The known: Culturally safe programs for improving the health of Aboriginal and Torres Strait Islander people living in remote communities are needed.
The new: A novel community-developed and -led dietary and lifestyle intervention focused on knowledge sharing, empowerment, and health coaching was associated with improved cardiometabolic health, and was well received by participants.
The implications: Culturally acceptable strategies for improving cardiometabolic risk factors could reduce the burden of cardiometabolic disease in remote Aboriginal and Torres Strait Islander communities. Embedding successful elements of this program in local services could improve the sustainability and better management of health services.
Aboriginal and Torres Strait Islander people were healthy and strong before Europeans arrived in Australia.1 However, the rate of type 2 diabetes among Indigenous people living in remote areas is now 8.8 times that for non-Indigenous Australians, and that of cardiovascular disease twice as high.2 These differences are underpinned by social, political, and economic inequities that have persisted since colonisation. During 2009–2017, the rate of avoidable deaths in Australia was highest in East Arnhem, home to the proud and culturally rich Yolŋu people, predominantly because of diabetes and cardiovascular disease.3
The Close the Gap campaign supports the genuine involvement of Aboriginal and Torres Strait Islander peoples in the design and delivery of programs and services that affect them.4 Solutions that are evidence-based, sustainable, and grounded in community development are required.5 Daily habits and actions profoundly affect the risk of chronic disease. Increased physical activity, healthy diet, weight management, reducing smoking, and stress reduction are all key approaches that lower the risk of cardiovascular disease and enhance quality of life.6,7 In 2016, the Hope for Health program, a novel dietary and lifestyle intervention focused on developing a shared understanding of physiological processes in metabolic health, empowerment, and health coaching, was co-designed with a group of senior Yolŋu women and successfully piloted.8,9 The program uses Mar?gikunhamirr (making known and sharing understanding) and Go?-?ayathanhamirr (supporting and walking alongside each other) to empower Yolŋu to gain control of their metabolic health.
Hope for Health promotes self-determined lifestyle changes to improve health and mitigate or prevent chronic disease. Yolŋu concepts, knowledge, and traditional practices are used to share information about the biological and socio-economic factors related to colonisation that lead to poor health. Go?-?ayathanhamirr, or health coaching, supports goal setting for individual solutions implemented at home on the basis of education and their experiences. The approach also aims to provide positive role models within kin networks and the community, potentially bringing broader community benefits.10
We comprehensively evaluated the Hope for Health program. The primary objective was to assess whether at least 10% of participants achieved clinically significant weight loss (at least 5% of initial weight) by the end of the four month program. Secondary objectives were to assess changes in metabolic markers, diet, and physical activity. As an exploratory objective, participant perceptions of Hope for Health were assessed in a process designed and led by Indigenous people.
Methods
We undertook a single arm, pre–post intervention study of the Hope for Health program, registered prospectively with the Australian New Zealand Clinical Trials Registry (ACTRN12622000174785; 2 February 2022). We initially co-designed a randomised controlled trial with a Yolŋu steering committee and senior Yolŋu researchers (authors GG, JD), reaching mutual understanding through discussions and presentations in Yolŋu Matha (Yolŋu language). However, unforeseen circumstances necessitated a protocol change at the time of recruitment: strong community concern because of worry that health might deteriorate were the program delayed (control group participants would have received the intervention eight months later, after the wet season); hesitation about participating without other household members also participating (which would have introduced a clustering effect); and a coronavirus disease 2019 (COVID-19) outbreak that closed the community, reducing the time for community sensitisation. For these reasons, neither an adequately powered randomised controlled trial nor another randomised design was practical. A pre–post evaluation with an adequate sample size was considered the most appropriate alternative, and this design received ethics approval on 18 July 2022, by which time all participants had been recruited (but not yet randomised) and were informed of the design change. We report our study according to CONSORT guidelines.11
Setting
The study was conducted in a remote northeast Arnhem Land community of about 2500 people. In this community, the prevalence of diabetes is highest among middle-aged people (40–60 years); during routine testing of 190 people in 2022, glycated haemoglobin (HbA1c) levels were high (greater than 54 mmol/mol) in 110 people (58%) (unpublished data).
The research team, distinct from the Hope for Health program team, undertook outcome assessments in the Miwatj Health Aboriginal Corporation ancillary health clinic in collaboration with Miwatj doctors. Recruitment and baseline assessments were conducted during 28 April – 15 July 2022, final assessments during 7 November – 14 December 2022. The Hope for Health program was delivered from 1 August to 30 November 2022.
Eligibility criteria
We disseminated information about the study through local organisations and in household visits. We recruited adult community residents (18–65 years) with body mass index (BMI) values of at least 25 kg/m2 or waist circumferences exceeding 94 cm (men) or 80 cm (women) who were willing to participate in the Hope for Health program and did not expect to leave the community for more than two weeks during the four months of the program. We excluded people who reported episodes of severe hypoglycaemia or ketoacidosis during the preceding twelve months, insulin-dependent diabetes, chronic renal failure that impaired daily function, cardiac failure, cirrhosis, other illnesses or conditions that would prevent participation, or pregnancy. The aim of these criteria was to include the community members at greatest risk of chronic disease and to ensure the safety of participants during the Hope for Health on-country (bush) retreat.
Hope for Health program
The Hope for Health program (Box 1) was led by a local steering committee of Yolŋu women, supported by a small Balanda (non-Indigenous) team.12 The program, delivered in Yolŋu language and concepts, provided knowledge about metabolic health and the causes of modern lifestyle diseases (Supporting Information, part 1). This information was shared in a supportive setting to encourage and allow people to make informed choices about how to manage the challenges of dietary and lifestyle improvement in their own way.
Outcomes
Baseline participant demographic, clinical, and lifestyle information, including smoking status, medication use, and allergies, were collected in standardised oral questionnaires, supplemented by review of electronic medical records. Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Melbourne.13
As lifestyle modification leading to even moderate weight loss (5%) improves cardiometabolic health and is a clinically meaningful goal for managing overweight and obesity,14 the primary outcome was defined as 5% weight loss. The secondary outcomes were changes in BMI, waist circumference, other metabolic markers (blood pressure, biomarkers of metabolic health and inflammation), diet,15 and physical activity16,17 (Box 2).
The exploratory outcome was participant perceptions, assessed in a process specifically designed and led by Indigenous researchers18 (Supporting Information, part 3).
