Culling low value care will cut health care carbon emissions
We are in a health emergency precipitated by climate change.1 As well as physical health threats, climate change and its effects are adversely affecting Australians’ mental health,2 and worsening the health inequities suffered by vulnerable populations.
In response, the Australian health care community must both adapt to increased demand and to deteriorating environmental conditions, and mitigate the carbon footprint of health care, currently 7% of our national carbon emissions.3 Using economic data from 360 sectors, Malik and colleagues estimated carbon emissions by Australian Institute of Health and Welfare categories of health care expenditure, finding that the hospital and pharmaceutical sectors had the largest footprints, together accounting for 63% of health care emissions. Of note, 90% of Australia’s health care emissions are indirect, stemming from the extensive national and global supply chains involved in the manufacture, distribution and provision of health care goods and services.3 Similarly, a more detailed United Kingdom breakdown revealed that emissions from building energy, water and sanitation together accounted for less than 20% of health care emissions, with the remainder coming from pharmaceuticals, medical devices, equipment and their supply chains, anaesthetic gases, metered dose inhalers, staff, patient and visitor travel, and other goods and services for patient care.4 In short, the business of clinical care itself.
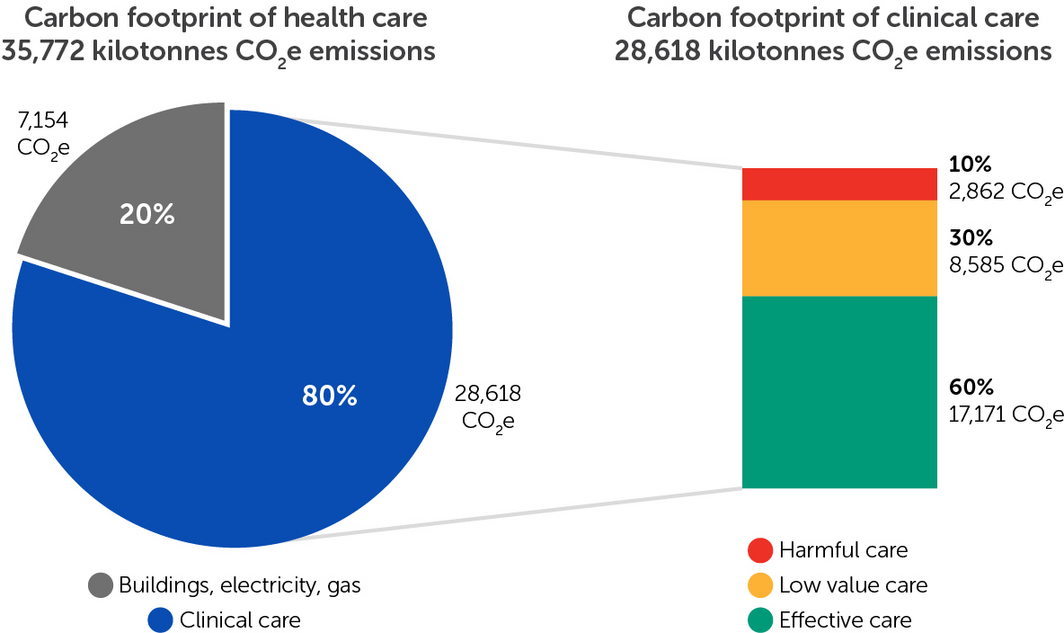
As we face the unprecedented challenge of climate change, it is widely acknowledged that much health care is wasteful and low value. Low value care remains stubbornly common and may be increasing, including in low and middle income countries.5 Recent estimates show that about 30% of health care is wasteful or low value, and a further 10% is harmful.6 Using these data, we can make explicit the carbon cost of low value and harmful health care in Australia (Box).
Greening hospitals’ electricity and water supplies and ending use of fossil gas is essential, but clearly changes to models of clinical care are also needed. This is where two key challenges to health system sustainability — low value care and climate risk — intersect, and why better value, low carbon emissions models of clinical care are urgently needed.
It can be hard to define and measure low value and harmful care, as evidence of a test or treatment’s benefit may be lacking and harms may be incompletely measured.5 It is clear, however, that many laboratory tests are overused, with vitamin D testing providing a good example.7 There were at least 80 million haematology, biochemistry and immunology tests requested in the community in 2020,8 of which an estimated 10–40% were likely unnecessary.10 Substantial carbon10 (and financial) savings could be achieved by omitting unnecessary pathology tests, without any detriment to health.
