The known: Over the course of the COVID‐19 pandemic, there have been heightened concerns for the health and wellbeing of First Nations people across Australia.
The new: This descriptive study was a retrospective epidemiological review of the impact of COVID‐19 on six remote First Nations communities in Queensland and their community‐led public health responses.
The implications: A community‐led approach should be prioritised in other public health responses throughout First Nations communities.
Over the course of the coronavirus disease 2019 (COVID‐19) pandemic, there were concerns for the health and wellbeing of Aboriginal and/or Torres Strait Islander (respectfully hereafter referred as First Nations) people across Australia.1,2 The health and socio‐economic inequities experienced by First Nations communities that contribute to increased morbidity and mortality are well described.3 Increased prevalence of medical comorbidities in First Nations people — including diabetes, heart disease and chronic kidney disease — place these individuals at higher risk of severe COVID‐19.3 In previous infectious disease epidemics, there have been higher rates of morbidity and mortality among First Nations people compared with non‐First Nations people, resulting in serious cause for concern with COVID‐19.4 Globally, the impact of COVID‐19 in some Indigenous groups has been devastating.5 First Nations communities in remote Australia experience barriers to health including reduced access to health care, limited availability of culturally safe and responsive health services, reduced health literacy and overcrowded housing.6
Before the first COVID‐19 outbreaks across Australia, the federal government enacted the 2015 Biosecurity Act (Cwlth), restricting entry into remote First Nations communities from March 2020 to May 2020.7 Local communities also restricted travel, including travel between the Torres Strait and Papua New Guinea by residents of Torres Strait Treaty communities. Remote First Nations communities initiated their own pandemic planning and preparedness, and the national Aboriginal and Torres Strait Islander Advisory Group on COVID‐19 was established to provide advice on pandemic preparedness and response through the principles of shared decision making, open communication and self‐determination.8 National guidelines for the management of COVID‐19 in remote First Nations communities were established.9 State‐based culturally appropriate COVID‐19 resources were also created.10
As of 30 June 2021, there were 984 000 Aboriginal and Torres Strait Islander people in Australia, representing 3.8% of the total Australian population.11 Across Queensland, there were 237 000 people who identify as First Nations people, representing 4.6% of the Queensland population and 24.1% of the national First Nations population.11 Before the start of the first severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) Omicron outbreak in Queensland, there had been a total of 228 930 cases of COVID‐19 reported across Australia (between 19 January 2020 and 12 December 2021), and 2104 deaths attributed to COVID‐19.12
After months of closure, the Queensland border opened for quarantine‐free travel from the rest of Australia on 13 December 2021. Soon after opening, there was a surge in COVID‐19 cases across the state, including in First Nations communities.13 Public health units across Queensland were primarily responsible for contact tracing and issuing isolation directions. During this period, the public health units partnered with First Nations communities in their public health response. In this article, we describe the preparedness for, epidemiological characteristics of and public health responses to the first two COVID‐19 waves in early 2022 across six discrete remote First Nations communities in Queensland: Badu Island, Cherbourg, Lockhart River, Palm Island, Yarrabah and Woorabinda.
Methods
Setting
Queensland Health provides public health services in Queensland and is comprised of 16 hospital and health services. Most of these have a public health unit that focuses on protecting health, preventing disease, and promoting health. Some public health units provide services for more than one hospital and health service.14 During the COVID‐19 pandemic, public health units were responsible for surveillance, analytics, logistics, risk communication and community engagement in partnership with other hospital and health service stakeholders.
In remote First Nations communities across Queensland throughout 2020 and 2021, local disaster management groups were formed in partnership with Aboriginal shire councils, local health services, public health units and other stakeholders to curate locally appropriate COVID‐19 plans and responses.15 Across the state throughout 2021, vaccination campaigns were a priority and were delivered through a variety of means, including clinics and door‐to‐door programs run by both Queensland Health services and Aboriginal community‐controlled health organisations. Between January 2021 and March 2021, the Queensland vaccine roll‐out offered the AstraZeneca COVID‐19 vaccine. From February 2021, the Queensland population was able to access the Pfizer COVID‐19 vaccine through the government vaccine roll‐out program. Local health services were supported by Aboriginal and Torres Strait Islander health workers and practitioners who were trained in vaccination delivery and contact tracing. To 9 January 2022, children younger than 12 years were ineligible for vaccination. From 10 January 2022, children younger than 5 years were ineligible for vaccination. There were strong partnerships between local First Nations communities and Queensland Health public health units in the planning and response phases of the first two COVID‐19 waves.
