The known: Life expectancy at birth is shorter in the Northern Territory than elsewhere in Australia, and the number of health workers per resident higher.
The new: When burden of disease and injury rather than population size is used as the benchmark, the Northern Territory health workforce is about 22% smaller than needed to match the national health workforce level.
The implications: The Northern Territory health workforce will face increasing pressure unless the number of health workers is increased to handle the high burden of illness, and to meet the health care requirements of Indigenous people.
Population health cannot be improved without an adequate, high quality health workforce.1 Health workforce needs are expected to increase substantially in Australia because of population growth and ageing, as well as changes in the epidemiology of disease and injury.2,3 Access to health services depends on the geographic distribution of the health workforce; in Australia, it is concentrated in major cities,4 and may therefore not reflect population health needs.5 These needs can be assessed as the burden of disease, measured in disability‐adjusted life‐years (DALYs),6 a summary statistic of mortality and morbidity that combines life years lost to premature deaths and disabilities caused by illness and injury.7
The Northern Territory includes 1% of the Australian population, but 18% of its area; 26% of NT people are Aboriginal or Torres Strait Islander (Indigenous) people, 75% of whom live in remote areas.8 About 3% of the national population are Indigenous Australians.8 The burden of disease for Indigenous people is higher in the NT than elsewhere in Australia, and their health outcomes are poorer; their life expectancy at birth is about 15 years shorter than for non‐Indigenous Territorians.9 Life expectancy at birth is lower in the NT than in all other states and territories.9,10
Australian governments recognise that improving Indigenous health in partnership with Aboriginal and Torres Strait Islander communities requires equity in needs‐based health workplace planning beyond matching its size to that of the population.11 Health workforce shortages and high turnover hamper health service delivery in remote areas of the NT.12 Greater efforts are needed to meet the health care needs of Indigenous people,13 and, to close Indigenous health gaps, health workforce planning must be evidence‐based.9 However, it is unknown whether the NT health workforce is adequate for dealing with the burden of disease in the NT.
We therefore assessed the adequacy of the NT health workforce with respect to both population size and burden of disease, overall and by selected health specialties, by comparing it with the national health workforce. We also investigated changes in workforce numbers to assess its sustainability. This study is part of the fourth NT burden of disease study (stage 3).14
Methods
We used burden of disease information to assess the size and skill mix of the health workforce, as recommended by the World Health Organization.15 We obtained health workforce data for Australia and the NT from the Australian Health Practitioner Regulation Agency (AHPRA) database using the Australian Department of Health and Aged Care Data Tool (https://hwd.health.gov.au/datatool). This tool can be used by government and non‐government organisations for monitoring and planning the health workforce, forecasting future workforce needs, and informing the education and supply of a qualified workforce. At the time of writing (July 2023), the database covered the period 1 January 2013 – 31 December 2021. We analysed health workforce data both overall and for 38 health professions; we included only people employed in their registered professions in Australia (as did the Australian Institute of Health and Welfare [AIHW] in their recent analysis4). Data for the paramedical health workforce were available only from 1 January 2019.
We calculated the size of the health workforce both as number of workers (person‐years) and as fulltime position equivalents (working hours as proportion of standard number of work hours4); if the number of fulltime equivalents is greater than the number of workers, it indicates that employees are working longer than standard work hours. Estimated resident populations for the NT and Australia were obtained from the Australian Bureau of Statistics website.8 The Aboriginal health practitioner workforce was assessed with reference to population and burden of disease data for the Indigenous population.7 All other professions were assessed using total population data and burden of disease data (DALYs) drawn from national and NT burden of disease studies.7,14,16,17 Because of its small population, we aggregated NT data for two five‐year periods, 2009–2013 and 2014–2018. The size of the health workforce for 2009–2013 was estimated from the 2013 data.
We assessed the adequacy of the overall NT health workforce by dividing the number of health practitioners by the total population number (health workers per 1000 population) or by total disease burden (health workers per 1000 DALYs). We respectively compared the NT values for 2009–2013 and 2014–2018 with Australian threshold values for 201317 and 20187 as ratios. For our primary analysis, sufficiency of supply was defined as the number of health workers per 1000 DALYs being at least as high for the NT as for Australia (ratio of one or more). For individual professions, results are reported as health workers per 100 000 population or 100 000 DALYs (overall burden of disease).
We estimated annual change in health workforce size from 2013 to 2021 (with respect to population or burden of disease) as the linear regression slope. NT burden of disease data were projected for 2019–2021, using linear extrapolation of the annual total DALYs because the relevant data have not yet been reported.14 An increase in number between 2013 and 2021 was deemed to indicate sustainability of supply, a decline non‐sustainability of supply.