Sample size
In the 2016 Hope for Health pilot evaluation, ten of 21 participants had lost at least 5% in weight four months after baseline. Without any intervention, we expected that fewer than 10% of participants would lose at least 5% weight over four months. Our primary hypothesis was that at least 10% of Hope for Health participants would achieve at least 5% weight reduction by the four-month endpoint. Assuming that 35% of study participants would experience at least 5% weight loss over four months, a total of 43 participants would provide greater than 95% power to detect a difference in the primary outcome between the intervention and control groups (a = 0.05, two-sided binomial test); to allow for 25% attrition, we estimated that 60 participants should be recruited for our study.
Statistical analysis
Continuous data were summarised as means with standard deviations (SDs) or medians with interquartile ranges (IQRs); categorical data were summarised as counts and proportions. Analyses included data for non-pregnant participants for whom complete weight data at baseline and program end were available (ie, per-protocol analysis). An additional analysis included all available data (ie, intention-to-treat analysis).
We estimated the proportion of participants who achieved at least 5% weight loss, with the Clopper–Pearson 95% confidence interval (CI). We also report the proportions (with 95% CI) of participants who achieved at least 3% weight loss (post hoc analysis) or at least 3 mmol/mol reduction in HbA1c level (a meaningful improvement for reducing the risk of long term diabetes complications19). We used a mixed effects model to estimate mean changes from baseline to program end (with 95% CIs) in weight, waist circumference, blood pressure, and blood levels of metabolic health and inflammation biomarkers (HbA1c, low-density lipoprotein [LDL] and high-density lipoprotein [HDL] cholesterol, triglycerides, C-reactive protein). The model included baseline and program end values as outcomes, time point as a covariate, and a random effect for participants; we used an unstructured variance–covariance matrix for repeated measures and the Kenward–Roger degrees of freedom approximation. C-reactive protein, HbA1c, and triglyceride values, visually assessed as being skewed, were log10 transformed before fitting the model.
Median changes in physical activity and dietary intake from baseline to program end were estimated using the Hodges–Lehmann estimator with distribution-free 95% CI, using large sample approximation.
Statistical analyses were performed in Stata 17.0. Analyses were not adjusted for multiple testing.
Ethics approval
Our study complied with the National Health and Medical Research Council Ethical conduct in research with Aboriginal and Torres Strait Islander Peoples and communities20 and the Declaration of Helsinki. The Northern Territory Health and Menzies School of Health Research Human Research Ethics Committee approved the study protocol (2021-4166). The Miwatj Health Board (16 March 2022), the East Arnhem Regional Council (2 December 2021), and the study-specific Data Safety Monitoring Board approved the study. Yolŋu researchers explained the consent form to participants in the local language.
Results
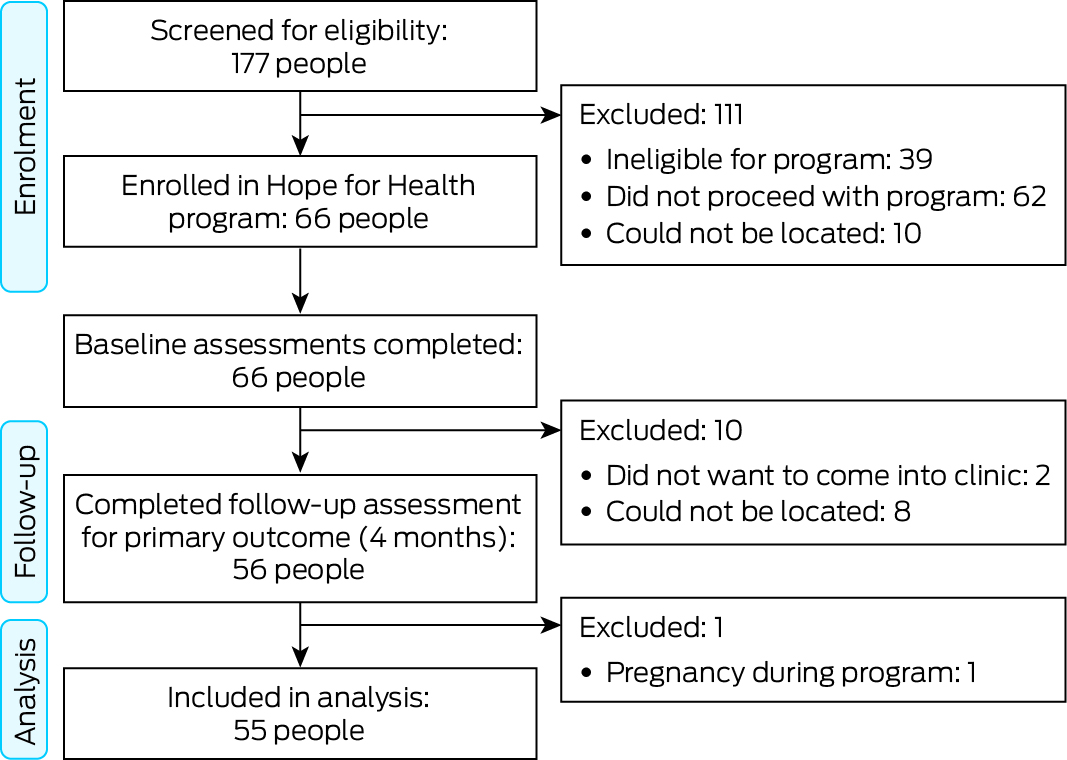
Of 177 people who registered interest in participation and provided consent to medical record review for eligibility screening, 138 (78%) were eligible and were invited to participate; 72 people did not subsequently proceed with the program or could not be located. A total of 66 people (37% of screened persons) provided consent to study participation and completed baseline assessments; data for the 55 participants who also completed the final study assessment were included in our analysis (Box 3). Mean follow-up time was 158 days (SD, 22 days).
The mean age of the 55 participants was 42.5 years (SD, 10.1 years); 36 were women (65%) (Box 4). HbA1c levels were high (48 mmol/mol or greater) in 17 participants (31%), LDL-cholesterol levels (2.5 mmol/L or greater) in 31 (63%), and C-reactive protein levels (greater than 5 mg/L) in 37 (69%); systolic blood pressure was greater than 135 mmHg in 18 participants (33%). Fifty-one participants (93%) reported at least one medical condition, most frequently liver impairment (30 participants), renal impairment (18 participants), or type 2 diabetes (17 participants). Thirty-five participants (64%) were prescribed at least one medication. The mean BMI was 30.7 kg/m2 (SD, 4.9 kg/m2; range, 20–42 kg/m2) (Box 5); the mean waist circumference was 109 cm for men (SD, 10 cm; range, 91–130 cm) and 109 cm for women (SD, 12 cm; range, 90–133 cm).
