The known: The Australian National Reform Program increased the overall organ donation rate from 12.1 donors per million population in 2008 to 21.6 donors per million population in 2019. Its impact on donations by children has not been examined.
The new: Median organ donation rates for children under 16 years of age were not higher during reform period than during the years preceding the reform.
The implications: To increase the number of consented potential donors under 16 years of age, the specific needs of the families of dying children must be taken into account, as strategies used in adult intensive care seem relatively ineffective.
Solid organ transplantation is the only treatment for people with end‐stage organ failure. Unfortunately, the number of people waiting for transplants exceeds that of donated organs. In 2019, there were 548 deceased organ donors and 1444 transplant recipients in Australia; 1700 people were on waiting lists, and an estimated 12 000 required dialysis.1 Children more frequently develop complications or die while waiting for organs than adults or teenagers, partly because they need size‐matched organs.2 Only a small proportion of organ donors are children,3 and, despite technological advances in support for people waiting for organs, mortality among children waiting for donor hearts is 8–17%.4 Increasing the number of donor organs from children would benefit people on waiting lists of all ages; children often need size‐matched organs, but kidneys donated by children are frequently used for transplantation in adults.5,6
To improve organ donation rates, the Australian government introduced, in an iterative process, the National Reform Program for organ and tissue donation in 2008. The program established a national coordinating organisation, the Organ and Tissue Authority, which employs dedicated nursing and medical donation specialists in hospitals to implement best practices for identifying potential donors and approaching families for organ donations. It also collects data to assess performance and report outcomes to inform clinical practice change.7 The National Reform Program has been successful; the overall organ donor rate increased in Australia from 12.1 donors per million population in 2008 to 21.6 donors per million population in 2019, and the number of kidney transplantations almost doubled.8,9 The effect of the program on organ donation by children, however, has not been specifically assessed. We therefore compared rates of organ donation by children under 16 years of age with those for people aged 16 years or more during 2000–2019. We also analysed the characteristics of child donors during this period to identify any changes since the start of the program.
Methods
We conducted a retrospective observational time series study, analysing data from the Australia and New Zealand Organ Donation Registry (ANZOD; https://www.anzdata.org.au/anzod) for all Australian children who were consented potential organ donors during 1 January 2000 – 31 December 2019. Child donors were defined as those under 16 years of age, the general age cut‐off for admission to a paediatric intensive care unit. Consented potential deceased organ donors include actual and intended donors. An actual donor is one whose family has provided consent and the person has undergone surgery for donation; an intended donor is one whose family has provided consent, but the donation process stopped prior to surgical incision. The definition of an intended donor remained the same throughout the study period. In order to compare donor rates and donor characteristics before and after the National Reform Program, we divided the study period into two periods: 2000–2008 (pre‐reform) and 2009–2019 (reform period). Annual donor rates were compared with those for donors aged 16 years or more, derived from ANZOD annual reports (https://www.anzdata.org.au/anzod/publications‐2/annual‐reports).
Statistical analysis
We calculated annual organ donor rates (donors per million population) during 2000–2019 for people under 16 years and those aged 16 years or more, based on Australian Bureau of Statistics population numbers by year10 (Supporting Information, table 1). We estimated incidence rate ratios (IRRs) with 95% confidence intervals (CIs) and changes for the two age groups and the two time periods in standard Poisson regression models fitted to donor numbers, with year as a continuous variable and log population (denominator) as an offset term. Changes in rates are reported as mean annual percentage changes (with 95% CIs), calculated from the exponential of the beta coefficient for year.
The characteristics available for descriptive analyses for donors under 16 years of age were age, gender, weight, actual or intended donor, and cause of death. We also stratified donors by weight category and donation pathway (donation following neurological determination of death, or donation following circulatory determination of death).
The statistical significance of between‐group differences was assessed in two‐sided non‐parametric tests: Wilcoxon rank‐sum tests for continuous outcomes, Fisher exact tests for categorical outcomes. P < 0.05 was deemed statistically significant. Analyses were conducted in R for Windows (R Foundation for Statistical Computing) 4.1.0.
Ethics approval
The Sydney Children's Hospitals Network human research ethics committee approved the study and waived the requirement for individual consent (HREC reference 2020/ETH01700).
