The known: Mental ill‐health is common in resident physicians. The behaviour of supervisors influences the mental health of their staff and can be improved by skills‐based mental health training.
The new: A brief online mental health training program for physician supervisors in Australia and New Zealand was associated with increases in self‐reported behaviour that is recommended for supporting the mental health of resident physicians.
The implications: Simple training programs for senior physicians can change self‐reported behaviour that may support the mental health of their staff. The impact of these changes on the psychosocial wellbeing of resident physicians should be investigated.
Rates of mental ill health and suicide are higher among resident physicians1,2,3 than in other professions and among more experienced doctors;2 about one in three physicians report symptoms of mental ill health during residency.1,2,3,4 The high level of psychological illness, often compounded by a reluctance to seek help,5 may increase the risk of medical errors.6
Working conditions influence the mental health of physicians; the risk of depression, anxiety, and suicidal ideation is twice as high for junior doctors working 55 or more hours per week as for those working 40–44 hours per week.7 Further, few uninterrupted breaks, making decisions under pressure, sleep deprivation, job insecurity, and working while needing to pass vital exams can amplify mental health problems.7,8,9 Protecting and promoting physician mental health with programs based on evidence‐informed workplace mental health frameworks are consequently critical.10,11
World Health Organization guidelines regarding mental health at work recommend evidence‐based manager training for employee wellbeing.12 As supportive supervisors are associated with lower levels of psychological distress in employees,8,13 improving supervisory behaviour with evidence‐based interventions is important.8,14 Studies in work environments with high risk of psychological distress have found that managers who completed mental health training had increased confidence and adopted recommended behaviours for supporting the mental health of their staff.15,16,17
We undertook a randomised controlled trial to rigorously evaluate training specifically designed for physician supervisors with the aim of promoting a mentally healthy workplace by improving supervisors’ use of both responsive strategies that support workers experiencing mental ill health, and preventive strategies that minimise work‐related psychosocial risks.
Methods
We undertook a cluster randomised waitlist‐controlled trial. Physicians were eligible to participate if they were current fellows of the Royal Australasian College of Physicians (RACP), lived in Australia or New Zealand, and supervised at least one resident physician. In Australia, a resident physician has completed their medical internship and holds general registration with the Medical Board of Australia. The trial was registered with the Australian New Zealand Clinical Trials Registry before recruitment commenced (ACTRN12619001496101; 29 October 2019). We report our study in accordance with the CONSORT statement.18
Intervention
In partnership with the RACP, a previously evaluated manager training program15,16 was adapted for physician supervisors. The tailored program comprised twelve modules grouped into three topics: common mental illnesses; helping trainees you are concerned about (responsive strategies); and minimising mental health risks at work (preventive strategies). The program was delivered online and included activities, case studies, videos, and podcasts. A pilot study ensured that the content met the needs of physician supervisors.17
Procedure
Clusters were defined by geographic health networks (all 31 primary health networks in Australia, and all 20 district health boards in New Zealand) to reduce the risk of contamination between the intervention and control groups. Clusters were stratified by the median number of physician supervisors in the health network; stratified clusters were randomly allocated to the intervention or control group using the RAND function in Excel (Microsoft), separately for Australian and New Zealand clusters.
All 2467 RACP fellows were invited by email to participate in a trial evaluating an online educational program for improving mental health in the workplace. Two email reminders, communications from the RACP president, and RACP eBulletin advertisements were disseminated between during the recruitment period (11 November 2019 – 11 February 2020) to prompt participation.
Recruitment materials directed participants to the online participant information statement and consent form. After completing the online baseline questionnaire, physicians allocated to the intervention group had three weeks to complete the training. Training was expected to take 2.0 to 2.5 hours, and participants received a follow‐up questionnaire after completing training. Physicians who did not complete the training and participants in the control group received the follow‐up survey three weeks after the baseline questionnaire. All participants were contacted by email for 3‐ and 6‐month follow‐up surveys (questionnaire for all time points: Supporting Information). Physicians in both trial groups received unrestricted access to the program after they had completed the final survey. Recruitment ceased on 11 February 2020; data collection was completed on 21 August 2020.
Primary outcome
The primary outcome was the change between baseline and the 3‐month assessment in self‐reported supervisor behaviours that promote a mentally healthy workplace. This outcome was also assessed immediately at the end of the intervention or three weeks after the baseline questionnaire if training was not completed (post‐training/3‐week assessment) and six months after the intervention. We selected the start of a new teaching term for commencing training and three months for the primary follow‐up assessment point to capture data on manager behaviour for a single cohort of resident physicians. Self‐reported manager behaviour was assessed with a 15‐item scale previously used to assess mental health interventions for managers.16 For each item, physician supervisors rated their agreement (from 1, strongly disagree to 5, strongly agree; overall score range: 15–75; higher scores reflect more positive behaviour). The scale included two subscales: six items that described responsive behaviours, including “I initiate a conversation with individuals I supervise about their mental health and wellbeing” (score range, 6–30), and nine items that described preventive behaviours that minimise workplace mental health risks, including “I monitor my trainee's workload on an ongoing basis” (score range, 9–45).