Finally, we used differences between the NT and Australia in the number of health workers per 100 000 DALYs in 2014–2018 (the most recent available data) to estimate the current need for more health workers in each profession. For example: during 2013–2021 the mean number of nurses in the NT was 5866 per 100 000 DALYs, in Australia 6537 nurses per 100 000 DALYs; we multiplied the difference (0.00671 per DALY) by the annual health burden in the NT during 2014–2018 (the most recent data available; 69 209 DALYs), yielding the need for 464 additional nurses. The estimated mean numbers of health workers in the NT and Australia by profession during 2013–2021 are provided in the Supporting Information (table 1).
Ethics approval
The NT Department of Health and Menzies School of Health Research Human Research Ethics Committee approved this study (HREC 2020‐3860).
Results
For 2009–2013, the aggregate total of registered health workers in the NT was 27 135 person‐years, or 5427 health workers per year; the aggregate for 2014–2018 was 31 670 person‐years, or 6334 health workers per year. Similarly, the aggregate number of fulltime equivalents increased from 28 305 (5661 per year) during 2009–2013 to 32 416 (6483 per year) during 2014–2018 (Box 1). During both periods, the number of fulltime equivalents exceeded that of health workers, particularly for medical and paramedical professionals (data not shown).
Health worker numbers with respect to population and disease burden: overall
For both time periods, the NT health workforce comprised 1.1% of the national health workforce, a slightly larger proportion than its population proportion (1.0%), but smaller than its proportion of the national disease burden (1.4%). The number of health workers per 1000 population was slightly higher in the NT than for Australia (2009–2013 v 2013: 23.30 v 21.79 per 1000 population, 6.9% larger; 2014–2018 v 2018: 25.79 v 23.47 per 1000 population, 9.9% larger) (Box 1; Box 2).
During 2009–2013, there were 82.64 health workers per 1000 DALYs in the NT (23.1% fewer than the 2013 national level), and 91.52 per 1000 DALYs during 2014–2018 (21.8% fewer than the 2018 national level) (Box 1; Box 2).
The rises in the overall numbers of health workers and fulltime equivalents by population or disease burden between the two time periods were similar for the NT and Australia. The number of NT health workers per 1000 DALYs during 2014–2018 would need to increase by 28% to achieve the national level (ie, [117.08 – 91.52]/91.52) (Box 1).
Health worker numbers with respect to disease burden: by specialty
The number of health workers with respect to disease burden was lower in the NT than in Australia overall for 28 of 38 specialties; the differences were greatest for nurses and midwives (670.6 per 100 000 DALYs), physiotherapists (283.9 per 100 000 DALYs), psychologists (272.6 per 100 000 DALYs), pharmacists (219.6 per 100 000 DALYs), and dentists (207.7 per 100 000 DALYs) (Box 3). These figures indicate that 464 more nurses and midwives (11.4% more than the mean number for 2013–2021), 196 more physiotherapists (115%), 189 more psychologists (102%), 152 more pharmacists (79%), and 144 more dentists (106%) are needed to match the corresponding numbers of health workers per 100 000 DALYs for Australia (Box 4).
The annual increases in the numbers of health workers by disease burden were lower in the NT than in Australia overall for 20 of 38 specialties. The differences were greatest for Aboriginal health practitioners (difference between NT decrease and national increase: 30.8 per 100 000 DALYs per year), psychologists (15.6 per 100 000 DALYs per year), and paramedical health workers (11.6 per 100 000 DALYs per year) (Box 3).
Health workers with respect to population: by specialty
Absolute differences between the NT and Australia in the numbers of health workers relative to population were not as marked as for numbers with respect to disease burden. For example, the differences for general practitioners were 13.1 more per 100 000 population (Supporting Information, table 2) and 93.8 fewer per 100 000 DALYs in the NT (Box 3). The estimated required annual growth in the number of Aboriginal health practitioners based on population was 4.9% (11.0/223.5 per 100 000 population; Supporting Information, table 2); based on disease burden it was 7.4% (30.8/418.5 per 100 000 DALYs; Box 3).
Discussion
Our analysis indicates that the size of the NT health workforce, relative to its population size, was about 10% larger than the Australian health workforce during 2009–2018 (Box 1). This finding was consistent with those of a recent AIHW report4 and our earlier study18 that the number of health workers per NT resident is higher than for Australia. However, another AIHW report noted a severe shortage of health workers in rural and remote areas of Australia, including in the NT.19 Geographic maldistribution of the health workforce results in widespread mismatching of health services with health needs in remote and very remote areas, but population‐based assessments at the state or territory level do not detect local pockets of mismatch.19
Our analysis provides a clear reason for the number of health workers by population being larger in the NT than Australia overall: the greater burden of disease in the NT (41% more DALYs per person in 2014–2018 than for Australia in 2018). The number of health workers per 1000 DALYs, however, was about 22% lower in the NT than for Australia overall. That is, the population‐based assessment of the adequacy of the health workforce does not take into account differences between health needs in the NT and Australia. The population proportion of Indigenous people in the NT (26% in 2021) is larger than for Australia (3%),8 and the burden of disease was more than three times as high for Indigenous as for non‐Indigenous people in the NT during 2014–2018.14 The 22% shortfall in health workers with respect to disease burden places pressure on the NT health workforce; to achieve parity with the national level, its size needs to be increased by about 28%.
