The known: Survival after hip fracture has improved in Australia in recent years. It is unknown whether the national hip fracture care clinical care standard has contributed to this improvement.
The new: Clinical care for two‐thirds of hip fractures in people who underwent surgery in New South Wales during 2015–2018 adhered to at least five of six acute care quality indicators; significantly lower short and longer term mortality were associated with such care.
The implications: Quality hip fracture care is associated with improved survival. However, as care for one‐third of fractures did not achieve high level adherence to quality care, the delivery of hip fracture care must be further improved.
Hip fractures, most of which are caused by falls, are devastating for older people. They are associated with substantial morbidity and mortality, reduced quality of life, and loss of independence; 25% of people die within twelve months of hip fractures, 50% do not regain their previous level of function, and for 11% the fracture leads to admission to residential care.1,2 It was estimated that there would be one hip fracture in Australia every 16.2 minutes in 2022,3 a substantial increase from one in every 33.5 minutes in 2002.4 The increase largely comprises fractures in people aged 85 years or older and among those living with dementia,5,6 adding to the complexity and cost of care.
Poor quality and coordination of care, including delayed surgery, delayed mobilisation, and not using an orthogeriatric model of care, have been associated with poor outcomes for people with hip fractures.7,8,9 In Australia, the aim of the Australian and New Zealand Hip Fracture Registry (ANZHFR; https://anzhfr.org) guideline for hip fracture care10 is to promote high quality care and reduce unnecessary variation in treatment. The guideline underpins the Australian Commission on Safety and Quality in Health Care (ACSQHC) hip fracture clinical care standard, introduced in 2016.11 ANZHFR has collected and reported data on a set of quality indicators that have been used to measure adherence to the standard since 2016. The introduction of evidence‐based clinical care standards has been associated with lower mortality in the United Kingdom12,13,14 and Norway.15 A recent study in New South Wales found that 30‐day mortality among people who underwent surgery after hip fracture declined by 3.0% per year and 12‐month mortality by 2.3% per year during 2011–2018.16 However, the contributions of the introduction of guidelines, standards, and ANZHFR to these declines is unclear.
The aim of our study was to determine whether adherence to clinical care quality indicators influences mortality among people who undergo surgery after hip fracture in New South Wales, both overall and for individual indicators.
Methods
For our retrospective, population‐based study, we analysed linked ANZHFR, hospital admissions, residential aged care facilities, and deaths data. We included data for all people aged 50 years or older who underwent hip fracture surgery in a participating NSW hospital during 1 January 2015 – 31 December 2018. The ANZHFR is a clinical quality registry that includes data from 21 New South Wales hospitals for the time period we examined. The registry includes patient‐level data on demographic characteristics and care received, including comparison with the ACSQHC quality care indicators. ANZFHR data were linked to the NSW Admitted Patient Data Collection, which records data for all hospitalisations in NSW public and private hospitals, including demographic information for patients, diagnosis codes, and procedures; the Registry of Births, Death and Marriages mortality database, which includes records for all deaths of NSW residents; and the National Aged Care Data Clearing House, which records the dates of entry to and departure from residential aged care facilities, enabling determination of residential aged care status at time of fracture. Linkage of registry and hospital and mortality data was undertaken by the Centre for Health Record Linkage (CHeReL); linkage to residential aged care was undertaken by the Australian Institute of Health and Welfare Data Linkage Unit. We report the study in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.17
Clinical indicators
The ACSQHC hip fracture care clinical care standard comprises seven quality statements supported by 16 quality indicators.11 Eight quality indicators are specifically related to the provision of acute care at the patient level; the six indicators for which the registry consistently collected data during the study period were included in our analysis (Box 1). Data for two acute care indicators — assessment of cognitive status prior to surgery; pain assessment within 30 minutes of emergency department presentation and provision of analgesia within this time if required — were only routinely collected from 2017, and were therefore not included in the analysis. Level of adherence to the indicators was classified as low (three or fewer indicators attained), moderate (four indicators attained), or high (five or six indicators attained), an approach that ensures reasonable proportions based on the frequency distribution of all patients.12
Outcomes and covariates
The primary outcome was 30‐day all‐cause mortality; secondary outcomes were 120‐day and 365‐day all‐cause mortality. Patient‐level factors that influence mortality included as covariates were age, sex, comorbidity, pre‐fracture mobility, residential aged care facility status, and year of admission. Comorbidity was determined from linked hospital records using the Charlson Comorbidity Index with a 12‐month lookback period, a good predictor of 30‐day mortality among people with hip fractures.18 The weighted Charlson Comorbidity Index score was classified as indicating no comorbidity (0), mild comorbidity (1 or 2), or severe comorbidity (3 or more). Pre‐fracture mobility was identified in ANZHFR data, and classified as walking without aids, walking with a stick or crutch, walking with two aids or a frame, or as being wheelchair‐ or bed‐bound. Pre‐admission residential aged care status was determined from residential aged care data.