Medical practitioners reviewed the medical histories of all 66 people who enrolled in the Hope for Health program; 14 participants (21%) attended the on-country retreat, 56 (85%) attended home-based or individual health coaching, and 19 (29%) attended community group activities. The low attendance at the on-country retreat was predominantly because participants were away from the community (17 participants) or looking after children and other family members (15 participants) (Supporting Information, tables 1 and 2). Between baseline and program end, seven participants had changed medications on clinical advice; four participants had attended a hospital and 23 attended the health clinic (Supporting Information, table 3). One participant was pregnant at program end; their outcome values during pregnancy were set to missing for the outcomes analysis.
Primary outcome
Of the 55 participants for whom complete study weight data were available, 40 (73%) lost weight and 15 (27%) gained weight between baseline and program end; the mean weight loss for the 55 participants was 1.5 kg (95% CI, 0.5–2.4 kg). Ten participants (18%; 95% CI, 9–31%) achieved at least 5% weight reduction by program end; eighteen participants (33%; 95% CI, 21–41%) achieved at least 3% weight reduction (post hoc analysis).
Secondary outcomes
The mean change in BMI (53 participants) was –0.60 kg/m2 (95% CI, –0.93 to –0.27 kg/m2), in waist circumference (53 participants) –3.2 cm (95% CI, –4.7 to –1.7 cm), and in low-density lipoprotein cholesterol level (37 participants) –0.28 mmol/L (95% CI, –0.47 to –0.08 mmol/L); the relative decline in the HbA1c level geometric mean (50 participants) was 11% (95% CI, 6–15%), and the mean increase in high-density lipoprotein cholesterol level was 0.06 mmol/L (95% CI, 0.01–0.12 mmol/L) (Box 6). Declines in HbA1c level of 3 mmol/mol or larger were measured in 26 of 50 participants (52%; 95% CI, 37–66%); reductions in systolic blood pressure of 5 mmHg or more were measured in 20 of 52 participants (38%; 95% CI, 25–53%).
The changes in anthropometric, blood pressure, and blood biomarker values were similar when data for all 66 enrolled participants for whom data at baseline and/or study end were included (Supporting Information, table 4).
For the nineteen participants with evaluable activity data at both time points (it was not available for all 55 because of differences in their use of the monitors), the amount of moderate and vigorous physical activity increased by a median of 103 min/day (95% CI, 74–136 min/day). For the 45 participants who completed baseline and final dietary assessments, the intake of breads and cereals (median change, –1.5 [95% CI, –2.0 to –1.0] serves/day) and sugar-sweetened beverages (–0.6 [95% CI, –1.4 to –0.1] serves/day) declined and that of meat increased (1.1 [95% CI, 0.7–1.4] serves/day) (Box 7).
During the on-country retreat, eight adverse events were reported; none were serious, and three were probably intervention-related (bloating, back ache, headache) (Supporting Information, table 5).
Perceptions of the Hope for Health program
The Hope for Health focus on integrating healthy bodies and networks of kin, healthy governance, vibrant language and ceremony, and a healthy environment were seen as central to the value and benefit of the program. One participant reflected that: “Later the story will get good, the shop will understand the dhu?i-dhäwu (the ultimate truth of things). Come and try out the Hope for Health, your future and your children's future … that's the story from me” (further results for this outcome: Supporting Information, part 3).
Discussion
A substantial proportion of the overweight and obese adult participants in our study in a remote Indigenous community had hyperglycaemia, dyslipidaemia, hypertension, or elevated blood inflammatory marker levels. At the end of the four-month Hope for Health program, ten of 55 participants (18%) had achieved at least 5% weight loss. Improvements in other key metabolic health indicators were also noted, including declines in mean waist circumference, BMI, HbA1c, and LDL-cholesterol levels, and in median sugar-sweetened beverage intake. The mean HDL-cholesterol level and median moderate and vigorous physical activity increased. Clinically significant HbA1c level reductions (3 mmol/mol or more)21 were recorded for 26 of 50 people. The participants’ perceptions of the program were positive.
Eighteen participants (33%) achieved weight reduction of at least 3% by the end of the program. This degree of change has been associated with clinically meaningful reductions in HbA1c and triglyceride levels and in the risk of type 2 diabetes,22 while weight loss greater than 5% has been associated with reduced blood pressure and improved HDL- and LDL-cholesterol levels.14 In our study, systolic blood pressure declined by 5 mmHg or more for 20 of 52 participants (36%); a recent meta-analysis found that the risk of cardiovascular events fell by 10% for each 5 mmHg reduction in systolic blood pressure.23
Four of nine studies included in a systematic review of nutrition programs for Aboriginal and Torres Strait Islander Australians reported BMI reductions and differing effects on other metabolic markers; a meta-analysis of the effect on weight was not performed because of the small sample sizes and the heterogeneity of the studies.24 Two included studies reported statistically significant mean weight reductions: 3.3 kg over twelve months with the GutBuster program,25 and 2.1 kg over three months with the Get Healthy Service.26 Mean weight loss in our study was 1.5 kg (95% CI, 0.5–2.4 kg) over four months. Differences in weight loss between studies could be related to intervention characteristics (duration, intensity, adherence), population characteristics (Hope for Health was delivered in a complex cross-cultural environment in a remote community where English was a second language), study design, and baseline weight.