Secondary outcomes
Supervisors’ confidence in supporting the mental health of physician trainees was assessed with a scale used in earlier trials of manager training.15,16 Physicians rated their level of confidence (from 1, not at all confident to 5, extremely confident) in dealing with each of six mental health scenarios they might encounter as supervisors (score range, 6–30; higher scores indicate more confidence; Cronbach alpha: 0.89). Psychological distress was assessed with the Kessler Psychological Distress Scale (K6; score range, 5–30; Cronbach alpha: 0.83; inadvertently omitted from trial protocol).19 Stigmatising attitudes regarding mental health were assessed with a 10‐item scale used for evaluating manager training;15 physicians rated their level of agreement, from 1, strongly agree to 5, strongly disagree (score range, 10–50); a lower score indicated lower levels of stigmatisation. Mental health knowledge was assessed with an adapted version of the Mental Health Knowledge Schedule (MAKS; 1, strongly disagree to 5, strongly agree; score range, 6–30);16,20 the 22‐item measure described in the study protocol was not used.
Data on demographic characteristics (age category, gender) and durations of employment at current hospital and in a supervisory role were also collected.
Statistical analysis
Statistical power analysis determined that 208 participants (104 per group) would be needed to detect an effect size of 0.4 standard deviations (SDs) (80% power; α = 0.05), assuming 20% loss to follow‐up, a mean of four participating physicians per cluster, and an intra‐cluster correlation coefficient (ICC) of 0.01. The predicted effect size and ICC assumed were based on an earlier randomised controlled trial of manager training.15
We undertook intention‐to‐treat analyses that included all participant data, irrespective of intervention adherence. For continuous outcomes, including the primary outcome, we undertook a mixed model repeated measures analysis (α = 0.05, a priori). Assessment (baseline, post‐training/3‐week, 3‐ and 6‐month follow‐up) was a within‐groups factor, and trial group (intervention, control) a between‐groups factor. Clusters were modelled as random intercepts. We used an unstructured variance covariance matrix to accommodate within‐participant dependency and assumed missing data to be missing at random. The primary outcome was assessed with a test of interaction between group and time. Planned contrasts were used to estimate intervention effects by calculating mean differences between groups in change from baseline at the post‐training/3‐week and 3‐month assessments, based on t tests with denominator degrees of freedom specified by the Kenward–Roger approximation. The ICC was calculated, and the statistical significance of clustering assessed in a likelihood ratio test (χ2 test) that compared models with and without the cluster random intercept.
Most analyses were conducted in SPSS 28; analyses of differences within baseline data were conducted in STATA/SE 17. As all data were collected online, the statistician performing the analysis was blind to treatment allocation.
Ethics approval
The University of New South Wales Human Research Ethics Committee approved the study (HC190628).
Results
Of the 2467 physicians invited, 209 (8.5%) consented to participate, and 178 (7.2%) met our eligibility criteria and completed the baseline questionnaire. Ninety physicians from twenty health network clusters were allocated to the intervention group (mean, 4.5 [SD, 3.1] physicians/cluster), 88 physicians from 22 clusters were allocated to the control group (mean, 4.0 [SD, 2.6] physicians/cluster) (Box 1). The characteristics of the two groups were broadly similar (Box 2).
The proportions of participants who did not fully complete the post‐training/3‐week questionnaire were similar for the intervention (28 physicians, 31%) and control groups (21 physicians, 24%; P = 0.28); the proportions who did not fully complete the 3‐month (41 physicians, 46% v 26 physicians, 30%; P = 0.035) and 6‐month assessments (44 physicians, 49% v 28 physicians, 32%; P = 0.021) were larger for the intervention than the control group (Box 1). No harm or unintended effects during the trial were reported.
Primary outcome
The participants in the intervention group reported more positive change in their behaviour across the study period than those in the control group (mixed model repeated measures analysis, group × time interaction: P < 0.001) (Box 3). The modelled mean difference between groups in change in self‐reported supervisory behaviour score at the post‐training/3‐week assessment was 1.6 (95% confidence interval [CI], 0.8–2.4) points, at the 3‐month assessment it was 0.9 (95% CI, 0.2–1.6) points, and at the 6‐month assessment it was 1.9 (95% CI, 1.1–2.7) points. The mean change in self‐reported responsive behaviour score was also greater for the intervention group: the modelled mean difference at the post‐training/3‐week assessment was 2.3 (95% CI, 1.5–3.1) points, at the 3‐month assessment 1.0 (95% CI, 0.2–1.9) points, and at the 6‐month assessment 2.0 (95% CI, 1.1–2.9) points. The mean difference in change in protective behaviour score was statistically significant at the post‐training/3‐week assessment (mean difference, 1.1 points; 95% CI, 0.1–2.2 points) and the 6‐month assessment (mean difference, 1.8 points; 95% CI, 0.8–2.8 points), but not at the 3‐month assessment (mean difference, 0.8 points; 95% CI, –0.1 to 1.7 points) (Box 4).