Statistical analysis
We summarise demographic characteristics, both overall and by level of quality indicator attainment, as means with standard deviations (SDs) for normally distributed continuous variables and as numbers and proportions for categorical variables. Associations between indicator attainment and short and longer term mortality were assessed in modified multivariable Poisson regression analyses, adjusted for age, sex, comorbidity, mobility, residential aged care status, and admission year; we report adjusted relative risks (aRRs) with 95% confidence intervals (CIs). To ensure complete capture of mortality outcomes, data for people admitted to hospital after 30 November 2018 were excluded from the 30‐day mortality analysis, after 31 August 2018 from the 120‐day mortality analysis, and after 31 December 2017 from the 365‐day mortality analysis. Only fractures for which complete indicator adherence data were available were included in the primary analysis. In a sensitivity analysis that included data for all hip fractures, indicator attainment was classified as “yes” if the indicator was attained or “no” if it was not attained or the outcome was not documented or was unknown. All analyses were performed in SAS Enterprise Guide 8.4.
Ethics approval
The study was approved by the NSW Population Health Service Research Ethics Committee (2019/ETH01622) and the Australian Institute of Health and Welfare Ethics Committee (EO2018/1/401).
Results
Registry data were available for 9058 people aged 50 years or older who underwent hip fracture surgery in a participating NSW hospital during 2015–2018; as 89 people had more than one hip fracture, data for 9236 fractures were available. Mean age at hip fracture was 82.8 years (SD, 9.3 years); 5510 of 9058 patients were women (69.4%).
Complete data regarding adherence to clinical care standard indicators were available for 7951 fractures (86.1%) and were included in our analysis. Indicator attainment varied widely: 1476 people (18.6%) received bone protection medication at the time of discharge from hospital, 7615 attained unrestricted weight‐bearing status immediately after surgery (95.8%), and 7723 did not develop new pressure injuries in hospital (97.1%) (Box 1).
For 5135 hip fractures (64.6%), the indicator adherence level was high, for 2249 fractures (28.3%) moderate, and for 567 fractures (7.1%) low. There was no clear pattern of change over the study period in the number of indicators attained or level of attainment (Supporting Information, figure 1). The proportions of fractures in women, people without other medical conditions, and people who were living in the community at the time of the fracture were larger for fractures with high indicator adherence than for fractures with low or moderate adherence (Box 2).
Unadjusted mortality was lowest for high indicator adherence hip fractures and greatest for low indicator adherence fractures at 30 days (high adherence, 4.1%; moderate adherence, 6.8%; low adherence, 10.8%), 120 days (high adherence, 11.7%; moderate adherence, 16.3%; low adherence, 25.2%), and 365 days (high adherence, 20.2%; moderate adherence, 27.5%; low adherence, 36.3%) (Box 2). Thirty‐day mortality risk was lower for high (aRR, 0.40; 95% CI, 0.30–0.52) and moderate indicator adherence hip fractures (aRR, 0.61; 95% CI, 0.46–0.82) than for low indicator adherence hip fractures, as was 120‐day risk (high adherence: aRR, 0.49 [95% CI, 0.41–0.57]; moderate adherence: aRR, 0.62 [95% CI, 0.52–0.75]) and 365‐day risk (high adherence: aRR, 0.59 [95% CI, 0.51–0.68]; moderate adherence: aRR, 0.74 [95% CI, 0.63–0.86]). Orthogeriatric care (365 days: aRR, 0.78; 95% CI, 0.61–0.98) and offering mobilisation by the day after surgery (365 days: aRR, 0.74; 95% CI, 0.67–0.83) were associated with lower risk of mortality at each time point, as was surgery within 48 hours of presentation (365 days: aRR, 0.81; 95% CI, 0.73–0.90) (Box 3). The sensitivity analysis that included data for all fractures, regardless of the completeness of indicator adherence data, yielded similar results) (Supporting Information, table 1).
Discussion
We found that adherence to evidence‐informed clinical quality indicators has a significant survival benefit for people aged 50 years or older who undergo surgery after a hip fracture. Short term mortality risk was 60% lower when five or six of the quality indicators were achieved, and 40% lower when four indicators were met, highlighting the cumulative impact of a number of care processes in hip fracture care and the need for a multidisciplinary approach to high quality care.
