The known: Access to early medical abortion can be difficult, particularly for women in rural and regional Australia. Providing it through primary care would be ideal, but the distribution of medical practitioners who provide early medical abortion services is unclear.
The new: We found that rates of early medical abortion are highest outside metropolitan centres, but about 30% of women live in areas in which it had not been prescribed by a local general practitioner during 2019.
The implications: General practitioners should be supported to enable them to provide early medical abortion services.
Abortion, both surgical and medical, is an essential healthcare service. Early medical abortion — using mifepristone and misoprostol to terminate a pregnancy — has been endorsed as safe and effective during early pregnancy by Australian and overseas peak medical bodies.1 In Australia, early medical abortion can be provided by telehealth or in person in primary care.2
Medical practitioners can register to provide early medical abortion services after undertaking online training delivered without cost by Marie Stopes Australia.3 If a practitioner holds a Fellowship or Advanced Diploma from the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG), they can register as prescribers without this training.1 Doctors in private practice or working with family planning organisations or Marie Stopes Australia can also provide early medical abortion. The locations of family planning and Marie Stopes clinics are publicly available, but national information on where general practitioners prescribe early medical abortion or pharmacists dispense the required drug has not been published.
Although the Therapeutic Goods Administration (TGA) approved mifepristone for use as a medical abortifacient during early pregnancy in 20121 and MS‐2 Step (composite regimen of mifepristone and misoprostol) has been subsidised by the Pharmaceutical Benefits Scheme since 2015,1 integration of early medical abortion into primary health care has been slow.4 In December 2020, only 2841 of 29 017 registered GPs were active prescribers of MS‐2 Step, and 5347 of 32 393 registered pharmacists were active dispensers.5
Several system, provider and patient factors have limited the integration of early medical abortion into general practice. Legislative differences have contributed to variations between Australian states and territories in its availability.1 Some GPs believe early medical abortion is not within their area of responsibility,4 while others lack training and awareness of how to provide it.6,7 Further, those who do provide the service can feel stigmatised and isolated, and speak of the need for peer support and supportive referral pathways.4,8 Fear of criminal prosecution for performing abortion and of potential complications have also been noted as barriers to GPs providing early medical abortion.4 Finally, many women are unaware that it is available or of the 63 days’ gestation eligibility limit; other barriers include needing to travel, take time off work, and to find childcare to access early medical abortion services, and many require financial support to pay for it.9
Access to abortion services can be difficult for women in rural and regional areas. Women in rural areas are 1.4 times as likely to experience an unintended pregnancy than women living in metropolitan areas, with contributory factors including geographic isolation, limited access to contraception services, and not knowing where these services are available.10 The cost is also a major barrier to access to early medical abortion, with a median out‐of‐pocket cost of $560.9
Understanding demographic differences in the provision of early medical abortion is crucial for tailoring interventions to improve access. We therefore assessed variability in early medical abortion availability and uptake in Australia, focusing on its provision in primary care.
Methods
We analysed aggregated data for all Pharmaceutical Benefits Scheme (PBS) claims for MS‐2 Step dispensing. The PBS is a federal government‐funded program that subsidises listed medicines dispensed by community pharmacies and private hospitals for all Australian citizens, permanent residents, and eligible foreign visitors (from countries with reciprocal healthcare agreements with Australia) medicines.11 In addition, the PBS subsidises medicines dispensed to public hospital outpatients and non‐admitted patients, as well as for inpatients on their discharge from hospital (in most, but not all, states after public hospital pharmaceutical reforms).11
Services Australia provided the number of MS‐2 Step prescriptions (PBS item 10211K) dispensed to women aged 15–54 years resident in each Australian Bureau of Statistics (ABS) level 3 statistical area (SA3) during the calendar years 2015–2019, irrespective of prescriber type or location, aggregated by ten‐year age group and year. MS‐2 Step is listed on the PBS for terminating intra‐uterine pregnancies of up to 63 days’ gestation. Services Australia also supplied the numbers by SA3 of MS‐2 Step prescriptions written by GPs and dispensed by pharmacists. Population data for each SA3 were derived from ABS data.12 SA3s provide a regional breakdown of Australia into areas that usually include populations of between 30 000 and 130 000 people. In urban centres, they are often closely aligned with local government areas; outside urban centres, they include areas recognised as sharing a distinct identity and socio‐economic characteristics.13
We calculated age‐standardised rates of MS‐2 Step dispensing to women of reproductive age in each SA3 for each year by applying the ABS 2001 standard population.14 We defined the magnitude of variation in dispensing for a given year as the ratio of the highest and lowest age‐standardised rates by SA3; we also calculated variation after excluding the 10% of SA3s with the lowest and the 10% with the highest age‐standardised rates. For these calculations, we excluded SA3s in which fewer than twenty prescriptions had been dispensed, those that included fewer than 1000 women of reproductive age, and SA3s in which any ten‐year age group (for women aged 15–54 years) included fewer than thirty women.