Our assessment of the adequacy of the health workforce with respect to burden of disease indicates that NT health services need 464 more nurses and midwives. This is alarming, as nurses and midwives comprise the largest single group of registered health professionals. There is both anecdotal and research evidence for large numbers of unfilled remote area nurse positions across the NT, resulting in overworked health workers, high staff turnover, and low patient satisfaction.12,20 Remote area nurses provide ambulance, emergency, acute, and chronic disease care that in urban centres is normally provided by general practitioners and ambulance paramedics. This broader scope of practice increases the need for nurses and midwives in remote and very remote areas, and partially explains the large nursing and midwifery workforce in the NT.
Our finding that the supply of health workers with respect to the burden of disease was also lower than the national level for most other specialties is consistent with the recent AIHW health workforce report that the five to ten locations with the greatest need for more workers in each professional category were in the NT.19 The undersupply with respect to burden of disease means that the number of health care staff treating diseases and injuries is insufficient.
The skills mix of the NT health workforce is also inadequate; for example, the numbers of physiotherapists and psychologists are not sufficient to meet health care needs. Our findings are consistent with previous reports on the health workforce in the NT, including shortages of remote area nurses and midwives,19,20 physiotherapists,21 psychologists,19,22 and Aboriginal health practitioners.23 The 51 fulltime equivalent dentistry positions per 100 000 NT people in 2022 was the lowest level in Australia.4 The corollary of the low numbers of specialists in the NT is the relatively high number of “other medical practitioners”, including junior clinicians. The fulltime equivalent numbers for many professions were higher than the number of specialists, indicating that health professionals often work longer than standard hours, probably reflecting understaffing relative to patient needs. Another possible explanation is that clinicians in other states devote a greater proportion of their time than NT clinicians to non‐clinical roles, such as research, teaching, and policy development.
Aboriginal health practitioners in the NT deserve special attention. The number of Aboriginal health practitioners relative to disease burden fell during the study period (Box 3), despite increases in the size of the Indigenous population.7,16 Further, remote primary care services rely on Aboriginal health practitioners as essential team members. Our findings indicate that this decline means that the size of the Aboriginal health practitioner workforce will become inadequate to meet demand. Community‐based Aboriginal health practitioners in the NT play important roles in collaborating with other health professionals to strengthen and deliver integrated primary care services in remote areas.
Our analysis is the first to use empirical burden of disease data to assess health workforce needs in Australia. The AIHW has recognised the limitations of the population density approach by incorporating Indigenous population, land size, and remoteness data as variables in its assessments of health needs.19 However, burden of disease is a more direct measure of health needs, and this approach is now seen by WHO as the standard for measuring population health needs.15
Limitations
Our analysis was largely based on the AHPRA National Health Workforce Dataset as provided by the Department of Health and Aged Care; the reliability of our findings depends on the data quality. The data were originally collected from state and territory professional registration boards and surveys managed by AHPRA covering only part of the health workforce; some details, such as locum arrangements, were not available in the dataset. Nevertheless, the AHPRA workforce dataset is the most accurate and complete available. Secondly, the 38 health profession categories did not cover all NT health specialities; for example, neither nephrologists nor geriatricians were separately listed, and general nurses were not distinguished from remote area nurses and midwives. The workforce assessments were based on overall burden of disease rather than specific disease categories. Profession‐specific analysis by disease burden in areas such as paediatric medicine, oncology, endocrinology, nephrology, and geriatric medicine, is planned for the next phase of this project, as is more detailed geographic analysis using NT Department of Health individual‐level data. Thirdly, national values were used as comparators for the assessment of workforce adequacy. This is not appropriate for some professions, including Aboriginal health practitioners, who largely work with Indigenous people in primary care clinics, so that the national value does not reflect need in the NT, where the proportion of Indigenous residents is large. The higher burden of disease among Indigenous people requires a larger number of Aboriginal health practitioners. Further, information on the age, sex and Indigenous composition of the workforce was not available, nor the impact of remoteness fully captured. Continuous, comprehensive monitoring of the workforce, including information on age, sex, Indigenous status, and location, is needed. Contributors to health care cost other than burden of disease were not considered by our analysis, but service delivery costs in the NT are higher than elsewhere in Australia because of its low population density, the remoteness of many communities, and the lack of economies of scale. We did not assess the impact of the coronavirus disease 2019 (COVID‐19) pandemic. Finally, estimating burden of disease depends more on data quality than population estimates; burden of disease data beyond 2018 are not yet available because of delays in reporting. Workforce data for the period 2009–2012 were estimates, as AHPRA data were not available.
