The known: The incidence of colorectal cancer is similar but the disease‐specific mortality higher among people with severe mental illness than other people. Differences in care may contribute to the difference, including a lower screening rate.
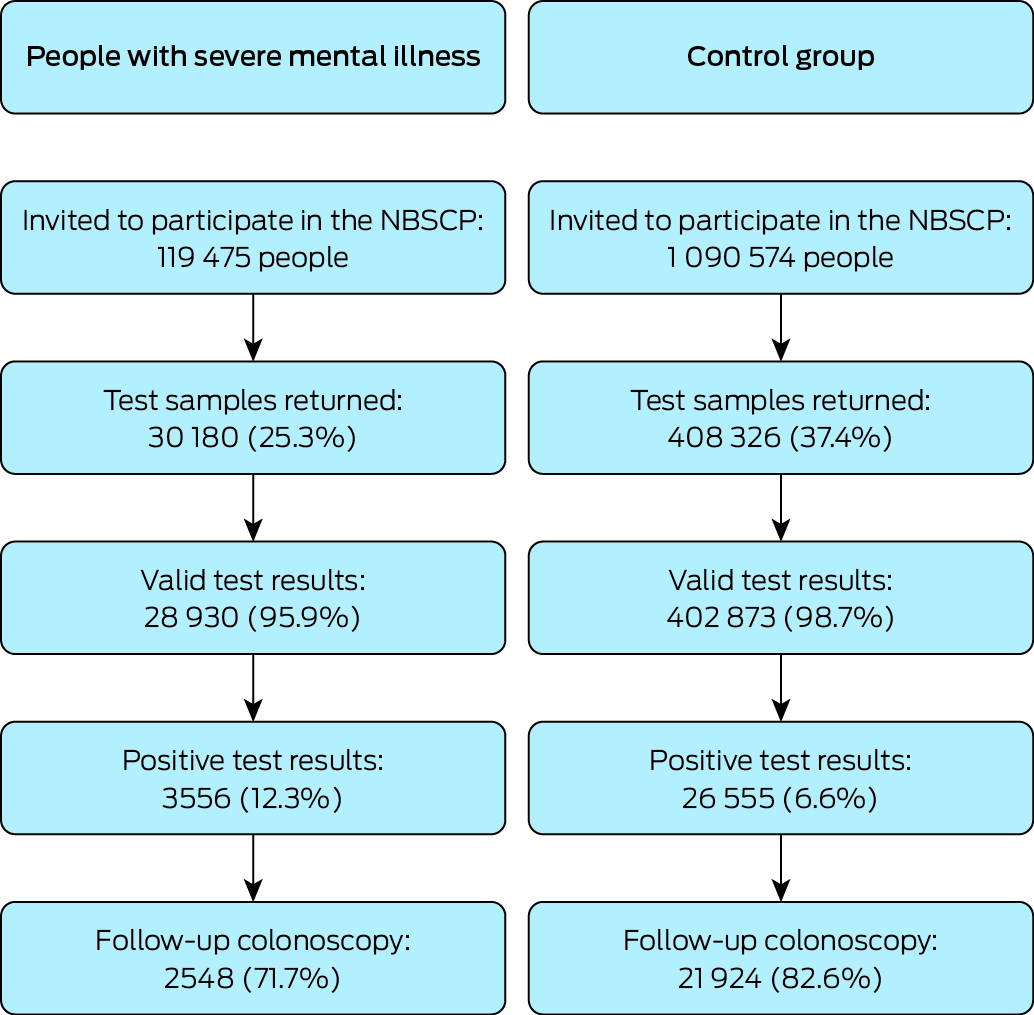
The new: Participation in the National Bowel Cancer Screening Program was significantly lower among people with severe mental illness than other Australians during 2006–2019. Their proportion of positive faecal occult blood test results was larger (12.3% v 6.6%), but the proportion who subsequently underwent colonoscopy was smaller (71.7% v 82.6%).
The implications: Barriers to screening may contribute to higher colorectal cancer case fatality rates in people with severe mental illness.
We have previously reported that people with psychiatric conditions who have colorectal cancer are up to 78% more likely to die from the condition than people without psychiatric illness;1,2 In some reports, the difference is greater for people with severe mental illness, such as schizophrenia.1As the incidence of colorectal cancer in people with mental illness and the general population is similar,1,2 the higher mortality may be linked with differences in cancer health care, including cancer screening.