In the dataset provided by Services Australia, counts were suppressed if one to six prescriptions had been dispensed for a combination of SA3, age group, and year. In our analysis, we replaced the suppressed counts with a value of five prescriptions.
In a separate analysis, we included data from all SA3s to calculate age‐standardised rates for the 2019 calendar year by state and ABS remoteness area.15 We also calculated the numbers and proportions of SA3s in which MS‐2 Step had not been prescribed by a GP or dispensed by a community pharmacy during 2019, both unweighted and weighted by the number of women aged 15–54 years resident in the SA3. As population data by SA3 were not available for 2019, we used population data for 2018.12
Ethics approval
Formal ethics approval was not required for our analysis of de‐identified Services Australia data.
Results
During 2015–2019, the PBS subsidised 91 643 MS‐2 Step prescriptions. The national age‐standardised rate increased from 1.63 prescriptions per 1000 women aged 15–54 years in 2015 to 3.79 prescriptions per 1000 in 2019. The magnitude of variation in age‐standardised dispensing rates declined from 19 in 2015 to 9.8 in 2019, but was fairly steady if the SA3s in the highest and lowest rate deciles were excluded (2015, 3.4; 2019, 3.0) (Box 1).
In 2019, the age‐standardised dispensing rate was highest in the Northern Territory (7.16 MS‐2 Step prescriptions per 1000 women aged 15–54 years) and lowest in the Australian Capital Territory (3.15 per 1000) and New South Wales (3.23 per 1000). On a national basis, rates were higher in outer regional Australia (6.53 prescriptions per 1000 women aged 15‐54 years) and remote Australia (6.02 per 1000) than in major cities (3.30 per 1000) (Box 2, Box 3).
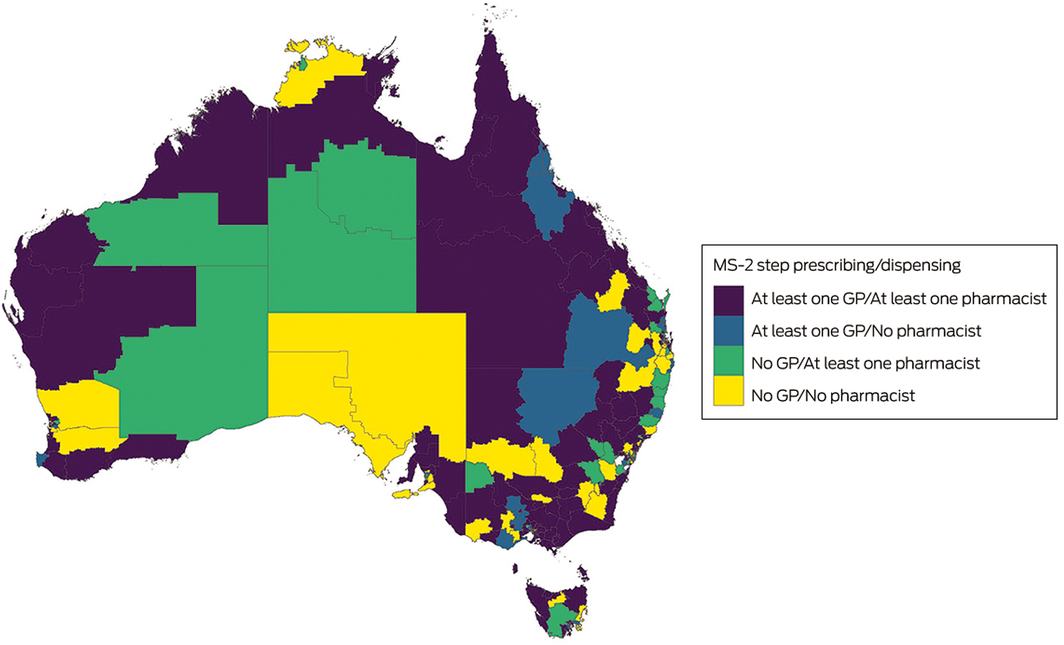
About 30% of women aged 15–54 years — and about 50% of those in remote Australia — lived in SA3s in which MS‐2 Step had not been prescribed by a GP during 2019; the proportion was highest in South Australia (64%) and New South Wales (40%) (Box 4). About 25% of women aged 15–54 years lived in areas in SA3s in which MS‐2 Step had not been dispensed by a community pharmacist; the proportion was highest in South Australia (46%) and the Australian Capital Territory (36%) (Box 5). In 74 of 338 SA3s (22%), MS‐2 Step was neither prescribed by a GP nor dispensed by a community pharmacist during 2019 (Box 6).