Results
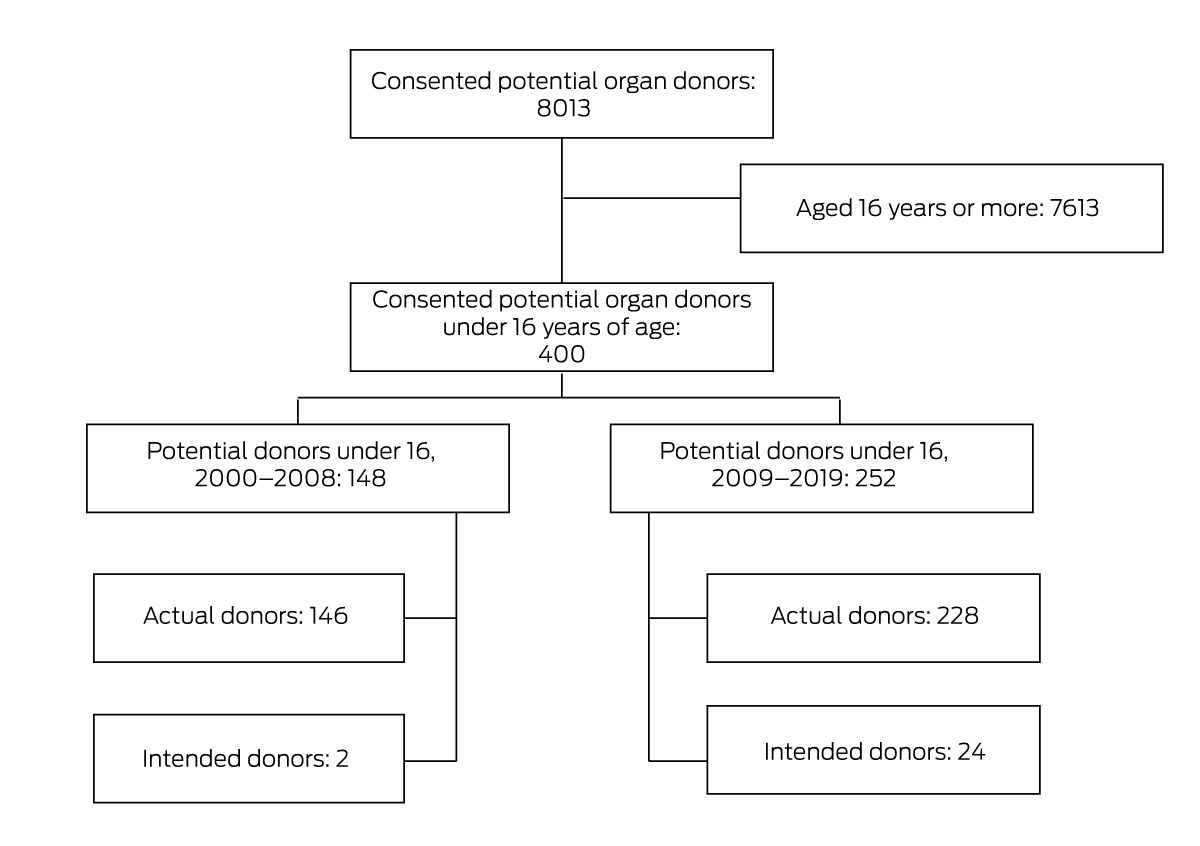
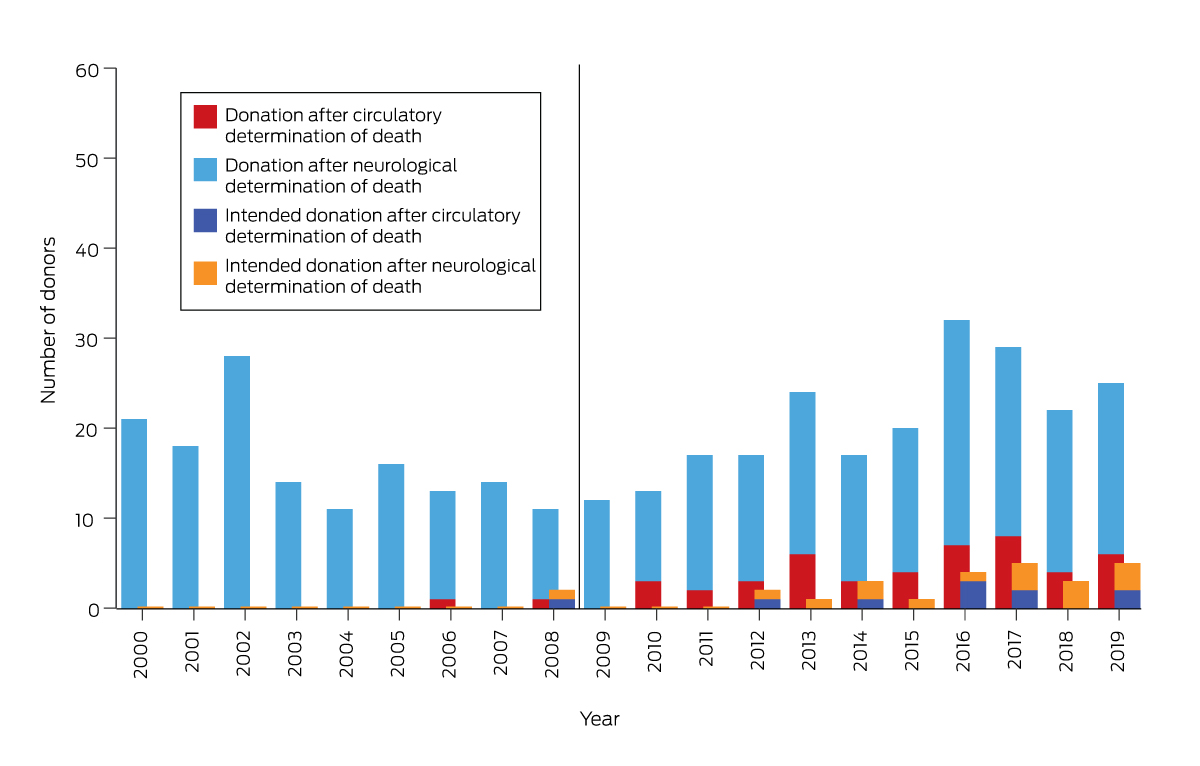
During 1 January 2000 – 31 December 2019, 400 children under 16 years of age were consented potential deceased organ donors, of whom 374 were actual deceased donors (94%). During 2000–2008, there were 146 actual deceased donors (median, 14 donors per year; interquartile range [IQR], 13–18 donors per year); during 2009–2019, there were 228 actual deceased donors (median, 20 donors per year; IQR, 17–25 donors per year) (Box 1, Box 2). The first donation following circulatory determination of death was in 2006, and the number of donors in this donation pathway remained low in subsequent years (maximum: eight donors in 2017). The first intended child donor was reported in 2008, and the numbers in both the neurological and circulatory determination of death pathways remained low during 2009–2019 (Box 2).
