The known: The 2023 Senate inquiry into universal access to reproductive health care identified major structural barriers to abortion care in Australia.
The new: During 2012–22, the number of hospital abortions declined in Victoria, while that of early medical abortions outside hospitals increased; the overall number of abortions did not change markedly. The availability of outpatient abortion was important for maintaining access during the COVID‐19 pandemic.
The implications: Outpatient medical abortion will probably be the primary option for early abortion in the near future. This approach has advantages for both women and the health system, but hospitals will still be crucial for safeguarding comprehensive abortion care.
In 2022, the Australian Senate launched an inquiry into barriers to achieving universal access to sexual and reproductive health information, treatment, and services, a priority aim of the National Women's Health Strategy. In its report, the Senate committee acknowledged the barriers and the “postcode lottery” experienced by people who need abortion care in Australia.1
Equitable access to abortion is a fundamental component of sexual and reproductive health,2 and the right to obtain an abortion in safety and with privacy and dignity is enshrined in Australian law.3 However, a range of barriers hinder access to safe, affordable abortion care, including geographic location and cost.4 The coronavirus disease 2019 (COVID‐19) pandemic and associated restrictions may have exacerbated these barriers, particularly for marginalised women.4
The number of COVID‐19 cases during 2020 was higher in Victoria than elsewhere in Australia, and Melbourne was subject to the strictest lockdown measures in the country.5 To preserve hospital capacity and reduce the exposure of patients and staff to infection, in‐person hospital outpatient services were restricted, many hospital‐based services were shifted to primary care, and elective surgery in Melbourne was cancelled from March 2020. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) urged health authorities to prioritise timely access to abortion services during the pandemic as category 1 (urgent) surgery.6
Whether hospital‐based abortion care was maintained during the pandemic or alternatives such as outpatient early medical abortions expanded capacity is unknown because of the inadequate collection and reporting of abortion care data at the state and national levels. The systematic collection of abortion and reproductive health care outcomes data was recognised as a priority by the Senate committee.1
In our study, we assessed the monthly number of hospital admissions and outpatient early medical abortions in Victoria during January 2012 – March 2022, with a particular interest in the impact of the COVID‐19 pandemic on abortion care.
Methods
We report our population‐based retrospective cohort study in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cohort study reporting.7
Data sources
We analysed Victorian Department of Health hospital admissions data in the Victorian Admitted Episodes Dataset (VAED). The VAED comprises demographic, clinical, and administrative details for all admitted care episodes in public and private health care facilities.8 The Victorian Agency for Health Information (VAHI) extracted data for all admitted care episodes during 1 January 2012 – 31 March 2022 with a recorded principal diagnosis of medical abortion (International Statistical Classification of Diseases, tenth revision, Australian modification [ICD‐10‐AM] code O04).9 “Medical abortion”, distinguished in the VAED from spontaneous abortion (miscarriage), includes all abortion types performed in health care facilities, including surgical and medication‐induced abortions. Reasons for abortion are not included in the dataset. VAHI supplied all data in deidentified form.
We estimated rates of outpatient early medication abortion in Victoria during 1 January 2015 – 31 March 2022 on the basis of claims to the Pharmaceutical Benefits Scheme (PBS) for mifepristone–misoprostol (MS‐2 Step), as reported in the Pharmaceutical Benefits Schedule report.10 Mifepristone–misoprostol was listed on the PBS in 2015 (item 10211K);11,12 it is approved for outpatient medical abortion up to nine weeks after the most recent menstrual period (ie, 63 days’ gestation).11
Outcomes
The primary outcomes were the changes in the monthly numbers of hospital admissions for abortion, outpatient early medical abortions, and all abortions (hospital and outpatient). We also assessed associations between socio‐demographic and clinical characteristics of women who had abortions in hospitals, and the characteristics of the hospitals, with changes in abortion numbers and the need for intensive care.
Time periods
The pandemic period was defined as the time from the halting of elective surgery in Melbourne (26 March 2020; as the data were aggregated by month, our pandemic period commenced in April 2020) to the end of our study period (March 2022). The pre‐pandemic period was defined as January 2012 – March 2020.
Statistical analysis
We report summary statistics for hospital‐based abortion admissions, by time period. We modelled changes in the monthly number of hospital admissions for abortion using interrupted time series analysis, and undertook subgroup analyses for the following variables:
- geographic location (major cities or inner regional/outer regional/remote), based on the Australian Bureau of Statistics remoteness structure;13
- socio‐economic status of residential postcode according to the Australian Bureau of Statistics Socio‐Economic Indexes for Areas (SEIFA) Index of Relative Socio‐economic Advantage and Disadvantage (IRSAD), derived from 2016 census data;14
- hospital type (private or public);
- length of gestation at time of abortion (less than 14 weeks, 14–19 weeks, 20 weeks or more); and
- age group of the woman (unequal age brackets because of uneven distribution of ages: under 18, 18–25, 26–29, 30–34, 35–39, 40 years or older).
We performed an interrupted time series analysis that incorporated harmonic terms (sine and cosine functions) to adjust for seasonal variation. We used Prais–Winsten generalised least squares regression to adjust for autocorrelation of residuals;15 the regression error terms were assumed to follow a first‐order autoregressive process. Assessment of the performance of the model adjusted for autocorrelation with the Durbin–Watson statistic16 indicated that adjustment was adequate. Time series figures are reported as monthly figures and fitted values, together with the pre‐pandemic period median (with the interquartile range, IQR). As coefficients we report the slopes of the fitted curves for the pre‐pandemic period (January 2018 – March 2020), for the first full month of the COVID‐19 pandemic (intervention; April 2020), and for the pandemic period May 2020 – March 2022.