Time to surgery has consistently been identified as an important determinant of survival for people with hip fracture,8 even after adjusting for delays related to comorbidity and acute illness. In Australia, the target has been surgery within 48 hours of presentation,11 but the revised ACSQHC standard now stipulates surgery within 36 hours,19 as also recommended in the United Kingdom, with evidence that this is associated with lower peri‐operative complication and mortality rates.8,20 Surgery was undertaken within 48 hours of presentation for more than 95% of high indicator adherence fractures in our study, but it was not for one‐quarter of all fractures. Access to operating theatres is among the problems that need to be overcome to ensure that older people with hip fractures do not wait in bed, in pain and fasting, for unacceptably long periods.
Orthogeriatric care is associated with better outcomes after hip fracture surgery, including lower mortality.9,21 In Australia, access to geriatricians is good in most hospitals that offer hip fracture surgery, but the model of care varies between hospitals, from shared care to intermittent review. Our findings included short and moderate term survival benefits of an orthogeriatric model of care (up to twelve months after surgery).
Similarly, early mobilisation is increasingly recognised as an important contributor to better outcomes after hip fracture surgery, including lower mortality22 and lower post‐surgery complication rates, including those of chest infection, thromboembolic disease, and pressure injuries.23 In our study, patients were offered mobilisation within one day of surgery for 86% of fractures (and after 97% of high indicator adherence fractures), but the mobilisation measure used during the study period did not record whether people were actually mobilised. ANZHFR data indicate that the availability of weekend physiotherapy is increasing and that hospital clinicians recognise the importance of encouraging people to leave bed early to maximise the likelihood of meaningful functional recovery, as well as potentially reducing the length of hospital stay.
Secondary fracture prevention was the most poorly achieved quality indicator. Providing patients with treatment for osteoporosis on discharge from acute care was recorded for only 29% of high indicator adherence fractures, and 20% of all fractures, despite strong evidence for the value of treating osteoporosis and reducing fracture risk, as well as some evidence for a survival benefit for people treated for osteoporosis after hip fracture.24,25 A recent ANZHFR sprint audit identified several reasons for this neglect of secondary fracture prevention, including patient‐related factors (low vitamin D levels, need for dental procedures) and the reluctance of hospitals to fund treatments for a condition deemed to be a chronic disease. In our study, bone protection therapy was associated with lower mortality at all time points, indicating the need for greater awareness of the survival benefits and importance of initiating timely treatment.
The large sample size in our population‐based study ensured that it was representative of all hip fractures in Australia, and that our findings are generalisable to other areas in Australia with similar demographic characteristics. Linkage of the registry data to hospital admissions and residential aged care data facilitated adjustment for comorbidity and accurate ascertainment of pre‐fracture residential status, each of which is an important risk factor for death after hip fracture surgery. Linkage to death registry data facilitated accurate ascertainment of longer term mortality (longer than 120 days) than data routinely collected by hip fracture registries. The lower mortality risk following fractures with high adherence to the acute care standards — 60% at 30 days and 50% at 120 days — was consistent with the improved survival associated with high adherence to national clinical care standards in England and Wales14 and Scotland,12 and adherence to the standard of surgery within 48 hour in Norway.15 Ours is the first study to report a survival benefit as long as one year after surgery was associated with adherence to clinical care standards that encompass a comprehensive approach to care.
While improving overall patient survival is important, assessments of health care should incorporate other measures meaningful to patients.26 Health‐related quality of life scores decline significantly after a hip fracture; they improve by 120 days, but remain lower than prior to the fracture.27,28 Encouragingly, a multicentre cohort study in twenty United Kingdom hospitals found that the cumulative attainment of several Best Practice Tariff indicators was associated with clinically relevant improvement in health‐related quality of life scores four months after hip fracture.13 Although EQ‐5D‐5L data (a standardised measure of health‐related quality of life) are collected by the ANZHFR, their reporting is not compulsory, and the available data are insufficient for robustly assessing the impact of attainment of care standards on health‐related quality of life.
Limitations
Some limitations are inherent to all analyses of registry and administrative data. To minimise the impact of the large proportion of missing data for some adherence measures, we excluded two acute care indicators for which data were not collected across the entire study period. Their exclusion was unlikely to influence our estimates of the influence of adherence to care standards on mortality, as they were not statistically associated with mortality during the two years for which data were available (2017, 2018) (data not shown). Further, we restricted our main analysis to fractures for which complete data were available for the six included indicators, excluding 14% of hip fractures. While this complete case approach could bias our analysis, the sensitivity analysis that included all fractures yielded similar results; further, the only misclassification bias in the sensitivity analysis attributable to missing data would affect the non‐adherence group and reduce the difference in outcomes between the two groups. We are therefore confident that the differences between the groups in our main analysis are robust and are generalisable to hip fractures in other Australian jurisdictions.
