There is increasing evidence for the benefits and clinical effectiveness of electronic health (eHealth) interventions,1,2,3,4,5,6 including those with a focus on First Nations populations globally.7,8,9 In Australia, positive outcomes are reported for eHealth interventions with Aboriginal and Torres Strait Islander peoples, including for mental health challenges,10,11 support for new fathers,12 upskilling health care staff,13 cultural connections,14 and specialist access for rural and remote areas.5,15 These and other eHealth interventions have been led by, and/or deployed in partnership with, Aboriginal Community Controlled Health Organisations (ACCHOs).16,17 Broader population use of digital devices and technology has also affected health care so that eHealth is no longer an add‐on, but almost an integral part of daily life for all Australians, including Aboriginal and Torres Strait Islander people.6,16,17,18 However, there remains a lack of guidance for culturally safe eHealth with Aboriginal and Torres Strait Islander people. A research program to develop a best practice framework for eHealth with Aboriginal and Torres Strait Islander people was established in 2022.16 Governance is held by a multi‐agency partnership (the Collaboration), which focuses on promoting an evidence base for eHealth that is specific to the interests and priorities of Aboriginal and Torres Strait Islander people. This narrative review contributes to the Collaboration's foundational work to better understand the characteristics of the intervention process that are important to Aboriginal and Torres Strait Islander people. Research has explored aspects of cultural safety and co‐design in single studies,11,19,20 for specific modalities such as mobile health (mHealth),8,17 or alongside the significance of cultural safety with other First Nation populations.7,9,21 The aim of this narrative review was to identify the important characteristics of eHealth interventions, and critique the cultural quality of eHealth research with Aboriginal and Torres Strait Islander peoples.
The eHealth modalities deployed within this review include mHealth, telehealth, and mobile diagnostic tools. Further definitions for key phrases are provided in the Supporting information, appendix 1 (eg, eHealth, Aboriginal and Torres Strait Islander people, ACCHOs, and cultural safety).
Our authorship reflects a diversity of background, career stage, gender and race. Specific to the focus of this article, Ray Mahoney and Andrew Goodman are Aboriginal, and Georgina Chelberg, Charankarthi Musuwadi, Liam Caffery and Sheleigh Lawler are non‐Indigenous.
Methods
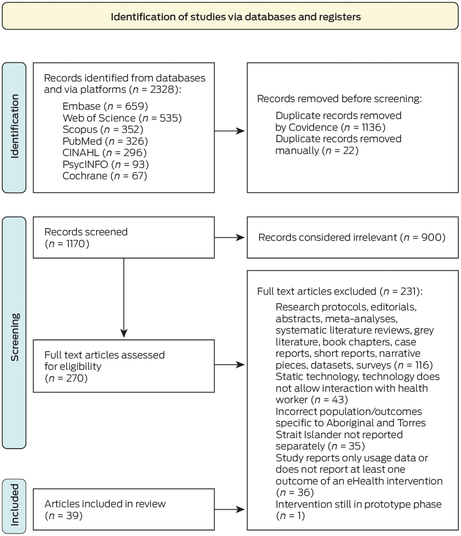
We conducted searches directly via electronic databases or Web of Science and EBSCOhost platforms (PubMed, Embase, Scopus, PsycInfo, Cochrane, CINAHL) to 2 December 2022, with no limit to publication year. The protocol was registered as a systematic review (PROSPERO 380254), but subsequently reported as a narrative review, retaining the PRISMA structure.22 Preliminary searches refined the strategy (Supporting information, appendix 2), with two themes: “Aboriginal and Torres Strait Islander” and “eHealth”. The Lowitja Institute's LIt.Search tool was also employed.23
Eligible studies were full text, published in English in peer‐reviewed scientific journals, and included narrative data regarding eHealth interventions with Aboriginal and Torres Strait Islander people using experimental, observational, mixed methods and qualitative designs. Exclusion was based on study design, technology type, and data aspects. Participants of eligible studies were either Aboriginal and Torres Strait Islander people or health staff (including non‐Indigenous people) who work with Aboriginal and Torres Strait Islander people. If study participants were culturally diverse, only outcomes relating to Aboriginal and Torres Strait Islander people were extracted.
Screening and data extraction were completed using Endnote (Clarivate) and Covidence (Veritas Health Innovation). Two authors (GC, CM) independently screened title and abstracts, then full text, and reached consensus with a third author (LC), noting reasons for exclusion.
Characteristics of final studies were collated and cross‐checked by two authors (CM, GC), with data extraction embedded in the data analysis phase, discussed below.
Although not standard for narrative reviews, quality assessments of the studies were completed using a hybrid approach. The Joanna Briggs Institute Levels of Evidence (JBI LoE) for effectiveness and meaningfulness were applied, based on study design, with lower scores indicating a more rigorous design.24,25 Two authors (GC, LC) independently scored studies against the JBI LoE with an average used as the final score. The Aboriginal and Torres Strait Islander Quality Appraisal Tool (the QAT)26,27 was applied to assess the studies’ cultural quality. Three authors (GC, AG, SL) worked collaboratively to appraise one study, and then independently appraised 13 articles each. To complement the QAT process for each study, authors’ positionality was sought using publicly available statements.
Two authors independently completed extraction of qualitative data segments in Excel (Microsoft), including direct quotes, statements and descriptions about the eHealth interventions from final studies (AG, n = 19; GC, n = 20). Iterative content analysis to develop codes and themes followed Bengtsson's approach to authentically represent the literature.28 One author (GC) systematically reviewed proposed themes by revisiting the full text articles. Consensus on final themes, subthemes and factors was established in discussion among three authors (AG, GC, SL). An odds ratio was calculated to determine the association between the number of Aboriginal and Torres Strait Islander authors and the QAT scores.
This review is considered exempt from ethics approval as it reports on non‐identifiable, publicly available data and is of negligible risk. The conduct of this review was informed by the Consolidated criteria for strengthening the reporting of health research involving Indigenous Peoples (CONSIDER) statement29 (Supporting information, appendix 3).