The ICC for behaviour at the 3‐month follow‐up was 0.11 (95% CI, –0.03 to 0.25; P = 0.13). Assessment of residuals in the primary outcome models found no evidence of substantial deviation from normality.
Secondary outcomes
The mean change in self‐reported confidence in supporting their trainees’ mental health was greater for the intervention than the control group at the post‐training/3‐week assessment (mean difference, 3.4; 95% CI, 2.4–4.5) and 3‐month assessment (mean difference, 2.5 points; 95% CI, 1.4–3.6 points), as was mean change in mental health knowledge at the post‐training/3‐week assessment (mean difference, 1.4 points; 95% CI, 0.7–2.1 points), but not at the 3‐month follow‐up (mean difference, 0.7 points; 95% CI, –0.4 to 1.5 points). The mean change in stigmatising attitudes regarding mental health care was greater in the intervention group than the control group at the 3‐month assessment (mean difference, –1.9 points; 95% CI, –3.1 to –0.6 points). Mean differences between the intervention and control groups in changes in physicians’ level of psychological distress were not statistically significant at either assessment (Box 5).
Discussion
Given the high rates of mental ill health and suicide among junior doctors,8 evidence‐based workplace interventions that better support the mental health of doctors in training are urgently needed. We undertook the first randomised controlled trial of training for physician supervisors for improving their support of the mental health of resident physicians. Our findings suggest that tailored online training can improve physicians’ self‐reported supervisory behaviour, as assessed immediately after the intervention and three and six months later. Participating in the skills‐based program improved physicians’ perceptions of their responsive strategies, such as initiating conversations with residents about their mental health, promoting help‐seeking, and facilitating their return to work after an absence for mental health reasons. Improved preventive behaviour was also reported.
The implications of our findings depend on the likely impact of the reported changes in physician supervisor behaviour on resident physicians’ mental health. As we did not assess it, we cannot definitively answer the question. However, when our findings are considered together with the results of similar studies in other occupational groups, some inferences are possible. Two consistent findings have emerged from studies of worker mental health in other occupational groups: manager behaviour is a very strong predictor of worker mental health outcomes; and the key to achieving meaningful changes in managers’ behaviour is improving their confidence and skills regarding questions of mental health.13,15,21,22 The degree of improved confidence and behaviour reported by the participants in our study is comparable with that reported following interventions in other occupational groups;15,16 among emergency service workers, for example, substantial changes in self‐reported confidence and manager behaviour were associated with substantial reductions in worker illness‐related absences over six months.15 However, different occupational groups may respond to training in different ways, and our findings cannot be interpreted as showing that mental health training for senior physicians will lead to better mental health outcomes for resident physicians.
Nevertheless, we are the first researchers to report that a brief online intervention can lead to changes in senior physicians’ self‐reported behaviour toward their junior staff. Given the importance of manager behaviour, this suggests that this type of intervention could improve junior doctors’ mental health, but this question will require specific investigation.
Limitations
The low participation rate meant that our trial included a small sample of the population of physician supervisors, and interest in mental health may have motivated participation, increasing the risk of selection bias. Although the program examined could be implemented on a larger scale in other areas of health care, the focus in our trial may limit the generalisability of our findings. Further, we assessed physicians’ self‐reported behaviour, which may be prone to reporting bias and not accurately reflect behaviour as experienced by their residents. In addition, the supervisor relationship in hospitals is often transient, and reporting structures for resident physicians are often complex and multidisciplinary. The responsibility of dealing with health problems may rest with supervising physicians, or with other key persons overseeing physician trainees, including directors of training and senior resident physicians. While our planned sample size was initially achieved, eighteen participants were excluded before the baseline survey, the level of intra‐cluster correlation in manager behaviour was greater than anticipated on the basis of trials in other occupational groups.15 While degrees of coalescence in behaviour in different occupations is not surprising, the combined effect was to reduce the statistical power of our study and to increase the risk of type 2 error. Finally, the selected timeframe for assessments seemed sufficient for detecting changes, albeit small, across the follow‐up period; how long the changes were sustained beyond this point, however, is unknown. More than half the intervention group completed the program; this participant adherence rate, although lower than for face‐to‐face training, was within the range of 50–70% adherence rates reported for other online mental health interventions,23 and illustrates one problem in successfully implementing workplace training online.