Conclusion
Our analysis provides both overall and profession‐specific assessments that could inform future workforce planning in the NT. Health worker population density alone is insufficient for reliably assessing health workforce needs; burden of disease information is important for workforce planning that meets population health needs. Linking population and burden of disease with health workforce data provides stronger evidence for health workforce planning across health professions than conventional population‐based assessments. Burden of disease information should be used for health workforce planning at the national level, as it reflects the heterogeneity of needs by states and territory. We found that the size of the NT health workforce needs to be increased by about 28% to reflect the population level of disease and injury to achieve parity with the national level of health care workers. Shortages in the NT health workforce need to be eliminated to close health gaps between Indigenous and non‐Indigenous Australians.
Box 1 – Population, health workforce, and burden of disease, Northern Territory (2009–2018) and Australia (2013 and 2018)
|
|
Northern Territory |
Australia |
Ratio |
||||||||||||
|
Characteristic |
2009–2013 |
2014–2018 |
2013 |
2018 |
NT 2009–2013 v Australia 2013 |
NT 2014–2018 v Australia 2018 |
|||||||||
|
|
|||||||||||||||
|
Population |
|
|
|
|
|
|
|||||||||
|
All people |
232 947 |
245 568 |
23 128 129 |
24 982 688 |
0.010 |
0.010 |
|||||||||
|
Indigenous people |
68 215 |
73 906 |
698 583 |
778 064 |
0.098 |
0.095 |
|||||||||
|
Disability‐adjusted life‐years |
|
|
|
|
|
|
|||||||||
|
All people |
65 671 |
69 209 |
4 691 450 |
5 008 057 |
0.014 |
0.014 |
|||||||||
|
Indigenous people |
37 210 |
38 885 |
204 431 |
239 942 |
0.182 |
0.162 |
|||||||||
|
Disability‐adjusted life‐years per person |
|
|
|
|
|
|
|||||||||
|
All people |
0.282 |
0.282 |
0.203 |
0.200 |
1.390 |
1.406 |
|||||||||
|
Indigenous people |
0.545 |
0.526 |
0.293 |
0.308 |
1.864 |
1.706 |
|||||||||
|
Health workers* |
5427† |
6334 |
504 001 |
586 341 |
0.011 |
0.011 |
|||||||||
|
Health workers per 1000 population |
23.30 |
25.79 |
21.79 |
23.47 |
1.069 |
1.099 |
|||||||||
|
Health workers per 1000 disability‐adjusted life‐years |
82.64 |
91.52 |
107.43 |
117.08 |
0.769 |
0.782 |
|||||||||
|
Fulltime equivalents* |
5661† |
6483 |
470 699 |
536 394 |
0.012 |
0.012 |
|||||||||
|
Health workers per 1000 population |
24.30 |
26.40 |
20.35 |
21.47 |
1.194 |
1.230 |
|||||||||
|
Health workers per 1000 disability‐adjusted life‐years |
86.20 |
93.68 |
100.33 |
107.11 |
0.859 |
0.875 |
|||||||||
|
|
|||||||||||||||
|
* Mean annual number for the Northern Territory is reported. † Based on 2013 data, as workforce data were not available for 2009‐2012. |
|||||||||||||||
Box 2 – Comparison of the sizes of Northern Territory and Australian health workforces with respect to population size and burden of disease, 2009–2013 v 2013 and 2014–2018 v 2018*
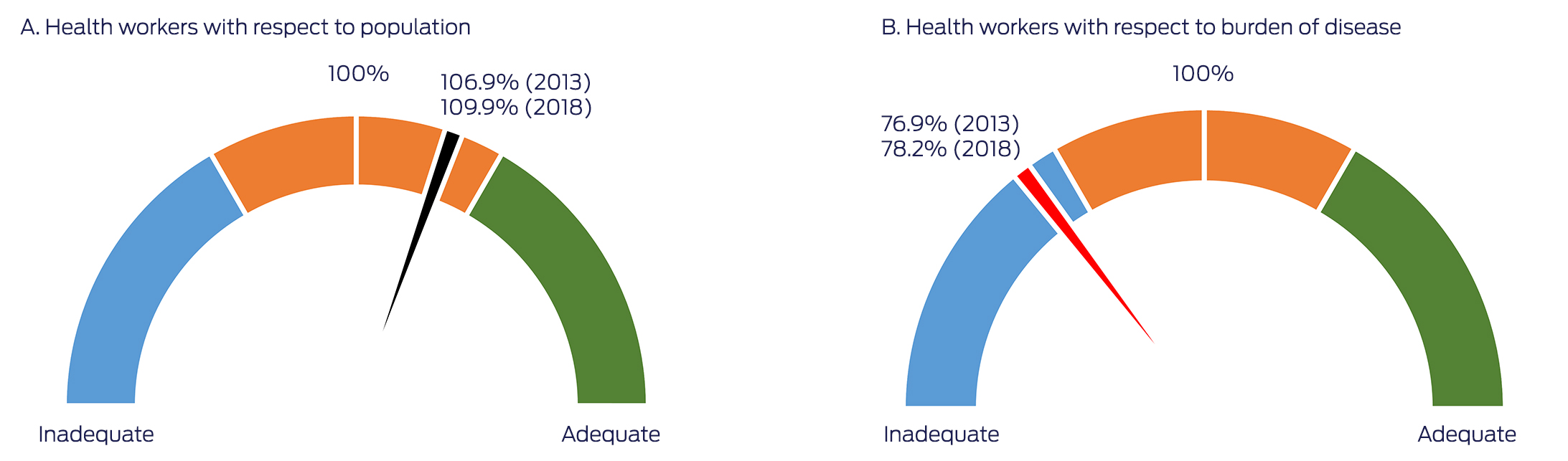
* That is: Northern Territory:Australia ratios for health workers per 1000 population and health workers per 1000 disability‐adjusted life‐years. The data for this figure are included in Box 1.