A systematic review found in 2020 that the likelihood of breast and cervical cancer screening was lower for people with any type of mental illness, but no corresponding studies of colorectal cancer screening were identified.3 More recent studies in England4 and Australia5 have found lower adjusted colorectal cancer screening rates among people with severe mental illness; however, the Australian study was based on opportunistic screening in primary care rather than a population‐based screening program.5
The staged introduction of the Australian government‐funded, population‐based National Bowel Cancer Screening Program (NBCSP) began in August 2006.6 A faecal occult blood test kit for self‐sampling is mailed to people aged 50–74 years every two years. However, some priority populations, such as Indigenous people7 and people living in areas of lower socio‐economic status,8 may be less likely to participate in such programs than other people. The participation of people with severe mental illness has not been investigated. Anticipatory anxiety about possible subsequent procedures can also be a barrier to screening.9
In the Colorectal cancer Outcomes in people with Severe Mental Illness Cohort (COSMIC) study, we compared rates of NBCSP participation on first invitation and of colonoscopy after positive faecal occult blood test results for people with severe mental illness, identified by the prescribing of lithium or atypical antipsychotic agents, with those for people without severe mental illness or not prescribed antidepressants.
Methods
COSMIC is a retrospective cohort study based on the analysis of de‐identified linked administrative data. A pre‐study protocol was published10 and the study was prospectively registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12620000781943; 3 August 2020). Our report conforms with the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines.11
Definition of cases and controls
We analysed Pharmaceutical Benefits Scheme (PBS) data to identify people dispensed lithium or atypical antipsychotic agents, and therefore deemed likely to have a severe mental illness.10 Lithium is specifically indicated for the treatment of bipolar affective disorder, but is sometimes prescribed for treatment‐resistant depression;12 other uses are off‐label or experimental.13,14 Atypical antipsychotic prescribing for people with schizophrenia or bipolar affective disorder requires an indication‐specific authority code to qualify for PBS subsidisation. We defined cases as people who had been dispensed two or more prescriptions since 1 July 2002 (commencement date for the PBS dataset) to minimise the inclusion of off‐label prescribing. We included people aged 50–74 years on 1 January 2006 (start of the NBCSP) and eligible people who reached their 50th birthday by 31 December 2019. Later data were not included because of the impact of coronavirus disease 2019‐related restrictions on NBCSP participation from 2020.
For our population‐based comparison group, we randomly selected one in nine people aged 50–74 years from the Medicare Enrolments File (includes data for all people eligible for Medicare‐subsidised services) who had never been prescribed psychotropic medications (antipsychotics, lithium, antidepressants) from the commencement of the PBS dataset.
Outcomes
We used NBCSP data to assess participation (test invitations, test samples returned, proportion of valid test samples) and screening outcomes (test results, follow‐up colonoscopy after positive test results) during 1 August 2006 – 31 December 2019. A valid test result was defined as a conclusive (positive or negative) result; that is, the result was not inconclusive because the sample was incorrectly collected, spoiled or damaged during transport, or could not be processed for another reason. Colonoscopy procedure data were obtained from the Medicare Benefits Schedule (MBS) dataset (before 1 November 2019: MBS item numbers 32084, 32087–32090, 32093; from 1 November 2019: 32084, 32087, 32222–32229). Data for faecal occult blood tests performed outside the NBCSP from 1 January 2004 to 31 December 2019 (the latest available data) were obtained from the MBS dataset (item numbers 66764, 66767, 66770).
Statistical analysis
Characteristics of people with severe mental illness and the control group were initially compared as relative risks (RRs) with 95% confidence intervals (CIs); that is, the relative risk of people in a category being in the severe mental illness group, compared with the reference category for the characteristic. Incidence rate ratios (IRRs) comparing people with severe mental illness with people never prescribed psychotropic medications (control group) were estimated for four outcomes using Poisson regression:
- returning a test sample after being invited to participate (censored at the next invitation, death, or 31 December 2019);
- received a valid test result after returning a test sample;
- receiving a positive test result after returning a valid test sample; and
- undergoing follow‐up colonoscopy after a positive test result.