Conclusion
Our findings indicate that online mental health training for physician supervisors can change self‐reported behaviour in accordance with recommendations for supporting the mental health of resident physicians. Although the consequences for resident physicians’ mental health are unknown, our study illustrates the potential of relatively low‐cost, organisational level mental health interventions. Almost all published trials of interventions for improving the mental health of junior doctors have focused on individual resilience training for junior doctors.24 This is despite doctors‐in‐training consistently stating that this is not what they need, asking instead for evidence‐based interventions that change their work environment.25 Ensuring that physician supervisors have the skills and confidence to better support resident physicians could be part of a multi‐level program for supporting the mental health of the next generation of doctors.11 Our findings indicate the potential of a relatively brief and expandable approach to improving the skills of physician supervisors. Further studies are needed to examine whether the reported changes in behaviour lead to improved mental health in resident physicians.
Box 1 – Recruitment and follow‐up of participants for our cluster randomised controlled trial of mental health training for physicians supervising resident physicians (CONSORT diagram)*
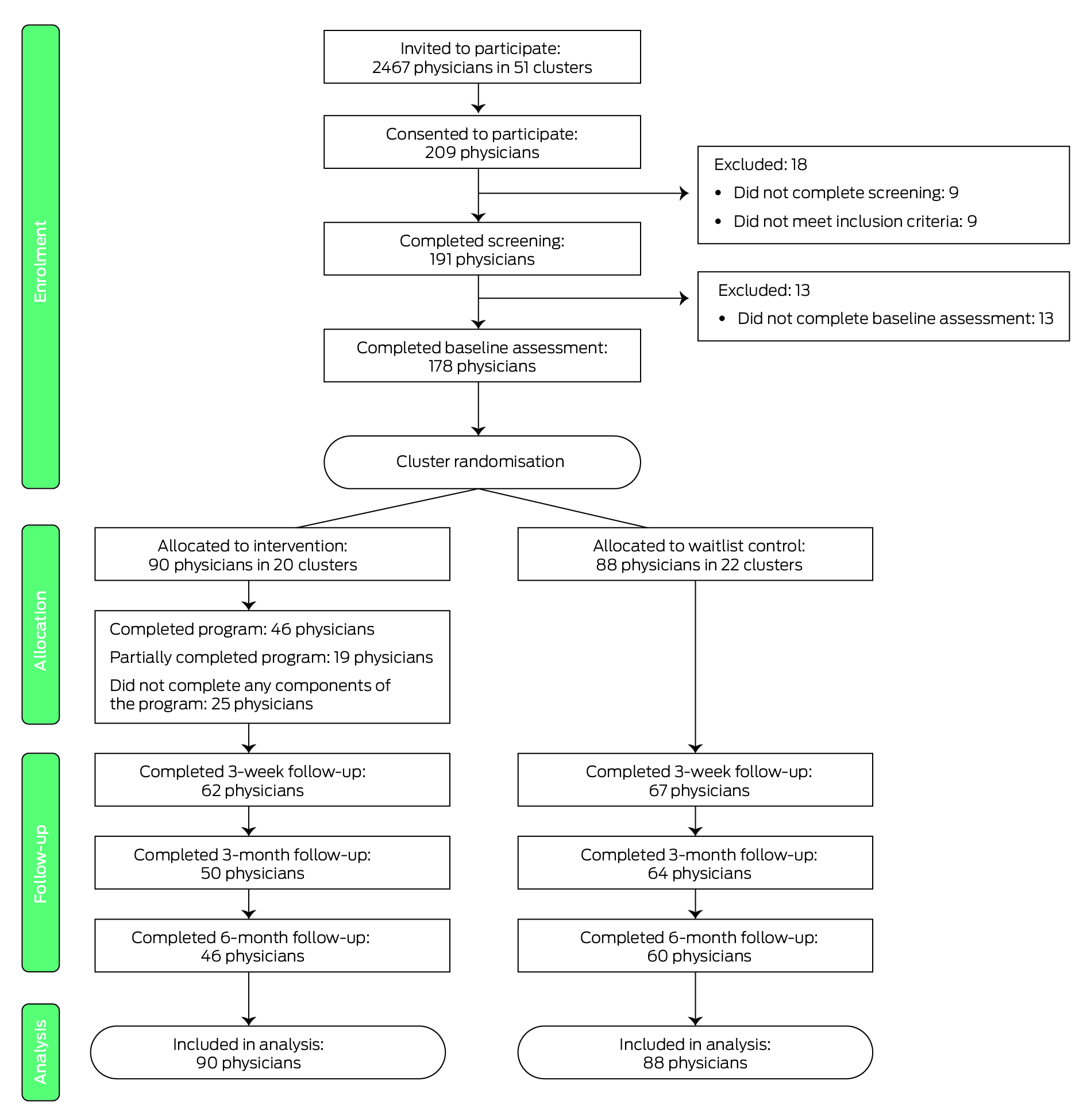
* The numbers in this diagram indicate the number of participants who provided primary outcome data at each follow‐up assessment. At the 3‐month follow‐up, 49 intervention group participants fully completed the questionnaires (one further participant partially completed it, but included full primary outcome data, and is therefore included here); 62 control group participants completed the questionnaires (a further two participants partially completed it, but included full primary outcome data, and are therefore included here).