Box 3 – Size and annual change in size of the Northern Territory and Australian health workforces with respect to overall burden of disease, 2013–2021, by profession*
|
|
Health workers/100 000 DALYs |
Annual change in health workers/100 000 DALYs |
|||||||||||||
|
Profession |
Northern Territory |
Australia |
Difference |
Northern Territory |
Australia |
Difference |
|||||||||
|
|
|||||||||||||||
|
Nursing and midwifery |
5866.4 |
6537.0 |
–670.6 |
76.6 |
65.2 |
11.4 |
|||||||||
|
Other medical practitioners |
857.8 |
727.5 |
130.4 |
9.8 |
8.3 |
1.6 |
|||||||||
|
Aboriginal health practitioners† |
418.5 |
132.2 |
286.3 |
–11.9 |
18.9 |
–30.8 |
|||||||||
|
General practice |
396.3 |
490.1 |
–93.8 |
17.6 |
10.2 |
7.4 |
|||||||||
|
Pharmacy |
275.9 |
495.5 |
–219.6 |
5.7 |
6.0 |
–0.38 |
|||||||||
|
Psychology |
268.1 |
540.7 |
–272.6 |
–2.6 |
13.1 |
–15.6 |
|||||||||
|
Physiotherapy |
246.0 |
529.9 |
–283.9 |
8.4 |
19.3 |
–10.9 |
|||||||||
|
Occupational therapy |
235.5 |
354.9 |
–119.4 |
11.7 |
19.2 |
–7.4 |
|||||||||
|
Paramedicine‡ |
230.4 |
330.8 |
–100.4 |
4.0 |
15.6 |
–11.6 |
|||||||||
|
Dentistry |
196.3 |
404.0 |
–207.7 |
–0.92 |
3.7 |
–4.6 |
|||||||||
|
Medical radiation |
148.6 |
278.1 |
–129.5 |
4.7 |
5.7 |
–1.0 |
|||||||||
|
General medicine |
104.7 |
159.6 |
–54.9 |
5.6 |
4.8 |
0.80 |
|||||||||
|
Emergency medicine |
56.1 |
37.8 |
18.3 |
4.9 |
2.6 |
2.3 |
|||||||||
|
Surgery |
51.8 |
102.3 |
–50.5 |
–0.32 |
0.89 |
–1.2 |
|||||||||
|
Anaesthesia |
46.4 |
88.0 |
–41.6 |
1.6 |
1.5 |
0.11 |
|||||||||
|
Optometry |
46.2 |
99.0 |
–52.7 |
–0.32 |
2.0 |
–2.4 |
|||||||||
|
Paediatric and child health |
41.2 |
40.6 |
0.5 |
1.5 |
1.7 |
–0.1 |
|||||||||
|
Podiatry |
32.7 |
91.1 |
–58.3 |
1.0 |
2.4 |
–1.3 |
|||||||||
|
Psychiatry |
31.9 |
70.0 |
–38.1 |
1.6 |
1.2 |
0.39 |
|||||||||
|
Chiropractic |
31.8 |
95.0 |
–63.2 |
–0.61 |
1.02 |
–1.6 |
|||||||||
|
Obstetrics and gynaecology |
26.2 |