We identified factors that influenced the likelihood of intensive care unit admission of women admitted to hospital for abortion using bivariate and multivariable logistic regression; we included the covariates COVID‐19 exposure (0 for the pre‐pandemic period, 1 for the intervention and pandemic periods), postcode‐level remoteness and socio‐economic status of the woman's residential address, age group, hospital type, gestational age, and quarter of the year. We report adjusted odds ratios (aORs) with 95% confidence intervals (CIs).
In a sensitivity analysis that controlled for changes in the conception rate during the pandemic period, we converted the absolute monthly numbers of hospital admissions for abortion and outpatient early medical abortions to rates per 1000 hospital births (ICD‐10‐AM codes for hospital births: Z370–Z379).
Statistical analyses were conducted in Stata 18.
Ethics approval
The Royal Children's Hospital Health Research Ethics Committee provided institutional approval for the analysis of the VAED dataset (QA/82339/RCHM‐2021). We did not seek ethics approval for our analysis of the publicly available PBS mifepristone–misoprostol dispensing data.
Results
During January 2012 – March 2022, 148 962 hospital admission episodes for abortion were recorded in Victoria: 127 060 during the pre‐pandemic period and 21 902 during the pandemic period. The median age of women who had hospital‐based abortions during the pandemic period (30 years; interquartile range [IQR], 23–34 years) was higher than during the pre‐pandemic period (28 years; IQR, 24–35 years). The proportions of hospital‐based abortions undertaken in private hospitals (72.0% v 80.4%), in hospitals in major cities (90.7% v 94.8%), or at less than 14 weeks’ gestation (88.5% v 91.3%) were smaller during the pandemic than during the pre‐pandemic period (Box 1). During January 2015 – March 2020 (pre‐pandemic period) there are 14 634 PBS claims for outpatient medical abortions, and 11 154 during the pandemic period.
All abortions: time series analysis
The monthly number of hospital‐based abortions declined during the pre‐pandemic period (slope, –2.92 [95% CI, –3.45 to –2.38] per month). The decline was greater during the first month of the pandemic (April 2020; slope, –128 [95% CI, –201 to –56.1] per month); during the remainder of the pandemic period, the decline was slower, but greater than during the pre‐pandemic period (slope, –5.74 [95% CI, –10.5 to –0.96] per month) (Box 2, Box 3).
The monthly number of outpatient early medical abortions increased from the listing of mifepristone–misoprostol on the PBS in 2015 until the end of the pre‐pandemic period (slope, 5.94 [95% CI, 5.34–6.34] per month). It declined during the first month of the pandemic (slope, –26.4 [95% CI, –70.1 to –17.3] per month), but did not significantly change thereafter (slope, –0.47 [95% CI, –3.33 to 2.39] per month) (Box 2, Box 3).
The total monthly number of abortions during the pandemic period did not deviate markedly from the pre‐pandemic median value, but the slow pre‐pandemic increase (slope, 1.95 [95% CI, 1.34–2.57] per month) was followed by a decline during the pandemic period (slope, –7.23 [95% CI, –12.8 to –1.71] per month) (Box 2, Box 3). During January 2015 – March 2020, 14 634 of 103 496 abortions were outpatient medical abortions (14%); during the pandemic period, 11 154 of 33 056 abortions were outpatient medical abortions (33%).
All abortions, by characteristic: time series analysis
The monthly number of hospital admissions for abortion declined during the pre‐pandemic period in major city hospitals (slope, –2.93 [95% CI, –3.46 to –2.39] per month) and private hospitals (slope, –2.75 [95% CI, –3.25 to –2.24] per month), for abortions at earlier than 14 weeks’ gestation (slope, –1.55 [95% CI, –2.27 to –0.83] per month), and for all women living in each postcode‐based socio‐economic quintile. Declines for each of these groups were steeper during the first month of the pandemic period; however, the declines during this month were not statistically significant for women living in areas in the two most disadvantaged IRSAD quintiles (Box 3, Box 4).
During the pre‐pandemic period, a median 252 (IQR, 236–269) abortions were undertaken in public hospitals each month, and 1020 (IQR, 964–1119) in private hospitals. The proportion of abortions undertaken in public hospitals was higher during the pandemic period (6130 of 21 092, 28.0%) than during the pre‐pandemic period (24 853 of 127 060, 19.6%), but the absolute monthly number undertaken in public hospitals was static.
Women admitted to intensive care during hospital admissions for abortion
The proportion of women admitted to intensive care during the pandemic (34 of 21 902, 0.16%; 1.48 per month) was larger than during the pre‐pandemic period (77 of 127 060, 0.06%; 0.77 per month). The median age of women admitted to intensive care during the pandemic (34 years; IQR, 28–37 years) was higher than during the pre‐pandemic period (28 years; IQR, 24–33 years). The likelihood of admission to intensive care was higher for women who had late term abortions (beyond 20 weeks’ gestation: aOR, 2.08; 95% CI, 1.15–3.77) or abortions in regional hospitals (aOR, 2.74; 95% CI, 1.44–2.82) (Box 5). Fourteen of 4175 women who had abortions in hospital at later than 20 weeks’ gestation were admitted to intensive care (0.34%).