Study characteristics
A total of 39 full text studies reported on the use of eHealth with Aboriginal and Torres Strait Islander people in mainstream and community‐controlled settings (Box 1 and Box 2).10,11,12,14,15,18,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62 Final studies used mHealth (n = 24; eg, mobile applications), telehealth (n = 10; eg, videoconferencing), mobile diagnostic tools (n = 2; eg, point‐of‐care device), other (n = 1; eg, social media) or multiple modalities (n = 2). Research partnerships and relationships were established with ACCHOs (n = 18) and other Aboriginal and Torres Strait Islander organisations (n = 9; eg, media company). The eHealth interventions addressed mental health and social emotional wellbeing (n = 9), chronic disease management (n = 6), health promotion (n = 6), screening (n = 6), health care access (n = 5), maternal and infant health (n = 5), substance use (n = 3), and caregiver support (n = 1). Participants included Aboriginal and Torres Strait Islander people who were direct or indirect consumers (patients and/or carers), as well as non‐Indigenous and Aboriginal and Torres Strait Islander health professionals. Studies were conducted in a variety of urban, regional and remote settings across Queensland (n = 12), New South Wales (n = 17), Victoria (n = 1), Western Australia (n = 3), South Australia (n = 4) and the Northern Territory (n = 12).
Quality assessment
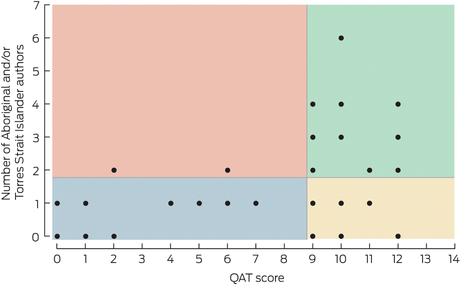
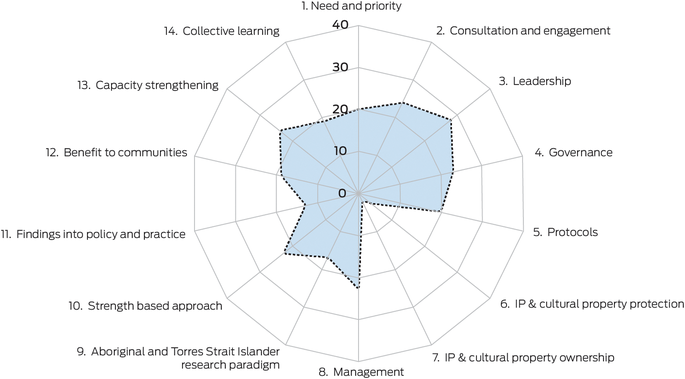
Significant heterogeneity of study designs resulted in a range of JBI LoE categories (Box 2). Individual QAT scores (Box 2) were also notably varied, with scores from 0 to 12 out of a possible 14 (Box 3). Analysis using the composite QAT scores of the final studies (Box 4) revealed strengths in Aboriginal and Torres Strait Islander leadership and consultation with Aboriginal and Torres Strait Islander community controlled organisations. Strengths‐based approaches and capacity building with Aboriginal and Torres Strait Islander people were also present. Areas for improvement were the reporting of intellectual property, cultural property, ownership and protection. There was a statistically significant association between the number of Aboriginal and Torres Strait Islander authors and higher scores on the QAT criteria (ρ = 0.0036). We created dichotomous variables, “Aboriginal and Torres Strait Islander authors” (< 2 or ≥ 2) and “QAT scores” (≤ 8 or ≥ 9), and found that studies with two or more Aboriginal and Torres Strait Islander authors were 12.75 times (95% confidence interval, 2.29–70.57) more likely to achieve a QAT score of 9 or more compared with articles with less than two Aboriginal and Torres Strait Islander authors (Box 5).
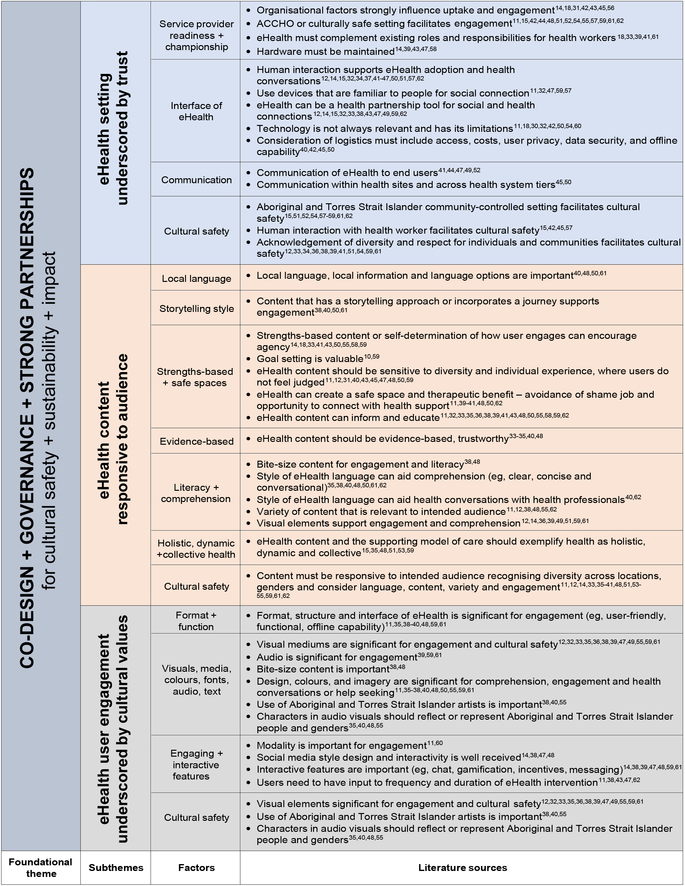
Content analysis
Extracted data segments contained the voices of a range of stakeholders, including Aboriginal and Torres Strait Islander and non‐Indigenous people, who were health care consumers, family, community members, health care workers, health professionals, researchers and creative professionals. Content analysis of these stakeholder perspectives yielded factors, subthemes and a foundational theme that is represented in the structure of the Box 6. The significance of the foundational theme, described as follows, is that it upholds the pragmatic subthemes of culturally safe eHealth interventions with Aboriginal and Torres Strait Islander people.
