic Disadvantage. * People in this category (which includes 95 people not approved for aged care services) may have received community home support packages. † More than one category may apply to an individual. ‡ Age at study entry if no aged care services received during study period. § Missing data: 51 (0.8%). ¶ Missing data: 57 (0.9%). ** Missing data: 110 (1.8%). †† Missing data: 137 (2.2%). ‡‡ Missing data: 74 (1.2%). |
|||||||||||||||
Box 2 – Health conditions recorded for 6208 Aboriginal and Torres Strait Islander people assessed for aged care service eligibility during 2017–2019, by subsequent aged care service use
|
Characteristic |
All people |
Any service after assessment |
No service after assessment* |
||||||||||||
|
|
|||||||||||||||
|
Number of people |
6208 |
3218 (51.8%) |
2990 (48.2%) |
||||||||||||
|
Number of health conditions, median (IQR) |
6 (4–8) |
6 (4–8) |
(4–8) |
||||||||||||
|
Number of health conditions (categories) |
|
|
|
||||||||||||
|
0 or 1 |
195 (3.1%) |
118 (3.7%) |
77 (2.6%) |
||||||||||||
|
2–4 |
1508 (24.3%) |
786 (24.4%) |
722 (24.2%) |
||||||||||||
|
5 or 6 |
1913 (30.9%) |
1003 (31.2%) |
910 (30.4%) |
||||||||||||
|
7 or 8 |
1655 (26.7%) |
824 (25.6%) |
831 (27.8%) |
||||||||||||
|
9 or more |
937 (15.1%) |
487 (15.1%) |
450 (15.1%) |
||||||||||||
|
Geriatric syndromes |
2265 (36.5%) |
1159 (36.0%) |
1106 (36.9%) |
||||||||||||
|
Dementia† |
630 (10.2%) |
402 (12.5%) |
228 (7.6%) |
||||||||||||
|
Gait/mobility problems‡ |
747 (12.0%) |
416 (12.9%) |
331 (11.1%) |
||||||||||||
|
History of falls‡ |
620 (10.0%) |
339 (10.5%) |
281 (9.4%) |
||||||||||||
|
Incontinence† |
603 (9.7%) |
326 (10.1%) |
277 (9.3%) |
||||||||||||
|
Pressure injuries‡ |
314 (5.1%) |
180 (5.6%) |
134 (4.5%) |
||||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range. * Includes 95 people not approved for aged care services. † Ascertained from aged care eligibility assessment data and Rx‐Risk pharmaceutical‐based comorbidity index. ‡ Ascertained from aged care eligibility assessment data only. |
|||||||||||||||
Box 3 – Ten most frequent health conditions recorded for 6208 Aboriginal and Torres Strait Islander people assessed for aged care service eligibility during 2017–2019*
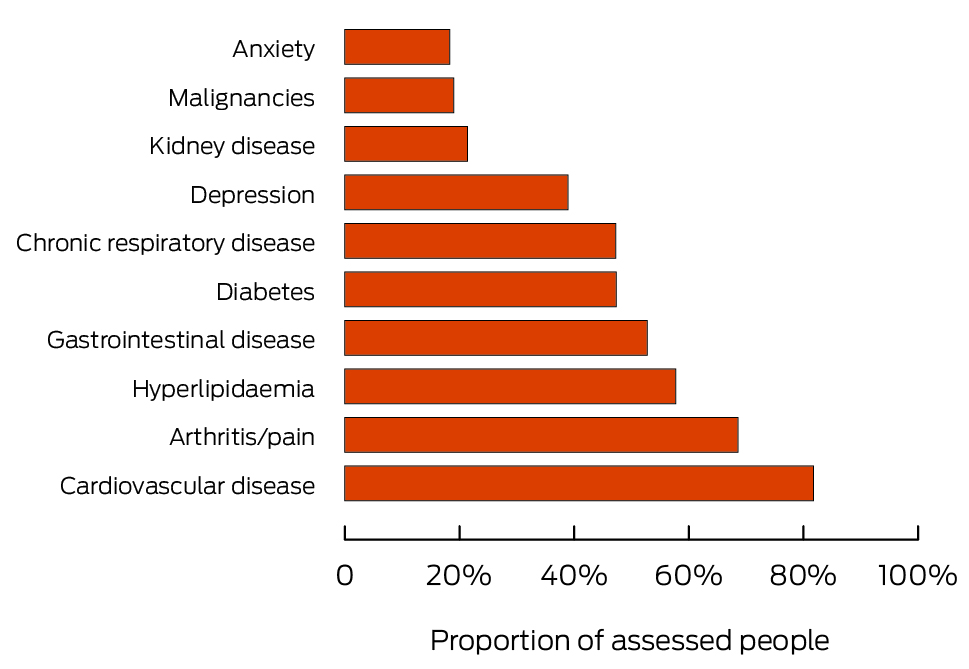
* The data underlying in this graph are included in the Supporting Information, table 4.