Sensitivity analysis
With respect to the monthly birth rate, the number of hospital‐based abortions declined more rapidly during the first month of the pandemic period (slope, –16.3 [95% CI, –28.2 to –4.41] per 1000 births per month) than during the pre‐pandemic period (slope, –0.51 [95% CI, –0.60 to –0.42] per 1000 births per month). The decline continued during the pandemic period (slope, –1.02 [95% CI, –1.81 to –0.23] per 1000 births per month). The monthly number of mifepristone–misoprostol prescriptions dispensed increased during the pre‐pandemic period (slope, 0.23; [95% CI, 0.10–0.37] per 1000 births per month) and declined during the first month of the pandemic period (slope, –10 [95% CI, –25 to –3] per 1000 births per month). The total number of abortions declined during the pandemic period (slope, –1.28 [95% CI, –2.29 to –0.26] per 1000 births per month) (Supporting Information, figure 5, table 1).
Discussion
We found that the monthly number of hospital‐based abortions in Victoria declined substantially during 2012–22, and that the speed of the decline increased during the COVID‐19 pandemic. The number was still falling in March 2022, despite the lifting of lockdown restrictions, widespread COVID‐19 vaccination, and the adoption of a “living with COVID‐19” public health policy. The decline was particularly marked for terminations undertaken in major city hospitals, in private hospitals, or before 14 weeks’ gestation. It may be linked with the rise in mifepristone–misoprostol dispensing numbers, as the overall monthly number of abortions was relatively stable during the pandemic period.
The decline in the number of hospital‐based abortions was not uniform across socio‐economic status categories, and at the end of the study period was no longer statistically significant among women in areas included in the two most disadvantaged quintiles. This finding suggests that patterns of hospital‐based and outpatient early medical abortion use differ by socio‐economic status. However, this possibility cannot be assessed without individual‐level data for mifepristone–misoprostol dispensing.
The decline in the proportion of surgical abortions and the rise in that of medical abortions is a pattern consistent with pre‐pandemic findings for Australia17 and other high income countries with liberal abortion laws.18 Our findings suggest that local efforts to move early abortion care from hospitals to primary care by increasing the numbers of mifepristone–misoprostol prescribers and dispensers12,19,20,21,22 helped safeguard abortion access in Victoria during the COVID‐19 pandemic, when demands on hospitals were unusually high. Access to abortion in other Australian states during the pandemic should also be investigated.
Our findings also suggest that mifepristone–misoprostol is increasingly the preferred method for early abortion; as is already the case in some European countries,18 we anticipate that outpatient abortions will eventually outnumber first trimester abortions in hospitals. The recent removal of restrictions on mifepristone–misoprostol prescribing and dispensing23 and the recommended retention of MBS telehealth items for reproductive health care (including termination care)1 will support this change, and also enhance the resilience of reproductive health care services during future emergencies.
Equity
Equitable access to abortion care is a priority of the National Women's Health Strategy.24 We found that overall abortion numbers in Victorian public hospitals were not markedly influenced by the dramatic contraction in access to private hospital‐based abortion during the COVID‐19 pandemic. This suggests that public hospitals did not provide “surge capacity” for abortion care to accommodate women who would otherwise have had abortions in private hospitals.
In Victoria, 75% of births are in public hospitals,25 but only 21% of hospital‐based abortions were provided in public hospitals during 2012–22. This difference was noted in the Senate inquiry report, as was the fact that many publicly funded maternity hospitals do not provide abortion services, and others provide only limited services or have complicated referral pathways.1 To improve access and affordability, the Senate committee recommended that “all public hospitals within Australia be equipped to provide surgical pregnancy terminations, or timely and affordable pathways to other local providers.”1 Monitoring patterns of abortion care in public hospitals is critical given the findings of the Senate inquiry.
Complications
The association between admission to intensive care and abortion at 20 weeks’ gestation or later was not surprising given the association between advanced gestation and abortion complications.26,27 Further, it is likely that some later abortions were indicated by obstetric complications during planned pregnancies, such as early onset pre‐eclampsia, and would therefore have involved women who needed high dependency care. The reasons for the association between intensive care admission and abortions in regional hospitals are less clear, but may reflect variations in the risk profiles of the women, or lower thresholds for transfer to intensive care units in regional centres.
Limitations
We analysed a complete Victorian dataset covering both private and public hospitals and including data on the need for intensive care, postcode‐level socio‐economic status, and socio‐demographic characteristics. However, we could measure the availability of abortion care but not the demand for it. Whether the decline in the number of hospital admissions for abortion was attributable to women's choices or reduced accessibility could not be determined. As the PBS dataset did not provide individual‐level data, we could not undertake subgroup analyses of mifepristone–misoprostol dispensing. The small number of women admitted to intensive care limited the statistical power to detect associations with socio‐demographic factors. Finally, mifepristone and misoprostol were registered for use in early medical abortion in Australia in 2012,28 three years prior to the PBS listing of the combination product mifepristone–misoprostol in 2015; dispensing data prior to its PBS listing were not available and therefore not included in our analysis.
Conclusions
Our findings highlight changing patterns of abortion care in Victoria and the gradual shift from metropolitan private hospital to outpatient early medical abortions. The increasing availability of mifepristone–misoprostol helped maintain access to abortion despite restricted hospital‐based care during the COVID‐19 pandemic. However, outpatient medical abortion is not always appropriate, and hospitals will continue to be essential for comprehensive abortion care. The priorities listed in the report of the Senate inquiry into universal access to reproductive health care, including adequate data collection and identifying differences in abortion service provision, will require further investigation.