For this study, we selected six communities to represent a broad geographic spread of discrete remote First Nations communities across Queensland: Badu Island, Cherbourg, Lockhart River, Palm Island, Yarrabah and Woorabinda (Box 1). Badu Island is 60 km north of Thursday Island, in the western cluster of the Torres Strait islands, and is home to the Mura Badulgal people.16 Cherbourg is on Wakka Wakka country, 267 km north‐west of Brisbane. Lockhart River is 800 km north of Cairns in Far North Queensland on the east coast of Cape York and has six traditional family groups: the Kuuku Ya'u, Wuthathi, Kanthanumpu, Uutaalnganu, Umpila and Kaanju peoples.17 Palm Island (also known as Bwgcolman) is 65 km north‐west of Townsville in North Queensland and is home to the Manbarra people.17 Yarrabah is 55 km east of Cairns in Far North Queensland and is home to the Gunggandji and Yidinji people. Woorabinda is 170 km south‐west of Rockhampton in Central Queensland and is home to the Wadja and Gungaloo peoples.17 Population and housing data for each community are shown in Box 2 and travel times to the nearest regional or tertiary hospital for each community are shown in Box 1.18 These communities were unaffected by COVID‐19 before December 2021.
Data collection and analysis
Descriptive outbreak preparation and response data for the first and second COVID‐19 Omicron waves were provided by the respective Queensland public health units for each community included in this study. Data on vaccination coverage for First Nations and non‐First Nations people in each community were obtained from published fortnightly Australian Immunisation Register (AIR) reports, which include vaccination data recorded on the AIR for individuals aged 15 years or older. Demographic and housing data were obtained from the Australian Bureau of Statistics.20 Unavailability of vaccination coverage rates relating to third and subsequent vaccine doses for First Nations and non‐First Nations people in each community was identified as data limitation. Mandatory reporting of all COVID‐19 cases to public health units was required under the Public Health Regulation 2018 (Qld).21 Case and outbreak characteristics were obtained from the Queensland Health Notifiable Conditions System (NOCS); the number of COVID‐19 vaccine doses received by each person before testing positive for COVID‐19 was sourced from AIR reports and other local medical records as part of the case investigation process. Descriptive statistics, including counts and proportions, were calculated using Microsoft Excel 2016, graphs were produced in R (Version 4.2.1) and the map in Box 1 was created using MapInfo Pro (Version 16.0).
COVID‐19 cases and close contacts were defined in accordance with the COVID‐19 national guidelines for public health units published by the Communicable Diseases Network Australia.22 Outbreak cases were those testing positive to COVID‐19 by polymerase chain reaction (PCR) test or rapid antigen test (RAT) between 13 December 2021 and 12 June 2022 and notified to NOCS, and who completed their 7‐day isolation period in one of the six included First Nations communities (irrespective of their usual place of residence or ethnicity). Public health units issued those who tested positive with an isolation direction under the Public Health Act 2005 (Qld), a legal directive to isolate for 7 days. The first wave included cases testing positive to COVID‐19 between 13 December 2021 and 13 March 2022, and the second wave included those testing positive between 14 March 2022 and 12 June 2022. The periods for the first and second waves in the six communities were consistent with the periods for Queensland's first and second Omicron waves. For the period of the outbreaks, participating public health units sought regular feedback from the communities, and community‐led solutions were implemented. Analysis of feedback from participating communities was completed by each participating public health unit. This epidemiological study complies with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.23
Ethics
Ethics review exemption was obtained from the Far North Queensland Human Research Ethics Committee (EX/2022/QCH/85537) and Darling Downs Health Human Research Ethics Committee (EX/2022/QTDD/85655). Ethics approval was obtained from Townsville Hospital and Health Service Human Research Ethics Committee (HREC/82362 and THHSAQUIRE1498). We acknowledge and have adhered to the Consolidated criteria for strengthening reporting of health research involving Indigenous peoples (CONSIDER) statement.24
Results
Vaccination coverage
Vaccination rates before the first COVID‐19 reported case in a remote First Nations community in Queensland were modest to high. Across all six communities as the state borders opened, COVID‐19 vaccine dose 1 rates ranged from 59.4% to 83.7% of the population. Dose 2 rates ranged from 39.4% to 75.5% of the population (Box 3).
Outbreak epidemiology
The first COVID‐19 case in a First Nations person was reported through NOCS and occurred in Cherbourg on 28 December 2021; this was followed by cases in the five other communities in the subsequent fortnight (Box 4). Across the six communities, there were a total of 2624 cases notified to Queensland Health during the first and second Omicron waves. The case attack rate among the population in each community was 160 of 704 (22.7%) in Badu Island, 402 of 1194 (33.7%) in Cherbourg, 117 of 640 (18.3%) in Lockhart River, 724 of 2098 (34.5%) in Palm Island, 355 of 1019 (34.8%) in Woorabinda and 866 of 2505 (34.6%) in Yarrabah. Of the 2624 cases, 52 (2%) involved hospital admission and two (<1%) were cases in which the person died from COVID‐19. Of the 52 people admitted to hospital, 30 (58%) were female and the median age was 30 years. Five (10%) had received three doses of vaccine, 25 (48%) had received two doses, four (8%) had received one dose and 18 (35%) had received zero doses (11 of whom were age ineligible); 61% of those who were vaccine eligible were up‐to‐date by Australian Technical Advisory Group on Immunisation standards.25 Of the two people who died, one had received three doses of vaccine (the third dose 5 days before they died, and the second dose 5 months before onset of symptoms) and the other was unvaccinated. The epidemiological curves for each community are shown in Box 5. Whole genome sequencing results were available for 101 cases; in 89 cases (88%) the B.1.1529 or BA.1 variant was identified, and in 12 cases (12%) the BA2 variant was identified.