Identification of other medical conditions relied on the quality of International Statistical Classification of Disease and Related Health Problems, tenth revision, Australian modification (ICD‐10‐AM) coding in the data we analysed, which depends on clinicians accurately identifying and recording these conditions in medical records. Despite controlling for factors known to influence mortality, uncontrolled confounding remains possible, including by factors such as general improvements in hospital care for older people (eg, better recognition and treatment of delirium) and changes to the coding of medical conditions. However, we attempted to adjust our analyses for temporal changes. We analysed data only to 2018, in part a reflection of the difficulty of timely linkage of datasets in Australia, a problem that needs to be overcome to maximise the benefits of clinical quality registries.
Conclusion
We found that clinical care for almost two‐thirds of hip fractures attained a high level of adherence to acute care clinical indicators. High level adherence was associated with 60% lower short term mortality, and moderate level adherence with 40% lower mortality; survival benefits were also evident one year after hip fracture surgery. That care for one‐third of hip fractures did not achieve a high level of adherence to recommendations indicates that the delivery of hip fracture care needs to be improved, which could in turn improve health outcomes for people with hip fractures.
Box 1 – Attainment of clinical care standards, by ACSQHC hip fracture clinical care standard indicator, for 7951 hip fractures in people aged 50 years or older who underwent surgery in 21 New South Wales hospitals after hip fractures, 2015–2018 (complete case analysis)
|
|
Indicator attained |
||||||||||||||
|
Indicator 11 |
Yes |
No |
|||||||||||||
|
|
|||||||||||||||
|
Standard 3. Orthogeriatric model of care |
|
|
|||||||||||||
|
3a. Orthogeriatric (or alternative physician or medical practitioner) management |
7378 (92.8%) |
573 (7.2%) |
|||||||||||||
|
Standard 4. Timing of surgery |
|
|
|||||||||||||
|
4a. Surgery within 48 hours of presentation with hip fracture |
6034 (75.9%) |
1917 (24.1%) |
|||||||||||||
|
Standard 5. Mobilisation and weight bearing |
|
|
|||||||||||||
|
5a. Offered mobilisation by day after hip fracture surgery |
7039 (88.5%) |
912 (11.5%) |
|||||||||||||
|
5b. Unrestricted weight‐bearing status immediately after hip fracture surgery |
7615 (95.8%) |
336 (4.2%) |
|||||||||||||
|
5c. Did not experience a new pressure ulcer (stage II or higher) during hospital stay |
7723 (97.1%) |
228 (2.9%) |
|||||||||||||
|
Standard 6. Minimising risk of another fracture |
|
|
|||||||||||||
|
6a. Received bone protection medication prior to discharge from hospital at which they underwent surgery |