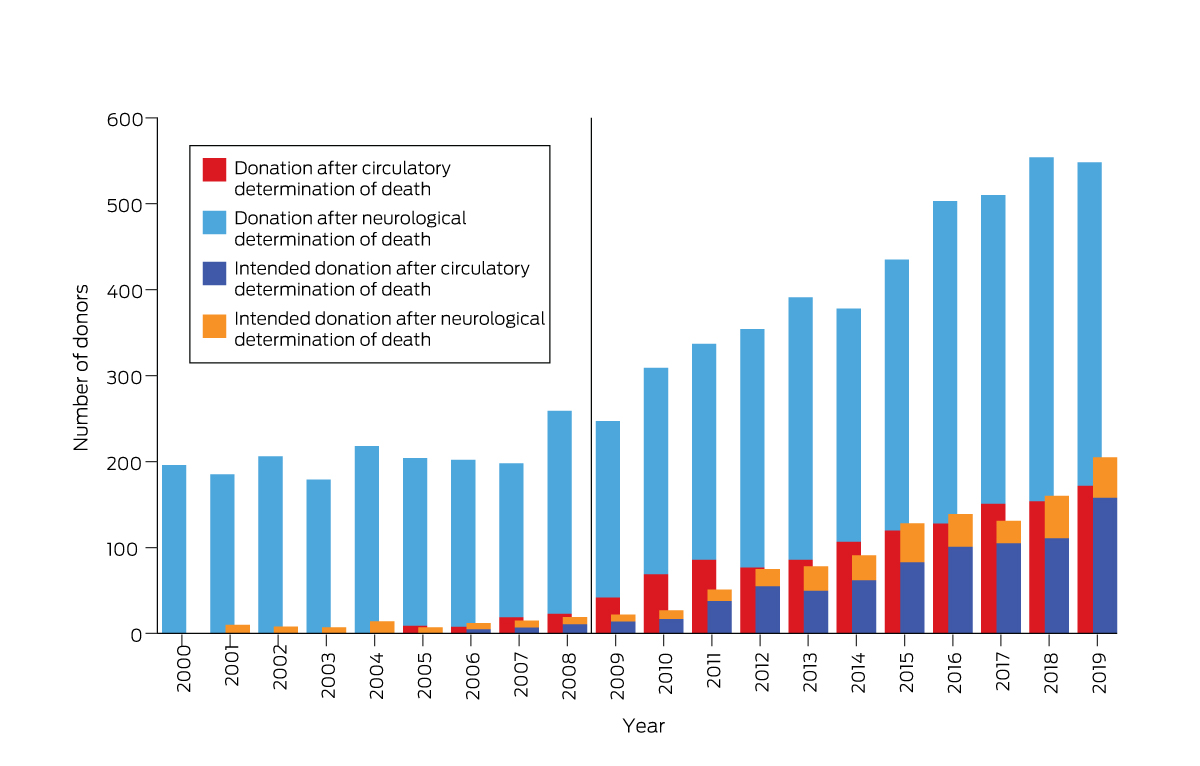
Of the 7613 consented potential deceased organ donors aged 16 years or more, 6413 became actual deceased donors (84.2%): 1847 during 2000–2008 (median, 202 donors per year; IQR, 197–215 donors per year), 4566 during 2009–2019 (median, 391 donors per year; IQR, 346–507 donors per year) (Box 3).