Outbreak response
All communities activated their local disaster management plans, and outbreak control teams were established in partnership with local councils, health services and public health units. COVID‐19 on‐site point‐of‐care PCR testing was available in four of the six communities (Box 6) and, in all but one community, surge testing commenced 1 day after their first community case. The mean PCR turnaround time in the two communities with no point‐of‐care PCR testing was 3 days. Rapid antigen tests (RATs) became available in Queensland from January 2022; in each of the six First Nations communities, they became available 5–8 days after the first case was identified. The numbers of vaccine doses administered in the week after the first case was identified in each community ranged from one to 303. Contact tracing was pursued in all but one community (Box 6). Isolation and quarantine directions were issued for durations of 3–69 days after the outbreak began in four of the six communities, after which this public health legislative process was no longer used.
In addition, intensive individual case management and follow‐up of contacts across all communities were performed by First Nations health workers supported by the local public health units. Social supports were offered to all people who tested positive for SARS‐CoV‐2 and their households, and virtual ward care was offered to those with COVID‐19 to monitor their clinical course and clinical escalation avenues if appropriate. During both waves, efforts were made to assess every person with COVID‐19 for risk of developing severe disease, and the need for treatments including sotrovimab (Box 4) and antiviral therapies (nirmatrelvir–ritonavir and molnupiravir). Statewide sotrovimab and antiviral prescribing guidelines, which outlined clinical criteria for treatment, were used.26 This approach was supplemented by community supports, including food and hygiene supply drop‐offs and phone support hotlines (Box 6).
Discussion
This is a descriptive analysis of the 2021 COVID‐19 outbreak and public health responses in six remote First Nations communities across Queensland: Badu Island, Cherbourg, Lockhart River, Palm Island, Woorabinda, and Yarrabah. All communities worked collaboratively in partnership with local councils, health services and public health units to provide case management and community support. As we await additional COVID‐19 waves, it is timely to examine lessons learnt during the first two SARS‐CoV‐2 Omicron waves of the COVID‐19 pandemic across these First Nations communities.
Common across all six communities was a community‐led approach to preparedness and response that was centred on collaborative partnerships with the communities, their leadership, community‐controlled health services, public health units and state health services. Decision making and governance focused on self‐determination and community ownership of the public health responses implemented in each community. Community ownership extended from the pandemic planning phases and the vaccination rollout into the public health response to COVID‐19 outbreaks, including case and contact management. This included the critical role of in‐community health staff in vaccinating, testing, and supporting those with COVID‐19. Based on our interactions with these communities, the leadership by First Nations community health care workers was identified as a key strategy for successfully overcoming the challenge of a lack of skilled workforce in these areas. This approach is consistent with that of other First Nations communities, including those in New Zealand and Canada.27,28 This community‐led approach highlights the importance of First Nations leadership in this public health response and other public health policies and initiatives.29
Overcrowded housing is a significant risk factor for SARS‐CoV‐2 transmission. The reality of isolation and quarantine in overcrowded housing in remote locations created challenges such as ensuring adequate food, medicines and other supplies for all residents. Some households did not have enough electricity credit. Overcrowding is more prevalent among First Nations people, who, Australia wide, are 3.7 times more likely to live in overcrowded housing than non‐First Nations people.30 This in turn, increases SARS‐CoV‐2 transmission risk and has negative impacts on the ability of people with COVID‐19 to isolate and the ability of their close contacts to quarantine effectively. The average number of people per household ranged between 3.3 and 4.5 — likely under‐representative of the true burden of overcrowding in these communities (Box 2). The high rates of overcrowding and poor standard of housing for First Nations communities contribute not only to communicable disease risk but also difficulties maintaining good hygiene and inhibition of general healthy living practices.30 Overcrowding featured as a policy outcome in the National Agreement on Closing the Gap. Outcome 9 of the agreement states that Aboriginal and Torres Strait Islander people need appropriate, affordable housing that is aligned with their priorities and needs, and includes a target of 88% of First Nations people living in non‐overcrowded housing by 2031.30 More policies and programs directed at reducing rates of overcrowding are needed to improve health outcomes.
Communities with SARS‐CoV‐2 point‐of‐care PCR testing had reduced turnaround times for results compared with those lacking point‐of‐care PCR testing, except for Woorabinda, located only 2 hours from the nearest hospital and pathology centre. In‐community point‐of‐care PCR testing facilitated increased testing and the ability to rapidly implement isolation, and therefore reduced the risk of contagion. Remote communities with point‐of‐care PCR testing were trained in using the technology, including troubleshooting and quality control.31 There is an ongoing need for point‐of‐care testing in remote communities to shorten the time to diagnostic decisions and targeted management plans for infectious diseases beyond COVID‐19. Although the availability of RATs was limited during the first COVID‐19 wave, supplies improved during the second wave.