Discussion
We found that rates of early medical abortion are higher among women in outer regional, remote, and inner regional Australia than in major cities; however, MS‐2 Step had not been prescribed by GPs or dispensed by community pharmacists in a large proportion of SA3s in these geographic areas during 2019. Women may have travelled long distances to access early medical abortion, or received it using telehealth services. The reduction in the range of dispensing rates by SA3 between 2015 and 2019 suggests, however, that equitable provision of early medical abortion improved during this period.
Higher rates of early medical abortion in rural and remote areas could be explained by several factors. Women in these areas may have difficulty accessing surgical abortion, as many public hospitals do not provide it at all or only in cases of fetal abnormality,16 and private clinics providing surgical abortion are predominantly located in major cities.2 Further, many women choose telehealth early medical abortion services for a range of geographic, financial, and social reasons.17 During the study period, telehealth was available across Australia (except in South Australia) from private providers.17 Early medical abortion delivered by telehealth is highly acceptable and convenient for women because they can remain at home and manage their personal responsibilities, and because it satisfies their privacy needs.17,18 Concerns about privacy and confidentiality, and perceived stigmatisation by health professionals, may diminish the acceptability of obtaining early medical abortion from local providers.19
As the number of early medical abortions increased during 2015–2019, that of surgical abortions declined; claims for Medicare Benefits Schedule (MBS) item number 35643 (evacuation of the contents of the gravid uterus by curettage or suction curettage) declined from about 50 000 in 2015 to 40 000 in 2019.20 However, these numbers do not provide a complete account of surgical abortion in Australia, as the delivery of surgical abortion services differs between states.21
Restrictive laws have also limited access to early medical abortion in Australia, especially in rural and remote areas.2 Abortion was decriminalised in the Northern Territory in 2017, in Queensland in 2018, and in New South Wales in 2019.22 South Australia decriminalised abortion in 2021, permitting service delivery in primary care settings.22 Inconsistencies in knowledge of the law pertaining to abortion also discourage GPs from providing the service.2
We used the lack of MS‐2 Step prescribing by GPs in an SA3 as a surrogate marker of GPs not providing early medical abortion. However, that GPs had not prescribed and pharmacists had not dispensed MS‐2 Step in some rural and remote SA3s could have a number of explanations. Firstly, rural and regional doctors may have concerns about support services, including after‐hours emergency and surgical care in case of complications, and about access to ultrasound services (recommended for gestation dating and to exclude ectopic pregnancy8,23). They might also have been concerned about their capacity to provide anti‐D, but recently updated guidelines no longer recommend the routine use of RhD immunoglobulin in medical terminations before ten weeks’ gestation.1 Early medical abortion can proceed without ultrasound assessment after careful screening for risk factors for ectopic pregnancy and when the gestational age can be accurately estimated on the basis of the woman’s history.24 Secondly, many doctors conscientiously object to performing abortions, and some refuse to refer patients for such procedures, despite a legal obligation to do so.25 Thirdly, many GPs do not have the training or knowledge required to confidently provide early medical abortion.25 Finally, women may choose not to use local GP providers for abortion services.