Foundational theme: authentic co‐design with Aboriginal and Torres Strait Islander governance and strong partnerships
Consistent reference throughout the literature signified a foundational need for authentic co‐design with Aboriginal and Torres Strait Islander people in eHealth interventions.10,11,12,14,15,18,32,35,36,38,40,41,43,46,47,48,50,51,58,59,61,62 Authentic co‐design was understood as a process of collaborative development and trials of eHealth interventions where Aboriginal and Torres Strait Islander people were valued as instrumental leaders, reflecting the priorities and values of their communities. Sixteen articles11,12,35,36,37,38,39,40,44,48,51,55,58,59,61,62 also referred to the significance of Aboriginal and Torres Strait Islander governance and trusted partnerships in the development and trial of eHealth interventions. Aboriginal and Torres Strait Islander governance and authentic co‐design are thus considered essential for eHealth.
References to cultural safety were also consistent throughout the literature regarding the pragmatics of eHealth design, development and implementation with end users (subthemes 1–3).
Subtheme 1: eHealth setting underscored by trust
The setting in which eHealth interventions are developed and deployed with Aboriginal and Torres Strait Islander people must engender trust through organisational factors, communication, readiness and resourcing.12,14,15,18,31,32,33,34,37,38,39,40,41,42,43,44,45,46,47,49,50,51,52,56,57,58,59,61,62 The literature consistently referred to ACCHOs as culturally appropriate and relevant settings for eHealth.11,15,42,44,48,51,52,54,55,57,59,61,62 Further, service providers and end users need confidence that an eHealth platform is culturally safe and has capabilities appropriate to the health condition of interest. Box 6 presents a range of factors, that can help make eHealth business‐as‐usual so that Aboriginal and Torres Strait Islander people experience the value of innovation, such as enabling people to remain on Country, and provision of health care in a familiar, trusted environment. Health professionals and service providers must also recognise that eHealth has limitations and is not necessarily relevant with certain health conditions or settings.11,18,30,32,42,50,54,60
Subtheme 2: eHealth content responsive to audience
This subtheme recognises the variety of modalities deployed across the studies and considers the nature of the health information embedded within a users’ experience of eHealth. For example, content viewed during user interaction with a mobile application, or shared between a service provider and end user during a telehealth appointment. The literature signalled that eHealth content must be responsive to the intended audience to aid engagement — recognising diversity across users’ gender, age, culture, language, health literacy and location.11,12,14,33,35,36,37,38,39,40,41,48,50,51,53,54,55,59,61,62 Evidence‐based content was important33,34,35,40,48 and some users expressed the value of a journey or storytelling approach to health content.38,40,50,61 Additional influencers of engagement were visual elements,12,14,36,39,49,51,59,61 goal setting,10,59 bite‐size content,38,48 and concise, conversational language.35,38,40,48,50,61,62 Study participants reported that eHealth can create a safe, anonymous space11,39,40,41,48,50,62 for Aboriginal and Torres Strait Islander people to explore and learn more about health (encouraging agency), through strengths‐based content14,33,41,43,50,55,58,59 that was non‐judgemental and culturally relevant.
Subtheme 3: eHealth user engagement underscored by cultural values
Features of the eHealth product, including imagery, design and functionality, have an impact on user engagement and re‐engagement over the course of an intervention.12,14,32,33,35,36,38,39,40,47,48,49,55,59,61 eHealth participants expected user‐friendly and viable technology with offline capability, that was free of broken links, lengthy load times or glitches.11,35,38,39,40,48,59,61 Visual and audio features were reported as strong influencers for user engagement where cultural safety and relevance are paramount.12,32,33,35,36,38,39,40,47,48,49,55,59,61 User preferences included authentic Aboriginal and/or Torres Strait Islander art, flag colours, and visual characters that closely reflect the appearance and voices of Aboriginal and Torres Strait Islander people. Interactive features (eg, chat, gamification, incentives) and layouts that mimicked other popular platforms were appealing to users.12,14,38,39,47,48,59,61 eHealth development should include consultation with end users about modality, intervention frequency and duration.11,38,43,47,62
Principal findings
A literature search (to 2 December 2022) yielded 39 studies that underwent analysis of content and cultural quality to identify the important characteristics of eHealth with Aboriginal and Torres Strait Islander people. The key finding is that authentic co‐design, governance and strong partnerships are foundational qualities of eHealth that is culturally safe and sustainable for impact. Without these, eHealth interventions may not meet the priorities and values of the Aboriginal and Torres Strait Islander communities for which they are intended. Three subthemes identified from factors in the literature included eHealth setting underscored by trust, eHealth content responsive to audience, and eHealth user engagement underscored by cultural values. These themes provide insight into the pragmatic aspects of eHealth interventions, where service providers and end users are confident, supported and engaged, with effective and culturally safe modalities that enable two‐way health care interactions.
This review further verifies that co‐design with Aboriginal and Torres Strait Islander people must move well beyond tokenistic participation to authentic participatory action research (PAR). This is an essential distinction given that a 2021 scoping review63 reported a nominal alignment with PAR (or community engagement and leadership) in a review of chronic disease interventions (including eHealth) with Aboriginal and Torres Strait Islander populations, despite the researchers stating the importance of PAR, and implying they had incorporated PAR into their studies.
A secondary analysis of a randomised clinical trial64 also emphasised the need for research processes that account for the greater cultural context of a technological innovation.64 The authors noted a scarcity of relevant literature and reported their retrospective analysis of qualitative data collated during a five‐year randomised controlled mHealth trial with six diverse First Nations communities in Canada. Based on their findings and reflective practice, the authors proposed a set of “wise practices” for culturally safe eHealth research that included building and maintaining respectful relationships, as well as commitment to co‐designing the innovation.64 Authentic co‐design places people most affected by an intervention or service at the centre of that process, and is guided by their voices, values and experiences.65 Further, in a 2022 editorial,66 the authors assert that “… the engagement, involvement, and leadership of Indigenous and Tribal people is an essential requirement for ensuring that research is consistent with the rights of Indigenous and Tribal peoples (including the right to self‐determination)”.