We do not intend to single out pathology for criticism, as pathologists have shown leadership in greening laboratory practice. Rather, we highlight that no matter how green the pathology laboratory, low value health care has a sizeable footprint, wherever it occurs.
The widespread occurrence of low value care helps explain why the carbon footprint of Australian health care is so large, representing almost half that of the entire construction sector (residential and non‐residential).3
The 60% of care that is effective care6 is critically important and will become ever more so as climate change unfolds. We must prioritise decarbonised energy and low carbon options, for example, by switching away from desflurane and nitrous oxide anaesthetic gases, which have large footprints.11 However, these changes will take time.
One thing that can be done today is a cull of low value care. That alone would save Australia over 8000 kilotonnes of carbon dioxide equivalent emissions per year (Box). It will require a whole of system approach, with macro (government), meso (organisational) and micro (individual) level elements. At the macro level, government regulatory agencies must continue to strengthen reform efforts such as the Medicare Benefits Schedule review, while also requiring manufacturers and sponsors to provide evidence of their products’ environmental impacts as well as costs and health effects, and using their purchasing power to preference carbon neutral suppliers. At the meso level, hospitals, health departments and professional colleges can institute training schemes and support clinical sustainability fellows to advance better value, low carbon health care. A model where registrars divide their time between their clinical role and sustainability projects is operating successfully in the United Kingdom (https://sustainablehealthcare.org.uk/who‐we‐are/fellows‐and‐scholars). At the micro level, individual clinicians can demonstrate local leadership by recognising the footprint of low value care and refusing to provide it, acting as a role model to those around them.
This article was published as a peer‐reviewed Accepted Article (prior to structural editing and typesetting) on 26 October 2021.
Provenance: Not commissioned; externally peer reviewed.
- 1. Beggs PJ, Zhang Y, McGushin A, et al. The report of the MJA–Lancet Countdown on health and climate change: Australia increasingly out on a limb. Med J Aust 2021; https://doi.org/10.5694/mja2.51302.
- 2. Cunsolo A, Ellis NR. Ecological grief as a mental health response to climate change‐related loss. Nat Clim Chang 2018; 8: 275–281.
- 3. Malik A, Lenzen M, McAlister S, et al. The carbon footprint of Australian health care. Lancet Planet Health 2018; 2: e27–e35.
- 4. Tennison I, Roschnik S, Ashby B, et al. Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health 2021; 5: e84–e92.
- 5. Brownlee SM, Chalkidou KMD, Doust JP, et al. Evidence for overuse of medical services around the world. Lancet 2017; 390: 156–168.
- 6. Braithwaite J, Glasziou P, Westbrook J. The three numbers you need to know about healthcare: the 60–30‐10 Challenge. BMC Med 2020; 18: 102–02.
- 7. Gordon L, Waterhouse M, Reid IR, et al. The vitamin D testing rate is again rising, despite new MBS testing criteria. Med J Aust 2020; 213: 155–155.e1. https://www.mja.com.au/journal/2020/213/4/vitamin‐d‐testing‐rate‐again‐rising‐despite‐new‐mbs‐testing‐criteria
- 8. Services Australia. Medicare group reports. http://medicarestatistics.humanservices.gov.au/statistics/mbs_group.jsp (viewed Oct 2021).
- 9. Zhi M, Ding EL, Theisen‐Toupal J, et al. The landscape of inappropriate laboratory testing: a 15‐year meta‐analysis. PLoS One 2013; 8: e78962.
- 10. McAlister S, Barratt AL, Bell KJL, McGain F. The carbon footprint of pathology testing. Med J Aust 2020; 212: 377–382.e1. https://www.mja.com.au/journal/2020/212/8/carbon‐footprint‐pathology‐testing
- 11. McGain F, Muret J, Lawson C, et al. Environmental sustainability in anaesthesia and critical care. Br J Anaesth 2020; 125: 680–692.






Alexandra Barratt received funding from the National Health and Medical Research Council (grant no. 1104136).
No relevant disclosures.