These barriers to providing early medical abortion are compounded by the shortage of GPs in rural and remote areas.26 While financial incentives are frequently used to recruit and retain GPs in rural and remote areas, recent research suggests they play only a limited role in improving access to primary care.26 Other strategies are therefore required. Options include increasing the use of collaborative task‐sharing arrangements and models in which nurses undertake most of the counselling, administration and follow‐up tasks of healthcare provision.8 While clinical trials have found nurse‐led models to be safe and effective,27 only medical practitioners are authorised to prescribe MS‐2 Step in Australia. An alternative approach has been facilitated by improved access to telehealth services. The introduction of MBS telehealth item numbers as part of the federal response to the coronavirus disease 2019 (COVID‐19) pandemic has meant that telehealth early medical abortion services are now covered by Medicare for eligible patients.28 One services provider reported a 30% increase in the number of early medical abortions provided via telehealth, an 8% increase in the number of regional clients, and a 20% increase in the number of remote clients during 2020.5
In addition to resolving workforce problems, supporting GPs in the local delivery of early medical abortion services should be a focus. Increased local training and opportunities for educating doctors about early medical abortion and referral pathways are required to ensure that women have access to abortion services. Peer support networks has been cited by GPs as crucial for delivering early medical abortion in primary care,8 and may include other prescribing GPs, as well as a pharmacist, sonographer, and the MS‐2 Step 24‐hour nurse hotline.
Limitations
In the dataset provided by Services Australia, counts were suppressed if one to six prescriptions had been dispensed for a combination of SA3, age group, and year; our replacing suppressed counts with a standard value (five) probably reduced the estimated variability in dispensing rates across SA3s. Allocation of dispensed scripts to SA3s was based on the location of the provider GP recorded by Services Australia; this may have been inaccurate if a GP practised in multiple locations.
Conclusion
Our analysis of aggregated PBS MS‐2 Step dispensing data indicated that early medical abortion rates are higher in outer regional, remote, and inner regional Australia than in major cities, but it had not been prescribed by GPs or dispensed by local pharmacists in many SA3s in these geographic regions during 2019. State and federal governments have a duty of care to ensure that essential health services, including early medical abortion and abortion services in general, are available, affordable, and accessible to all Australian women, in public hospitals and in primary care. Local provision of early medical abortion services by GPs should be supported, and delivery via telehealth should be included in Medicare.
Box 1 – Pharmaceutical Benefits Scheme‐subsidised MS‐2 Step dispensing rates (per 1000 women aged 15–54 years), 2015–2019, by year
|
|
2015 |
2016 |
2017 |
2018 |
2019 |
||||||||||
|
|
|||||||||||||||
|
Number of dispensed prescriptions |
9373 |
15 092 |
19 236 |
18 735 |
29 207 |
||||||||||
|
Age‐standardised rate |
1.63 |
2.39 |
2.93 |
3.46 |
3.79 |
||||||||||
|
Highest rate for an SA3 |
7.3 |
8.5 |
9.8 |
13.6 |
11.1 |
||||||||||
|
Lowest rate for an SA3 |
0.4 |
0.6 |
0.6 |
1.0 |
1.1 |
||||||||||
|
Magnitude of variation (ratio ofhighest to lowest SA3 rate) |
19 |
14 |
16 |
13 |
9.8 |
||||||||||
|
Age‐standardised rate, excluding SA3s in highest and lowest rate deciles |
|
|
|
|
|
||||||||||
|
Highest rate for an SA3 |
3.1 |
4.1 |
5.2 |
6.5 |
7.0 |
||||||||||
|
Lowest rate for an SA3 |
0.9 |
1.4 |
1.8 |
2.1 |
2.3 |
||||||||||
|
Magnitude of variation (ratio ofhighest to lowest SA3 rate) |
3.4 |
3.0 |
2.9 |
3.1 |
3.0 |
||||||||||
|
|