1476 (18.6%) |
6475 (81.4%) |
|||||||||||||
|
|
|||||||||||||||
|
ACSQHC = Australian Commission on Safety and Quality in Health Care. |
|||||||||||||||
Box 2 – Characteristics of people aged 50 years or older who underwent surgery in 21 New South Wales hospitals after hip fractures, 2015–2018 (7951 hip fractures: complete case analysis), by clinical care indicator adherence level
|
|
Clinical care indicator adherence level |
||||||||||||||
|
Characteristic |
Low |
Moderate |
High |
||||||||||||
|
|
|||||||||||||||
|
Number of hip fractures |
567 [7.1%] |
2249 [28.3%] |
5135 [64.6%] |
||||||||||||
|
Age group (years) |
|
|
|
||||||||||||
|
50–74 |
185 (33.5%) |
546 (24.9%) |
822 (16.4%) |
||||||||||||
|
75–84 |
154 (27.9%) |
641 (29.2%) |
1724 (34.4%) |
||||||||||||
|
85 or older |
214 (38.7%) |
1005 (45.9%) |
2469 (49.2%) |
||||||||||||
|
Unknown/missing data |
14 |
57 |
20 |
||||||||||||
|
Sex |
|
|
|
||||||||||||
|
Men |
208 (36.8%) |
755 (33.6%) |
1472 (28.7%) |
||||||||||||
|
Women |
358 (63.2%) |
1492 (66.4%) |
3660 (71.3%) |
||||||||||||
|
Unknown/missing data |
1 |
2 |
3 |
||||||||||||
|
Pre‐admission cognitive status |
|
|
|
||||||||||||
|
Normal cognition |
353 (63.9%) |
1356 (61.6%) |
3096 (62.0%) |
||||||||||||
|
Impaired cognition |
199 (36.1%) |
845 (38.4%) |
1894 (38.0%) |
||||||||||||
|
Unknown/missing data |
15 |
48 |
145 |
||||||||||||
|
American Society of Anaesthesiologists Classification |
|
|
|
||||||||||||
|
I |
7 (1.5%) |
49 (2.6%) |
121 (2.8%) |
||||||||||||
|
II |
63 (13.8%) |
289 (15.2%) |
795 (18.2%) |
||||||||||||
|
III |
251 (55.0%) |
1122 (58.8%) |
2718 (62.3%) |
||||||||||||
|
IV/V |
135 (29.6%) |
448 (23.5%) |
732 (16.8%) |
||||||||||||
|
Unknown/missing data |
111 |
341 |
769 |
||||||||||||
|
Charlson Comorbidity Index Score (weighted) |
|
|
|
||||||||||||
|
0 |
160 (28.7%) |
729 (33.1%) |
1991 (39.5%) |
||||||||||||
|
1 or 2 |
211 (37.8%) |
852 (38.7%) |
1883 (37.3%) |
||||||||||||
|
3 or more |
187 (33.5%) |
621 (28.2%) |
1171 (23.2%) |
||||||||||||
|
Unknown/missing data |
9 |
47 |
90 |
||||||||||||
|
Pre‐fracture mobility |
|
|
|
||||||||||||
|
Walks without walking aids |
246 (44.3%) |
1062 (47.6%) |
2371 (46.6%) |
||||||||||||
|
Walks with stick or crutch |
78 (14.1%) |
308 (13.8%) |
808 (15.9%) |
||||||||||||
|
Walks with two aids or frame |
187 (33.7%) |
788 (35.4%) |
1801 (35.4%) |
||||||||||||
|
Wheelchair/bedbound |
44 (7.9%) |
71 (3.2%) |
104 (2.1%) |
||||||||||||
|
Unknown/missing data |
12 |
20 |
51 |
||||||||||||
|
Pre‐fracture residence |
|
|
|
||||||||||||
|
Community‐dwelling |
414 (73.0%) |
1608 (71.5%) |
3778 (73.6%) |
||||||||||||
|
Residential aged care facility |
153 (27.0%) |
641 (28.5%) |
1357 (26.4%) |
||||||||||||
|
Deaths |
|
|
|
||||||||||||
|
In‐hospital (acute care) |
45 (7.9%) |