Box 4 – Number of other medical conditions recorded for 6208 Aboriginal and Torres Strait Islander people for whom one of the ten most frequent health conditions (index diseases) were recorded during assessment for aged care service eligibility during 2017–2019*
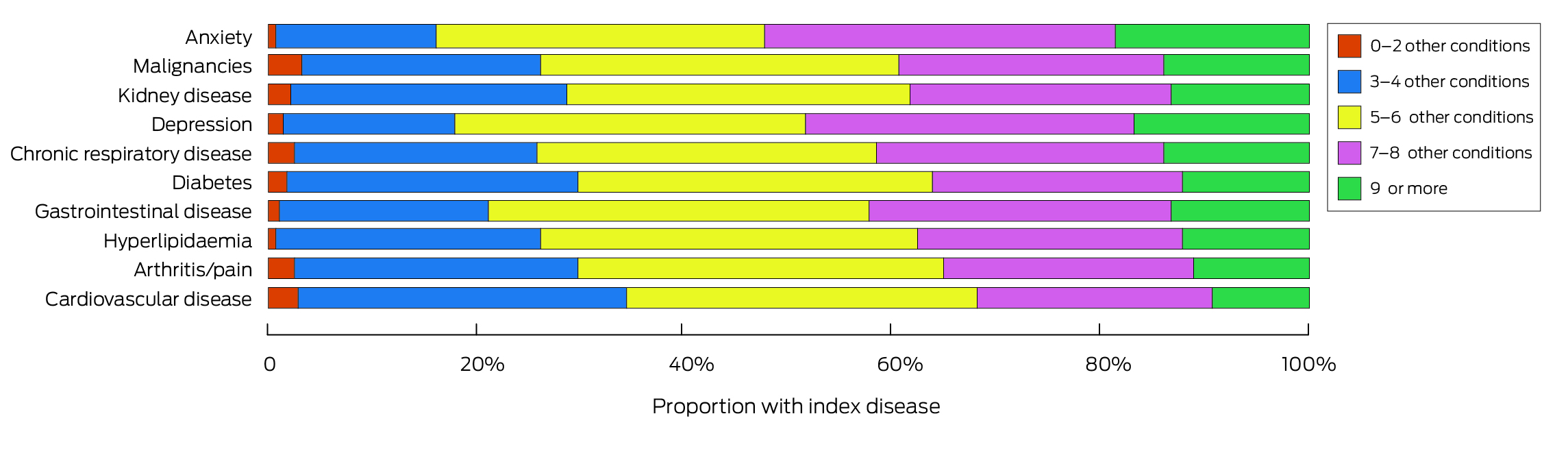
* The data underlying in this graph are included in the Supporting Information, table 5.
Box 5 – Ten most frequent activity limitations recorded for 6207 Aboriginal and Torres Strait Islander people assessed for aged care service eligibility during 2017–2019*
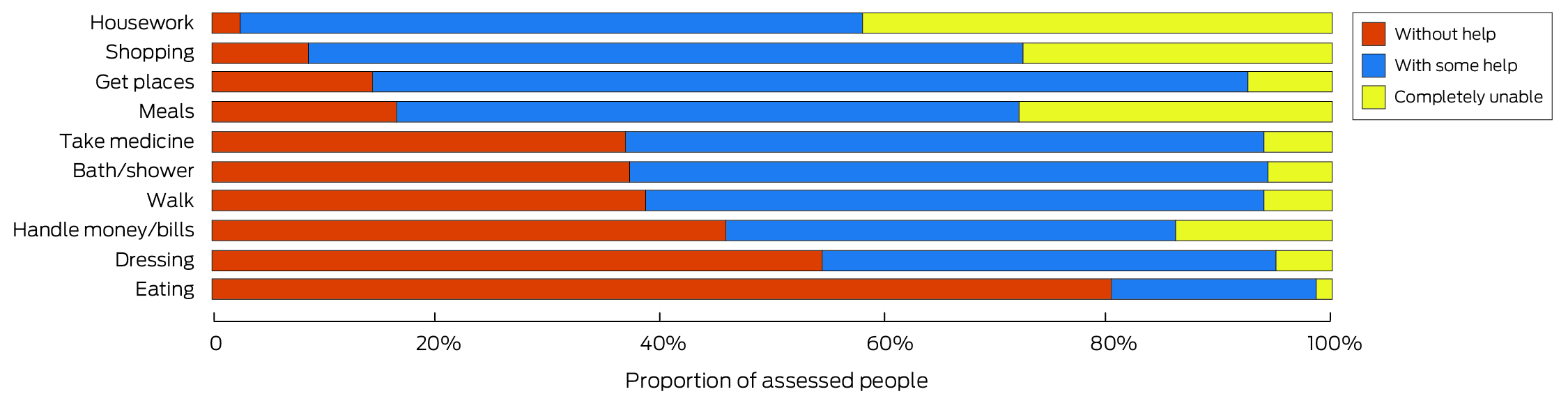
* The data underlying in this graph are included in the Supporting Information, table 6.