Box 2 – Baseline demographic characteristics of participants for our cluster randomised controlled trial of mental health training for physicians supervising resident physicians, by trial group allocation
|
Characteristic |
Intervention |
Control |
|||||||||||||
|
|
|||||||||||||||
|
Participants |
90 |
88 |
|||||||||||||
|
Age group (years) |
|
|
|||||||||||||
|
40 or younger |
27 (30%) |
27 (31%) |
|||||||||||||
|
41–50 |
38 (42%) |
36 (41%) |
|||||||||||||
|
51–60 |
19 (21%) |
16 (18%) |
|||||||||||||
|
61 or older |
6 (7%) |
9 (10%) |
|||||||||||||
|
Gender |
|
|
|||||||||||||
|
Men |
36 (40%) |
30 (34%) |
|||||||||||||
|
Women |
54 (60%) |
58 (66%) |
|||||||||||||
|
Time at current hospital (years) |
|
|
|||||||||||||
|
Less than one |
4 (4%) |
6 (7%) |
|||||||||||||
|
1 to 5 |
26 (29%) |
21 (24%) |
|||||||||||||
|
> 5 to10 |
23 (26%) |
23 (26%) |
|||||||||||||
|
> 10 to 15 |
19 (21%) |
23 (26%) |
|||||||||||||
|
More than 15 |
18 (20%) |
15 (17%) |
|||||||||||||
|
Time in supervisory role (years) |
|
|
|||||||||||||
|
Less than one |
8 (9%) |
6 (7%) |
|||||||||||||
|
1 to 5 |
32 (36%) |
33 (38%) |
|||||||||||||
|
> 5 to10 |
20 (22%) |
26 (30%) |
|||||||||||||
|
> 10 to 15 |
13 (14%) |
6 (7%) |
|||||||||||||
|
More than 15 |
17 (19%) |
17 (19%) |
|||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – Mean scores for recommended supervisor behaviours, by trial allocation group and assessment*
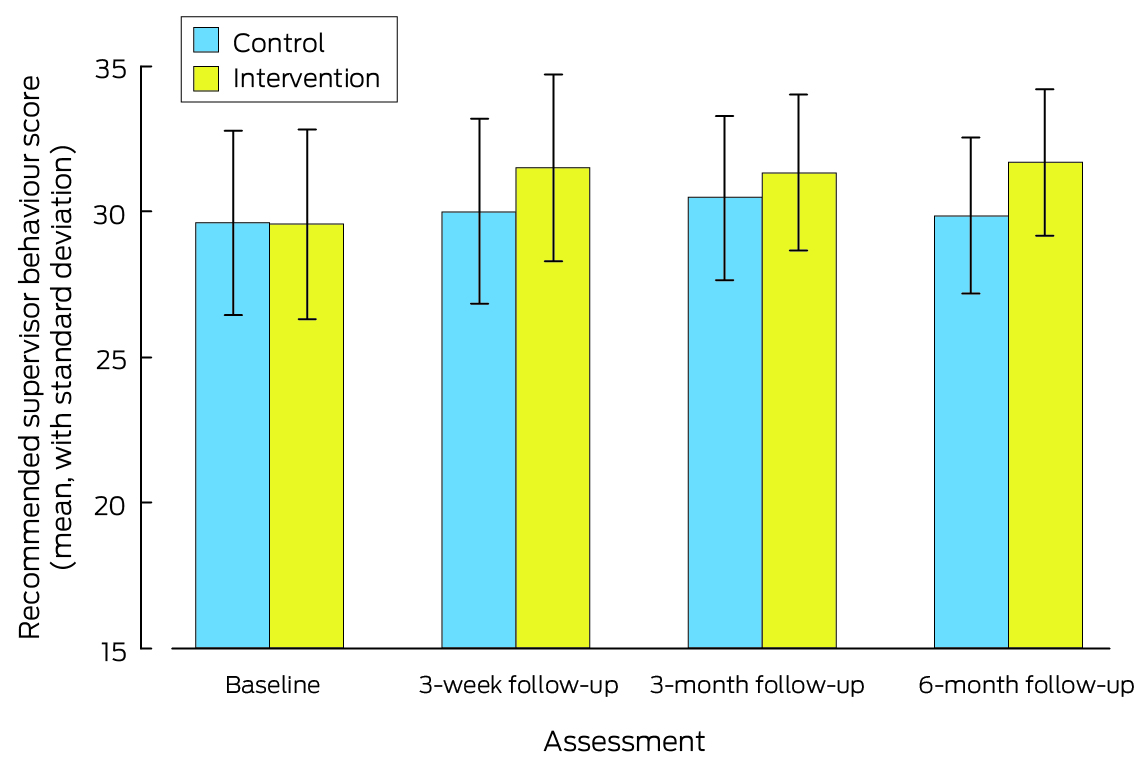
* The data for this graph are included in the Supporting Information, table 1.