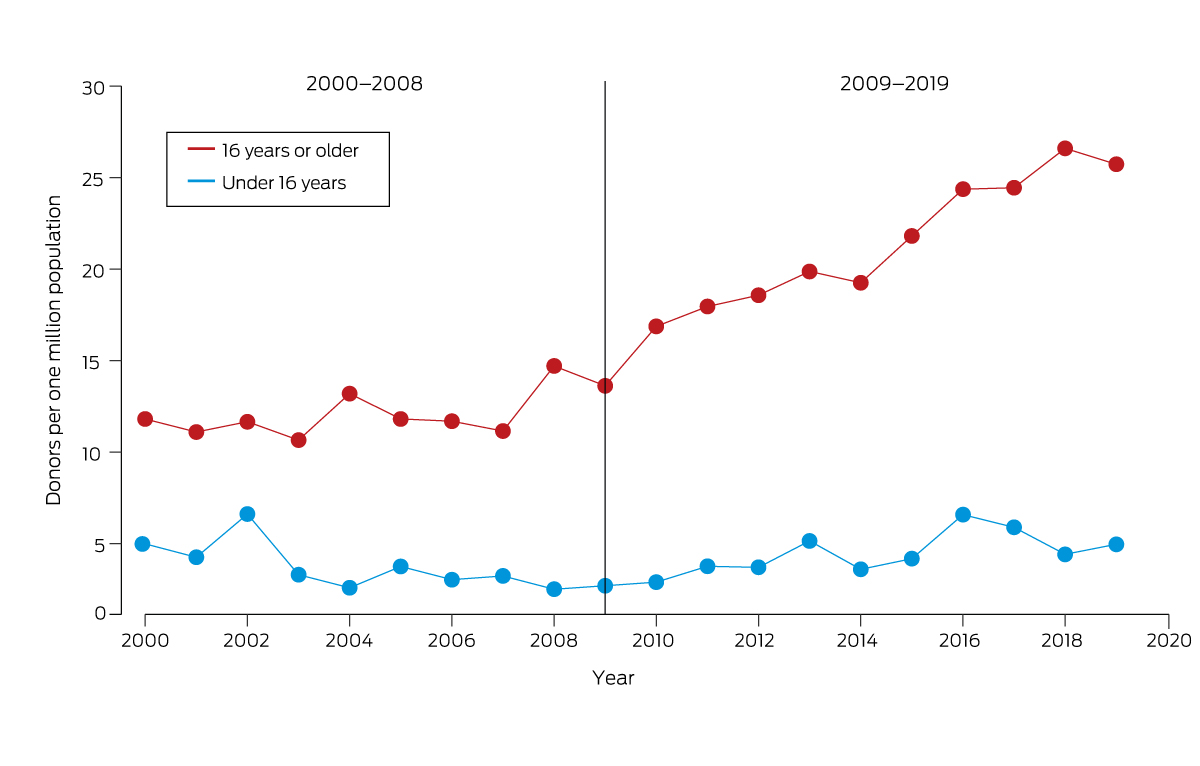
For donors under 16 years of age, the median annual incidence was 3.3 (IQR, 3.0–4.3) actual donors per million population during 2000–2008 and 4.2 (IQR, 3.6–5.2) donors per million population during 2009–2019 (IRR, 1.15; 95% CI, 0.93–1.42). For donors aged 16 years or more, the median annual incidence was 11.7 (IQR, 11.2–11.8) actual donors per million population during 2000–2008 and 19.9 (IQR, 18.3–24.4) donors per million during 2009–2019 (IRR, 1.75; 95% CI, 1.66–1.85).
In regression analyses, child organ donation rates declined by 8.3% (95% CI, –14% to –2.3%) per year during 2000–2008 and increased by 6.1% (95% CI, +1.8% to +11%) per year during 2009–2019 (Box 4). Annual donation rates by people aged 16 years or more did not significantly change during 2000–2008 (+0.9% per year; 95% CI, –0.8 to +2.7% per year) and increased during 2009–2019 by 5.9% (95% CI, +5.0% to +6.9%) per year.
Characteristics and pathways of actual organ donors
The median age of actual organ donors was similar during 2000–2008 (11 years; IQR, 7–14 years) and 2009–2019 (10 years; IQR, 4–14 years), as was their median weight (2000–2008: 37.5 kg; IQR, 25–55 kg; 2009–2019: 30 kg; IQR, 18–55 kg) (Box 5). The proportion of donors under 10 kg weight was twice as high during 2009–2019 (14 of 228, 6%) as during 2000–2008 (four of 146, 3%). During 2000–2008, traumatic brain injury was the most frequent cause of death for actual donors (71 of 146, 49%); during 2009–2019, it was cerebral hypoxia or ischaemia (111 of 228; 49%). Non‐neurological conditions were the causes of death for 24 children during 2000–2008 (16%) and 26 during 2009–2019 (11%). Two donations followed circulatory determination of death during 2000–2008 (1% of actual donations) and 46 during 2009–2019 (20%) (Box 6).
Intended organ donors
The proportion of children for whom consent for organ donation was provided but donation did not proceed was higher during 2009–2019 (24 of 252 [including eight girls], 9.5%) than during 2000–2008 (two of 148 [both girls], 1.4%). The median age of intended donors was one year (IQR, 0–2 years) during 2000–2008 and two years (IQR, 0–15 years) during 2009–2019. Eighteen of the intended donors during 2009–2019 weighed 10 kg or more (75%) (Supporting Information, table 2). Information about the planned donor pathway was available only for eighteen intended donors during 2009–2019; six were donors in the circulatory determination of death pathway.