Received 13 September 2023, accepted 1 May 2024
- Odette Pearson (Eastern Kuku‐Yalanji and Torres Strait Islander)1,2
- Tracy Air3
- Greer Humphrey1
- Clare Bradley4
- Noeleen Tunny5
- Alex Brown (Yuin Nation)6
- Steven L Wesselingh3
- Maria C Inacio3,7
- Gillian E Caughey2,3,7
- 1 Wardliparingga Aboriginal Health Equity, South Australian Health and Medical Research Institute, Adelaide, SA
- 2 Adelaide Medical School, the University of Adelaide, Adelaide, SA
- 3 Registry of Senior Australians, South Australian Health and Medical Research Institute, Adelaide, SA
- 4 UQ Poche Centre for Indigenous Health, University of Queensland, Brisbane, QLD
- 5 SNAICC: National Voice for our Children, Victoria, Melbourne, VIC
- 6 Telethon Kids Institute, Adelaide, SA
- 7 UniSA Allied Health and Human Performance, University of South Australia, Adelaide, SA
Correspondence: gillian.caughey@unisa.edu.au
Open access:
Open access publishing facilitated by University of South Australia, as part of the Wiley – University of South Australia agreement via the Council of Australian University Librarians.
Data sharing:
The data underlying this report are not available for sharing because of restrictions imposed by the ethics and original data custodian approval.
This investigation was supported by a National Health and Medical Research Council (NHMRC) Ideas Grant (GNT2004089). Odette Pearson is supported by an NHMRC Investigator Grant (GNT2026852), Maria Inacio by a Hospital Research Foundation Mid‐Career Fellowship (MCF‐27‐2019) and an NHMRC Investigator Grant, (GNT119378), and Gillian Caughey by an NHMRC Investigator Grant (GNT2026400). The funding sources had no role in the study design, data collection, analysis or interpretation, reporting or publication.
We acknowledge the Registry of Senior Australians (ROSA) Aboriginal and Torres Strait Islander Advisory Committee: Lesley Nelson (Whadjuk/Ballardong, Noongar Nation), James Atkinson (Yorta Yorta/Bangerang), Kym Thomas (Nukunu), Antoinette Liddell (Wajarri/Yugunga‐Nya), Graham Aitken (Yankunytjatjara), Lauren Aitken (Yankunytjatjara), and Renee Blackman (Gubbi Gubbi).
We also acknowledge the ROSA Steering Committee, ROSA Consumer and Community Advisory Committee, and the ROSA South Australian Health and Medical Research Institute (SAHMRI) Research Team for ensuring the success of the ROSA and support for our study. We also acknowledge the South Australian Department for Innovation and Skills who supported the establishment of ROSA (2017–2021), the Medical Research Future Fund (2021–2024, PHRDI000009) and ROSA collaborating partners (SAHMRI, ECH Inc, Silver Chain, Life Care) for ongoing support, and the Australian Institute of Health and Welfare for the linkage of input data.
Odette Person is a guest editor for the NAIDOC Week MJA issue; Mario Inacio is an MJA deputy editor. Neither author was involved in decisions regarding the peer review or acceptance for publication of the manuscript for this article.
- 1. Australian Bureau of Statistics. Estimates and projections, Aboriginal and Torres Strait Islander Australians, 2001 to 2026 (3238.0). 30 Apr 2014. https://www.abs.gov.au/ausstats/abs@.nsf/products/c19a0c6e4794a3faca257cc900143a3d?opendocument (viewed Mar 2023).
- 2. Australian Bureau of Statistics. Estimates of Aboriginal and Torres Strait Islander Australians, 30 June 2021 (3238.0.55.001). 31 Aug 2023. https://www.abs.gov.au/statistics/people/aboriginal‐and‐torres‐strait‐islander‐peoples/estimates‐aboriginal‐and‐torres‐strait‐islander‐australians/latest‐release (viewed Mar 2023).