The six remote First Nations communities included in our study all relied heavily on robust digital health systems to prepare for and manage the first COVID‐19 waves. This included NOCS to record COVID‐19 cases and contacts, AIR to keep track of immunisation records, and local electronic medical records to identify vulnerable community members. Moreover, telehealth was a vital component of health care delivery across the whole country, including in First Nations communities.32 A skilled workforce, empowered consumers, reformed funding arrangements and improved digital ecosystems are key to optimising digital health capacities in remote First Nations communities in the future.33
Strengths and limitations
Describing the response to the first two COVID‐19 waves in six remote First Nations communities has been vital in preparing for future culturally appropriate and community‐led outbreak responses in discrete communities in Australia. Key limitations of this work include case selection bias, vaccination coverage measurement, observer bias and a lack of available data. Firstly, bias in case ascertainment likely varied between study sites as in some communities the access and willingness to test may have been different to others. Some communities had more self‐testing done, compared with testing done by registered health professionals. Secondly, we reported on vaccination coverage of First Nations residents in remote communities despite there being a proportion of non‐Indigenous people residing in these communities. Thirdly, each community had varying methods for testing and for communicating positive test results with individuals, and varying approaches to data collection. Together with the difficulties documenting fluid households, this could have led to biases and measurement error. Finally, there was a lack of available data, including rates of vaccination with dose 3 of a COVID‐19 vaccine, secondary attack rates among close contacts, and information on comorbidities and other risk factors (eg, being employed as a health or care worker, or living with a disability). Future descriptive studies incorporating such data would be of value.
Conclusions
During the first two outbreaks of the SARS‐CoV‐2 Omicron variant, COVID‐19 morbidity and mortality were low in the six remote Queensland First Nations communities included in our study. Badu Island, Cherbourg, Lockhart River, Palm Island, Woorabinda and Yarrabah all successfully met the challenges of these unprecedented outbreaks. The co‐designed, collaborative partnerships between local First Nations councils, community‐controlled health services, state health services and public health units to prepare for and respond to these COVID‐19 outbreaks illustrate the importance of shared decision making and self‐determination in public health responses for remote First Nations communities.
Box 1 – Map of First Nations communities included in the study: Badu Island, Cherbourg, Lockhart River, Palm Island, Yarrabah and Woorabinda in Queensland, Australia*
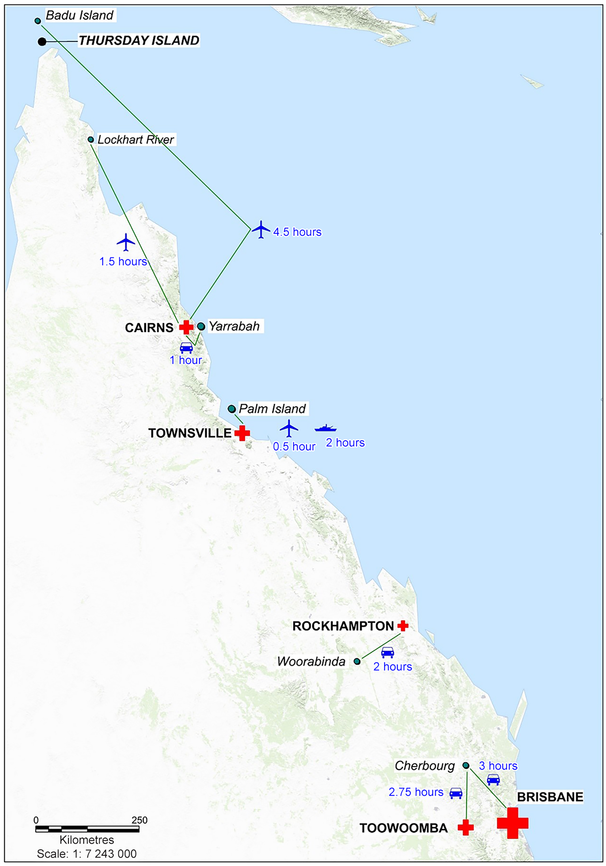
* Small red crosses represent regional hospitals; the large red cross represents a tertiary hospital; and the numbers of hours at each car, plane and boat icon indicate the time taken to travel by each of these modes of transport from the remote communities to nearest regional or tertiary hospital.