Box 1 – Hospital admissions for abortion, Victoria, January 2012 – March 2022: characteristics of the women and the hospitals, and the gestational age of the fetus
|
Characteristic |
Pre‐pandemic period (Jan 2012 – Mar 2020) |
Pandemic period (Apr 2020 – Mar 2022) |
|||||||||||||
|
|
|||||||||||||||
|
Number of admissions |
127 060 |
21 902 |
|||||||||||||
|
Age group (years) |
|
|
|||||||||||||
|
Under 18 |
3308 (2.6%) |
371 (1.7%) |
|||||||||||||
|
18–24 |
44 747 (35.2%) |
6313 (28.8%) |
|||||||||||||
|
25–29 |
25 050 (19.7%) |
4212 (19.2%) |
|||||||||||||
|
30–34 |
26 631 (21.0%) |
5315 (24.3%) |
|||||||||||||
|
35–39 |
18 685 (14.7%) |
4086 (18.7%) |
|||||||||||||
|
40 or older |
8639 (6.8%) |
1605 (7.3%) |
|||||||||||||
|
Geographic remoteness |
|
|
|||||||||||||
|
Major cities |
120 407 (94.8%) |
19 858 (90.7%) |
|||||||||||||
|
Inner regional/outer regional/remote |
6653 (5.2%) |
2044 (9.3%) |
|||||||||||||
|
Socio‐economic status (IRSAD quintile) |
|
|
|||||||||||||
|
1 (most disadvantaged) |
19 879 (15.7%) |
2963 (13.6%) |
|||||||||||||
|
2 |
19 520 (15.4%) |
3522 (16.2%) |
|||||||||||||
|
3 |
27 522 (21.7%) |
4935 (22.7%) |
|||||||||||||
|
4 |
27 226 (21.5%) |
4630 (21.3%) |
|||||||||||||
|
5 (most advantaged) |
32 560 (25.7%) |
5712 (26.2%) |
|||||||||||||
|
Health facility classification |
|
|
|||||||||||||
|
Private |
102 207 (80.4%) |
15 772 (72.0%) |
|||||||||||||
|
Public |
24 853 (19.6%) |
6130 (28.0%) |
|||||||||||||
|
Gestational age at abortion (weeks) |
|
|
|||||||||||||
|
Less than 14 |
109 486 (91.3%) |
18 868 (88.5%) |
|||||||||||||
|
14–19 |
6885 (5.7%) |
1803 (8.5%) |
|||||||||||||
|
20 or more |
3535 (3.0%) |
640 (3.0%) |
|||||||||||||
|
|
|||||||||||||||
|
IRSAD = Index of Relative Socio‐economic Advantage and Disadvantage.14 |
|||||||||||||||
Box 2 – Terminations of pregnancy, Victoria, 1 January 2012 – 31 March 2022, by termination type: time series analyses*
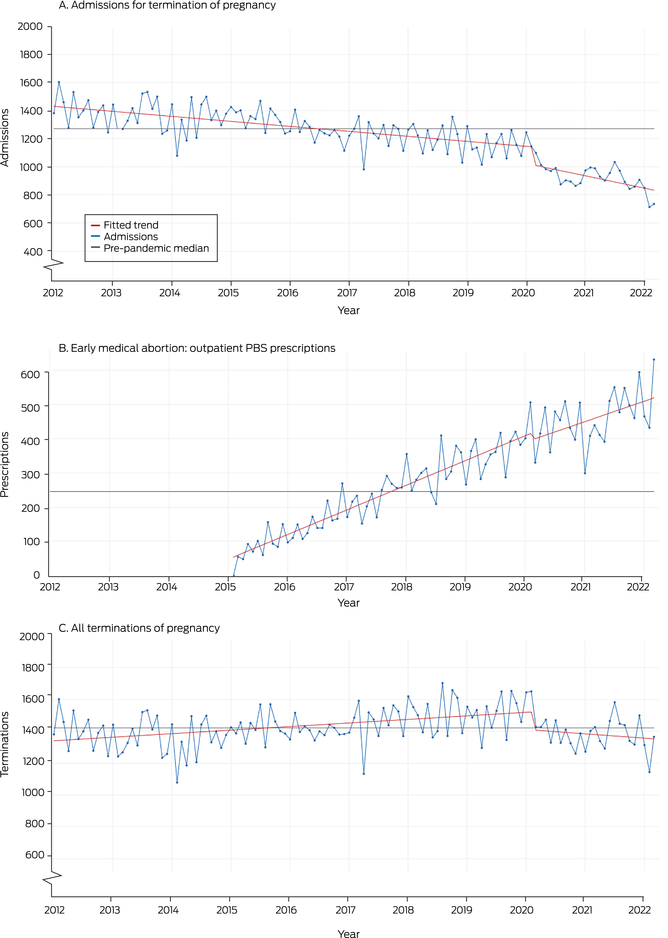
PBS = Pharmaceutical Benefits Scheme. * Median pre‐pandemic values: Admissions for termination of pregnancy, 1269 (interquartile range [IQR], 1218–1379); early medical abortions, 246 (IQR, 150–325); all terminations of pregnancy, 1422 (IQR, 1371–1520).