Discussion
Following the 2009 introduction of the National Reform Program for organ donation in Australia, the organ donor rate increased significantly. However, the median annual donor rate for people under 16 years of age was no higher during the first eleven years of the reform than during the nine years preceding it. Prior to the program, donor rates in this age group had been falling — possibly reflecting declining child mortality during 1998–201611,12 — but they slowly increased from 2009. Our finding that the general reform program did not increase the overall number of child donors is similar to the outcome of the Organ Donation Breakthrough Collaborative in the United States, which effetively increased the number of adult donors, but not that of donors under 18 years of age.13
The median age of donors under 16 years of age was similar before and after the reform, but the proportion weighing less than 10 kg was larger during 2009–2019. The number of intended and actual donors following circulatory determination of death was higher after the reform, suggesting that the criteria for considering child donors had shifted. The numbers of intended and actual donors in this pathway has generally increased in Australia.14 This is unsurprising, as one of the primary objectives of the reform was to increase donation following circulatory determination of death and to promote acceptance in the transplantation community of renal grafts from donors not meeting standard criteria.6 Before the reform, organ donation after circulatory determination of death in children was rare in Australia, the first taking place in 2006. Despite the post‐reform increase in donations by children after circulatory determination of death, donations in this pathway remain infrequent, as also in countries such as Spain and Canada.15 Some intensivists may be less likely to recognise the possibility of donation by patients for whom death is unlikely to be determined using neurological rather than circulatory criteria. Alternatively, the lack of certainty in predicting time to death may discourage some clinicians from initiating conversations with families about organ donation.16 Our findings suggest that recognition in Australia of potential organ donation following circulatory determination of death of children under 16 years of age is still relatively low. Donation sector clinicians should work with paediatric intensive care teams to promote recognition of potential donors by this pathway.
One difficulty in analysing data on child organ donors is that variation in annual donor numbers is greater than for older donors. This variability is attributable to several linked factors: relatively low child mortality and variations in causes of death,12 problems with potential donor identification, and varying family consent rates. Discussions of organ donation are complex and sensitive conversations, and consent needs to be an enduring decision for the child's parents. For people over 16 years of age, a registered wish to become an organ donor empowers the family to proceed, and consent rates are as high as 90% in such cases.17 Discussing organ donation by children is more difficult.18 One challenge is that few families believe their young child could have an opinion about organ donation, although children as young as seven years can express the wish to be donors.19 Further, many families are unaware that organ donation for children is possible.20 Public awareness campaigns may influence parental consent rates, giving families courage to ask whether organ donation is possible for their dying child.21 In 2016, for example, twenty Australian families asked about donations by their children, compared with a prior mean annual of ten such conversations (personal communication, Mark McDonald, Organ Transplantation Authority, January 2022). In the same year, a public awareness campaign had featured a story about a child donor.22 Whether this campaign influenced the number of conversations cannot be determined, but campaigns featuring organ donations by children have been infrequent.
Limitations
Causal relationships cannot be derived from our retrospective observational study. We do not know the overall size of the potential organ donor pool during the study period and consequently the number of children under 16 years of age eligible to be potential donors. The data we analysed were not collected with our study aim in mind and were therefore not tailored to our research questions. Further, the small numbers of young donors may have precluded the detection of statistically significant associations.
Conclusion
We report the first study to examine rates of organ donation by Australian children under 16 years of age based on the size of the age‐specific population, rather than in relation to the number of deaths of children in intensive care units.23 Our findings suggest that, despite its overall effect on organ donation rates, the National Reform Program was not effective in increasing the numbers of donations by children. Relying on broad initiatives that work with adults may not be appropriate. Future studies should assess how potential child donors were identified, families approached, and donor organs used during the National Reform Program, so that its strategies might be adjusted to meet the meets of the paediatric intensive care clinicians and to help increase donor rates (Box 7).