|||||||||||||||
|
SA3 = statistical area level 3. |
|||||||||||||||
Box 2 – Age‐standardised MS‐2 Step dispensing per 1000 women aged 15–54 years, 2019, by state and remoteness area14
|
State |
Remoteness area |
|
|||||||||||||
|
Major cities |
Inner regional |
Outer regional |
Remote |
Very remote |
All regions |
||||||||||
|
|
|||||||||||||||
|
Australia |
3.30 |
4.94 |
6.53 |
6.02 |
5.02 |
3.79 |
|||||||||
|
Australian Capital Territory |
3.16 |
0.00 |
— |
— |
— |
3.15 |
|||||||||
|
New South Wales |
2.94 |
4.31 |
5.12 |
8.19 |
0.00 |
3.23 |
|||||||||
|
Northern Territory |
— |
— |
9.75 |
4.30 |
4.31 |
7.16 |
|||||||||
|
Queensland |
3.51 |
4.55 |
6.21 |
8.04 |
6.01 |
4.06 |
|||||||||
|
South Australia |
4.70 |
4.73 |
4.57 |
4.36 |
— |
4.60 |
|||||||||
|
Tasmania |
— |
6.03 |
8.43 |
— |
— |
6.69 |
|||||||||
|
Victoria |
3.26 |
5.63 |
6.83 |
— |
— |
3.79 |
|||||||||
|
Western Australia |
3.35 |
6.45 |
7.24 |
7.44 |
5.05 |
3.90 |
|||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – Age‐standardised MS‐2 Step dispensing per 1000 women aged 15–54 years, 2019, by level 3 statistical area (SA3)

Box 4 – Level 3 statistical areas (SA3s) in which MS‐2 Step had not been prescribed by a general practitioner during 2019, by state and remoteness area
|
|
|
SA3s with no MS‐2 Step |
|||||||||||||
|
Location of SA3 |
SA3s |
Number |
Proportion (raw) |
Proportion |
|||||||||||
|
|
|||||||||||||||
|
Australia† |
338 |
128 |
38% |
30% |
|||||||||||
|
State |
|
|
|
|
|||||||||||
|
Australian Capital Territory |
10 |
4 |
40% |
25% |
|||||||||||
|
New South Wales |
90 |
43 |
48% |
40% |
|||||||||||
|
Northern Territory |
9 |
4 |
44% |
34% |
|||||||||||
|
Queensland |
82 |
29 |
35% |
31% |
|||||||||||
|
South Australia |
28 |
17 |
61% |
64% |
|||||||||||
|
Tasmania |
15 |
3 |
20% |
7% |
|||||||||||
|
Victoria |
66 |
12 |
18% |
10% |
|||||||||||
|
Western Australia |
34 |
12 |
35% |
29% |
|||||||||||
|
Remoteness area14 |
|
|
|
|
|||||||||||
|
Major cities |
190 |
76 |
40% |
31% |
|||||||||||
|
Inner regional |
82 |
28 |
34% |
25% |
|||||||||||
|
Outer regional |
47 |
15 |
32% |
21% |
|||||||||||
|
Remote |
8 |
3 |
38% |
50% |
|||||||||||
|
Very remote |
11 |
6 |
55% |
21% |
|||||||||||
|
|
|||||||||||||||
|
* By number of women in SA3 aged 15–54 years. † Includes SA3s not assigned to any state; eg, SA3 99999 = no usual address. |
|||||||||||||||
Box 5 – Level 3 statistical areas (SA3s) in which MS‐2 Step had not been dispensed by a community pharmacist during 2019, by state and remoteness area
|
|
|
SA3s with no MS‐2 Step |
|||||||||||||
|
Location of SA3 |
SA3s |
Number |
Proportion (raw) |
Proportion |
|||||||||||
|
|
|||||||||||||||
|
Australia† |
338 |
112 |
33% |
25% |
|||||||||||
|
State |
334 |
108 |
|
|
|||||||||||
|
Australian Capital Territory |
10 |
3 |
30% |
36% |
|||||||||||
|
New South Wales |
90 |
34 |
38% |
29% |
|||||||||||
|
Northern Territory |
9 |
1 |
11% |
7% |
|||||||||||
|
Queensland |
82 |
27 |
33% |
26% |
|||||||||||
|
South Australia |
28 |
14 |
50% |
46% |
|||||||||||
|
Tasmania |
15 |
4 |
27% |
15% |
|||||||||||
|
Victoria |
66 |
15 |
23% |
12% |
|||||||||||
|
Western Australia |
34 |
10 |
29% |
27% |
|||||||||||
|
Remoteness area14 |
|
|
|
|
|||||||||||
|
Major cities |
190 |
60 |
32% |
24% |
|||||||||||
|
Inner regional |
82 |
31 |
38% |
27% |
|||||||||||
|
Outer regional |
47 |
14 |
30% |
20% |
|||||||||||
|
Remote |
8 |
2 |
25% |
30% |
|||||||||||
|
Very remote |
11 |
5 |
45% |
16% |
|||||||||||
|
|
|||||||||||||||
|
* By number of women in SA3 aged 15–54 years. † Includes SA3s not assigned to any state; eg, SA3 99999 = no usual address. |
|||||||||||||||
Received 9 June 2021, accepted 1 September 2021
- Asvini K Subasinghe1
- Kevin McGeechan2
- Jessica E Moulton1
- Luke E Grzeskowiak3,4
- Danielle Mazza1
- 1 Monash University, Melbourne, VIC
- 2 The University of Sydney, Sydney, NSW
- 3 Flinders University, Adelaide, SA
- 4 South Australian Health and Medical Research Institute, Adelaide, SA
No relevant disclosures.