67 (3.0%) |
79 (1.5%) |
||||||||||||
|
30‐day* |
60 (10.8%) |
150 (6.8%) |
208 (4.1%) |
||||||||||||
|
120‐day† |
128 (25.2%) |
330 (16.3%) |
552 (11.7%) |
||||||||||||
|
365‐day‡ |
137 (36.3%) |
394 (27.5%) |
706 (20.2%) |
||||||||||||
|
|
|||||||||||||||
|
* Excludes 153 patients admitted after 30 November 2018. † Excludes 676 patients admitted after 31 August 2018. ‡ Excludes 2632 patients admitted after 31 December 2018. |
|||||||||||||||
Box 3 – Adherence to ACSQHC hip fracture clinical care standards and mortality risk, for 7951 hip fractures in people aged 50 years or older who underwent surgery in 21 New South Wales hospitals after hip fractures, 2015–2018 (complete case analysis): multivariable Poisson regression analyses*
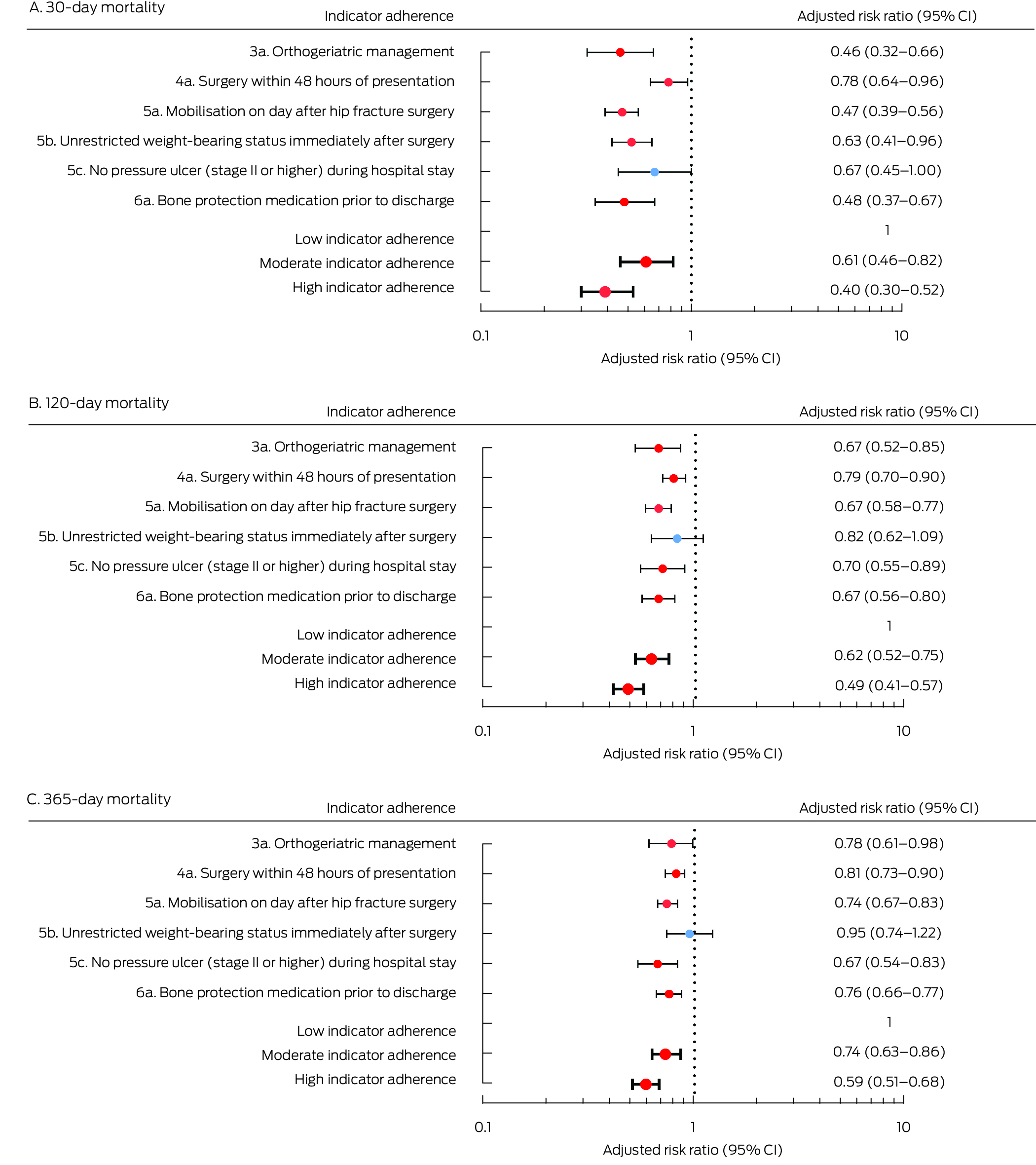
ACSQHC = Australian Commission on Safety and Quality in Health Care; CI = confidence interval.* 30‐day mortality: excludes 153 patients admitted after 30 November 2018; 120‐day mortality: excludes 676 patients admitted after 31 August 2018; 365‐day mortality: excludes 2,632 patients admitted after 31 December 2017.
Received 6 July 2023, accepted 6 August 2024
- Lara Harvey1,2
- Morag E Taylor1,2
- Ian A Harris2
- Rebecca J Mitchell3
- Ian D Cameron4
- Pooria Sarrami3,5
- Jacqueline Close1,2
- 1 Falls, Balance and Injury Research Centre, Neuroscience Research Australia, Sydney, NSW
- 2 UNSW Sydney, Sydney, NSW
- 3 Australian Institute of Health Innovation, Macquarie University, Sydney, NSW
- 4 John Walsh Centre for Rehabilitation Research, Northern Sydney Local Health District and University of Sydney, Sydney, NSW
- 5 New South Wales Institute of Trauma and Injury Management, Sydney, NSW
Open access:
Open access publishing facilitated by University of New South Wales, as part of the Wiley – University of New South Wales agreement via the Council of Australian University Librarians.
Data Sharing:
The data for this population‐based linked data study will not be shared as we do not have ethics approval to do so.
This study was supported by the National Health and Medical Research Council (NHMRC; project grant GNT1164680). Lara Harvey received salary support from the same NHMRC project grant. The NHMRC had no role in the study design, data collection, analysis, interpretation, reporting, or publication. Morag Taylor receives remuneration as a data analyst for the Australian and New Zealand Hip Fracture Registry (ANZHFR; 0.2 fulltime equivalent position).
We thank the NSW Ministry of Health, the NSW Register of Births, Deaths, and Marriages, and the Australian Institute of Health and Welfare for providing access to the administrative data, and the Centre for Health Record Linkage (CHeReL) and the Australian Institute of Health and Welfare Data Linkage Unit for the probabilistic linkage of records.