Box 1 – Australian children who were consented potential organ donors (consent provided), 1 January 2000 – 31 December 2019
Box 5 – Weight distribution of actual organ donors (under 16 years of age), Australia, 2000–2019
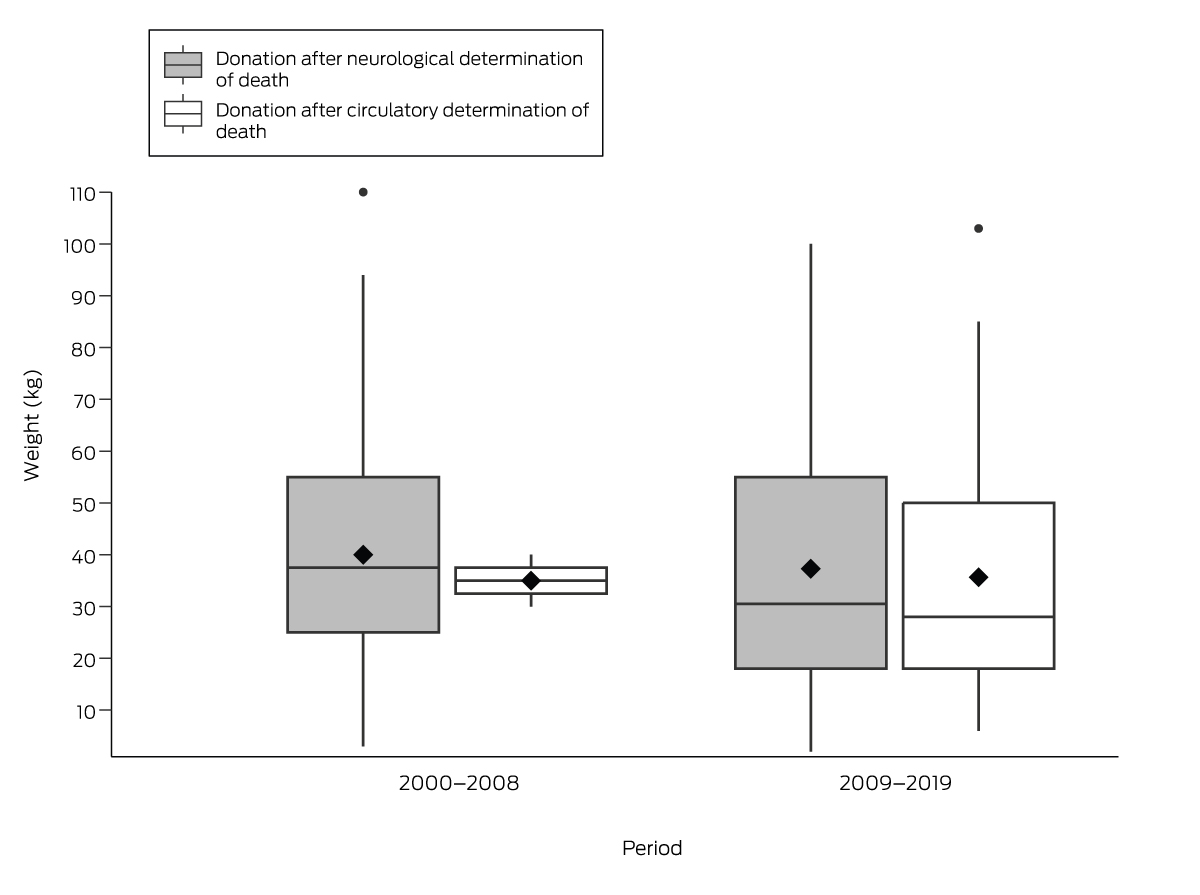
The horizontal line within each box depicts the median, the horizontal boundaries of the box the interquartile range; the diamond depicts the mean value; the whiskers depict the 25th and 75th centiles; the dots depict outliers.
Box 6 – Characteristics of actual organ donors (under 16 years of age), Australia, 2000–2019
|
|
2000–2008 |
2009–2019 |
|||||||||||||
|
Characteristic |
Neurological determination of death |
Circulatory determination of death |
Neurological determination of death |
Circulatory determination of death |
|||||||||||
|
|
|||||||||||||||
|
Number |
144 |
2 |
182 |
46 |
|||||||||||
|
Age (years), median (IQR) |
11 (7–13.5) |
11.5 (9–14) |
10 (4–14) |
10.5 (3–14) |
|||||||||||
|
Gender (boys) |
93 (65%) |
1 (50%) |
104 (57%) |
26 (56%) |
|||||||||||
|
Weight (kg), median (IQR) |
37.5 (25–55) |
35 (30–40) |
30.5 (18–55) |
28 (18–50) |
|||||||||||
|
20 kg or greater |
120 (83%) |
2 (100%) |
133 (73%) |
32 (70%) |
|||||||||||
|
10 kg to < 20 kg |
20 (14%) |
0 |
37 (20%) |
12 (26%) |
|||||||||||
|
5 kg to < 10 kg |
3 (2%) |
0 |
8 (4%) |
2 (4%) |
|||||||||||
|
< 5 kg |
1 (1%) |
0 |
4 (2%) |
0 |
|||||||||||
|
Cause of death |
|
|
|
|
|||||||||||
|
Cerebral hypoxia/ischaemia |
26 (18%) |
0 |
89 (49%) |
22 (48%) |
|||||||||||
|
Traumatic brain injury |
71 (49%) |
0 |
51 (28%) |
10 (22%) |
|||||||||||
|
Intracranial haemorrhage |
23 (16%) |
1 (50%) |
17 (9%) |
4 (9%) |
|||||||||||
|
Cerebral infarct |
1 (1%) |
0 |
2 (1%) |
2 (4%) |
|||||||||||
|
Other neurological condition |
0 |
0 |
3 (2%) |
2 (4%) |
|||||||||||
|
Non‐neurological condition |
23 (16%) |
1 (50%) |
20 (11%) |
6 (13%) |
|||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range. * Donor rates by year and pathway are included in the Supporting Information, table 1. |
|||||||||||||||
Box 7 – Differences between organ donation by children and adults in Australia
Donor identification
- The Organ and Tissue Authority Best practice guideline for offering organ donation24 states that DonateLife (https://www.donatelife.gov.au) should be notified about all patients at the end of life in intensive care units and emergency departments. However, there has been no specific engagement with paediatric intensive care units to ensure that these processes meet the needs of families and hospital staff.