Box 3 – Pregnancy terminations, Victoria, 1 January 2012 – 31 March 2022, by characteristics of the women and hospitals and the gestational age of the fetus: time series analyses*
|
|
Slope (95% confidence interval) |
||||||||||||||
|
Characteristic |
Pre‐pandemic period (Jan 2012 – Mar 2020) |
First month of the pandemic (Apr 2020) |
Pandemic period (May 2020 – Mar 2022) |
||||||||||||
|
|
|||||||||||||||
|
All abortions† |
1.95 (1.34 to 2.57) |
–87.3 (–171 to –3.93) |
–7.23 (–12.8 to –1.71) |
||||||||||||
|
Hospital‐based abortion |
–2.92 (–3.45 to –2.38) |
–128 (–201 to –56.1) |
–5.74 (–10.5 to –0.96) |
||||||||||||
|
Outpatient early medical abortion |
5.94 (5.34 to 6.54) |
–26.4 (–70.1 to 17.3) |
–0.47 (–3.33 to 2.39) |
||||||||||||
|
Age group (years)‡ |
|
|
|
||||||||||||
|
Under 18 |
–0.42 (–0.49 to –0.35) |
5.88 (–2.71 to 14.5) |
0.19 (–0.38 to 0.77) |
||||||||||||
|
18–24 |
–2.26 (–2.49 to –2.02) |
–28.5 (–59.6 to 2.64) |
–1.91 (–3.98 to 0.15) |
||||||||||||
|
25–29 |
–0.30 (–0.49 to –0.11) |
–57.8 (–82.7 to –32.8) |
–0.27 (–1.92 to 1.38) |
||||||||||||
|
30–34 |
0.11 (–0.02 to 0.25) |
–35.6 (–54.0 to –17.2) |
–1.82 (–3.04 to –0.61) |
||||||||||||
|
35–39 |
0.22 (0.10 to 0.33) |
–10.8 (–26.7 to 5.25) |
–1.89 (–2.95 to –0.83) |
||||||||||||
|
40 or older |
–0.28 (–0.33 to –0.22) |
–0.88 (–8.46 to 6.69) |
–0.12 (–0.62 to 0.38) |
||||||||||||
|
Geographic remoteness§ |
|
|
|
||||||||||||
|
Major cities |
–2.93 (–3.46 to –2.39) |
–138 (–207 to –71.4) |
–6.52 (–11.3 to –1.73) |
||||||||||||
|
Inner regional/outer regional/remote |
0.01 (–0.12 to 0.13) |
9.00 (–11.0 to 34.4) |
0.78 (–0.25 to 1.82) |
||||||||||||
|
Socio‐economic status (IRSAD quintile)‡ |
|
|
|
||||||||||||
|
1 (most disadvantaged) |
–1.01 (–1.17 to –0.85) |
–13.3 (–34.2 to 7.51) |
–0.13 (–1.51 to 1.25) |
||||||||||||
|
2 |
–0.47 (–0.62 to –0.33) |
–8.57 (–27.8 to 10.7) |
–0.91 (–2.18 to 0.37) |
||||||||||||
|
3 |
–0.54 (–0.69 to –0.40) |
–22.6 (–41.6 to –3.61) |
–1.39 (–2.64 to –0.13) |
||||||||||||
|
4 |
–0.57 (–0.75 to –0.39) |
–29.5 (–53.0 to –5.95) |
–1.80 (–3.35 to –0.24) |
||||||||||||
|
5 (most advantaged) |
–0.37 (–0.55 to –0.20) |
–53.1 (–76.4 to –29.8) |
–1.55 (–3.09 to –0.002) |
||||||||||||
|
Health facility classification§ |
|
|
|
||||||||||||
|
Private |
–0.18 (–0.35 to –0.01) |
11.7 (–11.0 to 34.4) |
0.55 (–0.96 to 2.05) |
||||||||||||
|
Public |
–2.75 (–3.25 to –2.24) |
–139 (–207 to –71.4) |
–6.31 (–10.8 to –1.81) |
||||||||||||
|
Gestational age at abortion (weeks)§ |
|
|
|
||||||||||||
|
Less than 14 |
–1.55 (–2.27 to –0.83) |
–155 (–250 to –60.8) |
–7.99 (–14.2 to –1.74) |
||||||||||||
|
14–19 |
0.19 (0.11 to 0.26) |
–10.7 (–20.7 to –0.65) |
0.35 (–0.32 to 1.01) |
||||||||||||
|
20 or more |
0.05 (–0.04 to 0.15) |
–13.4 (–25.3 to –1.50) |
–0.09 (–0.88 to 0.70) |
||||||||||||
|
|
|||||||||||||||
|
IRSAD = Index of Relative Socio‐economic Advantage and Disadvantage.14 * Adjusted for autocorrelation and seasonality. † These time series are depicted in Box 2. ‡ These time series are depicted in the Supporting Information, figures 1 and 2. § These time series are depicted in Box 4. |
|||||||||||||||
Box 4 – Pregnancy terminations, Victoria, 1 January 2012 – 31 March 2022, by geographic remoteness, hospital type, and gestational age at termination: time series analyses*