Box 4 – Primary outcome: mean recommended supervisor behaviour scores, by trial allocation group and assessment
|
|
Intervention |
Control |
|
||||||||||||
|
Outcome/assessment |
Participants |
Mean score (SD) |
Participants |
Mean score (SD) |
Modelled mean difference between groups in change from baseline (95% CI) |
||||||||||
|
|
|||||||||||||||
|
All behaviour (score range, 15–75) |
|
|
|
|
|
||||||||||
|
Baseline |
90 |
29.5 (2.8) |
88 |
29.6 (2.3) |
— |
||||||||||
|
Post‐training/3 weeks |
62 |
31.6 (3.2) |
67 |
29.9 (2.7) |
1.6 (0.8–2.4) |
||||||||||
|
3 months |
50 |
31.3 (2.6) |
64 |
30.4 (2.6) |
0.9 (0.2–1.6) |
||||||||||
|
6 months |
46 |
31.7 (2.6) |
60 |
29.8 (2.1) |
1.9 (1.1–2.7) |
||||||||||
|
Responsive behaviour (score range, 6–30) |
|
|
|
|
|
||||||||||
|
Baseline |
90 |
20.6 (3.1) |
88 |
20.6 (2.8) |
— |
||||||||||
|
Post‐training/3 weeks |
62 |
23.3 (2.9) |
68 |
20.7 (3.2) |
2.3 (1.5–3.1) |
||||||||||
|
3 months |
50 |
22.8 (2.3) |
64 |
21.8 (2.8) |
1.0 (0.2–1.9) |
||||||||||
|
6 months |
46 |
23.4 (2.4) |
61 |
21.1 (2.9) |
2.0 (1.1–2.9) |
||||||||||
|
Preventive behaviour (score range, 9–45) |
|
|
|
|
|
||||||||||
|
Baseline |
90 |
35.5 (3.3) |
88 |
35.7 (3.0) |
— |
||||||||||
|
Post‐training/3 weeks |
62 |
37.0 (3.9) |
67 |
36.1 (3.3) |
1.1 (0.1–2.2) |
||||||||||
|
3 months |
50 |
37.0 (3.2) |
64 |
36.2 (3.2) |
0.8 (–0.1 to 1.7) |
||||||||||
|
6 months |
46 |
37.3 (3.2) |
60 |
35.6 (2.4) |
1.8 (0.8–2.8) |
||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; SD = standard deviation. |
|||||||||||||||
Box 5 – Secondary outcomes: mean scores, by trial allocation group and assessment
|
|
Intervention |
Control |
|
||||||||||||
|
Outcome/assessment |
Participants† |
Mean score (SD) |
Participants† |
Mean score (SD) |
Modelled mean difference between groups in change from baseline (95% CI) |
||||||||||
|
|
|||||||||||||||
|
Confidence |
|
|
|
|
|
||||||||||
|
Baseline |
90 |
18.4 (4.5) |
88 |
18.2 (4.4) |
— |
||||||||||
|
Post‐training/3 weeks |
62 |
22.2 (4.1) |
68 |
18.5 (4.1) |
3.4 (2.4 to 4.5) |
||||||||||
|
3 months |
51 |
22.2 (3.8) |
64 |
19.6 (4.1) |
2.5 (1.4 to 3.6) |
||||||||||
|
Mental health knowledge |
|
|
|
|
|
||||||||||
|
Baseline |
90 |
24.6 (2.6) |
88 |
24.9 (2.6) |
|
||||||||||
|
Post‐training/3 weeks |
64 |
26.2 (2.1) |
71 |
25.2 (2.2) |
1.4 (0.7 to 2.1) |
||||||||||
|
3 months |
51 |
26.0 (2.2) |
62 |
25.6 (2.2) |
0.7 (–0.4 to 1.5) |
||||||||||
|
Stigmatising attitudes regarding mental health* |
|
|
|
|
|
||||||||||
|
Baseline |
90 |
18.2 (4.1) |
88 |
18.5 (4.1) |
— |
||||||||||
|
Post‐training/3 weeks |
62 |
17.0 (4.5) |
70 |
17.9 (4.6) |
–0.6 (–2.0 to 0.9) |
||||||||||
|
3 months |
50 |
16.5 (3.3) |
62 |
18.7 (3.4) |
–1.9 (–3.1 to –0.6) |
||||||||||
|
Psychological distress |
|
|
|
|
|
||||||||||
|
Baseline |
90 |
10.2 (3.7) |
88 |
9.9 (3.6) |
— |
||||||||||
|
Post‐training/3 weeks |
62 |
9.5 (3.0) |
67 |
9.4 (3.1) |
–0.2 (–0.9 to 0.5) |
||||||||||
|
3 months |
49 |
9.7 (3.2) |
62 |
9.6 (3.4) |
–0.2 (–1.2 to 0.7) |
||||||||||
|
|
|||||||||||||||
|
* Estimated in mixed models excluding the clustering random intercept as there was no estimable clustering effect. † Participant numbers differ between questionnaire items as some participants only partially completed the questionnaires; responses for items presented earlier in the questionnaire may therefore be more complete than for items later in the questionnaire. |
|||||||||||||||
Received 20 April 2023, accepted 22 December 2023
- Aimée Gayed1
- Jessica Strudwick1
- Nathasha Kugenthiran1
- Anthony D LaMontagne2,3