The Hope for Health program is a unique Yolŋu-led approach that uses traditional knowledge and concepts about diet and health to allow Yolŋu to integrate new knowledge about health and causes of illness.8 The genuine use of Yolŋu matha, liya, and rom (language, mindsets, and ways of being) is educationally effective but also values and acknowledges the interconnectedness of Indigenous health and wellbeing with identity, kinship, culture, and ancestral ways. The most successful element of the program (used by 56 of 66 participants) was individual home-based health coaching, particularly regarding understanding blood test results (informal participant feedback). The Hope for Health program as a whole, including its governance structure and the approach taken to deliver the program, is aligned with published recommendations regarding policies for advancing Aboriginal and Torres Strait Islander health equity and equality.4,27,28
The reductions in median intake of breads and cereals and sugar-sweetened beverages and the increase in meat intake in our study are consistent with the knowledge and health coaching provided by the Hope for Health program, which emphasises the health benefits of a traditional diet.29 The mean weight loss in our study was consistent with the findings of an American study of health professionals that reducing the consumption of refined grains, potatoes and other starchy vegetables, and sugar-sweetened beverages was associated with less weight gain during middle life, especially in overweight and obese people.30
Our study is the first to objectively measure physical activity in a remote community. Among the nineteen participants for whom adequate data were available, the median walking and moderate and vigorous physical activity time increased, as did the proportion of days on which they walked at least 30 minutes. These improvements could have a large effect on cardiometabolic risk indicators.31
Limitations
A randomised controlled trial would have provided stronger evidence for causal associations between the intervention and outcomes. Other authors have also reported difficulties with randomised controlled trials in Indigenous communities,32 and alternative study designs are needed. Without a control group, regression to the mean cannot be excluded, and we cannot infer causal relationships between the Hope for Health program and the changes reported. No other community health programs at the time of our study could explain the reported changes, and only two participants had medication changes that could have affected metabolic health. For the physical movement assessment, data were available for only 19 of 55 participants because of differences in their monitor use; participants who consistently wore monitors may have been more motivated than those who did not. As the program was conducted over four months, seasonality may have affected some outcomes; however, most foods consumed in the community were obtained from local stores supplied from the mainland with little variation throughout the year. Stand-alone retreats may not be sufficient for achieving sustainable changes in behaviour, but our retreat constituted only the initial twelve days of the four-month Hope for Health program.
Conclusions
We found that the four-month Hope for Health program was associated with clinically significant changes at the community level in several cardiometabolic risk factors for obese and overweight Aboriginal and Torres Strait Islander adults. Community support for the Hope for Health program and the improvements in cardiometabolic risk factors are encouraging, providing an example of a culturally sensitive, co-designed initiative led by Indigenous people for reducing the prevalence of chronic disease among Indigenous Australians in northeast Arnhem Land.5
Box 1 – Hope for Health program: overview*
|
Component |
Description |
||||||||||||||
|
|
|||||||||||||||
|
12-day retreat |
Immersive 12-day bush retreat focused on experiencing good health, reconnecting with the Yolŋu tradition of living, eating, and healing from the land, and learning about the body and health. Individual health coaching sessions explained pathology test results and explored health goals; support continued on return to the community. Traditional foods and activities are a daily part of the retreat. |
||||||||||||||
|
In-community support and mentoring |
Over 14 weeks following the retreat, focused on overcoming systemic barriers to instigating lifestyle changes. Includes group activities for identifying healthy food options at the store, storing and cooking fresh produce, hunting trips, walking, dancing, and yarning about healthy lifestyles. |
||||||||||||||
|
Individual and home-based health coaching |
During the retreat and subsequently in participants’ homes or chosen locations. Coaching about reviewing the results of health checks, videos about health, and yarning about chronic disease, the meaning of pathology test results, goal setting, and support. |
||||||||||||||
|
|
|||||||||||||||
|
* Further details on the Hope for Health program: Supporting Information, part 1; further details on study conduct: Supporting Information, part 2. |
|||||||||||||||
Box 2 – Procedures for each major assessment (pre- and post-intervention) in the Hope for Health single arm, pre–post intervention study, northeast Arnhem Land, Northern Territory, 2022
|
Assessment |
Description |
||||||||||||||
|
|
|||||||||||||||
|
Anthropometric measurements |
|