We used robust variance estimates and included an offset for time at risk (in person‐years) to account for differences in follow‐up time; it was calculated from 2006 (NBCSP commencement date) or the year in which an individual was first eligible for screening, whichever was later. If an individual was eligible for screening before they were dispensed lithium or an atypical antipsychotic agent, the time prior to the prescription was treated as unexposed. Colonoscopies were counted only if undertaken between receiving the positive test result and receiving a subsequent NBCSP invitation (or within two years if no further invitations were made). Covariates included age at time of invitation, sex, and postcode‐based residential remoteness (Accessibility/Remoteness Index of Australia15) and socio‐economic status (Index of Relative Socio‐economic Advantage and Disadvantage16). Indigenous status is collected by the NBCSP for people with positive test results, but the degree of missing data prevented including it as a covariate. A preliminary analysis found that the likelihood of responding to second or subsequent NBCSP screening invitations was heavily dependent on participation when first invited; we therefore focused on first invitations to simplify the analysis and remove prior participation as a factor.
Ethics approval
The University of Queensland Human Research Ethics Committee (2019000296) and the Australian Institute of Health and Welfare Ethics Committee (E2019‐5‐1108) approved the study.
Results
A total of 1 210 049 people invited to participate in the NBCSP were included in our analysis: 119 475 with severe mental illness and 1 090 574 who comprised our control group (Box 1). The proportion of women was larger in the severe mental illness group (51.3%) than the control group (48.7%; RR, 1.36; 95% CI, 1.34–1.38), as were the proportions who lived in inner regional areas (23.5% v 19.1%; v major cities: RR, 1.34; 95% CI, 1.31–1.37) or in areas in the lowest socio‐economic quintile (21.8% v 14.7%; v highest quintile: RR, 2.45; 95% CI, 2.40–2.50) (Box 2).
A total of 438 506 people (36.2%) participated in the NBCSP (ie, returned test samples); the participation rate was lower among people with severe mental illness than in the control group (25.7% v 37.4%; IRR, 0.68; 95% CI, 0.67–0.69). The participation rate was also lower among people in remote areas than in major cities (28.3% v 35.7%; IRR, 0.68; 95% CI, 0.67–0.69), and among people living in areas of greatest socio‐economic disadvantage than in areas of lowest socio‐economic disadvantage (33.0% v 38.3%; IRR, 0.86; 95% CI, 0.85–0.87). The proportion of women who participated was larger than that of men (39.0% v 31.9%; IRR, 1.17; 95% CI, 1.16–1.17); the participation rate was higher in inner (38.5%; IRR, 1.08; 95% CI, 1.08–1.09) and outer regional areas (38.5%; IRR, 1.05; 95% CI, 1.04–1.06) than in major cities. By age group, participation was highest for people aged 65–69 years (45.1%) and lowest for those aged 50–54 years (31.3%) (Box 3).
In the adjusted analyses, the participation rate was lower among people with severe mental illness (adjusted IRR, 0.70; 95% CI, 0.69–0.84). The proportion of valid test results was smaller for people with severe mental illness (95.9% v 98.7%; adjusted IRR, 0.97; 95% CI, 0.96–0.99), and the positive test result proportion was larger (12.3% v 6.6%; adjusted IRR, 2.01; 95% CI, 1.94–2.09). The proportion of positive test results followed by colonoscopy was smaller for people with severe mental illness (71.7% v 82.6%; adjusted IRR, 0.88; 95% CI, 0.85–0.92) (Box 4).
Discussion
In our large national study, we found that NBCSP participation was significantly lower among people prescribed medications for bipolar disorder and schizophrenia than other people. Further, valid screening test results were less likely for people with severe mental illness who participated, they were more likely to receive positive test results, and those with positive results were less likely to undergo follow‐up colonoscopy. The proportion of women was larger in the severe mental illness group than the control group, reflecting the gender distribution of these diagnoses in older age groups.17,18 Overall participation (both groups) was similar to that reported for the NBCSP as a whole.19,20 As also reported by Cancer Australia,19 participation was also lower in areas of greater socio‐economic disadvantage, and in remote areas than in major cities, while participation was higher among women, increased with age, and was higher among people in inner or outer regional areas than in major cities.