35.8 |
–9.6 |
0.33 |
0.32 |
0.02 |
|||||||||
|
Public health medicine |
20.8 |
4.9 |
15.9 |
–1.4 |
–0.03 |
–1.41 |
|||||||||
|
Chinese medicine |
16.4 |
79.8 |
–63.4 |
–0.54 |
–0.55 |
0.01 |
|||||||||
|
Intensive care medicine |
14.3 |
13.5 |
0.8 |
0.56 |
0.46 |
0.11 |
|||||||||
|
Pathology |
11.0 |
27.9 |
–16.9 |
0.16 |
–0.01 |
0.18 |
|||||||||
|
Ophthalmology |
7.6 |
18.7 |
–11.1 |
0.54 |
0.05 |
0.50 |
|||||||||
|
Radiology |
7.6 |
41.5 |
–33.8 |
–0.05 |
0.81 |
–0.86 |
|||||||||
|
Medical administration |
4.6 |
4.4 |
0.2 |
–0.50 |
–0.05 |
–0.45 |
|||||||||
|
Palliative medicine |
4.6 |
5.0 |
–0.4 |
0.15 |
0.26 |
–0.10 |
|||||||||
|
Rehabilitation medicine |
4.3 |
8.7 |
–4.4 |
–0.04 |
0.22 |
–0.27 |
|||||||||
|
Osteopathy |
3.7 |
42.8 |
–39.1 |
1.0 |
2.0 |
–1.0 |
|||||||||
|
Addiction medicine |
2.5 |
2.1 |
0.4 |
0.30 |
0.01 |
0.29 |
|||||||||
|
Radiation oncology |
2.4 |
7.1 |
–4.7 |
0.26 |
0.11 |
0.16 |
|||||||||
|
Sport and exercise medicine |
2.4 |
2.3 |
0.1 |
0.18 |
0.05 |
0.13 |
|||||||||
|
Dermatology |
1.9 |
10.2 |
–8.3 |
–0.30 |
0.18 |
–0.48 |
|||||||||
|
Occupational and environmental medicine |
1.9 |
4.8 |
–2.9 |
0.06 |
–0.08 |
0.13 |
|||||||||
|
Sexual health medicine |
1.9 |
1.8 |
0.1 |
0.19 |
0.01 |
0.17 |
|||||||||
|
Pain medicine |
0.5 |
2.9 |
–2.4 |
0.27 |
0.18 |
0.09 |
|||||||||
|
|
|||||||||||||||
|
DALY = disability‐adjusted life‐year. * Sources: references 4,7,14,16,17. † Based on burden of disease among Aboriginal and Torres Strait Islander people. ‡ Data available only for 2019–2021. |
|||||||||||||||
Box 4 – Number of additional health workers needed for the Northern Territory health workforce to match number with respect to burden of disease for the Australian health workforce, 2013–2021, by specialty*
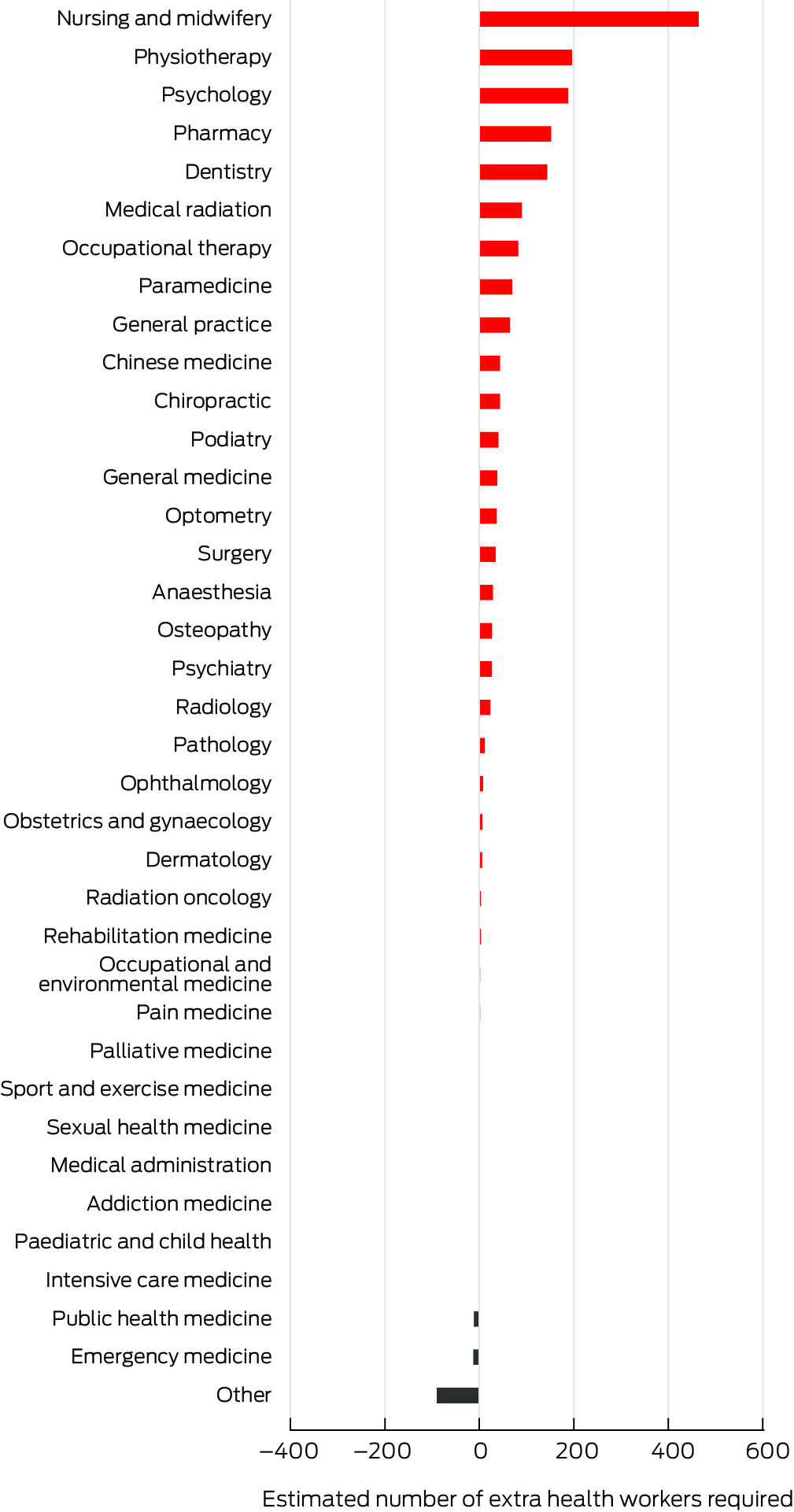
* Aboriginal health practitioners data not shown because Northern Territory and Australian numbers are not comparable.