- 3. Randall DA, Lujic S, Havard A, et al. Multimorbidity among Aboriginal people in New South Wales contributes significantly to their higher mortality. Med J Aust 2018; 209: 19‐23. https://www.mja.com.au/journal/2018/209/1/multimorbidity‐among‐aboriginal‐people‐new‐south‐wales‐contributes‐significantly
- 4. Australian Institute of Health and Welfare. Insights into vulnerabilities of Aboriginal and Torres Strait Islander people aged 50 and over (AIHW cat. no. IHW 218). 30 July 2019. https://www.aihw.gov.au/reports/indigenous‐australians/vulnerabilities‐aboriginal‐torres‐strait‐50‐full/summary (viewed Sept 2023).
- 5. Royal Commission into Aged Care Quality and Safety. Final report: Care, dignity and respect. Volume 1: Summary and recommendations. 1 Mar 2021. https://www.royalcommission.gov.au/aged‐care/final‐report (viewed Mar 2023).
- 6. Australian Institute of Health and Welfare. Aged care for First Nations people. 7 Sept 2023. https://www.aihw.gov.au/reports/australias‐welfare/aged‐care‐for‐indigenous‐australians (viewed May 2024).
- 7. Australian Department of Health and Aged Care. National Aboriginal and Torres Strait Islander Flexible Aged Care Program. Canberra: Updated 2 June 2023. https://www.health.gov.au/our‐work/national‐aboriginal‐and‐torres‐strait‐islander‐flexible‐aged‐care‐program (viewed Mar 2023).
- 8. Thomas K, Dettwiller P, Gonzalez‐Chica D. Who cares about Aboriginal aged care? Evidence of home care support needs and use in rural South Australia. Aust J Rural Health 2023; 31: 704‐713.
- 9. Productivity Commission. Aged care services. In: Report on Government Services 2019; part F, chapter 14. 1 Feb 2019. https://www.pc.gov.au/ongoing/report‐on‐government‐services/2019/community‐services/aged‐care‐services (viewed Nov 2023).
- 10. Australian Department of Health and Aged Care. 2018–19 Report on the operation of the Aged Care Act 1997. 27 Nov 2019. https://www.health.gov.au/resources/publications/2018‐19‐report‐on‐the‐operation‐of‐the‐aged‐care‐act‐1997 (viewed Mar 2023).
- 11. Australian Department of Health and Aged Care. Reforms. In: Aged care supports for First Nations people. Updated 6 June 2023. https://www.health.gov.au/topics/aboriginal‐and‐torres‐strait‐islander‐health/aged‐care‐support#reforms (viewed May 2023).
- 12. Inacio MC, Caughey GE, Wesselingh S; ROSA Research Team and Steering Committee Members. Registry of Senior Australians (ROSA): integrating cross‐sectoral information to evaluate quality and safety of care provided to older people. BMJ Open 2022; 12: e066390.
- 13. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453‐1457.
- 14. Huria T, Palmer SC, Pitama S, et al. Consolidated criteria for strengthening reporting of health research involving indigenous peoples: the CONSIDER statement. BMC Med Res Methodol 2019; 19: 173.
- 15. Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS), volume 5: remoteness structure, July 2016 (1270.0.55.005). 16 Mar 2018. https://www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005 (viewed Jan 2024).
- 16. Australian Bureau of Statistics. IRSD. In: Census of Population and Housing: Socio‐Economic Indexes for Areas (SEIFA), Australia, 2016 (2033.0.55.001). 27 Mar 2018. https://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001 (viewed Jan 2024).
- 17. Inacio M, Amare A, Whitehead C, et al. Factors associated with accessing aged care services in Australia after approval for services: Findings from the historical cohort of the Registry of Senior Australians. Australas J Ageing 2020; 38: e382–e392.
- 18. Lindeman M, Smith K, LoGiudice D, Elliott M. Community care for Indigenous older people: an update. Australas J Ageing 2017; 36: 124‐127.
- 19. Wettasinghe PM, Allan W, Garvey G, et al. Older Aboriginal Australians’ health concerns and preferences for healthy ageing programs. Int J Environ Res Public Health 2020; 17: 7390.
- 20. Yashadhana A, Howie A, Veber M, et al. Experiences and perceptions of ageing among older First Nations Australians: a rapid review. Australas J Ageing 2022; 41: 8‐19.
- 21. Gibson C, Dudgeon P, Crockett J. Listen, look and learn: exploring cultural obligations of Elders and older Aboriginal people. J Occup Sci 2020; 27: 193‐203.