Our finding that the NBCSP screening rate was lower among people with severe mental illness was consistent with the lower opportunistic colorectal cancer testing rate in primary care, after adjustment for age, gender, and number of clinic visits, found by the analysis of a 10% PBS dispensing data sample for 2004–2014.5 The NBCSP has not reduced inequity in bowel cancer screening for people with severe mental illness, similar to findings in England of lower screening participation among people with severe mental illness (42.11% v 58.89%).4
Our findings suggest that access to screening may be one factor in poorer colorectal cancer outcomes for people with severe mental illness. However, the influence of other factors along the colorectal cancer care pathway, from screening to end‐of‐life care, should also be investigated. For instance, we found in our recent systematic review that people with severe mental illness were less likely to receive colorectal cancer treatment (any, surgical resection, or adjuvant therapy), even after adjustment for socio‐demographic characteristics and cancer stage at the time of presentation.21 Cancer stage is potentially an important factor, as people with mental illness are more likely than other people to have more advanced cancer at diagnosis.1
Strategies for increasing NBCSP participation by people with severe mental illness could include alternative approaches to distributing test kits, such as providing them in mental health services for opportunistic screening, together with dedicated health personnel for follow‐up and support. In Japan, case management, including education and patient navigation, increased participation in colorectal cancer screening by people with schizophrenia.22 Identifying other barriers in the colorectal cancer care pathway should also be investigated, including their effects on outcomes; delays at some stages may be more harmful than others, depending on age.23 More broadly, our findings indicate the need to consider people with mental illness as a priority group at risk of poorer colorectal cancer outcomes.
Limitations
We used prescription authority codes rather than medical records to define cases of severe mental illness, and these codes do not capture private prescriptions or people not using any other medications. However, these omissions would include only a small proportion of people with severe mental illness. An Australian survey of adults aged 18–64 years with psychotic illness and in contact with public specialist mental health services during 2009 and 2010 found that 81.6% were taking prescribed antipsychotic medications;24 further, private prescriptions account for fewer than 10% of all community medication prescriptions.25 Similarly, some prescriptions of first generation antipsychotics, which do not require authority codes, may have been off‐label prescriptions for conditions other than severe mental illness (eg, organic brain syndromes). In an American study, for instance, first generation antipsychotics accounted for about 20% of off‐label antipsychotic prescribing for Department of Veterans Affairs patients.26 However, less than 14% of antipsychotics dispensed in Australia during 2015–20 were first generation antipsychotics.27
Some second generation antipsychotic prescriptions may not have been for people with severe mental illness (ie, incorrect use of authority codes); we therefore excluded second generation antipsychotic prescriptions with authority codes for behavioural disturbances associated with dementia, as well as people prescribed low‐dose antipsychotics. Lithium can be prescribed as adjuvant therapy for people with treatment‐resistant depression, but the most frequent indication is bipolar disorder. Finally, we restricted our analyses to people eligible for the NBCSP (50–74 years of age).
The general effect of any misclassification of whether people had severe mental illness in our analyses would be underestimation of differences between the two groups; that is, our estimates are conservative. In addition, as the MBS database does not include information on colonoscopies in public hospitals, the availability of this information depended on clinicians directly informing the NBCSP; without access to state and territory hospitals data, we could not assess how often this was not provided, and we may have underestimated colonoscopy rates among people with severe mental illness, as they are especially likely to use public hospital care. Nevertheless, the data we analysed is more likely to be nationally representative than data analysed in studies that require individual consent.
We could not include Indigenous status as a covariate in our analysis because the NBCSP data is incomplete for this characteristic. However, as the proportion of Indigenous people in Australia is about 4%, it is unlikely that this factor would explain the differences between people with and without severe mental illness we have reported. The rate of participation in colorectal cancer screening programs is lower for Indigenous than non‐Indigenous people,7 and screening rates among Indigenous Australians with severe mental illness should therefore be investigated.
We restricted the study period to before the coronavirus disease 2019 (COVID‐19) pandemic, as it may have affected screening behaviour and outcomes; we therefore assessed neither its immediate nor its long term effects. Finally, we assessed process measures, not clinical outcomes.
Conclusion
In our large population‐based study of people with access to universal health care, we found that participation in the NBCSP was lower among people with severe mental illness, and their rate of follow‐up colonoscopy after positive test results was also lower. As differences in screening frequency may partially explain the higher mortality associated with colorectal cancer in people with severe mental illness, the screening of people in this disadvantaged group must be improved.