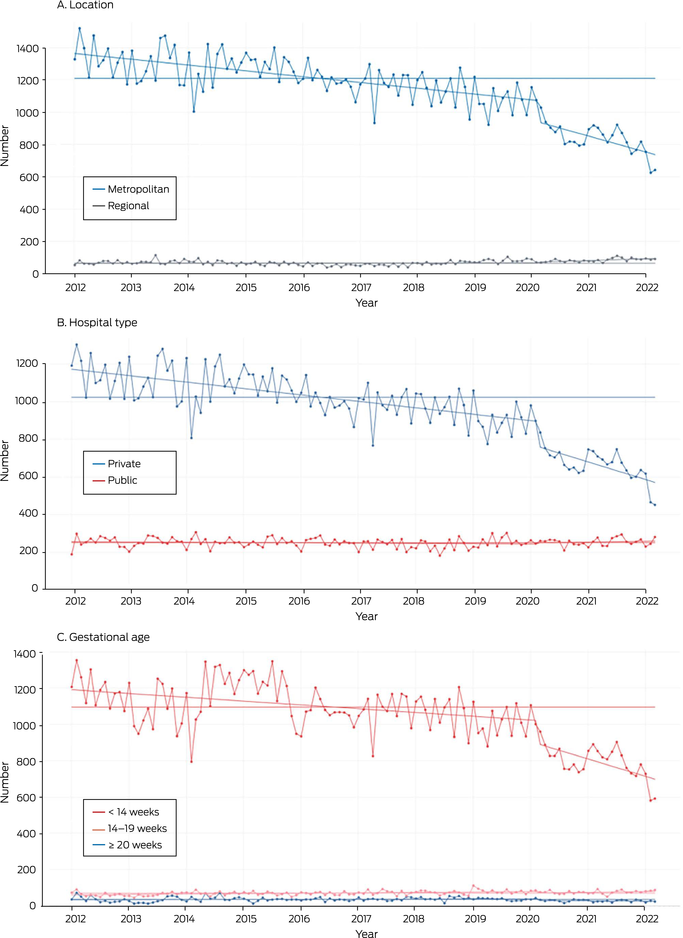
* Adjusted for autocorrelation and seasonality. For clarity, each time series is graphed separately in the Supporting Information, figures 1 and 2. Median pre‐pandemic values: A. metropolitan, 1209 (interquartile range [IQR], 1151–1311), regional, 65 (IQR, 58–76); B. private, 1024 (IQR, 964–1118), public, 252 (IQR, 236–268); C. < 14 weeks, 1096 (IQR, 1024–1194), 14–19 weeks, 70 (IQR, 61–76), 20 weeks or later, 35 (IQR, 28–42).
Box 5 – Admissions to intensive care of women admitted to hospital for abortions, Victoria, January 2012 – March 2022: characteristics of the women and the gestational age of the fetus
|
Characteristic |
Pre‐pandemic period (1 Jan 2012 – 30 Mar 2020) |
Pandemic period (31 Mar 2020 – 31 Mar 2022) |
Adjusted odds ratio* (95% confidence interval) |
||||||||||||
|
|
|||||||||||||||
|
Intensive care admissions/total admissions |
77/127 060 [0.06%] |
34/21 902 [0.16%] |
— |
||||||||||||
|
Age group (years) |
|
|
|
||||||||||||
|
Under 18 |
< 5 |
< 5 |
0.62 (0.19–2.08) |
||||||||||||
|
18–24 |
23 (30%) |
6 (18%) |
0.74 (0.42–1.28) |
||||||||||||
|
25–29 |
18 (23%) |
5 (15%) |
1 |
||||||||||||
|
30–34 |
19 (25%) |
8 (24%) |
0.77 (0.43–1.38) |
||||||||||||
|
35–39 |
10 (13%) |
9 (26%) |
0.82 (0.44–1.54) |
||||||||||||
|
40 or older |
< 5 |
6 (18%) |
1.23 (0.58–2.59) |
||||||||||||
|
Geographic remoteness |
|
|
|
||||||||||||
|
Major cities |
69 (90%) |
29 (85%) |
1 |
||||||||||||
|
Inner regional/outer regional/remote |
8 (10%) |
5 (15%) |
2.74 (1.44–2.82) |
||||||||||||
|
Socio‐economic status (IRSAD quintile)* |
|
|
|
||||||||||||
|
1 (most disadvantaged) |
11 (14%) |
< 5 |
0.89 (0.46–1.72) |
||||||||||||
|
2 |
19 (25%) |
8 (25%) |
1.34 (0.76–2.37) |
||||||||||||
|
3 |
16 (21%) |
7 (22%) |
1 |
||||||||||||
|
4 |
19 (25%) |
5 (16%) |
1.13 (0.63–2.01) |
||||||||||||
|
5 (most advantaged) |
12 (16%) |
8 (25%) |
0.85 (0.45–1.61) |
||||||||||||
|
Gestational age at abortion (weeks) |
|
|
|
||||||||||||
|
Less than 14 |
52 (68%) |
13 (38%) |
1 |
||||||||||||
|
14–19 |
12 (16%) |
14 (41%) |
1.56 (0.97–2.50) |
||||||||||||
|
20 or more |
11 (14%) |
< 5 |
2.08 (1.15–3.77) |
||||||||||||
|
|
|||||||||||||||
|
IRSAD = Index of Relative Socio‐economic Advantage and Disadvantage.14 * Adjusted for COVID‐19 exposure (0 for the pre‐pandemic period, 1 for the intervention and pandemic periods), postcode‐level remoteness and socio‐economic status of the woman's residential address, age group, hospital type, gestational age, and quarter of the year. |
|||||||||||||||
Received 8 August 2023, accepted 2 November 2023
- Melvin B Marzan1,2
- Eleanor Johnson3
- Patricia Moore1,4
- Heng Jiang5,6
- Lisa Hui1,2
- 1 Melbourne Medical School, the University of Melbourne, Melbourne, VIC
- 2 Murdoch Children's Research Institute, Melbourne, VIC
- 3 Northern Centre for Health Education Research, Northern Health, Melbourne, VIC
- 4 Royal Women's Hospital, Melbourne, VIC
- 5 La Trobe University, Melbourne, VIC
- 6 Centre for Health Equity, the University of Melbourne, Melbourne, VIC
Open access:
Open access publishing facilitated by The University of Melbourne, as part of the Wiley – The University of Melbourne agreement via the Council of Australian University Librarians.