||||||||||||||
|
Weight (kg) |
Measured with Seca 803 digital weight scale by two trained personnel. |
||||||||||||||
|
Height (cm) |
Measured with Seca 213 portable stadiometer by two trained personnel. |
||||||||||||||
|
Waist circumference (cm) |
Measured with a measuring tape by two trained personnel. |
||||||||||||||
|
Blood pressure |
|
||||||||||||||
|
Systolic and diastolic blood pressure (mmHg) |
Single measurement in sitting position in a resting state by trained personnel using SphygmoCor XCEL device. |
||||||||||||||
|
Blood biomarkers of metabolic health and inflammation |
|
||||||||||||||
|
Haemoglobin A1c (reflecting blood glucose level over preceding 2–3 months), lipids (low- and high-density lipoprotein cholesterol, triglycerides), C-reactive protein |
Blood collected (non-fasting); analysis performed by Western Diagnostic Pathology (Jandakot, Western Australia). |
||||||||||||||
|
Dietary intake |
|
||||||||||||||
|
Daily intake (serves) of vegetables, fruit, breads and cereals, meat, dairy, sugar-sweetened beverages, discretionary foods, and traditional food |
The Menzies Remote Short-item Dietary Assessment Tool,15 a 32-item food frequency questionnaire used and validated in remote communities was administered by an experienced dietitian and a local researcher in Yolŋu Matha. |
||||||||||||||
|
Physical activity |
|
||||||||||||||
|
Walking (min/day), moderate and vigorous physical activity (min/day), proportion of days on which participant walked for at least 30 min, number of days monitored |
Assessed using research-grade activity monitors (ActiGraph GT9X) worn on the non-dominant wrist for seven days each at baseline and program end. Data were included if the activity monitor was worn for at least 600 minutes while awake for at least one day at baseline and endline. Validated algorithms were used to identify non-wear time16 and activity as walking and total moderate and vigorous activity (including walking and more intense activity.17 |
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – Enrolment and assessment of participants in the Hope for Health single arm, pre–post intervention study, northeast Arnhem Land, Northern Territory, 2022
Box 4 – Baseline demographic characteristics of enrolled and included participants in the Hope for Health single arm, pre–post intervention study, northeast Arnhem Land, Northern Territory, 2022
|
Characteristic |
Enrolled |
Included in analysis* |
|||||||||||||
|
|
|||||||||||||||
|
Number of participants |
66 |
55 |
|||||||||||||
|
Age (years), mean (SD) |
42.2 (9.7) |
42.5 (10.1) |
|||||||||||||
|
Age group (years) |
|
|
|||||||||||||
|
18–34 |
18 (28%) |
14 (25%) |
|||||||||||||
|
35–45 |
24 (36%) |
20 (36%) |
|||||||||||||
|
46–54 |
16 (24%) |
14 (25%) |
|||||||||||||
|
55–65 |
8 (12%) |
7 (13%) |
|||||||||||||
|
Gender |
|
|
|||||||||||||
|
Men |
22 (33%) |
19 (35%) |
|||||||||||||
|
Women |
44 (67%) |
36 (65%) |
|||||||||||||
|
Indigenous status |
|
|
|||||||||||||
|
Aboriginal |
61 (92%) |
50 (91%) |
|||||||||||||
|
Aboriginal and Torres Strait Islander |
5 (8%) |
5 (9%) |
|||||||||||||
|
Employment status |
|
|
|||||||||||||
|
Paid work |
25 (38%) |
24 (44%) |
|||||||||||||
|
Receives Centrelink benefits |
52 (79%) |
42 (76%) |
|||||||||||||
|
Highest level of education |
|
|
|||||||||||||
|
Year 7 or below |
3 (5%) |
3 (6%) |
|||||||||||||
|
Years 8–10 |
22 (34%) |
17 (32%) |
|||||||||||||
|
Years 11 or 12 |
34 (53%) |
29 (55%) |
|||||||||||||
|
Higher education |
5 (8%) |
4 (8%) |
|||||||||||||
|
Missing data |
2 |
2 |
|||||||||||||
|
Number of people living in house |
|
|
|||||||||||||
|
1–4 |
5 (8%) |
3 (5%) |
|||||||||||||
|
5 or 6 |
13 (20%) |
12 (22%) |
|||||||||||||
|
7–10 |
33 (50%) |
28 (51%) |
|||||||||||||
|
More than 10 |
15 (23%) |
12 (22%) |
|||||||||||||
|
Ownership |
|
|
|||||||||||||
|
Own a car |
19 (29%) |
13 (24%) |
|||||||||||||
|
Own a television |
22 (33%) |
17 (31%) |
|||||||||||||
|
Own a refrigerator |
49 (74%) |
40 (73%) |
|||||||||||||
|
Own an air conditioner |
43 (65%) |
37 (67%) |
|||||||||||||
|
|
|||||||||||||||
|
SD = standard deviation. * Non-pregnant participants for whom complete baseline and program end weight measurement data were available. |
|||||||||||||||
Box 5 – Baseline clinical characteristics of enrolled and included participants in the Hope for Health single arm, pre–post intervention study, northeast Arnhem Land, Northern Territory, 2022*
|
Characteristic |
Enrolled |
Included in analysis† |
|||||||||||||
|
|
|||||||||||||||
|
Number of participants |
66 |
55 |
|||||||||||||
|
Smoked at least one cigarette per day during preceding month |
|
|
|||||||||||||
|
No |
25 (38%) |
21 (38%) |
|||||||||||||
|
Yes |
41 (62%) |
34 (62%) |
|||||||||||||
|
Medications prescribed |
|
|
|||||||||||||
|
0 |
21 (33%) |
20 (36%) |
|||||||||||||
|
1 or 2 |
25 (38%) |
20 (36%) |
|||||||||||||
|
3–5 |
12 (18%) |
9 (16%) |
|||||||||||||
|
6 or more |
8 (12%) |
6 (11%) |
|||||||||||||
|
Medical conditions |
|
|
|||||||||||||
|
0 |
5 (8%) |
4 (7%) |
|||||||||||||
|
1 or 2 |
30 (45%) |
26 (47%) |
|||||||||||||
|
3–5 |
27 (41%) |
22 (40%) |
|||||||||||||
|
6 or more |
4 (6%) |
3 (5%) |
|||||||||||||
|
Allergies |
|
|
|||||||||||||
|
0 |
59 (89%) |
48 (87%) |
|||||||||||||
|
1 or 2 |
6 (9%) |
5 (9%) |
|||||||||||||
|
3–5 |
1 (2%) |
1 (2%) |
|||||||||||||
|
Body mass index (kg/m2), mean (SD) |
30.3 (5.4) |
30.7 (4.9) |
|||||||||||||
|
Healthy |
9 (14%) |
5 (9%) |
|||||||||||||
|
Overweight |
27 (41%) |
23 (42%) |
|||||||||||||