Box 1 – National Bowel Cancer Screening Program (NBCSP) participation and outcomes for people aged 50–74 years with severe mental illness and for a randomly selected control group of people aged 50–74 years, Australia, 2006–2019
Box 2 – Baseline characteristics of people aged 50–74 years with a severe mental illness (prescribed lithium or atypical antipsychotic agents) and a randomly selected control group of people aged 50–74 years, Australia, 2006–2019
|
Characteristic |
Control group |
People with severe mental illness |
Unadjusted relative risk (95% CI)* |
||||||||||||
|
|
|||||||||||||||
|
Overall |
1 090 574 |
119 475 |
— |
||||||||||||
|
Sex |
|
|
|
||||||||||||
|
Men |
605 949 (55.6%) |
58 227 (48.7%) |
1 |
||||||||||||
|
Women |
484 625 (44.4%) |
61 248 (51.3%) |
1.36 (1.34–1.38) |
||||||||||||
|
Residential remoteness |
|
|
|
||||||||||||
|
Major cities |
775 499 (71.1%) |
80 455 (67.3%) |
1 |
||||||||||||
|
Inner regional |
208 562 (19.1%) |
28 046 (23.5%) |
1.34 (1.32–1.36) |
||||||||||||
|
Outer regional |
88 630 (8.1%) |
9713 (8.1%) |
1.06 (1.04–1.09) |
||||||||||||
|
Remote/very remote |
17 883 (1.6%) |
1261 (1.1%) |
0.66 (0.62–0.69) |
||||||||||||
|
Socio‐economic status (IRSD), quintile |
|
|
|
||||||||||||
|
5 (least disadvantage) |
304 194 (28.3%) |
22 073 (19.0%) |
1 |
||||||||||||
|
4 |
226 931 (21.1%) |
21 573 (18.6%) |
1.34 (1.31–1.37) |
||||||||||||
|
3 |
207 289 (19.3%) |
23 376 (20.1%) |
1.63 (1.59–1.66) |
||||||||||||
|
2 |
179 234 (16.7%) |
23 915 (20.6%) |
1.97 (1.93–2.01) |
||||||||||||
|
1 (most disadvantage) |
157 735 (14.7%) |
25 353 (21.8%) |
2.45 (2.40–2.50) |
||||||||||||
|
Missing data |
15 191 |
3185 |
— |
||||||||||||
|
Age group at first invitation (years) |
|
|
|
||||||||||||
|
50–54 |
548 416 (50.3%) |
68 052 (57.0%) |
1 |
||||||||||||
|
55–59 |
260 678 (23.9%) |
24 555 (20.6%) |
0.73 (0.72–0.75) |
||||||||||||
|
60–64 |
14 940 (1.4%) |
694 (0.6%) |
0.34 (0.32–0.37) |
||||||||||||
|
65–69 |
255 918 (23.5%) |
25 376 (21.2%) |
0.78 (0.77–0.79) |
||||||||||||
|
70–74 |
10 622 (1.0%) |
798 (0.7%) |
0.57 (0.53–0.62) |
||||||||||||
|
Year of first invitation |
|
|
|
||||||||||||
|
2006–2007 |
87 362 (8.0%) |
6601 (5.5%) |
1 |
||||||||||||
|
2008–2010 |
282 162 (25.9%) |
26 075 (21.8%) |
1.25 (1.21–1.28) |
||||||||||||
|
2011–2013 |
319 311 (29.3%) |
35 382 (29.6%) |
1.53 (1.48–1.57) |
||||||||||||
|
2014–2016 |
243 569 (22.3%) |
29 977 (25.1%) |
1.72 (1.67–1.77) |
||||||||||||
|
2017–2019 |
158 170 (14.5%) |
21 440 (17.9%) |
1.92 (1.86–1.98) |
||||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; IRSD = Index of Socio‐Economic Disadvantage. * That is, the relative risk of included people in category being in the severe mental illness group, compared with the reference category for the characteristic. |
|||||||||||||||
Box 3 – Participation in the National Bowel Cancer Screening Program, Australia, 2006–2019, by people aged 50–74 years with a severe mental illness and a randomly selected control group of people aged 50–74 years*
|
Characteristic |
Participated |
Did not participate |
Unadjusted incidence rate ratio (95% CI) |
||||||||||||
|
|
|||||||||||||||
|
Study group |
438 506 |
771 543 |
|
||||||||||||
|
Control |
408 326 (37.4%) |
682 248 (62.6%) |
1 |
||||||||||||
|
Severe mental illness |
30 180 (25.3%) |
89 295 (74.7%) |
0.68 (0.67–0.69) |
||||||||||||
|
Sex |
|
|
|
||||||||||||
|
Men |
211 940 (31.9%) |
438 589 (68.1%) |
1 |
||||||||||||
|
Women |
212 919 (39.0%) |
332 954 (61.0%) |
1.17 (1.16–1.17) |
||||||||||||
|
Residential remoteness |
|
|
|
||||||||||||
|
Major cities |
305 245 (35.7%) |
550 709 (64.3%) |
1 |
||||||||||||
|
Inner regional |
91 202 (38.5%) |