Box 2 – Demographic characteristics of six First Nations communities in Queensland based on Australian Bureau of Statistics 2021 census data18
|
|
Badu Island |
Cherbourg |
Lockhart River |
Palm Island |
Woorabinda |
Yarrabah |
|||||||||
|
|
|||||||||||||||
|
Total population, n |
704 |
1194 |
640 |
2098 |
1019 |
2505 |
|||||||||
|
Adults, n (%)* |
463 (65.8%) |
775 (64.9%) |
468 (73.1%) |
1440 (68.6%) |
777 (76.3%) |
1757 (70.1%) |
|||||||||
|
First Nations people, n (%) |
612 (86.9%) |
1151 (96.4%) |
502 (78.4%) |
1918 (91.4%) |
933 (91.6%) |
2402 (95.9%) |
|||||||||
|
Female sex, n (%) |
363 (51.6%) |
614 (51.4%) |
304 (47.5%) |
1092 (52.0%) |
545 (53.4%) |
1286 (51.3%) |
|||||||||
|
Age in years, median |
27 |
23 |
27 |
26 |
23 |
25 |
|||||||||
|
People per household, mean |
3.3 |
3.4 |
3.4 |
3.7 |
3.3 |
4.5 |
|||||||||
|
People living in overcrowded housing, %† |
41.9%‡ |
47.9% |
57.4% |
63.2% |
45.8% |
68.3% |
|||||||||
|
|
|||||||||||||||
|
* Aged 15 years or older. † Defined as living in a dwelling which requires four or more extra bedrooms to accommodate the people who usually live there, as defined by the Canadian National Occupancy Standard.19 ‡ Australian Bureau of Statistics overcrowding rates for Badu Island are reported as those for the Torres Strait Island Regional Council area of which the island is a part. |
|||||||||||||||
Box 3 – COVID‐19 vaccination coverage among First Nations people in each community (local government area level), 22 December 2021*,†
|
|
Vaccination coverage (Indigenous AIR population) |
||||||||||||||
|
|
Badu Island‡ |
Cherbourg |
Lockhart River |
Palm Island |
Woorabinda |
Yarrabah |
|||||||||
|
|
|||||||||||||||
|
First Nations individuals who had received dose 1, % |
83.7% |
68.8% |
82.8% |
72.0% |
59.4% |
72.2% |
|||||||||
|
First Nations individuals who had received dose 2, % |
71.9% |
57.9% |
75.5% |
58.4% |
39.4% |
58.3% |
|||||||||
|
|
|||||||||||||||
|
AIR = Australian Immunisation Register; COVID‐19 = coronavirus disease 2019. * Data obtained from the Australian Government Department of Health and Aged Care; the website is no longer publicly available. ‡ Vaccination rate denominators are based on the eligible populations. † AIR vaccination rates for Badu Island are reported as those for the Torres Strait Island Regional Council area of which the island is a part. |
|||||||||||||||
Box 4 – COVID‐19 outbreak characteristics in six First Nations communities in Queensland
|
|
Badu Island |
Cherbourg |
Lockhart River |
Palm Island |
Woorabinda |
Yarrabah |
|||||||||
|
|
|||||||||||||||
|
First positive test date |
9 Jan 2022 |
28 Dec 2021 |
4 Jan 2022 |
31 Dec 2021 |
6 Jan 2022 |
5 Jan 2022 |
|||||||||
|
Total cases, n |
160 |
402 |
117 |
724 |
355 |
866 |
|||||||||
|
Attack rate, n/N (%)* |
160/704 (22.7%) |
402/1194 (33.7%) |
117/640 (18.3%) |
724/2098 (34.5%) |
355/1019 (34.8%) |
866/2505 (34.6%) |
|||||||||
|
Cases in wave 1, n (%)† |
127 (79.4%) |
271 (67.4%) |
97 (82.9%) |
655 (90.5%) |
249 (70.1%) |
775 (89.5%) |
|||||||||
|
Cases in wave 2, n (%)‡ |
33 (20.6%) |
131 (32.6%) |
20 (17.1%) |
69 (9.5%) |
106 (29.9%) |
91 (10.5%) |
|||||||||
|
Characteristics of people who tested positive |
|
|
|
|
|
|
|||||||||
|
First Nations person, n (%) |
152 (95.0%) |
387 (96.3%) |
101 (86.3%) |
705 (97.4%) |
338 (95.2%) |
849 (98.0%) |
|||||||||
|
Female sex, n (%) |
91 (56.9%) |
231 (57.3%) |
59 (50.4%) |
410 (56.6%) |
202 (56.9%) |
483 (55.8%) |
|||||||||
|
Age in years, median (IQR) |
22.9 (34.7) |
28.9 (29.0) |
28.1 (23.4) |
25.6 (32.2) |
27.1 (29.6) |
29.8 (26.5) |
|||||||||
|
Vaccine doses received, n (%) |
|
|
|
|
|
|
|||||||||
|
0 |
44 (27.5%) |
123 (30.6%) |
16 (13.7%) |
181 (25.0%) |
105 (29.6%) |
157 (18.1%) |
|||||||||
|
1 |
14 (8.8%) |
41 (10.2%) |
12 (10.3%) |
88 (12.2%) |
43 (12.1%) |
95 (11.0%) |
|||||||||
|
2 |
41 (25.6%) |
169 (42.0%) |
61 (52.1%) |
271 (37.4%) |
109 (30.7%) |
471 (54.4%) |
|||||||||
|
3 |
44 (27.5%) |
44 (10.9%) |
23 (19.7%) |
104 (14.4%) |
57 (16.1%) |
94 (10.9%) |
|||||||||
|
Not age eligible, n (%)§ |
17 (10.6%) |
25 (6.2%) |
5 (4.3%) |
80 (11.0%) |
41 (11.5%) |
49 (5.7%) |
|||||||||
|
Treated with sotrovimab, n (%) |
0 |
5 (1.2%) |
0 |
7 (1.0%) |
4 (1.1%) |
2 (0.2%) |
|||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; IQR = interquartile range.* Attack rates were calculated using population denominators from Australian Bureau of Statistics 2021 census data.18 † Wave 1 period was 13 December 2021 to 13 March 2022. ‡ Wave 2 period was 14 March 2022 to 12 June 2022. § To 9 January 2022, children younger than 12 years were ineligible for vaccination; from 10 January 2022, children younger than 5 years were ineligible for vaccination. |
|||||||||||||||
Box 5 – Numbers of cases of COVID‐19 and rates of cases per 1000 people in six First Nations communities in Queensland by date of specimen collection (13 December 2021 to 12 June 2022)

COVID‐19 = coronavirus disease 2019.