|
Obese |
30 (45%) |
27 (49%) |
|||||||||||||
|
Waist circumference (cm), mean (SD) |
108.6 (12.5) |
108.9 (11.1) |
|||||||||||||
|
Systolic blood pressure (mmHg), mean (SD) |
131.4 (16.5) |
131.7 (17.3) |
|||||||||||||
|
≤ 135 mmHg |
46 (70%) |
37 (67%) |
|||||||||||||
|
> 135 mmHg |
20 (30%) |
18 (33%) |
|||||||||||||
|
Diastolic blood pressure (mmHg), mean (SD) |
81.2 (11.6) |
80.8 (12.2) |
|||||||||||||
|
< 85 mmHg |
42 (64%) |
36 (65%) |
|||||||||||||
|
≥ 85 mmHg |
24 (36%) |
19 (35%) |
|||||||||||||
|
C-reactive protein (mg/L), median (IQR) |
8.5 (4.0–13.0) |
7.5 (4.0–13.0) |
|||||||||||||
|
≤ 5 mg/L |
19 (30%) |
17 (31%) |
|||||||||||||
|
> 5 mg/L |
45 (70%) |
37 (69%) |
|||||||||||||
|
Missing data |
2 |
1 |
|||||||||||||
|
HbA1c (mmol/mol), median (IQR) |
41.0 (37.0–51.0) |
41.0 (36.0–50.0) |
|||||||||||||
|
< 48 mmol/mol |
45 (68%) |
38 (69%) |
|||||||||||||
|
≥ 48 mmol/mol |
21 (32%) |
17 (31%) |
|||||||||||||
|
Cholesterol (mmol/L), mean (SD) |
4.9 (1.1) |
4.8 (1.1) |
|||||||||||||
|
< 4.0 mmol/L |
15 (23%) |
12 (22%) |
|||||||||||||
|
≥ 4.0 mmol/L |
51 (77%) |
43 (78%) |
|||||||||||||
|
Triglycerides (mmol/L), median (IQR) |
2.4 (1.6–3.5) |
2.4 (1.6–3.5) |
|||||||||||||
|
< 2.0 mmol/L |
24 (36%) |
20 (36%) |
|||||||||||||
|
≥ 2.0 mmol/L |
42 (64%) |
35 (64%) |
|||||||||||||
|
HDL-cholesterol (mmol/L), mean (SD) |
0.9 (0.2) |
0.9 (0.2) |
|||||||||||||
|
> 1.0 mmol/L |
13 (20%) |
9 (16%) |
|||||||||||||
|
≥ 1.0 mmol/L |
53 (80%) |
46 (84%) |
|||||||||||||
|
LDL-cholesterol (mmol/L), mean (SD) |
2.7 (0.9) |
2.7 (1.0) |
|||||||||||||
|
< 2.5 mmol/L |
22 (37%) |
18 (37%) |
|||||||||||||
|
≥ 2.5 mmol/L |
37 (67%) |
31 (63%) |
|||||||||||||
|
Missing data |
7 |
6 |
|||||||||||||
|
Cholesterol ratio (LDL:HDL), mean (SD) |
5.5 (1.3) |
5.5 (1.3) |
|||||||||||||
|
|
|||||||||||||||
|
HbA1c = glycated haemoglobin; HDL = high-density lipoprotein; IQR = interquartile range; LDL = low-density lipoprotein; SD = standard deviation. * Non-fasting blood collection. † Non-pregnant participants for whom complete baseline and program end weight measurement data were available. |
|||||||||||||||
Box 6 – Secondary outcomes (anthropometric, blood pressure, biomarker outcomes) for participants in the Hope for Health single arm, pre–post intervention study, northeast Arnhem Land, Northern Territory, 2022
|
Outcome |
Participants |
Baseline |
Program end |
Mean change (95% CI) |
|||||||||||
|
|
|||||||||||||||
|
Anthropometry |
|
|
|
|
|||||||||||
|
Weight (kg), mean (SD) |
55 |
85.1 (16.8) |
83.6 (17.0) |
–1.47 (–2.42 to –0.52) |
|||||||||||
|
Body mass index (kg/m2), mean (SD) |
53 |
30.6 (5.0) |
30.0 (5.2) |
–0.60 (–0.93 to –0.27) |
|||||||||||
|
Waist circumference (cm), mean (SD) |
53 |
108.9 (11.2) |
105.7 (11.5) |
–3.19 (–4.71 to –1.66) |
|||||||||||
|
Blood pressure |
|
|
|
|
|||||||||||
|
Systolic (mmHg), mean (SD) |
52 |
132.0 (17.4) |
131.1 (19.0) |
–0.94 (–4.83 to 2.95) |
|||||||||||
|
Diastolic (mmHg), mean (SD) |
52 |
81.3 (12.2) |
79.4 (12.8) |
–1.90 (–4.29 to 0.48) |
|||||||||||
|
Biomarkers |
|
|
|
|
|||||||||||
|
C-reactive protein (mg/L), median (IQR)* |
46 |
8.5 (4.0–13.0) |
9.0 (4.0–14.0) |
0.98 (0.76 to 1.26) |
|||||||||||
|
HbA1c (mmol/mol), median (IQR)* |
50 |
41.0 (37.0–50.0) |
39.0 (34.0–44.0) |
0.89 (0.85 to 0.94) |
|||||||||||
|
Cholesterol (mmol/L), mean (SD) |
50 |
4.8 (1.1) |
4.8 (1.6) |
0.01 (–0.30 to 0.31) |
|||||||||||
|
Triglycerides (mmol/L), median (IQR)* |
50 |
2.4 (1.6–3.6) |
2.5 (1.8–4.0) |
1.07 (0.91 to 1.25) |
|||||||||||
|
HDL-cholesterol (mmol/L), mean (SD) |
49 |
0.9 (0.2) |
1.0 (0.2) |
0.06 (0.01 to 0.12) |
|||||||||||
|
LDL-cholesterol (mmol/L), mean (SD) |
37 |
2.8 (0.9) |
2.5 (0.8) |
–0.28 (–0.47 to –0.08) |
|||||||||||
|
Cholesterol ratio, mean (SD) |
49 |
5.5 (1.4) |
5.0 (1.5) |
–0.46 (–0.87 to –0.05) |
|||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; HbA1c = glycated haemoglobin; HDL = high-density lipoprotein; IQR = interquartile range; LDL = low-density lipoprotein; SD = standard deviation. * Change reported as geometric mean ratio (ie, relative change in geometric mean). |
|||||||||||||||
Box 7 – Secondary outcomes (physical activity, dietary outcomes) for participants in the Hope for Health single arm, pre–post intervention study, northeast Arnhem Land, Northern Territory, 2022
|
Outcome |
Participants |
Baseline |
Program end |
Median change (95% CI) |
|||||||||||
|
|
|||||||||||||||
|
Physical activity |
|
|
|
|
|||||||||||
|
Walking (min/day), median (IQR) |
19 |
16.8 (10.5–27.1) |
117.2 (76.9–176.5) |
103.2 (74.4 to 135.8) |
|||||||||||
|
Moderate and vigorous physical activity* (min/day), median (IQR) |
19 |
20.6 (12.5–31.9) |
118.2 (77.1–179.3) |
102.7 (70.9 to 135.2) |
|||||||||||
|
Proportion of days walking at least 30 min, median (IQR) |
19 |
14.3% (0.0–50%) |
100% (100–100%) |
71.4 (51.2 to 87.5) percentage points |
|||||||||||
|
Days monitored, median (IQR) |
19 |
7.0 (6.0–8.0) |
7.0 (5.0–8.0) |
0.0 (–2.0 to 1.5) |
|||||||||||
|
Dietary intake (serves per day), median (IQR) |
|
|
|
|
|||||||||||
|
Vegetables |
45 |
1.0 (0.4–1.6) |
1.3 (0.8–1.9) |
0.2 (–0.1 to 0.5) |
|||||||||||
|
Fruit |
45 |
0.9 (0.3–1.3) |
0.9 (0.4–2.0) |
0.2 (–0.2 to 0.6) |
|||||||||||
|
Breads and cereals |
45 |
5.0 (3.0–7.0) |
3.0 (3.0–5.0) |
–1.5 (–2.0 to –1.0) |
|||||||||||
|
Meat |
45 |
3.1 (2.5–3.9) |
4.4 (3.6–5.2) |
1.1 (0.7 to 1.4) |
|||||||||||
|
Dairy |
45 |
1.4 (0.9–2.1) |
1.1 (1.1–1.4) |
–0.2 (–0.6 to 0.1) |
|||||||||||
|
Discretionary food |
45 |
5.0 (3.5–6.5) |