145 406 (61.5%) |
1.08 (1.08–1.09) |
||||||||||||
|
Outer regional |
36 643 (37.3%) |
61 700 (62.7%) |
1.05 (1.04–1.06) |
||||||||||||
|
Remote/very remote |
5416 (28.3%) |
13 728 (71.7%) |
0.80 (0.78–0.81) |
||||||||||||
|
Socio‐economic status (IRSD), quintile |
|
|
|
||||||||||||
|
5 (least disadvantage) |
124 979 (38.3%) |
201 288 (61.7%) |
1 |
||||||||||||
|
4 |
91 802 (36.9%) |
156 702 (63.1%) |
0.96 (0.96–0.97) |
||||||||||||
|
3 |
83 082 (36.0%) |
147 583 (64.0%) |
0.94 (0.93–0.95) |
||||||||||||
|
2 |
72 402 (35.6%) |
130 747 (64.4%) |
0.93 (0.92–0.94) |
||||||||||||
|
1 (most disadvantage) |
60 436 (33.0%) |
122 652 (67.0%) |
0.86 (0.85–0.87) |
||||||||||||
|
Age group at first invitation (years) |
|
|
|
||||||||||||
|
50–54 |
193 041 (31.3%) |
423 427 (68.7%) |
1 |
||||||||||||
|
55–59 |
108 243 (37.9%) |
176 990 (62.1%) |
1.21 (1.20–1.22) |
||||||||||||
|
60–64 |
5620 (35.9%) |
10 014 (64.1%) |
1.15 (1.12–1.17) |
||||||||||||
|
65–69 |
126 797 (45.1%) |
154 497 (54.9%) |
1.44 (1.43–1.45) |
||||||||||||
|
70–74 |
4805 (42.1%) |
6615 (57.9%) |
1.34 (1.31–1.37) |
||||||||||||
|
Year of first invitation |
|
|
|
||||||||||||
|
2006–2007 |
40 542 (43.1%) |
53 421 (56.9%) |
1 |
||||||||||||
|
2008–2010 |
122 692 (39.8%) |
185 545 (60.2%) |
0.92 (0.91–0.93) |
||||||||||||
|
2011–2013 |
125 765 (35.5%) |
228 928 (64.5%) |
0.82 (0.81–0.83) |
||||||||||||
|
2014–2016 |
90 710 (33.2%) |
182 836 (66.8%) |
0.77 (0.76–0.78) |
||||||||||||
|
2017–2019 |
58 797 (32.7%) |
120 813 (67.3%) |
0.76 (0.75–0.77) |
||||||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * That is: returned faecal occult blood test samples. |
|||||||||||||||
Box 4 – National Bowel Cancer Screening Program screening participation and follow‐up for people aged 50–74 years with a severe mental illness and a randomly selected control group of people aged 50–74: univariate and multivariate regression analyses
|
|
|
|
Incidence rate ratio (95% CI) |
||||||||||||
|
Outcome |
Severe mental illness |
Control group |
Unadjusted |
Adjusted* |
|||||||||||
|
|
|||||||||||||||
|
Returned faecal occult blood test sample |
30 180 (25.3%) |
408 326 (37.4%) |
0.68 (0.67–0.69) |
0.70 (0.69–0.70) |
|||||||||||
|
Valid test result |
28 930 (95.9%) |
402 873 (98.7%) |
0.97 (0.96–0.98) |
0.97 (0.96–0.99) |
|||||||||||
|
Positive test result |
3556 (12.3%) |
26 555 (6.6%) |
1.96 (1.89–2.03) |
2.01 (1.94–2.09) |
|||||||||||
|
Colonoscopy after positive test result positive |
2548 (71.7%) |
21 924 (82.6%) |
0.90 (0.86–0.94) |
0.88 (0.85–0.92) |
|||||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * Adjusted for sex, postcode‐based residential remoteness and socio‐economic position (Index of Relative Socioeconomic Disadvantage), age at first invitation, and year of first invitation. |
|||||||||||||||
Received 15 November 2023, accepted 15 March 2024
- Steve Kisely1
- Rebecca Seth2
- Susan J Jordan1
- Bradley Kendall1
- Dan J Siskind1,3
- Grant Sara4,5
- Justin Chapman3
- Lisa Brophy6
- David M Lawrence2
- 1 The University of Queensland, Brisbane, QLD
- 2 Curtin University, Perth, WA
- 3 Metro South Addiction and Mental Health Service, Brisbane, QLD
- 4 The University of Sydney, Sydney, NSW
- 5 NSW Ministry of Health, Sydney, NSW
- 6 La Trobe University, Melbourne, VIC
Data Sharing:
The data underlying this report are held in the Secure Unified Research Environment (SURE) at the Sax Institute in Sydney, and used with permission from the Australian Institute of Health and Welfare and relevant data custodians. The linked administrative data used in this study are owned by the respective government agencies and cannot be made available to third parties by the authors.