Data availability:
Lisa Hui has a National Health and Medical Research Council fellowship (1105603). Eleanor Johnson is supported by a Melbourne Academic Centre for Health fellowship. The funders had no role in study design, data collection, data analysis, data interpretation, or the writing of the report.
We thank Harriet Hiscock (University of Melbourne) for her leadership of the Impact of COVID‐19 on Healthcare project, part of the Victorian Collaborative Healthcare Recovery Initiative. The study described in this article was an extension of this project with a separate ethics approval. We acknowledge the Victorian Department of Health as the source of the Victorian Admitted Episodes Dataset (VAED) data we analysed.
No relevant disclosures.
- 1. Community Affairs References Committee. Ending the postcode lottery: addressing barriers to sexual, maternity and reproductive healthcare in Australia. May 2023. https://parlinfo.aph.gov.au/parlInfo/download/committees/reportsen/RB000075/toc_pdf/EndingthepostcodelotteryAddressingbarrierstosexual,maternityandreproductivehealthcareinAustralia.pdf (viewed June 2023).
- 2. World Health Organization. Abortion: quality abortion care. 2023. https://www.who.int/health‐topics/abortion#tab=tab_3 (viewed Feb 2023).
- 3. Children by Choice. Australian abortion law and practice, 2023. https://www.childrenbychoice.org.au/organisational‐information/legislation/australian‐abortion‐law‐and‐practice (viewed Feb 2023).
- 4. Sifris R, Penovic T. Barriers to abortion access in Australia before and during the COVID‐19 pandemic. Womens Stud Int Forum 2021; 86: 102470.
- 5. Department of Health and Human Services (Victoria). Premier's statement on changes to Melbourne's restrictions. [media release]. 2 Aug 2020. Archived: https://web.archive.org/web/20230322130015/https://www.dhhs.vic.gov.au/updates/coronavirus‐covid‐19/premiers‐statement‐changes‐melbournes‐restrictions‐2‐august‐2020 (viewed June 2022).
- 6. Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG). COVID‐19: Category 1 (Australia) and Urgent (New Zealand) gynaecological conditions and surgical risks [media release]. 25 Mar 2020; updated 27 Aug 2021. Archived: https://web.archive.org/web/20210922080027/https://ranzcog.edu.au/news/category‐1‐gynaecological‐conditions (viewed Oct 2021).
- 7. Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453‐1457.
- 8. Department of Health and Human Services (Victoria). Victorian Admitted Episodes Dataset. Updated 23 Oct 2023. https://www2.health.vic.gov.au/hospitals‐and‐health‐services/data‐reporting/health‐data‐standards‐systems/data‐collections/vaed (viewed Nov 2023).
- 9. Independent Health and Aged Care Pricing Authority. ICD‐10‐AM/ACHI/ACS tenth edition. 1 July 2017. https://www.ihacpa.gov.au/resources/icd‐10‐amachiacs‐tenth‐edition (viewed Oct 2023).
- 10. Services Australia. Pharmaceutical Benefits Schedule items report [website]. http://medicarestatistics.humanservices.gov.au/statistics/pbs_item.jsp (viewed Mar 2023).
- 11. NPS Medicinewise. Mifepristone and misoprostol (MS‐2 Step) composite pack: use extended to 63 days’ gestation. 1 Feb 2015. https://www.nps.org.au/radar/articles/mifepristone‐and‐misoprostol‐ms‐2‐step‐composite‐pack‐use‐extended‐to‐63‐days‐gestation (viewed Feb 2023).
- 12. Subasinghe AK, McGeechan K, Moulton JE, et al. Early medical abortion services provided in Australian primary care. Med J Aust 2021; 215: 366‐370. https://www.mja.com.au/journal/2021/215/8/early‐medical‐abortion‐services‐provided‐australian‐primary‐care
- 13. Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS). Volume 5. Remoteness structure, July 2016 (1270.0.55.005). 16 Mar 2016. https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/1270.0.55.005Main+Features1July%202016?OpenDocument= (viewed Nov 2022).
- 14. Australian Bureau of Statistics. IRSAD. In: Census of Population and Housing: Socio‐Economic Indexes for Areas (SEIFA), Australia, 2016 (2033.0.55.001). 27 Mar 2018. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2033.0.55.001~2016~Main%20Features~IRSAD~20 (viewed Mar 2023).
- 15. Hardin JW. Prais–Winsten regression. Stata Technical Bulletin 1996; 5 (STB‐25): 26‐29.
- 16. Becketti S. Introduction to time series using Stata. College Station: Stata Press, 2013.
- 17. Keogh LA, Gurrin LC, Moore P. Estimating the abortion rate in Australia from National Hospital Morbidity and Pharmaceutical Benefits Scheme data. Med J Aust 2021; 215: 375‐376. https://www.mja.com.au/journal/2021/215/8/estimating‐abortion‐rate‐australia‐national‐hospital‐morbidity‐and
- 18. Popinchalk A, Sedgh G. Trends in the method and gestational age of abortion in high‐income countries. BMJ Sex Reprod Health 2019; 45: 95‐103.