5.0 (3.5–8.5) |
0.3 (–0.8 to 1.3) |
|||||||||||
|
Sugar-sweetened beverages |
45 |
0.6 (0.1–3.0) |
0.4 (0.1–1.0) |
–0.6 (–1.4 to –0.1) |
|||||||||||
|
Weekly traditional food consumption† |
45 |
4.0 (4.0–6.0) |
4.0 (2.0–4.0) |
–1.0 (–2.0 to 0.0) |
|||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; IQR = interquartile range. * Including walking and more intense activity. † Measured as weekly frequency of intake: never = 0; less than once per week = 2; once or twice per week = 4; 3 or 4 times per week = 6; 5 or 6 times per week = 8; every day = 10. |
|||||||||||||||
Received 16 October 2023, accepted 6 August 2024
- Hasthi UW Dissanayake1
- George Gurruwiwi1
- J Dhurrkay1
- Josh C Tynan1
- Sabine Braat1,2
- Benjamin Harrap3
- Tim Trudgen4
- Sarah Hanieh1
- Bronwyn Clark5
- Michaela Spencer6
- Michael Christie7
- Emma Tonkin8
- Emily Armstrong6
- Leonard C Harrison9
- John M Wentworth9
- Julie K Brimblecombe10
- Beverley‐Ann Biggs1,11
- 1 Peter Doherty Institute for Infection and Immunity, University of Melbourne, Melbourne, VIC
- 2 Centre for Epidemiology and Biostatistics, Melbourne School of Population and Global Health, University of Melbourne, Melbourne, VIC
- 3 Yardhura Walani, Australian National University, Canberra, ACT
- 4 Hope for Health (Why Warriors Pty Ltd), Nhulunbuy, NT
- 5 The University of Queensland, Brisbane, QLD
- 6 Northern Institute, Charles Darwin University, Darwin, NT
- 7 Charles Darwin University, Darwin, NT
- 8 Monash University, Melbourne, VIC
- 9 Walter and Eliza Hall Institute of Medical Research, Melbourne, VIC
- 10 Menzies School of Health Research, Darwin, NT
- 11 Victorian Infectious Diseases Service, Melbourne, VIC
Open access:
Open access publishing facilitated by the University of Melbourne, as part of the Wiley – the University of Melbourne agreement via the Council of Australian University Librarians.
Data Sharing:
Correspondence regarding data sharing should be directed to Hasthi Dissanayake (
This study was supported by a National Health and Medical Research Council Targeted Research grant (APP1179067). The educational videos were funded by an Agility grant from the Peter Doherty Institute for Infection and Immunity.
Tim Trudgen is employed by Why Warriors Org Ltd (Hope for Health). The late Joanne Dhurrkay was a founding Hope for Health steering committee member (voluntary).
- 1. Jackson LR, Ward JE. Aboriginal health: why is reconciliation necessary? Med J Aust 1999; 170: 437‐440. https://www.mja.com.au/journal/1999/170/9/aboriginal‐health‐why‐reconciliation‐necessary
- 2. Australian Institute of Health and Welfare. Aboriginal and Torres Strait Islander health performance framework: summary report (here: sections 1.05, 1.09). Updated 7 Aug 2024. https://www.indigenoushpf.gov.au/report‐overview/overview/summary‐report (viewed Aug 2024).
- 3. Australian Institute of Health and Welfare. Life expectancy and potentially avoidable deaths in 2015–2017 (here: data tables). Updated 2 Aug 2019. https://www.aihw.gov.au/reports/life‐expectancy‐deaths/life‐expectancy‐avoidable‐deaths‐2015‐2017/contents/summary (viewed Aug 2024).
- 4. Australian Human Rights Commission. Close the Gap: Indigenous health campaign. 17 Mar 2022. https://humanrights.gov.au/our‐work/aboriginal‐and‐torres‐strait‐islander‐social‐justice/projects/close‐gap‐indigenous‐health (viewed Aug 2024).
- 5. Strate K, Brimblecombe J, Maple‐Brown L, et al. Chronic condition risk factor change over time in a remote Indigenous community. Rural Remote Health 2020; 20: 4452.
- 6. Rippe JM. Lifestyle strategies for risk factor reduction, prevention, and treatment of cardiovascular disease. Am J Lifestyle Med 2019; 13: 204‐212.
- 7. Thomas SA, Browning CJ, Charchar FJ, et al. Transforming global approaches to chronic disease prevention and management across the lifespan: integrating genomics, behavior change, and digital health solutions. Front Public Health 2023; 11: 1248254.
- 8. Why Warriors Org Ltd. What is the Hope For Health program? https://hopeforhealth.com.au/whatwedo (viewed Mar 2024).
- 9. Why Warriors Org Ltd. Pilot Yolngu “on‐country” health retreat and coaching program (2016). 2024. https://hopeforhealth.com.au/our‐full‐story/impact (viewed Mar 2024).
- 10. Wolfer TA, Wilson BL. Seeking champions for change: a positive deviance approach for social work. Fam Soc 2019; 100: 151‐163.
- 11. Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother 2010; 1: 100‐107.
- 12. Why Warriors Org Ltd. Governance strategic management committee. 2024. https://hopeforhealth.com.au/our‐full‐story/governance (viewed Mar 2024).
- 13. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap): a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377‐381.
- 14. Kompaniyets L, Freedman DS, Belay B, et al. Probability of 5% or greater weight loss or BMI reduction to healthy weight among adults with overweight or obesity. JAMA Netw Open 2023; 6: e2327358.
- 15. Rohit A, Brimblecombe J, O'Dea K, et al. Development of a short‐item diet quality questionnaire for Indigenous mothers and their young children: the Menzies remote short‐item dietary assessment tool. Aust J Rural Health 2018; 26: 220‐224.
- 16. Ahmadi MN, Nathan N, Sutherland R, et al. Non‐wear or sleep? Evaluation of five non‐wear detection algorithms for raw accelerometer data. J Sports Sci 2020; 38: 399‐404.
- 17. Pavey TG, Gilson ND, Gomersall SR, et al. Field evaluation of a random forest activity classifier for wrist‐worn accelerometer data. J Sci Med Sport 2017; 20: 75‐80.