Although previous reviews have offered global evidence about the value of collaborative approaches, authentic relationship building and co‐design with First Nations peoples,7,8,17,64 this narrative review positions authentic co‐design as a foundational approach — specific to Aboriginal and Torres Strait Islander people. This foundation of co‐design, encapsulating Aboriginal and Torres Strait Islander governance and strong partnerships, determines the pragmatic plans within subsequent stages of the eHealth intervention. This linkage strongly aligns with a key recommendation by national experts, led by Pat Dudgeon, regarding the potential for telehealth and other forms of eHealth to support mental health and wellbeing for Aboriginal and Torres Strait Islander people during the coronavirus disease 2019 (COVID‐19) pandemic. “Therefore, optimism is contingent on the adoption of best practice, including Indigenous governance and culturally safe services that accommodate models of cultural healing and holistic well‐being.”67
This narrative review emphasises the strengths of ACCHOs (and other community controlled Aboriginal and Torres Strait Islander organisations) as key entities with which strong partnerships and governance must be established. Despite most of the studies that partnered with ACCHOs scoring higher in the QAT analysis for cultural quality, further research will help establish the value and potential of these collaborations for eHealth. Not only do these organisations represent the voices and priorities of the communities they service, their holistic models of care are integral to closing the gap in health and social disparities between Aboriginal and Torres Strait Islander and non‐Indigenous people in Australia.16,68,69 Consequently, ACCHOs are a critical component of the supporting ecosystem for eHealth impact with Aboriginal and Torres Strait Islander people.
While the final iteration of the best practice framework is in development, we recommend from the outset that researchers and service providers undertake early planning for any health interventions with Aboriginal and Torres Strait Islander people and apply tools such as the QAT26,27 alongside an appropriate ethics review. Although intended as an appraisal tool, the QAT content was designed by, and with, the voices of Aboriginal and Torres Strait Islander peoples. Deeper analysis about a potential eHealth project, using the QAT prompts, will enhance the quality, relevance and benefits of intervention research to enhance community health and wellbeing.
Significantly higher cultural quality scores were achieved in studies that included more Aboriginal and Torres Strait Islander authors. This further underscores the key theme of this review. To achieve appropriate, high quality and relevant eHealth research with Aboriginal and Torres Strait Islander people, an authentic approach to governance and co‐design is essential. These findings indicate a direct correlation to the influence Aboriginal and Torres Strait Islander leadership and authorship has on beneficial and quality eHealth research, countering the long history of colonising health research.66
Future work by the Collaboration will continue the program of research previously outlined.16 Building on the key findings of this narrative review, modified‐Delphi processes with health and community stakeholders as well as national experts are being conducted to further establish the values and priorities of Aboriginal and Torres Strait Islander people in shaping a foundational eHealth best practice framework.
Strengths and limitations
This review was conducted according to the PRISMA 2020 statement.22 Two reviewers completed each stage of screening (GC, CM) and JBI LoE rankings (GC, LC). However, although pre‐analysis discussion and cross‐checks occurred, a portion of articles underwent single‐author QAT analysis. Author positionality of final articles was limited to desktop research and we thus acknowledge we may have missed some authors, given that, historically, scientific publications rarely provided an opportunity for Aboriginal and Torres Strait Islander authors to identify as such. Publication bias toward effective studies may have affected the identification of articles relating to eHealth with Aboriginal and Torres Strait Islander people. Further, it should be recognised that not all eHealth interventions used in practice would necessarily result in an academic publication, potentially leading to incomplete data about best practices. Further, with the evolving nature and breadth of eHealth modalities, the research team faced challenges in determining the pragmatic application of technology within some trials. Iterative discussions with principal researchers on the authorship team were used to reach consensus. The heterogeneity of eHealth modalities identified for this study meant that some findings regarding a modality (eg, mobile diagnostic tools) may only be supported by a small subset of studies and, hence, are likely to be underpowered.
Conclusion
This narrative review is fundamental to the development of a best practice framework for eHealth interventions with Aboriginal and Torres Strait Islander people for cultural safety, sustainability and impact.16 The need for a framework to guide researchers and service providers is driven by the ubiquitous presence of digital devices and the growth of eHealth across health settings.7,8,17,64 Content analysis of scientific literature asserts that authentic Aboriginal and Torres Strait Islander co‐design, governance and strong community partnerships are foundational qualities of culturally safe eHealth practice and research with Aboriginal and Torres Strait Islander people. With these foundations in place throughout the intervention lifespan, the pragmatics of eHealth including setting, content and user engagement, are more likely to meet the priorities and values of the Aboriginal and Torres Strait Islander people and communities for which they are intended.