Lara Harvey is a member of the ANZHFR Research Sub‐committee. Morag Taylor is a parttime data analyst at the ANZHFR and a member of the ANZHFR Research Sub‐committee. Ian Harris is a past and inaugural co‐chair of the ANZHFR. Rebecca Mitchell is a member of the ANZHFR Steering Group, chairs the ANZHFR Data Sub‐committee, and is a member of the ANZHFR Research Sub‐committee. Ian Cameron is a member of the ANZHFR Steering Group. Jacqueline Close is an inaugural and current co‐chair of the ANZHFR.
- 1. Australian and New Zealand Hip Fracture Registry. Annual report 2022. Sept 2022. https://anzhfr.org/wp‐content/uploads/sites/1164/2022/08/ANZHFR‐2022‐Annual‐Report‐Full‐e‐Report‐v2.pdf (viewed July 2024).
- 2. Dyer SM, Crotty M, Fairhall N, et al; Fragility Fracture Network (FFN) Rehabilitation Research Special Interest Group. A critical review of the long‐term disability outcomes following hip fracture. BMC Geriatr 2016; 16: 158.
- 3. Watts JJ, Abimanyi‐Ochom J, Sanders KM. Osteoporosis costing all Australians: a new burden of disease analysis 2012 to 2022 (here: table 41). Sydney: Osteoporosis Australia, 2012. https://healthybonesaustralia.org.au/wp‐content/uploads/2022/09/burden‐of‐disease‐analysis‐2012‐2022.pdf (viewed July 2024).
- 4. Australian Institute of Health and Welfare. The problem of osteoporotic hip fracture in Australia (Bulletin 76) (here: table A2.2). Mar 2010. https://www.aihw.gov.au/getmedia/ea96bc4d‐0b97‐4c5a‐b792‐08b343752adc/10695.pdf.aspx?inline=true (viewed July 2024).
- 5. Stephens AS, Toson B, Close JCT. Current and future burden of incident hip fractures in New South Wales, Australia. Arch Osteoporos 2014; 9: 200.
- 6. Harvey L, Mitchell R, Brodaty H, et al. Differing trends in fall‐related fracture and non‐fracture injuries in older people with and without dementia. Arch Gerontol Geriatr 2016; 67: 61‐67.
- 7. Kenyon‐Smith T, Nguyen E, Oberai T, Jarsma R. Early mobilization post‐hip fracture surgery. Geriatr Orthop Surg Rehabil 2019; 10: 2151459319826431.
- 8. Klestil T, Röder C, Stotter C, et al. Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta‐analysis. Sci Rep 2018; 8: 13933.
- 9. Zeltzer J, Mitchell RJ, Toson B, et al. Orthogeriatric services associated with lower 30‐day mortality for older patients who undergo surgery for hip fracture. Med J Aust 2014; 201: 409‐411. https://www.mja.com.au/journal/2014/201/7/orthogeriatric‐services‐associated‐lower‐30‐day‐mortality‐older‐patients‐who
- 10. Australian and New Zealand Hip Fracture Registry Steering Group. Australian and New Zealand guideline for hip fracture care: improving outcomes in hip fracture management of adults. Sept 2014. https://anzhfr.org/wp‐content/uploads/sites/1164/2021/12/ANZ‐Guideline‐for‐Hip‐Fracture‐Care.pdf (viewed July 2024).
- 11. Australian Commission on Safety and Quality in Health Care. Hip fracture: clinical care standard. Sept 2016. https://www.safetyandquality.gov.au/publications‐and‐resources/resource‐library/hip‐fracture‐clinical‐care‐standard‐2016 (viewed July 2024).
- 12. Farrow L, Hall A, Wood AD, et al. Quality of care in hip fracture patients: the relationship between adherence to national standards and improved outcomes. J Bone Joint Surg Am 2018; 100: 751‐757.
- 13. Griffin XL, Achten J, Parsons N, Costa ML. Does performance‐based remuneration improve outcomes in the treatment of hip fracture? Bone Joint J 2021; 103‐B: 881‐887.
- 14. Patel R, Judge A, Johansen A, et al. Multiple hospital organisational factors are associated with adverse patient outcomes post‐hip fracture in England and Wales: the REDUCE record‐linkage cohort study. Age Ageing 2022; 51: afac183.
- 15. Kjærvik C, Stensland E, Byhring HS, et al. Hip fracture treatment in Norway: deviation from evidence‐based treatment guidelines: data from the Norwegian Hip Fracture Register, 2014 to 2018. Bone Jt Open 2020; 1: 644‐653.
- 16. Harvey LA, Harris IA, Mitchell R, et al. Improved survival rates after hip fracture surgery in New South Wales, 2011–2018. Med J Aust 2022; 216: 420‐421. https://www.mja.com.au/journal/2022/216/8/improved‐survival‐rates‐after‐hip‐fracture‐surgery‐new‐south‐wales‐2011‐2018
- 17. von Elm E, Altman DG, Egger M, et al; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61: 344‐349.