Received 28 September 2023, accepted 28 March 2024
- Yuejen Zhao1
- Jo Wright1
- Renu Unnikrishnan1
- Ramakrishna Chondur1
- Danielle Green1
- Northern Territory Department of Health, Darwin, NT
Data Sharing:
The data underlying this report will not be available for sharing. Australian health workforce data, including for the Northern Territory, are available from the Australian Department of Health and Aged Care (https://hwd.health.gov.au/datatool).
We thank the staff in the births, deaths and marriages registries, cancer registers, notifiable diseases registers, remote clinics, and public hospitals in the Northern Territory and across Australia for their dedication to burden of disease and injury data collection. Parts of this report were published in an NT Department of Health report (https://hdl.handle.net/10137/13550).
No relevant disclosures.
- 1. Global Health Workforce Alliance (World Health Organization). A universal truth: no health without a workforce. 8 Nov 2014. https://www.who.int/publications/m/item/hrh_universal_truth (viewed Dec 2023).
- 2. Australian Department of Health and Aged Care. National medical workforce strategy 2021–2031. Updated 18 June 2024. https://www.health.gov.au/our‐work/national‐medical‐workforce‐strategy‐2021‐2031 (viewed July 2024).
- 3. Castillo‐Laborde C. Human resources for health and burden of disease: an econometric approach. Hum Resour Health 2011; 9: 4.
- 4. Australian Institute of Health and Welfare. Health workforce. Updated 7 July 2022. https://www.aihw.gov.au/reports/workforce/health‐workforce (viewed Dec 2023).
- 5. GBD 2019 Human Resources for Health Collaborators. Measuring the availability of human resources for health and its relationship to universal health coverage for 204 countries and territories from 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2022; 399: 2129‐2154.
- 6. Murray CJL, Lopez AD, Mathers CD. Assessing health needs: the global burden of disease approach. In: Detels R, Beaglehole R, Lansang MA, Gulliford M, editors. Oxford textbook of public health, 5th edition. London: Oxford University Press, 2009; pp. 256–272.
- 7. Australian Institute of Health and Welfare. Australian burden of disease study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018. 10 Mar 2022. https://www.aihw.gov.au/reports/burden‐of‐disease/illness‐death‐indigenous‐2018/summary (viewed Mar 2024).
- 8. Australian Bureau of Statistics. Census of population and housing: counts of Aboriginal and Torres Strait Islander Australians, 2021. 31 Aug 2022. https://www.abs.gov.au/statistics/people/aboriginal‐and‐torres‐strait‐islander‐peoples/census‐population‐and‐housing‐counts‐aboriginal‐and‐torres‐strait‐islander‐australians/2021 (viewed Sept 2024).
- 9. Zhao Y, Li SQ, Wilson T, Burgess CP. Improved life expectancy for Indigenous and non‐Indigenous people in the Northern Territory, 1999–2018: overall and by underlying cause of death. Med J Aust 2022; 217: 30‐35. https://www.mja.com.au/journal/2022/217/1/improved‐life‐expectancy‐indigenous‐and‐non‐indigenous‐people‐northern‐territory
- 10. Australian Bureau of Statistics. Life expectancy: statistics about life tables and life expectancy at birth estimates for Australia, states and territories and sub‐state regions, 2020–2022. 8 Nov 2023. https://www.abs.gov.au/statistics/people/population/life‐expectancy/latest‐release (viewed Sept 2024).
- 11. Australian Government. National agreement on closing the gap. July 2020. https://www.closingthegap.gov.au/sites/default/files/2022‐09/ctg‐national‐agreement_apr‐21‐comm‐infra‐targets‐updated‐24‐august‐2022_0.pdf (viewed Mar 2024).
- 12. Russell DJ, Zhao Y, Guthridge S, et al. Patterns of resident health workforce turnover and retention in remote communities of the Northern Territory of Australia, 2013–2015. Hum Resour Health 2017; 15: 52.
- 13. Jongen C, McCalman J, Campbell S, Fagan R. Working well: strategies to strengthen the workforce of the Indigenous primary healthcare sector. BMC Health Serv Res 2019; 19: 910.