Box 2 – Characteristics of studies that reported on eHealth interventions with Aboriginal and Torres Strait Islander people in Australia
|
|
|
Participants |
eHealth modality |
Study site* |
Joanna Briggs Institute Levels of Evidence |
Quality Appraisal Tool score† |
|||||||||
|
Study (year) |
Focus of intervention |
Aboriginal and Torres Strait Islander |
Role |
||||||||||||
|
|
|||||||||||||||
|
Amos (2022)30 |
Mental health and social emotional wellbeing |
36 |
Clients |
Telehealth |
Far North and Central West, QLD |
4 |
0 |
||||||||
|
Ashman (2017)31 |
Maternal and infant care |
8 |
Participants |
mHealth |
Tamworth and Newcastle, NSW |
2 |
2 |
||||||||
|
Bennett‐Levy (2017)‡,32 |
Mental health and social emotional wellbeing |
21 |
Health professionals (health worker, youth worker, family wellbeing coordinator) |
Multiple |
North NSW |
3 |
7 |
||||||||
|
Bird (2017)33 |
Mental health and social emotional wellbeing |
15 |
Service providers |
Multiple |
North NSW |
3 |
5 |
||||||||
|
Caffery (2018)‡,15 |
Health care access |
9 |
Health workers |
Telehealth |
Western QLD |
3 |
0 |
||||||||
|
Cashman (2016)34 |
Maternal and infant care |
89 |
Infants and parents |
Telehealth |
Hunter New England, NSW |
3 |
12§ |
||||||||
|
Clark (2015)‡,35 |
Chronic disease management and education |
5 |
Patients |
mHealth |
Ipswich, QLD |
2 |
10§ |
||||||||
|
Davies (2015)‡,36 |
Chronic disease management and education |
27 |
Patients and health workers |
mHealth |
Arnhem Land, NT |
2 |
9 |
||||||||
|
Dingwall (2021)37 |
Mental health and social emotional wellbeing |
156 |
Patients |
mHealth |
Alice Springs and Darwin, NT |
1 |
7 |
||||||||
|
Fletcher (2017)‡,12 |
Maternal and infant care |
20 |
Patients |
mHealth |
Regional, NSW |
4 |
12§ |
||||||||
|
Kennedy (2021)‡,38 |
Maternal and infant care |
35 |
Participants |
mHealth |
Newcastle, NSW |
3 |
11§ |
||||||||
|
Lee (2018)‡,40 |
Screening: substance use |
44 |
Patients and health workers |
mHealth |
QLD, NSW, SA and VIC |
4 |
10§ |
||||||||
|
Lee (2021)‡,39 |
Screening: substance use |
(i) 246, (ii) 5 |
(i) Patients, (ii) field researchers |
mHealth |
Regional SA and urban QLD |
3 |
9§ |
||||||||
|
Macniven (2019)‡,41 |
Screening: cardiac |
18 |
ACCHO staff |
Mobile diagnostic tool |
Urban, regional and remote, NT, WA and NSW |
3 |
12§ |
||||||||
|
Martin (2017)42 |
Healthy behaviour promotion |
24 |
Health workers |
Telehealth |
SA |
3 |
6§ |
||||||||
|
Maxwell (2021)43 |
Healthy behaviour promotion |
8 |
Participants |
mHealth |
Sydney, NSW |
3 |
4 |
||||||||
|
McCallum (2014)44 |
Chronic disease management |
186 |
Families of patients |
mHealth |
Darwin, NT, and Townsville, QLD |
4 |
2§ |
||||||||
|
McPhail‐Bell (2018)‡,14 |
Healthy behaviour promotion |
Unspecified |
Social media users |
Social media |
Southeast, QLD |
3 |
9§ |
||||||||
|
Mooi (2012)45 |
Health care access |
9 |
Patients |
Telehealth |
Townsville and remote QLD |
3 |
0 |
||||||||
|
Nagel (2022)‡,10 |
Mental health and social emotional wellbeing |
147 |
Patients |
mHealth |
Alice Springs and Darwin, NT |
3 |
12 |
||||||||
|
Noble (2014)‡,46 |
Screening: health risk factors |
135 |
Patients |
mHealth |
Regional NSW |
4 |
1 |
||||||||
|
Peiris (2019)‡,47 |
Healthy behaviour promotion |
49 |
Participants |
mHealth |
NSW |
1 |
9 |
||||||||
|
Perkes (2022)‡,48 |
Maternal and infant care |
(i) 4, (ii) 31 |
(i) Health professionals, (ii) carers, children, pregnant women |
mHealth |
Coffs Harbour, Newcastle and Inverell, NSW |
4 |
9§ |
||||||||
|
Phillips (2014)49 |
Health care access |
53 |
Parents of children |
mHealth |
Remote NT |
1 |
1 |
||||||||
|
Povey (2016)50 |
Mental health and social emotional wellbeing |
8 |
Community members |
mHealth |
Darwin, NT |
3 |
9§ |
||||||||
|
Quinn (2017)‡,51 |
Healthy behaviour promotion |
1462 |
Participants |
Telehealth |
NSW |
2 |
9 |
||||||||
|
Raphiphatthana (2020)‡,18 |
Mental health and social emotional wellbeing |
65 |
Health professionals from primary health care |
mHealth |
Darwin and Alice Springs, NT, and Adelaide, SA |
3 |
2 |
||||||||
|
Roberts (2015)52 |
Health care access |
5 |
Participants |
Telehealth |
Darwin, NT |
4 |
1 |
||||||||
|
Sabesan (2012)53 |
Health care access |
18 |
Patients |
Telehealth |
Townsville and Mt Isa, QLD |
4 |
1 |
||||||||
|
Shanley (2004)54 |
Caregiver support |
(i) 4–6, (ii) 1 |
(i) Carers, (ii) health workers |
Telehealth |
NSW |
3 |
0 |
||||||||
|
Snijder (2021)‡,55 |
Substance use |
41 |
Children |
mHealth |
NSW and QLD |
4 |
12§ |
||||||||
|
Spaeth (2016)56 |
Chronic disease management |
> 900 patients |
4 Case studies |
Mobile diagnostic tool |
NT |
4 |
1 |
||||||||
|
Spurling (2021)‡,57 |
Screening: auditory |
(i) 50, (ii) 9 |
(i) Children, (ii) caregivers |
mHealth |
Inala, QLD |
3 |
9 |
||||||||
|
Tighe (2017)‡,58 |
Mental health and social emotional wellbeing |
61 |
Participants |
mHealth |
Kimberley, WA |
1 |
9 |
||||||||
|
Tighe (2020)‡,11 |
Mental health and social emotional wellbeing |
13 |
Participants |
mHealth |
Kimberley, WA |
3 |
11 |
||||||||
|
Tonkin (2017)‡,59 |
Healthy behaviour promotion |
20 |
Participants |
mHealth |
Remote NT |
3 |
6 |
||||||||
|
Veinovic (2022)‡,60 |
Screening: cognitive |
20 |
Participants |
Telehealth |
Urban and regional NSW |
2 |
10§ |
||||||||
|
Versteegh (2022)‡,61 |
Chronic disease management and education |
80 |
Carers of children |
mHealth |
NT and QLD |
2 |
10 |
||||||||
|
Waller (2022)‡,62 |
Chronic disease management and education |
20 |
Participants |
mHealth |
Illawarra, NSW |
2 |
10 |
||||||||
|
|
|||||||||||||||
|