This study was funded by Cancer Australia (APP1157870) and is affiliated with the ALIVE National Centre for Mental Health Research Translation. Dan Siskind holds a National Health and Medical Research Council Early Career Fellowship (GNT11111136). The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
No relevant disclosures.
- 1. Kisely S, Crowe E, Lawrence D. Cancer‐related mortality in people with mental illness. JAMA Psychiatry 2013; 70: 209‐217.
- 2. Kisely S, Sadek J, MacKenzie A, et al. Excess cancer mortality in psychiatric patients. Can J Psychiatry 2008; 53: 753‐761.
- 3. Solmi M, Firth J, Miola A, et al. Disparities in cancer screening in people with mental illness across the world versus the general population: prevalence and comparative meta‐analysis including 4 717 839 people. Lancet Psychiatry 2020; 7: 52‐63.
- 4. Kerrison RS, Jones A, Peng J, et al. Inequalities in cancer screening participation between adults with and without severe mental illness: results from a cross‐sectional analysis of primary care data on English screening programmes. Br J Cancer 2023; 129: 81‐93.
- 5. Tuesley KM, Jordan SJ, Siskind DJ, et al. Colorectal, cervical and prostate cancer screening in Australians with severe mental illness: retrospective nation‐wide cohort study. Aust N Z J Psychiatry 2019; 53: 550‐558.
- 6. Ee HC, St John J. The National Bowel Cancer Screening Program: time to achieve its potential to save lives. Public Health Res Pract 2019; 29: 2921915.
- 7. Christou A, Katzenellenbogen JM, Thompson SC. Australia's national bowel cancer screening program: does it work for Indigenous Australians? BMC Public Health 2010; 10: 373.
- 8. von Wagner C, Baio G, Raine R, et al. Inequalities in participation in an organized national colorectal cancer screening programme: results from the first 2.6 million invitations in England. Int J Epidemiol 2011; 40: 712‐718.
- 9. Goodwin B, Anderson L, Collins K, et al. Anticipatory anxiety and participation in cancer screening. A systematic review. Psychooncology 2023; 32: 1773‐1786.
- 10. Protani MM, Jordan SJ, Kendall BJ, et al. Colorectal cancer Outcomes in people with Severe Mental Illness Cohort (COSMIC): a protocol for an Australian retrospective cohort using linked administrative data. BMJ Open 2021; 11: e044737.
- 11. von Elm E, Altman DG, Egger M, et al; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61: 344‐349.
- 12. Malhi GS, Bell E, Bassett D, et al. The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry 2021; 55: 7‐117.
- 13. Singh A, Arora S, Chavan M, et al. An overview of the neurotrophic and neuroprotective properties of the psychoactive drug lithium as an autophagy modulator in neurodegenerative conditions. Cureus 2023; 15: e44051.
- 14. Lund NLT, Petersen AS, Fronczek R, et al. Current treatment options for cluster headache: limitations and the unmet need for better and specific treatments: a consensus article. J Headache Pain 2023; 24: 121.
- 15. Australian Bureau of Statistics. Remoteness structure. Australian Statistical Geography Standard (ASGS), edition 3, July 2021 – June 2026. 20 July 2021. https://www.abs.gov.au/statistics/standards/australian‐statistical‐geography‐standard‐asgs‐edition‐3/latest‐release (viewed Oct 2023).
- 16. Australian Bureau of Statistics. Index of Relative Socio‐economic Disadvantage (IRSD). In: Socio‐Economic Indexes for Areas (SEIFA), Australia, 2021. 27 Apr 2021. https://www.abs.gov.au/statistics/people/people‐and‐communities/socio‐economic‐indexes‐areas‐seifa‐australia/latest‐release#index‐of‐relative‐socio‐economic‐disadvantage‐irsd‐ (viewed Oct 2023).
- 17. Kirkbride JB, Errazuriz A, Croudace TJ, et al. Incidence of schizophrenia and other psychoses in England, 1950–2009: a systematic review and meta‐analyses. PLoS One 2012; 7: e31660.