- 22. McCausland R, Jamieson S, Robinson V, et al. Elders’ perspectives and priorities for ageing well in a remote Aboriginal community. Ageing Soc 2023; https://doi.org/10.1017/S0144686X23000156.
- 23. Bourke S, Wright A, Guthrie J, et al. Evidence review of Indigenous culture for health and wellbeing. International Journal of Health Wellness and Society 2018; 8: 11‐27.
- 24. Parrella A, Pearson O, Davy C, et al. Understanding culturally safe aged care from the perspectives of older Aboriginal Australians in rural and remote communities. Health Promot J Austral 2022; 33: 566‐575.
- 25. Larke BM, Broe GA, Daylight G, et al. Patterns and preferences for accessing health and aged care services in older Aboriginal and Torres Strait Islander Australians. Australas J Ageing 2021; 40: 145‐153.
- 26. Davy C, Kite E, Aitken G, et al. What keeps you strong? A systematic review identifying how primary health‐care and aged‐care services can support the well‐being of older Indigenous peoples. Australas J Ageing 2016; 35: 90‐97.
- 27. Australian Government, Department of Health. 2020 Aged care workforce census report. 2 Sept 2021. https://www.health.gov.au/resources/publications/2020‐aged‐care‐workforce‐census?language=en (viewed Jan 2024).
- 28. Australian Department of Health and Aged Care. Aged care support for First Nations people. Updated 6 June 2023. https://www.health.gov.au/topics/aboriginal‐and‐torres‐strait‐islander‐health/aged‐care‐support (viewed May 2023).
- 29. Australian Institute of Health and Welfare. Cardiovascular disease, diabetes and chronic kidney disease: Australian facts: Aboriginal and Torres Strait Islander people (AIHW cat. no. CDK 5). 25 Nov 2015. https://www.aihw.gov.au/reports/indigenous‐australians/cardiovascular‐diabetes‐chronic‐kidney‐indigenous/summary (viewed Mar 2023).
- 30. Australian Bureau of Statistics. National Aboriginal and Torres Strait Islander Health Survey 2018–19. 11 Dec 2019. https://www.abs.gov.au/statistics/people/aboriginal‐and‐torres‐strait‐islander‐peoples/national‐aboriginal‐and‐torres‐strait‐islander‐health‐survey/latest‐release (viewed Mar 2023).
- 31. Caughey GE, Roughead EE. Multimorbidity research challenges: where to go from here? J Comorb 2011; 1: 8‐10.
- 32. Smith K, Gilchrist L, Taylor K, et al. Good spirit, good life: a quality of life tool and framework for older Aboriginal peoples. Gerontologist 2021; 13: e163‐e172.






Abstract
Objective: To characterise the socio‐demographic characteristics, aged and health care needs, and aged care services used by older Aboriginal and Torres Strait Islander people assessed for aged care service eligibility.
Study design: Population‐based retrospective cohort study; analysis of Registry of Senior Australians (ROSA) National Historical Cohort data.
Setting, participants: Aboriginal and Torres Strait Islander people aged 50 years or older who were first assessed for aged care service eligibility (permanent residential aged care, home care package, respite care, or transition care) during 1 January 2017 – 31 December 2019.
Major outcome measures: Socio‐demographic and aged care assessment characteristics; health conditions and functional limitations recorded at the time of the assessment; subsequent aged care service use.
Results: The median age of the 6209 people assessed for aged care service eligibility was 67 years (interquartile range [IQR], 60–75 years), 3626 were women (58.4%), and 4043 lived in regional to very remote areas of Australia (65.1%). Aboriginal health workers were involved in 655 eligibility assessments (10.5%). The median number of health conditions was six (IQR, 4–8); 6013 (96.9%) had two or more health conditions, and 2592 (41.8%) had seven or more. Comorbidity was most frequent among people with mental health conditions: 597 of 1136 people with anxiety (52.5%) and 1170 of 2416 people with depression (48.5%) had seven or more other medical conditions. Geriatric syndromes were recorded for 2265 people (36.5%); assistance with at least one functional activity was required by 6190 people (99.7%). A total of 6114 people (98.5%) were approved for at least one aged care service, 3218 of whom (52.6%) subsequently used these services; the first services used were most frequently home care packages (1660 people, 51.6%).
Conclusion: Despite the high care needs of older Aboriginal and Torres Strait Islander people, only 52% used aged care services for which they were eligible. It is likely that the health and aged care needs of older Aboriginal and Torres Strait Islander people are not being adequately met.