- 1. Mazza D, Burton G, Wilson S, et al. Medical abortion. Aust J Gen Pract 2020; 49: 324–330.
- 2. de Costa C, Douglas H, Hamblin J, et al. Abortion law across Australia: a review of nine jurisdictions. Aust N Z J Obstet Gynecol 2015; 55: 105–111.
- 3. Marie Stopes Australia. Become a prescriber or dispenser. https://www.mariestopes.org.au/become‐a‐prescriber (viewed Aug 2021).
- 4. Subasinghe AK, Deb S, Mazza D. Primary care providers’ knowledge, attitudes and practices of medical abortion: a systematic review. BMJ Sex Reprod Health 2021; 47: 9–16.
- 5. Marie Stopes Australia. Impact report 2020. Australia, Apr 2021. https://www.mariestopes.org.au/wp‐content/uploads/MSA‐Impact‐Report‐2020.pdf (viewed July 2021).
- 6. Hulme‐Chambers A, Clune S, Tomnay J. Medical termination of pregnancy service delivery in the context of decentralization: social and structural influences. Int J Equity Health 2018; 17: 172.
- 7. Keogh L, Croy S, Newton D, et al. General practitioner knowledge and practice in relation to unintended pregnancy in the Grampians region of Victoria, Australia. Rural Remote Health 2019; 19: 5156.
- 8. Deb S, Subasinghe A, Mazza D. Providing medical abortion in general practice: general practitioner insights and tips for future providers. Aust J Gen Pract 2020; 49: 331–337.
- 9. Shankar M, Black KI, Goldstone P, et al. Access, equity and costs of induced abortion services in Australia: a cross‐sectional study. Aust N Z J Public Health 2017; 41: 309–314.
- 10. Doran FM, Hornibrook J. Barriers around access to abortion experienced by rural women in New South Wales, Australia. Rural Remote Health 2016; 16: 3538.
- 11. Mellish L, Karanges EA, Litchfield MJ, et al. The Australian Pharmaceutical Benefits Scheme data collection: a practical guide for researchers. BMC Res Notes 2015; 8: 634.
- 12. Australian Bureau of Statistics. People > Population > Estimated resident population > ERP by SA2 and above (ASGS 2016), 2001 onwards. https://stat.data.abs.gov.au/Index.aspx (viewed July 2020).
- 13. Australian Bureau of Statistics. Statistical Area Level 3 (SA3). July 2016. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/1270.0.55.001~July%202016~Main%20Features~Statistical%20Area%20Level%203%20(SA3)~10015 (viewed Aug 2021).
- 14. Australian Bureau of Statistics. Standard population for use in age‐standardisation. 20 June 2013. https://www.abs.gov.au/statistics/people/population/national‐state‐and‐territory‐population/dec‐2020/31010DO003_200106.xls (viewed July 2020).
- 15. Australian Bureau of Statistics. 1270.0.55.005. Australian Statistical Geography Standard (ASGS), volume 5: remoteness structure, July 2016. Updated Mar 2018. https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/1270.0.55.005Main+Features1July%202016?OpenDocument= (viewed Aug 2020).
- 16. Dawson A, Bateson D, Estoesta J, Sullivan E. Towards comprehensive early abortion service delivery in high income countries: insights for improving universal access to abortion in Australia. BMC Health Serv Res 2016; 16: 612.
- 17. Fix L, Seymour JW, Sandhu MV, et al. At‐home telemedicine for medical abortion in Australia: a qualitative study of patient experiences and recommendations. BMJ Sex Reprod Health 2020; 46: 172–176.