Box 6 – COVID‐19 public health outbreak response for six First Nations communities in Queensland
|
|
Badu Island |
Cherbourg |
Lockhart River |
Palm Island |
Woorabinda |
Yarrabah |
|||||||||
|
|
|||||||||||||||
|
COVID‐19 testing |
|
|
|
|
|
|
|||||||||
|
Access to on‐site point‐of‐care PCR testing |
Yes |
No |
Yes |
Yes |
No |
Yes |
|||||||||
|
Surge testing commenced, number of days after first case |
1* |
1 |
5* |
1 |
1 |
1 |
|||||||||
|
Mean PCR turnaround time in first week of outbreak, days |
0 |
3 |
0 |
0 |
0 |
0 |
|||||||||
|
RAT testing available in community, number of days after first case |
7 |
5 |
8 |
7 |
7 |
0 |
|||||||||
|
Residents tested (by PCR and/or RAT) in first week of outbreak, n (%) |
19† (2.7%) |
100 (8.4%) |
66* (10.3%) |
12 (0.6%) |
765 (75.1%) |
NA |
|||||||||
|
COVID‐19 vaccinations |
|
|
|
|
|
|
|||||||||
|
Surge vaccinations commenced, number of days after first case |
2 |
4 |
Not undertaken |
Not undertaken |
3 |
Not undertaken |
|||||||||
|
Vaccine doses administered in first week after first case, n |
9 |
140 |
1 |
10 |
72 |
303 |
|||||||||
|
Contact tracing |
|
|
|
|
|
|
|||||||||
|
Duration of use of contact tracing, number of days after first case |
Not undertaken |
3–5 |
0 |
3–5 |
69 |
39 |
|||||||||
|
Duration of use of isolation directions, number of days after first case |
10 |
0 |
10 |
7 |
69 |
0 |
|||||||||
|
Duration of use of quarantine directions, number of days after first case |
3 |
0 |
3 |
6 |
69 |
0 |
|||||||||
|
Community supports |
|
|
|
|
|
|
|||||||||
|
Food drop‐off |
No |
Yes |
Yes |
Yes |
Yes |
Yes |
|||||||||
|
Support hotline |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
|||||||||
|
Response team |
No |
Yes: Indigenous health workers |
No |
Yes: Indigenous health workers |
Yes: Indigenous health workers |
Yes: Indigenous health workers |
|||||||||
|
Community messaging |
Radio, social media |
Radio, social media |
Radio, social media |
Radio, social media |
Radio, social media |
Delivered by local council |
|||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; NA = not available; PCR = polymerase chain reaction; RAT = rapid antigen test. * Tested by RAT. † Tested by PCR; numbers tested by RAT before 24 January 2022 are not available. |
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
Received 19 January 2023, accepted 18 March 2024
- Allison Hempenstall1,2
- Barbara Telfer3
- Sean Cowley3
- Shalomie Shadrach4
- Caroline Taunton2
- Jay Short5
- Nicolas Smoll6
- Roy Rasalam5
- Oscar Whitehead7
- Peter Roach8
- Karen Koko9
- Josh Stafford9
- Rittia Matysek2
- Renarta Whitcombe6
- Gulam Khandaker6
- Jason King8
- Nishila Moodley5
- Maree Finney5
- Rica Lacey4
- Steven Donohue5
- Richard Gair7
- Katie Panaretto3
- 1 James Cook University, Townsville, QLD
- 2 Torres and Cape Hospital and Health Service, Cairns, QLD
- 3 Queensland Health, Brisbane, QLD
- 4 Darling Downs Hospital and Health Service, Toowoomba, QLD
- 5 Townsville Hospital and Health Service, Townsville, QLD
- 6 Central Queensland Hospital and Health Service, Rockhampton, QLD
- 7 Cairns and Hinterland Health Service, Cairns, QLD
- 8 Gurriny Yealamucka Health Service, Yarrabah, QLD
- 9 Lockhart River Primary Health Care Centre, Lockhart River, QLD
Data sharing:
No data sharing is available from this study in line with Indigenous data sovereignty.
We acknowledge the people living in the six communities included in our study, and are grateful for the support from and partnerships with the local councils: Torres Strait Island Regional Council, Cherbourg Aboriginal Shire Council, Lockhart River Aboriginal Shire Council, Palm Island Aboriginal Shire Council, Woorabinda Aboriginal Shire Council and Yarrabah Aboriginal Shire Council. We also thank the local public health unit staff, Queensland Health primary health care centres and other stakeholders from these six communities for their support. In addition, we thank Marko Simunovic, Principal Business Analyst, Queensland Health, for his data quality work and Kathy Piotrowski, Data Manager, Queensland Health, for creating the figure in Box 1.