- Andrew Mackinnon1
- Helen Christensen1
- Nicholas Glozier4
- Samuel Harvey1
- 1 Black Dog Institute, UNSW, Sydney, NSW
- 2 Institute for Health Transformation, Deakin University, Geelong, VIC
- 3 Melbourne School of Population and Global Health, the University of Melbourne, Melbourne, VIC
- 4 The University of Sydney, Sydney, NSW
Open access:
Open access publishing facilitated by University of New South Wales, as part of the Wiley ‐ University of New South Wales agreement via the Council of Australian University Librarians.
Data sharing:
Enquiries regarding access to the data that underlie this report should be directed to the corresponding author.
The preparation of this report received funding support from the Australian Department of Health and Aged Care through the Prevention Hub (grant 4‐81K7SSM). Additional funding was provided by iCare NSW. The funders had no role in study design, data collection, analysis, interpretation, or writing of this report. Samuel B Harvey is supported by a National Health and Medical Research Council Investigator Grant. We are extremely grateful to Allison Milner (University of Melbourne) for her contribution to this study before her tragic death.
Open access publishing facilitated by University of New South Wales, as part of the Wiley ‐ University of New South Wales agreement via the Council of Australian University Librarians.
Aimee Gayed, Nathasha Kugenthiran, Jessica Strudwick, Andrew Mackinnon, Helen Christensen and Samuel B Harvey are employed by the Black Dog Institute, which provides manager training to workplaces.
- 1. Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta‐analysis. JAMA 2015; 314: 2373‐2383.
- 2. BeyondBlue. National mental health survey of doctors and medical students. 2013. Oct 2013; updated Feb 2019. https://medicine.uq.edu.au/files/42088/Beyondblue%20Doctors%20Mental%20health.pdf (viewed July 2021).
- 3. Clarke R, McKee M. Suicides among junior doctors in the NHS. BMJ 2017; 357: j2527.
- 4. Harvey SB, Epstein RM, Glozier N, et al. Mental illness and suicide among physicians. Lancet 2021; 398: 920‐930.
- 5. Stanton J, Randal P. Doctors accessing mental‐health services: an exploratory study. BMJ Open 2011; 1: e000017.
- 6. Pereira‐Lima K, Mata DA, Loureiro SR, et al. Association between physician depressive symptoms and medical errors: a systematic review and meta‐analysis. JAMA Netw Open 2019; 2: e1916097.
- 7. Petrie K, Crawford J, LaMontagne AD, et al. Working hours, common mental disorder and suicidal ideation among junior doctors in Australia: a cross‐sectional survey. BMJ Open 2020; 10: e033525.
- 8. Forbes MP, Iyengar S, Kay M. Barriers to the psychological well‐being of Australian junior doctors: a qualitative analysis. BMJ Open 2019; 9: e027558.
- 9. Petrie K, Crawford J, Shand F, Harvey SB. Workplace stress, common mental disorder and suicidal ideation in junior doctors. Intern Med J 2021; 51: 1074‐1080.
- 10. Petrie K, Joyce S, Tan L, et al. A framework to create more mentally healthy workplaces: a viewpoint. Aust N Z J Psychiatry 2017; 52: 15‐23.
- 11. LaMontagne AD, Martin A, Page KM, et al. Workplace mental health: developing an integrated intervention approach. BMC Psychiatry 2014; 14: 131.
- 12. World Health Organization. WHO guidelines on mental health at work. 28 Sept 2022. https://www.who.int/publications/i/item/9789240053052 (viewed June 2024).
- 13. Petrie K, Gayed A, Bryan BT, et al. The importance of manager support for the mental health and well‐being of ambulance personnel. PLoS One 2018; 13: e0197802.