- 18. Toson B, Harvey LA, Close JC. The ICD‐10 Charlson Comorbidity Index predicted mortality but not resource utilization following hip fracture. J Clin Epidemiol 2015; 68: 44‐51.
- 19. Australian Commission on Safety and Quality in Health Care. Hip fracture: clinical care standard. Sept 2023. https://www.safetyandquality.gov.au/publications‐and‐resources/resource‐library/hip‐fracture‐clinical‐care‐standard‐2023 (viewed July 2024).
- 20. Aqil A, Hossain F, Sheikh H, et al. Achieving hip fracture surgery within 36 hours: an investigation of risk factors to surgical delay and recommendations for practice. J Orthop Traumatol 2016; 17: 207‐213.
- 21. Grigoryan KV, Javedan H, Rudolph JL. Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta‐analysis. J Orthop Trauma 2014; 28: e49‐e55.
- 22. Aprisunadi, Nursalam N, Mustikasari M, et al. Effect of early mobilization on hip and lower extremity postoperative: a literature review. SAGE Open Nurs 2023; 9: 23779608231167825.
- 23. Sheehan KJ, Goubar A, Almilaji O, et al. Discharge after hip fracture surgery by mobilisation timing: secondary analysis of the UK National Hip Fracture Database. Age Ageing 2021; 50: 415‐422.
- 24. Lyles KW, Colón‐Emeric CS, Magaziner JS, et al; HORIZON Recurrent Fracture Trial. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 2007; 357: 1799‐1809.
- 25. Yu SF, Cheng JS, Chen YC, et al. Adherence to anti‐osteoporosis medication associated with lower mortality following hip fracture in older adults: a nationwide propensity score‐matched cohort study. BMC Geriatr 2019; 19: 290.
- 26. Griffiths F, Mason V, Boardman F, et al. Evaluating recovery following hip fracture: a qualitative interview study of what is important to patients. BMJ Open 2015; 5: e005406.
- 27. Amarilla‐Donoso FJ, López‐Espuela F, Roncero‐Martín R, et al. Quality of life in elderly people after a hip fracture: a prospective study. Health Qual Life Outcomes 2020; 18: 71.
- 28. Griffin XL, Parsons N, Achten J,et al. Recovery of health‐related quality of life in a United Kingdom hip fracture population. The Warwick Hip Trauma Evaluation: a prospective cohort study. Bone Joint J 2015; 97‐B: 372‐382.






Abstract
Objectives: To determine whether adherence to hip fracture clinical care quality indicators influences mortality among people who undergo surgery after hip fracture in New South Wales, both overall and by individual indicator.
Study design: Retrospective population‐based study; analysis of linked Australian and New Zealand Hip Fracture Registry (ANZHFR), hospital admissions, residential aged care, and deaths data.
Setting, participants: People aged 50 years or older with hip fractures who underwent surgery in 21 New South Wales hospitals participating in the ANZHFR, 1 January 2015 – 31 December 2018.
Main outcome measures: Thirty‐day (primary outcome), 120‐day, and 365‐day mortality (secondary outcomes) by clinical care indicator adherence level (low: none to three of six indicators achieved; moderate: four indicators achieved; high: five or six indicators achieved) and by individual indicator.
Results: Registry data were available for 9236 hip fractures in 9058 people aged 50 years or older during 2015–2018; the mean age of patients was 82.8 years (standard deviation, 9.3 years), 5510 patients were women (69.4%). Complete data regarding adherence to clinical care indicators were available for 7951 fractures (86.1%); adherence to these indicators was high for 5135 (64.6%), moderate for 2249 (28.3%), and low for 567 fractures (7.1%). After adjustment for age, sex, comorbidity, admission year, pre‐admission walking ability, and residential status, 30‐day mortality risk was lower for high (adjusted relative risk [aRR], 0.40; 95% confidence interval [CI], 0.30–0.52) and moderate indicator adherence hip fractures (aRR, 0.61; 95% CI, 0.46–0.82) than for low indicator adherence hip fractures, as was 365‐day mortality (high adherence: aRR, 0.59 [95% CI, 0.51–0.68]; moderate adherence: aRR, 0.74 [95% CI, 0.63–0.86]). Orthogeriatric care (365 days: aRR, 0.78; 95% CI, 0.61–0.98) and offering mobilisation by the day after surgery (365 days: aRR, 0.74; 95% CI, 0.67–0.83) were associated with lower mortality risk at each time point.
Conclusions: Clinical care for two‐thirds of hip fractures attained a high level of adherence to the six quality care indicators, and short and longer term mortality was lower among people who received such care than among those who received low adherence care.