- 19. Hannon CM. Sexual and Reproductive Health Clinical Champion Project [presentation: The Royal Women's Hospital]. Aug 2022. https://www.childrenbychoice.org.au/wp‐content/uploads/2022/09/Catherine‐Hannon‐Beyond‐the‐hospital‐walls‐The‐Clinical‐Champion‐Project‐supporting‐access‐and‐equity‐to‐abortion‐and‐contraception‐services‐.pdf (viewed Feb 2023).
- 20. Mazza D, James S, Black K, et al. Increasing the availability of long‐acting reversible contraception and medical abortion in primary care: the Australian Contraception and Abortion Primary Care Practitioner Support Network (AusCAPPS) cohort study protocol. BMJ Open 2022; 12: e065583.
- 21. Mazza D, Shankar M, Botfield JR, et al. Improving rural and regional access to long‐acting reversible contraception and medical abortion through nurse‐led models of care, task‐sharing and telehealth (ORIENT): a protocol for a stepped‐wedge pragmatic cluster‐randomised controlled trial in Australian general practice. BMJ Open 2023; 13: e065137.
- 22. Women's Health Victoria. Delivering optimal sexual and reproductive health outcomes for Victorian women: priorities for the next women's sexual and reproductive health plan 2021–2025. 2021. https://womenshealthvic.com.au/resources/WHV_Publications/Position‐Paper_2021.01.11_Priorities‐for‐the‐next‐womens‐sexual‐and‐reproductive‐health‐plan‐2021‐2025_single‐page_(Fulltext‐PDF).pdf (viewed Feb 2023).
- 23. Therapeutic Goods Administration. Amendments to restrictions for prescribing of MS‐2 Step (mifepristone and misoprostol). 11 July 2023. https://www.tga.gov.au/news/media‐releases/amendments‐restrictions‐prescribing‐ms‐2‐step‐mifepristone‐and‐misoprostol (viewed Oct 2023).
- 24. Australian Department of Health. National Women's Health Strategy 2020–2030. 2018. https://www.health.gov.au/sites/default/files/documents/2021/05/national‐women‐s‐health‐strategy‐2020‐2030_0.pdf (viewed Feb 2023).
- 25. Victorian Department of Health. Maternity and newborn services. Updated 16 Oct 2023. https://www.health.vic.gov.au/patient‐care/maternity‐and‐newborn‐services (viewed Nov 2023).
- 26. Stewart B, Kane SC, Unterscheider J. Medical termination of pregnancy for fetal anomaly at or beyond 20 weeks' gestation: what are the maternal risks? Prenat Diagn 2022; 42: 1562‐1570.
- 27. White K, Carroll E, Grossman D. Complications from first‐trimester aspiration abortion: a systematic review of the literature. Contraception 2015; 92: 422‐438.
- 28. Goldstone P, Walker C, Hawtin K. Efficacy and safety of mifepristone–buccal misoprostol for early medical abortion in an Australian clinical setting. Aust N Z J Obstet Gynaecol 2017; 57: 366‐371.






Abstract
Objectives: To assess changes in the monthly numbers of hospital‐based abortions and outpatient early medical abortions in Victoria during January 2012 – March 2022, with a particular interest in the impact of the coronavirus disease 2019 (COVID‐19) pandemic.
Study design: Population‐based retrospective cohort study; time series analysis of Victorian Admitted Episodes Dataset (VAED) and Pharmaceutical Benefits Scheme (PBS) data.
Setting, participants: All admitted care episodes in Victoria during 1 January 2012 – 31 March 2022 with medical abortion as the principal diagnosis; all PBS claims for mifepristone–misoprostol (MS‐2 Step) during 1 January 2015 (date of listing) – 31 March 2022.
Main outcome measures: Changes in monthly numbers (with 95% confidence intervals [CIs]) of admissions for hospital‐based and outpatient early medical abortions during the pre‐pandemic period (January 2012 – March 2020), the first full month of the COVID‐19 pandemic (April 2020), and the pandemic period (May 2020 – March 2022).
Results: The monthly number of hospital‐based abortions declined in Victoria during the pre‐pandemic period (slope, –2.92 [95% CI, –3.45 to –2.38] per month); the rate of decline was greater during the pandemic period (slope, –5.74 [95% CI, –10.5 to –0.96] per month). The monthly number of outpatient early medical abortions increased during the pre‐pandemic period (slope, 5.94 [95% CI, 5.34–6.34] per month); it declined during the first month of the pandemic (slope, –26.4 [95% CI, –70.1 to –17.3] per month), but did not significantly change thereafter. The total monthly number of abortions during the pandemic period did not deviate markedly from the pre‐pandemic median value. The pre‐pandemic declines in monthly numbers of abortions in major city hospitals, in private hospitals, or at earlier than 14 weeks’ gestation intensified during the pandemic period. During January 2015 – March 2020, 14 634 of 103 496 abortions were outpatient medical abortions (14%); during the pandemic period, 11 154 of 33 056 abortions were outpatient medical abortions (33%).
Conclusions: The use of outpatient early medical abortion has steadily increased in Victoria since the PBS listing of mifepristone–misoprostol, which helped ensure access to abortion during the COVID‐19 pandemic. Outpatient medical abortions may eventually outnumber surgical early abortions in Victoria, but they are not always appropriate: hospitals will continue to be essential for comprehensive abortion care.