ACCHO = Aboriginal Community Controlled Health Organisation; mHealth = mobile health; NSW = New South Wales; NT = Northern Territory; QLD = Queensland; SA = South Australia; VIC = Victoria; WA = Western Australia. * States and regions in Australia for eHealth interventions with Aboriginal and Torres Strait Islander people. Regions were not identified in all studies. † Application of the Aboriginal and Torres Strait Islander Quality Appraisal Tool.26,27 ‡ The study involved an Aboriginal and/or Torres Strait Islander Community Controlled Organisation. § The study included two or more Aboriginal and Torres Strait Islander authors. |
|||||||||||||||
Box 3 – Aboriginal and Torres Strait Islander Quality Appraisal Tool (QAT) score26,27 versus the number of Aboriginal and Torres Strait Islander authors for included studies
Box 4 – Composite strengths and areas for improvement of final studies after application of the Aboriginal and Torres Strait Islander Quality Appraisal Tool (QAT)26,27
Box 5 – Frequency table for Aboriginal and Torres Strait Islander authors and Quality Appraisal Tool26,27 scores
|
|
Quality Appraisal Tool scores |
||||||||||||||
|
≥ 9 |
≤ 8 |
Total |
|||||||||||||
|
|
|||||||||||||||
|
Number of Aboriginal and Torres Strait Islander authors |
|
|
|
||||||||||||
|
≥ 2 |
12 (85.7%) |
2 (14.3%) |
14 |
||||||||||||
|
< 2 |
8 (32%) |
17 (68%) |
25 |
||||||||||||
|
Total |
20 (51.3%) |
19 (48.7%) |
39 |
||||||||||||
|
Odds ratio |
|
|
12.749 |
||||||||||||
|
P value |
|
|
0.0036 |
||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
- Georgina R Chelberg1,2
- Andrew Goodman1
- Charankarthi Musuwadi1
- Sheleigh Lawler3
- Liam J Caffery4
- Ray Mahoney1
- the eHRCATSIH Group
- 1 Australian eHealth Research Centre, Commonwealth Scientific and Industrial Research Organisation (CSIRO), Brisbane, QLD
- 2 Centre for Ageing Research and Translation, University of Canberra, Canberra, ACT
- 3 University of Queensland, Brisbane, QLD
- 4 Centre for Online Health, Centre for Health Services Research, University of Queensland, Brisbane, QLD
This research has governance from an existing multiagency research partnership, the eHealth Research Collaboration for Aboriginal and Torres Strait Islander Health that was established in 2019. The research activities of the Collaboration are financially supported by CSIRO. We thank the following members of the Collaboration for their contributions to this manuscript: Kaley Butten (Australian eHealth Research Centre, Commonwealth Scientific and Industrial Research Organisation), Danielle Gallegos (Queensland University of Technology), Steven McPhail (Australian Centre for Health Services Innovation, and Centre for Healthcare Transformation, Queensland University of Technology), Courtney Ryder (Flinders University), and Marlien Varnfield (Australian eHealth Research Centre, Commonwealth Scientific and Industrial Research Organisation).
A member of the Collaboration, Danielle Gallegos, is supported by the Queensland Children's Hospital via a philanthropic grant from Woolworths.
- 1. Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform 2010; 79: 736‐771.
- 2. Free C, Phillips G, Galli L, et al. The effectiveness of mobile‐health technology‐based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med 2013; 10: e1001362.
- 3. Peiris D, Praveen D, Johnson C, Mogulluru K. Use of mHealth systems and tools for non‐communicable diseases in low‐ and middle‐income countries: a systematic review. J Cardiovasc Transl Res 2014; 7: 677‐691.
- 4. Hall AK, Cole‐Lewis H, Bernhardt JM. Mobile text messaging for health: a systematic review of reviews. Annu Rev Public Health 2015; 36: 393‐415.
- 5. Snoswell CL, Caffery LJ, Haydon HM, et al. A cost‐consequence analysis comparing patient travel, outreach, and telehealth clinic models for a specialist diabetes service to Indigenous people in Queensland. J Telemed Telecare 2019; 25: 537‐544.
- 6. Backholer K, Browne J, Wright A, et al. Digital determinants of health: the digital transformation. Med J Aust 2021; 214(Suppl): S32‐S35. https://www.mja.com.au/system/files/2021‐05/MJA%20supplement_214_8_3%20May.pdf
- 7. Jones L, Jacklin K, O'Connell ME. Development and use of health‐related technologies in Indigenous communities: critical review. J Med Internet Res 2017; 19: e256.
- 8. Hobson GR, Caffery LJ, Neuhaus M, Langbecker DH. Mobile health for First Nations populations: systematic review. JMIR Mhealth and Uhealth 2019; 7: e14877.
- 9. Reilly R, Stephens J, Micklem J, et al. Use and uptake of web‐based therapeutic interventions amongst Indigenous populations in Australia, New Zealand, the United States of America and Canada: a scoping review. Syst Rev 2020; 9: 1‐17.
- 10. Nagel T, Dingwall KM, Sweet M, et al. The stay strong app as a self‐management tool for first nations people with chronic kidney disease: a qualitative study. BMC Nephrol 2022; 23: 244.
- 11. Tighe J, Shand F, McKay K, et al. Usage and acceptability of the iBobbly app: pilot trial for suicide prevention in Aboriginal and Torres Strait Islander youth. JMIR Ment Health 2020; 7: e14296.
- 12. Fletcher R, Hammond C, Faulkner D, et al. Stayin’ on Track: the feasibility of developing Internet and mobile phone‐based resources to support young Aboriginal fathers. Aust J Primary Health 2017; 23: 329‐334.
- 13. Haydon HM, Caffery LJ, Snoswell CL, et al. Dementia ECHO: evaluation of a telementoring programme to increase dementia knowledge and skills in First Nations‐led health services. J Telemed Telecare 2022; 28: 757‐763.
- 14. McPhail‐Bell K, Appo N, Haymes A, et al. Deadly Choices empowering Indigenous Australians through social networking sites. Health Promot Int 2018; 33: 770‐780.
- 15. Caffery LJ, Bradford NK, Smith AC, Langbecker D. How telehealth facilitates the provision of culturally appropriate healthcare for Indigenous Australians. J Telemed Telecare 2018; 24: 676‐682.
- 16. Chelberg GR, Butten K, Mahoney R; eHealth Research Collaboration for Aboriginal and Torres Strait Islander Health. Culturally safe eHealth interventions with Aboriginal and Torres Strait Islander people: protocol for a best practice framework. JMIR Res Protoc 2022; 11: e34904.