- The Organ and Tissue Authority guideline24 states that all discussions with families about organ donation should include a donation specialist to ensure a fully informed conversation. Paediatric health intensivists frequently develop close professional relationships with the families of critically ill children and may be uncomfortable involving a donation specialist. Specific engagement with paediatric intensive care units is needed to ensure that these processes meet the needs of families and hospital staff.
- Family donation conversation training courses25 have been designed to primarily meet the needs of staff who work with adult donors and families. There is no specific course for staff who work in paediatric intensive care units.
- Several national and state community campaigns have promoted organ and tissue donation, but none have provided information about organ and tissue donation by children.
- The Kidney Donor Profile Index26 is used to assess the quality of renal grafts from adult donors. The index negatively weights the calculation if the kidney is donated by a child, despite evidence that such renal grafts are more successful than organs from extended criteria donors.5
- The Transplant Society of Australia and New Zealand Clinical guidelines for organ transplantation from deceased donors6 provide guidance for assessing adult donors, but child donor assessment is included only as an appendix to the document.
- Organ perfusion machines are available for organs from donors weighing at least 50 kg.
- Neonatal renal grafts could expand the renal donor pool, but no programs routinely accept neonatal renal grafts in Australia.
Received 31 August 2022, accepted 30 March 2023
- Tal T Klein1
- Michael J O'Leary2
- Lukas Staub3
- Elena Cavazzoni2
- 1 Children's Hospital at Westmead, Sydney, NSW
- 2 NSW Organ and Tissue Donation Service, Sydney, NSW
- 3 Talus Research Consulting, Sydney, NSW
No relevant disclosures.
- 1. Australian and New Zealand Organ Donation Registry. 2019 organ waiting list. https://www.anzdata.org.au/anzod/publications‐2/organ‐waiting‐list (viewed Jan 2022).
- 2. Yoo PS, Olthoff KM, Abt PL. Donation after cardiac death in pediatric organ transplantation. Cur Opin Organ Transplant 2011; 16: 483‐488.
- 3. NHS Blood and Transplant. Organ donation and transplantation activity report 2019/20. https://nhsbtdbe.blob.core.windows.net/umbraco‐assets‐corp/19481/activity‐report‐2019‐2020.pdf (viewed Jan 2022).
- 4. Almond CSD, Thiagarajan RR, Piercey GE, et al. Waiting list mortality among children listed for heart transplantation in the United States. Circulation 2009; 119: 717‐727.
- 5. Suneja M, Kuppachi S, Katz D, Hunsicker L. Small split pediatric kidneys to expand the donor pool: an analysis of scientific registry of transplant recipients (SRTR) data. Transplantation 2019; 103: 2549‐2557.
- 6. Transplant Society of Australia and New Zealand. Clinical guidelines for organ transplantation from deceased donors; version 1.10. Oct 2022. https://tsanz.com.au/storage/documents/TSANZ_Clinical_Guidelines_Version‐110_Final.pdf (viewed Mar 2023).
- 7. Australian National Audit Office. Organ and tissue donation: community awareness, professional education and family support, performance audit report 2015. 29 Apr 2015. https://www.anao.gov.au/work/performance‐audit/organ‐and‐tissue‐donation‐community‐awareness‐professional‐education‐and (viewed Jan 2022).
- 8. Australian and New Zealand Organ Donation Registry. ANZOD registry report 2009. https://www.anzdata.org.au/report/anzod‐annual‐report‐2009 (viewed Jan 2022).
- 9. Organ and Tissue Authority. 2019 Australian donation and transplantation activity report. 26 Feb 2020. https://www.donatelife.gov.au/sites/default/files/2021‐05/ota_2019activityreport_2020017.pdf (viewed Jan 2022).
- 10. Australian Bureau of Statistics. 3101.0. Australian demographic statistics, Jun 2019. Table 59: estimated resident population by single year of age, Australia. 19 Dec 2019. https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3101.0Jun%202019?OpenDocument (viewed Jan 2021).
- 11. Australian Institute of Health and Welfare. Australia's children (Cat. no. CWS 69). Canberra: AIHW, 2020. https://www.aihw.gov.au/getmedia/6af928d6‐692e‐4449‐b915‐cf2ca946982f/aihw‐cws‐69‐print‐report.pdf (viewed Jan 2022).
- 12. Moynihan KM, Alexander PMA, Schlapbach LJ, et al; Australian and New Zealand Intensive Care Society Pediatric Study Group; ANZICS Centre for Outcome and Resource. Epidemiology of childhood death in Australian and New Zealand intensive care units. Intensive Care Med 2019; 45: 1262‐1271.