- 18. Kisely S, Xiao J, Jian L. Changes in determinants of compulsory community treatment over 11 years. A population‐based analysis of linked mental health databases. Psychiatry Res 2015; 230: 400‐405.
- 19. National Cancer Control Indicators. Colorectal screening rate. 12 Oct 2023. https://ncci.canceraustralia.gov.au/screening/colorectal‐screening‐rates/colorectal‐screening‐rates (viewed Aug 2023).
- 20. Worthington J, Lew JB, Feletto E, et al. Improving Australian National Bowel Cancer Screening Program outcomes through increased participation and cost‐effective investment. PLoS One 2020; 15: e0227899.
- 21. Protani MM, Alotiby MKN, Seth R, et al. Colorectal cancer treatment in people with severe mental illness: a systematic review and meta‐analysis. Epidemiol Psychiatr Sci 2022; 31: e82.
- 22. Fujiwara M, Yamada Y, Shimazu T, et al. Encouraging participation in colorectal cancer screening for people with schizophrenia: a randomized controlled trial. Acta Psychiatr Scand 2021; 144: 318‐328.
- 23. Castelo M, Sue‐Chue‐Lam C, Paszat L, et al. Clinical delays and comparative outcomes in younger and older adults with colorectal cancer: a systematic review. Curr Oncol 2022; 29: 8609‐8625.
- 24. Morgan VA, Waterreus A, Jablensky A, et al. People living with psychotic illness in 2010: the second Australian national survey of psychosis. Aust N Z J Psychiatry 2012; 46: 735‐752.
- 25. Australian Department of Health. Australian statistics on medicines 2011. 2013. https://www.pbs.gov.au/statistics/asm/2011/australian‐statistics‐on‐medicines‐2011.pdf (viewed Aug 2023).
- 26. Leslie DL, Mohamed S, Rosenheck RA. Off‐label use of antipsychotic medications in the department of Veterans Affairs health care system. Psychiatr Serv 2009; 60: 1175‐1181.
- 27. Taylor M, Dangelo‐Kemp D, Liu D, et al. Antipsychotic utilisation and persistence in Australia: a nationwide 5‐year study. Aust N Z J Psychiatry 2022; 56: 1155‐1163.






Abstract
Objective: To compare rates of participation in the National Bowel Cancer Screening Program (NBCSP) and follow‐up for people with severe mental illness with those for people without severe mental illness or not prescribed antidepressants.
Study design: Retrospective cohort study; analysis of de‐identified linked NBCSP, Pharmaceutical Benefits Scheme (PBS), and Medicare Benefits Schedule (MBS) data.
Setting: Australia, 2006–2019.
Participants: People aged 50–74 years (NBCSP‐eligible) with severe mental illness, defined as those dispensed two or more prescriptions for second generation antipsychotics or for lithium (PBS data), and a random sample of people aged 50–74 years eligible for Medicare‐subsidised services but never prescribed psychotropic medications (antipsychotics, lithium, antidepressants).
Main outcome measures: NBCSP participation (returned faecal occult blood test sample), valid test result, positive test result, and follow‐up colonoscopy rates.
Results: A total of 119 475 people with severe mental illness and 1 090 574 control group people were included in our analyses. The proportion of women was larger in the severe mental illness group (51.3%) than the control group (48.7%), as were the proportions who lived in inner regional areas (23.5%v 19.1%) or in areas in the lowest socio‐economic quintile (21.8% v 14.7%). The NBCSP participation rate was lower among people with severe mental illness (adjusted incidence rate ratio [IRR], 0.70; 95% confidence interval [CI], 0.69–0.84). The proportion of valid test results was smaller for people with severe mental illness (95.9% v 98.7%; adjusted IRR, 0.97; 95% CI, 0.96–0.99), and the positive test result proportion larger (12.3% v 6.6%; adjusted IRR, 2.01; 95% CI, 1.94–2.09). The proportion of positive test results followed by colonoscopy was smaller for people with severe mental illness (71.7% v 82.6%; adjusted IRR, 0.88; 95% CI, 0.85–0.92).
Conclusions: People with severe mental illness were less likely to participate in the NBCSP or to undergo colonoscopy after a positive test result than other Australians. These differences may contribute to higher colorectal cancer mortality among people with severe mental illness. The contributions of differences in cancer stage at diagnosis and subsequent treatment to higher colorectal cancer mortality require further study.