- 14. Petrie K, Deady M, Lupton D, et al. “The hardest job I've ever done”: a qualitative exploration of the factors affecting junior doctors’ mental health and well‐being during medical training in Australia. BMC Health Serv Res 2021; 21: 1342.
- 15. Milligan‐Saville JS, Tan L, Gayed A, et al. Workplace mental health training for managers and its effect on sick leave in employees: a cluster randomised controlled trial. Lancet Psychiatry 2017; 4: 850‐858.
- 16. Gayed A, Bryan BT, LaMontagne AD, et al. A cluster randomized controlled trial to evaluate HeadCoach: an online mental health training program for workplace managers. J Occup Environ Med 2019; 61: 545‐551.
- 17. Gayed A, Kugenthiran N, LaMontagne AD, et al. Can an online mental health training programme improve physician supervisors’ behaviour towards trainees? Intern Med J 2021; 51: 1441‐1449.
- 18. Campbell MK, Elbourne DR, Altman DG; CONSORT Group. CONSORT statement: extension to cluster randomised trials. BMJ 2004; 328: 702‐708.
- 19. Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non‐specific psychological distress. Psychol Med 2002; 32: 959‐976.
- 20. Evans‐Lacko S, Little K, Meltzer H, et al. Development and psychometric properties of the Mental Health Knowledge Schedule. Can J Psychiatry 2010; 55: 440‐448.
- 21. Gayed A, Milligan‐Saville JS, Nicholas J, et al. Effectiveness of training workplace managers to understand and support the mental health needs of employees: a systematic review and meta‐analysis. Occup Environ Med 2018; 75: 462‐470.
- 22. Bryan BT, Gayed A, Milligan‐Saville JS, et al. Managers’ response to mental health issues among their staff. Occup Med (Lond) 2018; 68: 464‐468.
- 23. Christensen H, Griffiths KM, Farrer L. Adherence in internet interventions for anxiety and depression. J Med Internet Res 2009; 11: e13.
- 24. Petrie K, Crawford J, Baker STE, et al. Interventions to reduce symptoms of common mental disorders and suicidal ideation in physicians: a systematic review and meta‐analysis. Lancet Psychiatry 2019; 6: 225‐234.
- 25. Hodge E, Witter E. Doctors‐in‐training need system reform, not more resilience. InSight+ (Australia), 28 Aug 2023. https://insightplus.mja.com.au/2023/32/doctors‐in‐training‐need‐system‐reform‐not‐more‐resilience (viewed July 2024).






Abstract
Objective: To evaluate an online training program for physician supervisors with the aim of promoting a mentally healthy workplace by improving their use of both responsive and preventive mental health support strategies.
Study design: Cluster randomised, waitlist‐controlled trial.
Setting, participants: Royal Australasian College of Physicians fellows who were supervising at least one resident physician in any of the 31 primary health networks in Australia and 20 district health boards in New Zealand (health network clusters).
Intervention: A brief online skills‐based mental health training program, comprising twelve modules grouped into three topics: common mental illnesses; helping trainees you are concerned about (responsive strategies); and minimising mental health risks at work (preventive strategies).
Main outcome measures: Change between baseline and the 3‐month assessment in self‐reported recommended supervisor behaviours; differences between intervention and control groups in recommended behaviour scores three weeks, three months, and six months after the program.
Results: Ninety physicians from 20 health network clusters were allocated to the intervention group, 88 physicians from 22 clusters to the control group. Intervention group participants reported greater positive change in behaviour across the study period than those in the control group (mixed model repeated measures analysis, group × time interaction:P < 0.001). The mean change in self‐reported supervisory behaviour score was higher for the intervention than the control group at the 3‐week (mean difference in score, 1.6; 95% confidence interval [CI], 0.8–2.4), 3‐month (0.9; 95% CI, 0.2–1.6), and 6‐month assessments (1.9; 95% CI, 1.1–2.7). The mean change in self‐reported responsive behaviour score was also greater for the intervention group at the 3‐week (mean difference, 2.3; 95% CI, 1.5–3.1), 3‐month (1.0; 95% CI, 0.2–1.9), and 6‐month assessments (2.0; 95% CI, 1.1–2.9); differences in the mean change in preventive behaviour scores were statistically significant at the 3‐week (mean difference, 1.1; 95% CI, 0.1–2.2) and 6‐month assessments (1.8; 95% CI, 0.8–2.8), but not the 3‐month assessment (0.8; 95% CI, –0.1 to 1.7).
Conclusions: Brief online mental health training for senior physicians can lead to changes in their self‐reported behaviour for supporting the mental health needs of resident physicians. Whether this leads to better mental health for resident physicians should be investigated.
Trial registration: Australian New Zealand Clinical Trials Registry, ACTRN12619001496101 (prospective).