- 18. Ḻäwurrpa E, Garŋgulkpuy J. Methodology for Yolŋu research [draft document]. Charles Darwin University, 19 Apr 2005. https://digitalcollections.cdu.edu.au/nodes/view/7871 (viewed Aug 2024).
- 19. Zhang W, Liu Y, Sun B, et al. Improved HbA1c and reduced glycaemic variability after 1‐year intermittent use of flash glucose monitoring. Sci Rep 2021; 11: 23950.
- 20. National Health and Medical Research Council. Ethical conduct in research with Aboriginal and Torres Strait Islander Peoples and communities (IND2). Aug 2018. https://www.nhmrc.gov.au/about‐us/resources/ethical‐conduct‐research‐aboriginal‐and‐torres‐strait‐islander‐peoples‐and‐communities (viewed Aug 2024).
- 21. Living Evidence for Diabetes Consortium. Australian evidence‐based clinical guidelines for diabetes. Nov 2020. https://www.diabetessociety.com.au/20211104%20Guideline‐Australian‐Evidence‐Based‐Clinical‐Guidelines‐for‐Diabetes.pdf (viewed Aug 2024).
- 22. Jensen MD, Ryan DH, Apovian CM, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American heart association task force on practice guidelines and the obesity society. Circulation 2014; 129 (Suppl 2): S102‐S138.
- 23. Canoy D, Nazarzadeh M, Copland E, et al. How much lowering of blood pressure is required to prevent cardiovascular disease in patients with and without previous cardiovascular disease? Curr Cardiol Rep 2022; 24: 851‐860.
- 24. Gwynn J, Sim K, Searle T, et al. Effect of nutrition interventions on diet‐related and health outcomes of Aboriginal and Torres Strait Islander Australians: a systematic review. BMJ Open 2019; 9: e025291.
- 25. Egger G, Fisher G, Piers S, et al. Abdominal obesity reduction in indigenous men. Int J Obes Relat Metab Disord 1999; 23: 564‐569.
- 26. Quinn E, O'Hara BJ, Ahmed N, et al. Enhancing the get healthy information and coaching service for Aboriginal adults: evaluation of the process and impact of the program. Int J Equity Health 2017; 16: 168.
- 27. Cargo M, Marks E, Brimblecombe J, et al. Integrating an ecological approach into an Aboriginal community‐based chronic disease prevention program: a longitudinal process evaluation. BMC Public Health 2011; 11: 299.
- 28. Cass A, Lowell A, Christie M, et al. Sharing the true stories: improving communication between Aboriginal patients and healthcare workers. Med J Aust 2002; 176: 466‐470. https://www.mja.com.au/journal/2002/176/10/sharing‐true‐stories‐improving‐communication‐between‐aboriginal‐patients‐and
- 29. Bussey C. Food security and traditional foods in remote Aboriginal communities: a review of the literature. Australian Indigenous Health Bulletin 2013; 13: 2. https://healthbulletin.org.au/articles/food‐security‐and‐traditional‐foods‐in‐remote‐aboriginal‐communities‐a‐review‐of‐the‐literature (viewed Aug 2024).
- 30. Wan Y, Tobias DK, Dennis KK, et al. Association between changes in carbohydrate intake and long term weight changes: prospective cohort study. BMJ 2023; 382: e073939.
- 31. Blodgett JM, Ahmadi MN, Atkin AJ, et al; ProPASS Collaboration. Device‐measured physical activity and cardiometabolic health: the prospective physical activity, sitting, and sleep (ProPASS) consortium. Eur Heart J 2024; 45: 458‐471.
- 32. Marley JV, Kitaura T, Atkinson D, et al. Clinical trials in a remote Aboriginal setting: lessons from the BOABS smoking cessation study. BMC Public Health 2014; 14: 579.






Abstract
Objective: To evaluate the impact of a 4‐month dietary and lifestyle program co‐designed and led by Aboriginal and Torres Strait Islander people on weight and metabolic markers, diet, and physical activity in overweight and obese adults in a remote Indigenous community.
Study design: Single arm, pre–post intervention study.
Setting, participants: Adult residents (18–65 years) of a remote Northern Territory community with body mass index (BMI) values of at least 25 kg/m2 or waist circumferences exceeding 94 cm (men) or 80 cm (women).
Intervention: Hope for Health, a culturally sensitive 4‐month program supporting self‐managed health improvement based on dietary and lifestyle change, 1 August to 30 November 2022.
Main outcome measures: Weight loss of at least 5%; changes in BMI, waist circumference, other metabolic markers (blood pressure, biomarkers of metabolic health and inflammation), diet, and physical activity; participant perceptions of the program.
Results: We assessed outcomes for 55 participants who completed weight assessments at both baseline and program end (mean age, 42.5 years [standard deviation, 10.1 years]; 36 women [65%]). Forty participants lost and 15 gained weight; overall mean weight loss was 1.5 kg (95% confidence interval [CI], 0.5–2.4 kg), and ten participants (18%; 95% CI, 9–31%) achieved at least 5% weight reduction. The mean change in BMI (53 participants) was –0.60 kg/m2 (95% CI, –0.93 to –0.27 kg/m2), in waist circumference (53 participants) –3.2 cm (95% CI, –4.7 to –1.7 cm), and in low‐density lipoprotein cholesterol level (37 participants) –0.28 mmol/L (95% CI, –0.47 to –0.08 mmol/L); the relative decline in the HbA1c level geometric mean (50 participants) was 11% (95% CI, 6–15%). The intake of breads and cereals (median change, –1.5 [95% CI, –2.0 to –1.0] serves/day) and sugar‐sweetened beverages (–0.6 [95% CI, –1.4 to –0.1] serves/day) declined; the amount of moderate and vigorous physical activity increased by a median of 103 min/day (95% CI, 74–136 min/day; 19 participants). The program focus on integrating healthy bodies and networks of kin, healthy governance, vibrant language and ceremony, and a healthy environment were seen as central to its value and benefit.
Conclusions: Community appreciation of the program and the improvements in cardiometabolic risk factors are encouraging, providing an example of a culturally sensitive, co‐designed initiative led by Indigenous people for reducing the prevalence of chronic disease in remote areas.
Trial registration: Australian New Zealand Clinical Trials Registry (ACTRN12622000174785; prospective: 2 February 2022).