- 18. Meurice ME, Whitehouse KC, Blaylock R, et al. Client satisfaction and experience of telemedicine and home use of mifepristone and misoprostol for abortion up to 10 weeks’ gestation at British Pregnancy Advisory Service: a cross‐sectional evaluation. Contraception 2021; 104: 61–66.
- 19. Hulme‐Chambers A, Temple‐Smith M, Davidson A, et al. Australian women’s experiences of a rural medical termination of pregnancy service: a qualitative study. Sex Reprod Healthc 2018; 15: 23–27.
- 20. Services Australia. Medicare item reports. http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp (viewed Aug 2021).
- 21. Australian Institute of Health and Welfare. Use of routinely collected national data sets for reporting on induced abortion in Australia (Cat. no. PER 30). Canberra: AIHW, 2005. https://www.aihw.gov.au/reports/mothers‐babies/use‐national‐data‐sets‐reporting‐induced‐abortion/contents/executive‐summary (viewed Aug 2021).
- 22. Sifris R, Penovic T. Barriers to abortion access in Australia before and during the COVID‐19 pandemic. Women’s Studies International Forum 2021; 86: 102470.
- 23. Moel‐Mandel C, Graham M, Taket A. Snapshot of medication abortion provision in the primary health care setting of regional and rural Victoria. Aust J Rural Health 2019; 27: 237–244.
- 24. Royal College of Obstetricians and Gynaecologists. Coronavirus (COVID‐19) infection and abortion care. Information for healthcare professionals. Version 3.1; 31 July 2020. https://www.rcog.org.uk/globalassets/documents/guidelines/2020‐07‐31‐coronavirus‐covid‐19‐infection‐and‐abortion‐care.pdf (viewed July 2021).
- 25. Keogh LA, Gillam L, Bismark M, et al. Conscientious objection to abortion, the law and its implementation in Victoria, Australia: perspectives of abortion service providers. BMC Med Ethics 2019; 20: 11.
- 26. Swami M, Scott A. Impact of rural workforce incentives on access to GP services in underserved areas: evidence from a natural experiment. Soc Sci Med 2021; 281: 114045.
- 27. Kopp Kallner H, Gomperts R, Salomonsson E, et al. The efficacy, safety and acceptability of medical termination of pregnancy provided by standard care by doctors or by nurse‐midwives: a randomised controlled equivalence trial. BJOG 2015; 122: 510–517.
- 28. Mazza D, Deb S, Subasinghe A. Telehealth: an opportunity to increase access to early medical abortion for Australian women. Med J Aust 2020; 213: 298–299.e1. https://www.mja.com.au/journal/2020/213/7/telehealth‐opportunity‐increase‐access‐early‐medical‐abortion‐australian‐women





Abstract
Objectives: To examine primary care provision of early medical abortion services in Australia.
Design: Cross‐sectional study; analysis of Pharmaceutical Benefits Scheme (PBS) dispensing data.
Setting, participants: Women of child‐bearing age (15–54 years), Australia, 2015–2019.
Main outcome measures: Age‐standardised rates of MS‐2 Step prescriptions dispensed by year for 2015–2019, and age‐standardised rates by state, remoteness area, and level 3 statistical areas (SA3s) for 2019. Numbers and proportions of SA3s in which MS‐2 Step was not prescribed by a GP or dispensed by a community pharmacy during 2019 (unweighted and weighted by number of women of reproductive age), by state and remoteness area.
Results: During 2015–2019, 91 643 PBS prescriptions for MS‐2 Step were dispensed; the national age‐standardised rate increased from 1.63 in 2015 to 3.79 prescriptions per 1000 women aged 15–54 years in 2019. In 2019, rates were higher in outer regional Australia (6.53 prescriptions per 1000 women aged 15–54 years) and remote Australia (6.02 per 1000) than in major cities (3.30 per 1000). However, about 30% of women in Australia lived in SA3s in which MS‐2 Step had not been prescribed by a GP during 2019, including about 50% of those in remote Australia.
Conclusions: The rate of early medical abortion is greater among women in remote, outer regional, and inner regional Australia than in major cities, but a considerable proportion of women live in areas in which MS‐2 Step was not locally prescribed or dispensed during 2019. Supporting GPs in the delivery of early medical abortion services locally should be a focus of health policy.