- 13. Godown J, McKane M, Wujcik K, et al. Expanding the donor pool: regional variation in pediatric organ donation rates. Pediatr Transplant 2016; 20: 1093‐1097.
- 14. Australia and New Zealand Organ Donation Registry. ANZOD Registry Report 2020. https://www.anzdata.org.au/report/anzod‐annual‐report‐2020 (viewed Jan 2022).
- 15. Weiss MJ, Domínguez‐Gil B, Lahaie N, et al; Canadian Critical Care Trials Group. Development of multinational registry of pediatric deceased organ donation activity. Pediatr Transplant 2019; 23: e13345.
- 16. Bennett EE, Sweney J, Aguayo C, et al. Pediatric organ donation potential at a children's hospital. Pediatr Crit Care Med 2015; 16: 814‐820.
- 17. Radford S, D'Costa R, Opdam H, et al. The impact of organ donation specialists on consent rate in challenging organ donation conversations. Crit Care Resusc 2020; 22: 297‐302.
- 18. Gelbart B. Challenges of paediatric organ donation. J Paediat Child Health 2017; 53: 534‐539.
- 19. Rajchandra S. #doitforDeyaan: Saffron Day honours the life of little Deyaan Udani. 2023. https://saffronday.org (viewed Jan 2022).
- 20. RCH National Child Health Poll. Organ donation: Do families know the facts? 30 Oct 2019. https://www.rchpoll.org.au/polls/organ‐donation‐do‐families‐know‐the‐facts (viewed Jan 2022).
- 21. Palmer M. The role of families in organ donation: international evidence review. Cardiff: Welsh Government Social Research, 2012. https://gov.wales/sites/default/files/statistics‐and‐research/2019‐08/121203familiesorgandonationen.pdf (viewed Jan 2022).
- 22. Transplant Australia. Gifted campaign. Updated 2019. https://transplant.org.au/gifted‐campaign (viewed Jan 2022).
- 23. Corkery‐Lavender T, Millar J, Cavazzoni E, Gelbart B. Patterns of organ donation in children in Australia and New Zealand. Crit Care Resusc 2017; 19: 296‐302.
- 24. Organ and Tissue Authority. Best practice guideline for offering organ and tissue donation in Australia. Edition 2. Apr 2021. https://www.donatelife.gov.au/sites/default/files/2021‐05/final_best_practice_guideline_for_offering_organ_and_tissue_donation_apr2021.pdf (viewed Mar 2023).
- 25. Organ and Tissue Authority. Core family donation conversation (FDC) workshop. 2023. https://www.donatelife.gov.au/for‐healthcare‐workers/professional‐training/core‐family‐donation‐conversation‐fdc‐workshop (viewed Mar 2023).
- 26. Israni AK, Salkowski N, Gustafson S, et al. New national allocation policy for deceased donor kidneys in the United States and possible effect on patient outcomes. J Am Soc Nephrol 2014; 25: 1842‐1848.





Abstract
Objectives: To assess the impact of the 2009 National Reform Program for organ donation in Australia on the number and characteristics of organ donors under 16 years of age.
Design, setting, participants: Retrospective observational time series study; analysis of Australia and New Zealand Organ Donation (ANZOD) registry data for all consented potential deceased organ donors under 16 years of age during 2000–2019, and of numbers of donors aged 16 years or more reported in ANZOD annual reports.
Main outcome measures: Difference between 2000–2008 (pre‐reform) and 2009–2019 (reform period) in annual organ donor rates (donors per million population), by age group (under 16 years, 16 years or more), reported as incidence rate ratio (IRR). Secondary outcomes: Differences in child donor characteristics during 2000–2008 and 2009–2019.
Results: During 2000–2019, 400 children under 16 years of age were consented potential deceased organ donors, of whom 374 were actual deceased donors (94%): 146 during 2000–2008, 228 during 2009–2019. The median annual rate was 3.3 (interquartile range [IQR], 3.0–4.3) actual donors per million population during 2000–2008 and 4.2 (IQR, 3.6–5.2) donors per million population during 2009–2019 (IRR, 1.15; 95% confidence interval [CI], 0.93–1.42). In contrast, the difference between the two periods was statistically significant for donors aged 16 years or more, rising from 11.7 (IQR, 11.2–11.8) to 19.9 (IQR, 18.3–24.4) actual donors per million population (IRR, 1.75; 95% CI, 1.66–1.85). The median age of actual organ donors under 16 was similar during 2000–2008 (11 years; IQR, 7–14 years) and 2009–2019 (10 years; IQR, 4–14 years), as was the proportion of donors in this age group under 10 kg (2000–2008: four of 146, 3%; 2009–2019: 14 of 228, 6%).
Conclusions: Despite its overall effect on organ donation rates, the National Reform Program was not effective in increasing the numbers of donors under 16 years of age. Relying on broad initiatives for adult donors may not be appropriate for achieving this aim.