No relevant disclosures.
- 1. Yashadhana A, Pollard‐Wharton N, Zwi AB, Biles B. Indigenous Australians at increased risk of COVID‐19 due to existing health and socioeconomic inequities. Lancet Reg Health West Pac 2020; 1: 100007.
- 2. Thurber KA, Barrett EM, Agostino J, et al. Risk of severe illness from COVID‐19 among Aboriginal and Torres Strait Islander adults: the construct of ‘vulnerable populations’ obscures the root causes of health inequities. Aust N Z J Public Health 2021; 45: 658‐663.
- 3. Australian Bureau of Statistics. National Aboriginal and Torres Strait Islander Health Survey. Canberra: Australian Bureau of Statistics, 2019. https://www.abs.gov.au/statistics/people/aboriginal‐and‐torres‐strait‐islander‐peoples/national‐aboriginal‐and‐torres‐strait‐islander‐health‐survey/latest‐release (viewed Dec 2022).
- 4. Rudge S, Massey PD. Responding to pandemic (H1N1) 2009 influenza in Aboriginal communities in NSW through collaboration between NSW Health and the Aboriginal community‐controlled health sector. N S W Public Health Bull 2010; 21: 26‐29.
- 5. Millalen P, Nahuelpan H, Hofflinger A, Martinez E. COVID‐19 and Indigenous peoples in Chile: vulnerability to contagion and mortality. AlterNative 2020; 16(4): 399‐402.
- 6. Australian Institute of Health and Welfare. First Nations people and the health system. Canberra: AIHW, 2024. https://www.aihw.gov.au/reports/australias‐health/indigenous‐australians‐use‐of‐health‐services (viewed July 2024).
- 7. Maclean H, Elphick K. COVID‐19 legislative response—human biosecurity emergency declaration explainer. Flagpost (Parliament of Australia); 19 Mar 2020. https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/FlagPost/2020/March/COVID‐19_Biosecurity_Emergency_Declaration (viewed Dec 2022).
- 8. Crooks K, Casey D, Ward JS. First Nations peoples leading the way in COVID‐19 pandemic planning, response and management. Med J Aust 2020; 213: 151‐152.e1. https://www.mja.com.au/journal/2020/213/4/first‐nations‐peoples‐leading‐way‐covid‐19‐pandemic‐planning‐response‐and
- 9. Australian Government Department of Health and Aged Care. CDNA national guidance for remote Aboriginal and Torres Strait Islander communities for COVID‐19. Canberra: Australian Government, 2022. https://www.health.gov.au/sites/default/files/documents/2022/02/cdna‐national‐guidance‐for‐remote‐aboriginal‐and‐torres‐strait‐islander‐communities‐for‐covid‐19.pdf (viewed Dec 2022).
- 10. Queensland Aboriginal and Islander Health Council. COVID‐19 (coronavirus) resources. Brisbane: QAIHC, 2022. https://www.qaihc.com.au/resources/covid‐19‐coronavirus‐resources (viewed Dec 2022).
- 11. Australian Bureau of Statistics. Queensland: Aboriginal and Torres Strait Islander population summary. Canberra: ABS, 2022. https://www.abs.gov.au/articles/queensland‐aboriginal‐and‐torres‐strait‐islander‐population‐summary (viewed Dec 2022).
- 12. Australian Government Department of Health and Aged Care. Coronavirus (COVID‐19) at a glance – 12 December 2021 [infographic]. Canberra: Australian Government, 2021. https://www.health.gov.au/resources/publications/coronavirus‐covid‐19‐at‐a‐glance‐12‐december‐2021?language=en (viewed Dec 2022).
- 13. Queensland Government. Queensland borders re‐open [media release]. 6 Dec 2021. Brisbane: Queensland Government, 2021. https://statements.qld.gov.au/statements/93994 (viewed Dec 2022).
- 14. Queensland Health. Public health units. Brisbane: Queensland Health, 2023. https://www.health.qld.gov.au/system‐governance/contact‐us/contact/public‐health‐units (viewed Mar 2023).
- 15. Queensland Government. Disaster management [website]. Brisbane: Queensland Government, 2021. https://www.disaster.qld.gov.au (viewed Dec 2022).
- 16. Torres Strait Island Regional Council. Badu. Cairns: TSIRC, 2022. https://www.tsirc.qld.gov.au/communities/badu (viewed Dec 2022).
- 17. National Indigenous Australians Agency. Communities. Canberra: Australian Government, 2022. https://www.indigenous.gov.au/communities (viewed Dec 2022).
- 18. Australian Bureau of Statistics. 2021 census all persons quickstats. Canberra: ABS, 2021. https://abs.gov.au/census/find‐census‐data/quickstats/2021/AUS (viewed Dec 2022).
- 19. Australian Institute of Health and Welfare. Canadian National Occupancy Standard. Canberra: AIHW, 2017. https://meteor.aihw.gov.au/content/386254 (viewed Mar 2023).