- 14. Zhao Y, Unnikrishnan R, Chondur R, Burgess P. Morbidity burden of disease and injury in the Northern Territory 2014–2018. 14 Aug 2023. https://health.nt.gov.au/__data/assets/pdf_file/0011/1267184/morbidity‐burden‐of‐disease‐and‐injury‐in‐the‐northern‐territory‐2014‐2018.pdf (viewed Mar 2024).
- 15. World Health Organization. Health workforce requirements for universal health coverage and the sustainable development goals [Human Resources for Health Observer, 17)]. 2016. https://iris.who.int/handle/10665/250330 (viewed Mar 2024).
- 16. Zhang X, Zhao Y, Guthridge S. Burden of disease and injury study: impact and causes of illness, injury and death in the Northern Territory, 2004–2013. 26 Sept 2018. https://digitallibrary.health.nt.gov.au/entities/publication/c54ec423‐a68b‐4128‐a2cc‐a2c06eb69180/details (viewed Mar 2024).
- 17. Australian Institute of Health and Welfare. Australian burden of disease study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011 [Cat no. BOD 7]. 23 Sept 2016. https://www.aihw.gov.au/reports/burden‐of‐disease/illness‐death‐indigenous‐australians/summary (viewed Mar 2024).
- 18. Malyon R, Zhao Y, Guthridge S. Health workforce modelling, Northern Territory, 2006–2022. Darwin: Northern Territory Department of Health and Families, 2010. https://digitallibrary.health.nt.gov.au/prodjspui/handle/10137/442 (viewed Mar 2024).
- 19. Australian Institute of Health and Welfare. Spatial distribution of the supply of the clinical health workforce 2014: relationship to the distribution of the Indigenous population. 28 Nov 2016. https://www.aihw.gov.au/reports/indigenous‐australians/spatial‐distribution‐of‐the‐supply‐of‐the‐clinical/summary (viewed Mar 2024).
- 20. Zhao Y, Russell DJ, Guthridge S, et al. Long‐term trends in supply and sustainability of the health workforce in remote Aboriginal communities in the Northern Territory of Australia. BMC Health Serv Res 2017; 17: 836.
- 21. Sheppard L. Work practices of rural and remote physiotherapists. Aust J Rural Health 2001; 9: 85‐91.
- 22. Castle P. Practice learnings from the Psychologist Integration into Primary Health Care Pilot Program on the Tiwi Islands, Northern Territory. Aust Psychol 2021; 56: 137‐141.
- 23. Bailey J, Blignault I, Carriage C, et al. Career pathways for the Aboriginal and Torres Strait Islander health workforce: secondary data workforce report. Melbourne: Lowitja Institute, 2020. https://www.lowitja.org.au/wp‐content/uploads/migrate/CPP%20Secondary%20Data%20Report_Final_July%202020(1).pdf (viewed Mar 2024).





Abstract
Objectives: To assess the adequacy of the Northern Territory health workforce with respect to population size and burden of disease, overall and by selected health specialties; to assess its sustainability by investigating changes in workforce numbers.
Study design: Analysis of Australian Health Practitioner Regulation Agency (AHPRA) health workforce data (2013–2021) and burden of disease data (disability‐adjusted life‐years, DALYs) drawn from national and NT burden of disease studies (and projected for 2019–2021).
Setting, participants: NT and Australian health workforces, 2009–2021.
Main outcome measures: Adequacy of the NT health workforce, assessed as the ratio of the mean annual numbers of NT health workers per 1000 population or health workers per 1000 DALYs (2009–2013 and 2014–2018) to those of the Australian workforce (2013 and 2018); sustainability of the NT health workforce, defined as the number of health workers per 1000 population or per 1000 DALYs increasing between 2013 and 2021.
Results: The number of health workers per 1000 population was slightly higher in the NT than for Australia in both time periods (2009–2013v 2013: 23.30 v 21.79 per 1000 population, 6.9% larger; 2014–2018 v 2018: 25.79 v 23.47 per 1000 population, 9.9% larger); however, it was smaller with respect to burden of disease (2009–2013 v 2013: 82.6 v 107.4 health workers per 1000 DALYs, 23.1% fewer; 2014–2018 v 2018: 91.5 v 117.1 per 1000 DALYs, 21.8% fewer). In particular, 464 more nurses and midwives (11.4% more than the mean for 2013–2021), 196 more physiotherapists (115%), 189 more psychologists (102%), 152 more pharmacists (79%), and 144 more dentists (106%) are needed in the NT to match the corresponding numbers of health workers by disease burden for Australia as a whole. The number of Aboriginal health practitioners per 100 000 DALYs fell during the study period.
Conclusion: Health worker population density alone does not reliably assess health workforce needs; burden of disease information is important for workforce planning that meets population health needs. The NT health workforce needs to be increased by about 28% to reflect the population burden of disease and injury. Shortages in the NT health workforce must be eliminated to close health gaps between Indigenous and non‐Indigenous Australians.