- 17. Goodman A, Mahoney R, Spurling G, Lawler S. Influencing factors to mHealth uptake with Indigenous populations: qualitative systematic review. JMIR Mhealth Uhealth 2023; 11: e45162.
- 18. Raphiphatthana B, Sweet M, Puszka S, et al. Evaluation of a three‐phase implementation program in enhancing e‐mental health adoption within Indigenous primary healthcare organisations. BMC Health Serv Res 2020; 20: 576.
- 19. Dingwall KM, Puszka S, Sweet M, et al. Evaluation of a culturally adapted training course in Indigenous e‐mental health. Australas Psychiatry 2015; 23: 630‐635.
- 20. Dingwall KM, Puszka S, Sweet M, Nagel T. “Like drawing into sand”: acceptability, feasibility, and appropriateness of a new e‐Mental health resource for service providers working with Aboriginal and Torres Strait Islander people. Australian Psychologist 2015; 50: 60‐69.
- 21. Fraser S, Mackean T, Grant J, et al. Use of telehealth for health care of Indigenous peoples with chronic conditions: a systematic review. Rural Remote Health 2017; 17: 4205.
- 22. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71.
- 23. Tieman JJ, Lawrence MA, Damarell RA, et al. LIt.search: fast tracking access to Aboriginal and Torres Strait Islander health literature. Aust Health Rev 2014; 38: 541‐545.
- 24. Joanna Briggs Institute. Critical appraisal tools. Adelaide: JBI, 2018. http://jbi.global/critical‐appraisal‐tools (viewed Jan 2024).
- 25. Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. Supporting document for the Joanna Briggs Institute Levels of Evidence and Grades of Recommendation. Adelaide: JBI, 2014. https://jbi.global/sites/default/files/2019‐05/JBI%20Levels%20of%20Evidence%20Supporting%20Documents‐v2.pdf (viewed Jan 2024).
- 26. Harfield S, Pearson O, Morey K, et al. The Aboriginal and Torres Strait Islander Quality Appraisal Tool: companion document. Adelaide: South Australian Health and Medical Research Institute and University of Adelaide, 2018. https://sahmri.blob.core.windows.net/communications/Aboriginal‐and‐Torres‐Strait‐Islander‐Quality‐Appraisal‐Tool‐Companion‐Document‐1.pdf (viewed Jan 2024).
- 27. Harfield S, Pearson O, Morey K, et al. Assessing the quality of health research from an Indigenous perspective: the Aboriginal and Torres Strait Islander quality appraisal tool. BMC Med Res Methodol 2020; 20: 79.
- 28. Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open 2016; 2: 8‐14.
- 29. Huria T, Palmer SC, Pitama S, et al. Consolidated criteria for strengthening reporting of health research involving Indigenous peoples: the CONSIDER statement. BMC Med Res Methodol 2019; 19: 173.
- 30. Amos AJ, Middleton J, Gardiner FW. Remote mental health clients prefer face‐to‐face consultations to telehealth during and after the COVID‐19 pandemic. Australas Psychiatry 2022; 30: 18‐22.
- 31. Ashman AM, Collins CE, Brown LJ, et al. Validation of a smartphone image‐based dietary assessment method for pregnant women. Nutrients 2017; 9: 73.
- 32. Bennett‐Levy J, Singer J, DuBois S, Hyde K. Translating e‐Mental health into practice: what are the barriers and enablers to e‐Mental health implementation by Aboriginal and Torres Strait Islander health professionals? J Med Internet Res 2017; 19: e1.
- 33. Bird J, Rotumah D, Bennett‐Levy J, Singer J. Diversity in eMental health practice: an exploratory qualitative study of Aboriginal and Torres Strait Islander service providers. JMIR Ment Health 2017; 4: e17.
- 34. Cashman PM, Allan NA, Clark KK, et al. Closing the gap in Australian Aboriginal infant immunisation rates — the development and review of a pre‐call strategy. BMC Public Health 2016; 16: 514.
- 35. Clark RA, Fredericks B, Buitendyk NJ, et al. Development and feasibility testing of an education program to improve knowledge and self‐care among Aboriginal and Torres Strait Islander patients with heart failure. Rural Remote Health 2015; 15: 3231.
- 36. Davies J, Bukulatjpi S, Sharma S, et al Development of a culturally appropriate bilingual electronic app about hepatitis B for Indigenous Australians: towards shared understandings. JMIR Res Protoc 2015; 4: e70.
- 37. Dingwall KM, Sweet M, Cass A, et al. Effectiveness of wellbeing intervention for Chronic Kidney Disease (WICKD): results of a randomised controlled trial. BMC Nephrol 2021; 22: 136.
- 38. Kennedy M, Kumar R, Ryan NM, et al. Codeveloping a multibehavioural mobile phone app to enhance social and emotional well‐being and reduce health risks among Aboriginal and Torres Strait Islander women during preconception and pregnancy: a three‐phased mixed‐methods study. BMJ Open 2021; 11: e052545.
- 39. Lee KK, Conigrave JH, Al Ansari M, et al. Acceptability and feasibility of a computer‐based application to help Aboriginal and Torres Strait Islander Australians describe their alcohol consumption. J Ethn Subst Abuse 2021; 20: 16‐33.
- 40. Lee KSK, Wilson S, Perry J, et al. Developing a tablet computer‐based application (‘App’) to measure self‐reported alcohol consumption in Indigenous Australians. BMC Med Inform Decis Mak 2018; 18: 8.
- 41. Macniven R, Gwynn J, Fujimoto H, et al. Feasibility and acceptability of opportunistic screening to detect atrial fibrillation in Aboriginal adults. Aust N Z J Public Health 2019; 43: 313‐318.
- 42. Martin K, Dono J, Rigney N, et al. Barriers and facilitators for health professionals referring Aboriginal and Torres Strait Islander tobacco smokers to the Quitline. Aust N Z J Public Health 2017; 41: 631‐634.
- 43. Maxwell H, O'Shea M, Stronach M, Pearce S. Empowerment through digital health trackers: an exploration of Indigenous Australian women and physical activity in leisure settings. Annals of Leisure Research 2021; 24: 150‐167.