- 20. Australian Institute of Health and Welfare; National Indigenous Australians Agency. Measures. 2.01 Housing. In: Aboriginal and Torres Strait Islander Health Performance Framework. Canberra: AIHW. https://www.indigenoushpf.gov.au/measures/2‐01‐housing (viewed Dec 2022).
- 21. Queensland Health. List of notifiable conditions. Brisbane: Queensland Government, 2023. https://www.health.qld.gov.au/clinical‐practice/guidelines‐procedures/diseases‐infection/notifiable‐conditions/list (viewed Mar 2023).
- 22. Australian Government Department of Health and Aged Care. Coronavirus (COVID‐19) – CDNA national guidelines for public health units. Canberra: Australian Government, 2020. https://www.health.gov.au/resources/publications/coronavirus‐covid‐19‐cdna‐national‐guidelines‐for‐public‐health‐units?language=en (viewed Dec 2022).
- 23. von Elm E, Altman DG, Egger M, et al; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007; 335: 806‐808.
- 24. Huria T, Palmer SC, Pitama S, et al. Consolidated criteria for strengthening reporting of health research involving indigenous peoples: the CONSIDER statement. BMC Med Res Methodol 2019; 19: 173.
- 25. Australian Government Department of Health and Aged Care. Stay up to date with your COVID‐19 vaccines. Canberra: Australian Government, 2023. https://www.health.gov.au/our‐work/covid‐19‐vaccines/getting‐your‐vaccination/stay‐up‐to‐date (viewed Mar 2023).
- 26. Queensland Health. Sotrovimab prescribing guideline [guideline retired]. Brisbane: Queensland Health, 2021. https://www.health.qld.gov.au/clinical‐practice/guidelines‐procedures/novel‐coronavirus‐qld‐clinicians (viewed Mar 2023).
- 27. Power T, Wilson D, Best O, et al. COVID‐19 and Indigenous peoples: an imperative for action. J Clin Nurs 2020; 29: 2737‐2741.
- 28. Smith CR, Enns C, Cutfeet D, et al. COVID‐19 in a remote First Nations community in British Columbia, Canada: an outbreak report. CMAJ Open 2021; 9: E1073‐E1079.
- 29. Markham F, Smith D, Morphy F. Indigenous Australians and the COVID‐19 crisis: perspectives on public policy. Canberra: Australian National University, 2020. https://caepr.cass.anu.edu.au/research/publications/indigenous‐australians‐and‐covid‐19‐crisis‐perspectives‐public‐policy (viewed Dec 2022).
- 30. National Agreement on Closing the Gap. August 2022. https://www.closingthegap.gov.au/sites/default/files/2022‐09/ctg‐national‐agreement_apr‐21‐comm‐infra‐targets‐updated‐24‐august‐2022_0.pdf (viewed Dec 2022).
- 31. Hengel B, Causer L, Matthews S, et al. A decentralised point‐of‐care testing model to address inequities in the COVID‐19 response. Lancet Infect Dis 2021; 21: e183‐e190. Erratum in: Lancet Infect Dis 2021; 21: e182.
- 32. Begay M, Kakol M, Sood A, Upson D. Strengthening digital health technology capacity in Navajo communities to help counter the COVID‐19 pandemic. Ann Am Thorac Soc 2021; 18: 1109‐1114.
- 33. Thomas EE, Haydon HM, Mehrotra A, et al. Building on the momentum: sustaining telehealth beyond COVID‐19. J Telemed Telecare 2022; 28: 301‐308.






Abstract
Objective: To describe the preparedness for, epidemiological characteristics of and public health responses to the first and second waves of coronavirus disease 2019 (COVID‐19) in six remote Aboriginal and Torres Strait Islander communities in Queensland from late 2021.
Design: This was a descriptive epidemiological study. Data were collated by each participating public health unit. Case and outbreak characteristics were obtained from the statewide Notifiable Conditions System.
Setting, participants: Six discrete remote First Nations communities across Queensland were selected to represent a broad geographic spread across the state: Badu Island, Cherbourg, Lockhart River, Palm Island, Woorabinda and Yarrabah. People with a positive severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) test result recorded between 13 December 2021 and 12 June 2022 who acquired the infection and isolated in one of the six communities.
Main outcome measures: COVID‐19 vaccination coverage among First Nations people; number of COVID‐19 cases reported; and attack rates for each community.
Results: All six First Nations communities led the COVID‐19 preparedness and planning. COVID‐19 vaccination coverage rates before the first outbreak ranged from 59% to 84% for the first dose and from 39% to 76% for the second dose across the six communities. During the study period, 2624 cases of COVID‐19 in these communities were notified to Queensland Health. Attack rates for each community were: Badu Island, 23%; Cherbourg, 34%; Lockhart River, 18%; and Palm Island, Woorabinda and Yarrabah, 35% each. The 2624 cases included 52 cases (2%) involving hospital admission and two cases (< 1%) in which the person died from COVID‐19.
Conclusions: It is likely that the co‐designed, collaborative partnerships between local councils, community‐controlled health services, state health services and public health units positively impacted the management and outcomes of COVID‐19 in each of the six communities.