- 44. McCallum GB, Versteegh LA, Morris PS, et al. Mobile phones support adherence and retention of Indigenous participants in a randomised controlled trial: strategies and lessons learnt. BMC Public Health 2014; 14: 622.
- 45. Mooi JK, Whop LJ, Valery PC, Sabesan SS. Teleoncology for Indigenous patients: the responses of patients and health workers. Aust J Rural Health 2012; 20: 265‐269.
- 46. Noble NE, Paul CL, Carey ML, et al. A cross‐sectional survey assessing the acceptability and feasibility of self‐report electronic data collection about health risks from patients attending an Aboriginal Community Controlled Health Service. BMC Med Inform Decis Mak 2014; 14: 34.
- 47. Peiris D, Wright L, News M, et al. A smartphone app to assist smoking cessation among Aboriginal Australians: findings from a pilot randomized controlled trial. JMIR Mhealth Uhealth 2019; 7: e12745.
- 48. Perkes SJ, Huntriss B, Skinner N, et al. Development of a maternal and child mHealth intervention with Aboriginal and Torres Strait Islander mothers: co‐design approach. JMIR Form Res 2022; 6: e33541.
- 49. Phillips JH, Wigger C, Beissbarth J, et al. Can mobile phone multimedia messages and text messages improve clinic attendance for Aboriginal children with chronic otitis media? A randomised controlled trial. J Paediatr Child Health 2014; 50: 362‐367.
- 50. Povey J, Mills PP, Dingwall KM, et al. Acceptability of mental health apps for Aboriginal and Torres Strait Islander Australians: a qualitative study. J Med Internet Res 2016; 18: e65.
- 51. Quinn E, O'Hara BJ, Ahmed N, et al. Enhancing the get healthy information and coaching service for Aboriginal adults: evaluation of the process and impact of the program. Int J Equity Health 2017; 16: 168.
- 52. Roberts S, Spain B, Hicks C, et al. Telemedicine in the Northern Territory: an assessment of patient perceptions in the preoperative anaesthetic clinic. Aust J Rural Health 2015; 23: 136‐141.
- 53. Sabesan S, Larkins S, Evans R, et al. Telemedicine for rural cancer care in North Queensland: bringing cancer care home. Aust J Rural Health 2012; 20: 259‐264.
- 54. Shanley C, Roddy M, Cruysmans B, Eisenberg M. The humble telephone: a medium for running carer support groups. Australas J Ageing 2004; 23: 82‐85.
- 55. Snijder M, Stapinski L, Ward J, et al. Strong and deadly futures: co‐development of a web‐based wellbeing and substance use prevention program for Aboriginal and Torres Strait Islander and non‐Aboriginal adolescents. Int J Environ Res Public Health 2021; 18: 2176.
- 56. Spaeth BA, Shephard MDS. Clinical and operational benefits of international normalized ratio point‐of‐care testing in remote Indigenous communities in Australia's Northern Territory. Point Care 2016; 15: 30‐34.
- 57. Spurling GK, Tyson C, Askew D, Reath J. Mixed‐methods evaluation of screening for hearing loss using the hearScreen™ mobile health application in Aboriginal and Torres Strait Islander children presenting to an urban primary healthcare service. Aust J Prim Health 2021; 27: 371‐376.
- 58. Tighe J, Shand F, Ridani R, et al. Ibobbly mobile health intervention for suicide prevention in Australian Indigenous youth: a pilot randomised controlled trial. BMJ Open 2017; 7: e013518.
- 59. Tonkin E, Jeffs L, Wycherley TP, et al. A smartphone app to reduce sugar‐sweetened beverage consumption among young adults in Australian remote Indigenous communities: design, formative evaluation and user‐testing. JMIR Mhealth Uhealth 2017; 5: e192.
- 60. Veinovic M, Hill TY, Lavrencic L, et al. Telephone cognitive screening with older Aboriginal Australians: a preliminary study. Australas J Ageing 2023; 42: 311‐316.
- 61. Versteegh LA, Chang AB, Chirgwin S, et al. Multi‐lingual “Asthma APP” improves health knowledge of asthma among Australian First Nations carers of children with asthma. Front Pediatr 2022; 10: 925189.
- 62. Waller K, Furber S, Bauman A. Acceptability, feasibility and preliminary impact evaluation of a pilot text‐message study on improving the health of Aboriginal people with, or at risk of, chronic disease in Australia. Health Promot J Austr 2023; 34: 24‐29.
- 63. Wali S, Superina S, Mashford‐Pringle A, et al. What do you mean by engagement? — evaluating the use of community engagement in the design and implementation of chronic disease‐based interventions for Indigenous populations — scoping review. Int J Equity Health 2021; 20: 8.
- 64. Maar MA, Beaudin V, Yeates K, et al. Wise practices for cultural safety in electronic health research and clinical trials with Indigenous people: secondary analysis of a randomized clinical trial. J Med Internet Res 2019; 21: e14203.
- 65. Clarence C. Reflective resource: how ready are you to embark on an authentic co‐design process? Adelaide: Australian Centre for Social Innovation, 2022. https://www.tacsi.org.au/news‐ideas/how‐ready‐are‐you‐to‐embark‐on‐an‐authentic‐co‐design‐process‐prompt‐book (viewed Jan 2024).
- 66. Griffiths K, Diaz A, Whop LJ, Cunningham J. The health and wellbeing of indigenous and tribal peoples around the globe: ensuring and promoting best practice in research. Int J Environ Res Public Health 2022; 19: 261.
- 67. Dudgeon P, Alexi J, Derry K, et al. Mental health and well‐being of Aboriginal and Torres Strait Islander peoples in Australia during COVID‐19. Aust J Soc Issues 2021; 56: 485‐502.
- 68. National Aboriginal Community Controlled Health Organisation. Who we are. Canberra: NACCHO, 2022. https://www.naccho.org.au/about‐us/ (viewed Jan 2024).
- 69. National Aboriginal Health Strategy Working Party. A national Aboriginal health strategy. Canberra: Australian Government Department of Aboriginal Affairs, 1989. https://aodknowledgecentre.ecu.edu.au/key‐resources/policies‐and‐strategies/10967/?title=A+national+Aboriginal+health+strategy&contentid=10967_1 (viewed Jan 2024).






Summary