The known: The profile of Australian aged care residents has changed markedly in recent years. Residents are older and frailer, with an annual mortality rate of around 32%.
The new: Residential aged care needs and cost predictors are captured in the Australian National Aged Care Classification by measures of frailty, mobility impairment, functional decline, cognitive loss, behavioural disturbance and technical nursing needs.
The implications: The Australian National Aged Care Classification is a new casemix system for classifying aged care residents, and for determining funding and staffing requirements. It can be used in routine evaluation of aged care facility outcomes, taking into account the mix of residents in each facility.
As in all developed nations, the Australian population is ageing and the need to provide care for older people who cannot live independently is increasing. In 2017–18, total government expenditure for aged care services was $18.4 billion, including $12.4 billion (67%) for residential aged care.1 Expenditure will inevitably increase as the number of older people grows, and must also increase to mitigate the quality and safety problems care identified by the Royal Commission into Aged Care Quality and Safety.2,3
Since the introduction in 2008 of the current aged care funding model, the Aged Care Funding Instrument (ACFI), the profile of people entering residential care has changed substantially, partly because of the success of programs that enable people to stay at home longer. Residents are now typically older and frailer on entry (about half are over 84 years old), and their annual mortality rate is around 32%. Consequently, about half of those who enter residential care will live there for two years or less.4,5
The 2017 review of the ACFI found that it does not sufficiently discriminate between the care needs of residents, that it is administratively inefficient, and that it provides perverse incentives; for example, if a resident's functioning improves, ACFI funding can be reduced. It concluded that the ACFI is “no longer fit for purpose”.6
The 2017 review investigated overseas funding models and found that none were suitable for Australia. The only well developed system for classifying people in long term care is the Resource Utilization Groups (RUG) system, a casemix system developed through a series of research studies and designed to explain and predict resource use. The original version, developed in the United States in 1994, comprised 44 classes and explained 55.5% of variance in daily costs; the most recent version, RUG‐IV, includes 66 classes. The statistical performance of the RUG system has varied in overseas studies, reported reduction in variation statistics ranging between 0.12 and 0.56.7 Designed for use in both nursing homes and skilled nursing facilities in the US, it has a hierarchic patient category structure — rehabilitation, extensive services, special care, clinically complex, impaired cognition, behaviour problems, and reduced physical function — not directly relevant to the Australian aged care system.
The 2017 ACFI review proposed developing a new funding model for Australian residential aged care.6 In this article, we describe the development of a new classification system to underpin this funding model.8
Methods
Sampling
The population of interest comprised residents in non‐government aged care facilities in Australia. As it was impractical to include all of Australia, three regions — Melbourne, the Hunter region of New South Wales, and northern Queensland — were purposively selected to respectively represent major cities, regional areas, and remote areas. Within each region, homes were stratified by type (not for profit, for profit) and size (large, medium, small) to ensure that these characteristics were adequately represented in our sample. The number of facilities selected from each stratum was proportional to its size. Facilities were then randomly selected from each stratum, and all residents in each selected facility invited to participate.
Our sample size calculation took into account the mean and variance in cost for each stratum, based on Department of Health data on the location, type, size and government funding received for each residential aged care facility in Australia. The required sample size, determined such that the margin of error for mean daily costs was no more than $10, was calculated to be 2200 residents from 30 facilities. After the classification was developed, it was verified in a representative national sample of a further 69 facilities (data not reported in this article).9
Clinical data design and collection
Our resident assessment tool was designed after reviewing the relevant international literature and with the advice of four clinical advisory panels. The panels included clinicians and researchers with expertise in aged care, rehabilitation, geriatric medicine, psychiatry of older people, wound management, and palliative care. Each panel focused on one area of clinical need: function, cognition and behaviour; wound management; palliative care; and technical nursing. The design of the tool has been described in detail elsewhere.10 The tool was designed to capture resident attributes that best predict differences in their need for care. Its development was guided by four principles:
- it should be suitable for use by independent clinical assessors;
- it should be possible to complete it in one session, with minimal burden for the resident;
- the validity and reliability of instruments comprising the tool should be established;
- the instruments should not be subject to royalty or copyright restrictions.
The final version of the assessment tool included seven existing instruments, as well as items related to palliative care, frailty, and technical nursing (Box 1).
Participating residents were assessed during March 2018 – June 2018 by registered nurses recruited and trained for the study.
Service data collection
Concurrent with resident assessments, service use data (staff time) were collected for one calendar month in each home. The data collection period was staggered over three months to allow the research team to support staff during data collection.
All care delivery staff recorded service use data each day using handheld barcode scanners and purpose‐designed scan cards. Each staff member, resident, and type of activity undertaken during a shift were assigned unique barcodes. Staff scanned details of activities and uploaded the data from the scanner to a secure server at the end of each shift. This approach enabled data to be captured by shift in real time.
A unique feature of our study was the distinction between shared care and individual care. Individual care was defined as care tailored to the needs of an individual resident. Shared care was defined as care not tailored to individual resident needs; that is, care received equally by all residents, including general supervision in common areas, clinical care management and quality activities, and brief incidental interactions.
Data preparation
Prior to class‐finding, the datasets were checked for completeness, consistency, accuracy, validity, and timeliness. The datasets were then linked to create one record for each resident, including both assessment and service use data. For the analyses, cost was defined as staff time per resident, as a preliminary analysis indicated that 92% of all care costs were for staffing.
Data analysis
The goal of our study was to develop a casemix classification system with classes that were:
- clinically meaningful to care staff and useful for clinical management;
- based on resident characteristics rather than on provided services;
- comprehensive, consistent, and mutually exclusive, so that each resident can be assigned to one, and only one, class;
- homogeneous with respect to resource use, so that the cost of care for residents in a given class is similar.
Clinical meaning was determined by the clinical advisory panels. We aimed to ensure that the classification was administratively and operationally feasible, and sufficiently flexible to allow progressive refinement in response to practice changes, technical advances, and the identification of new cost drivers. Moreover, its application should not give rise to perverse incentives.
We used classification and regression tree analysis — that is, a decision tree algorithm for generating regression tree predictive models — to develop the classification.11 This procedure predicts values of the dependent variable (resource use) based on the values of independent variables (resident characteristics). Overall performance of the classification was assessed with the reduction in variation statistic (RIV; the variance explained by the classification as the proportion of total variance). The homogeneity of each class was measured as the coefficient of variation (standard deviation divided by the mean; online Supporting Information).
An iterative series of statistical analyses and clinical reviews were undertaken: initial statistical results were reviewed by clinical advisory panel members, and their advice was incorporated into subsequent analyses. This iterative process continued until an outcome was achieved that was both statistically robust and meaningful from a clinical perspective.
The stability and reliability of the classification model was determined with test–retest methodology, using 1042 records for the test dataset and 613 records for the validation dataset.
Statistical analyses were conducted in SPSS 21.
Ethics approval
This study was approved by the University of Wollongong and Illawarra Shoalhaven Local Health District Human Research Ethics Committee (reference, 2017/546).
Results
Our initial sample included 1967 residents from 30 aged care facilities; 56 (2.8%) did not consent to participation, 19 (0.9%) were unavailable, and 15 who consented (0.7%) died before the study start date. A total of 1877 clinical assessments were therefore available for analysis. Staff time was reported for 60 990 resident days, comprising 315 029 staff time activity records collected by 1600 staff members.
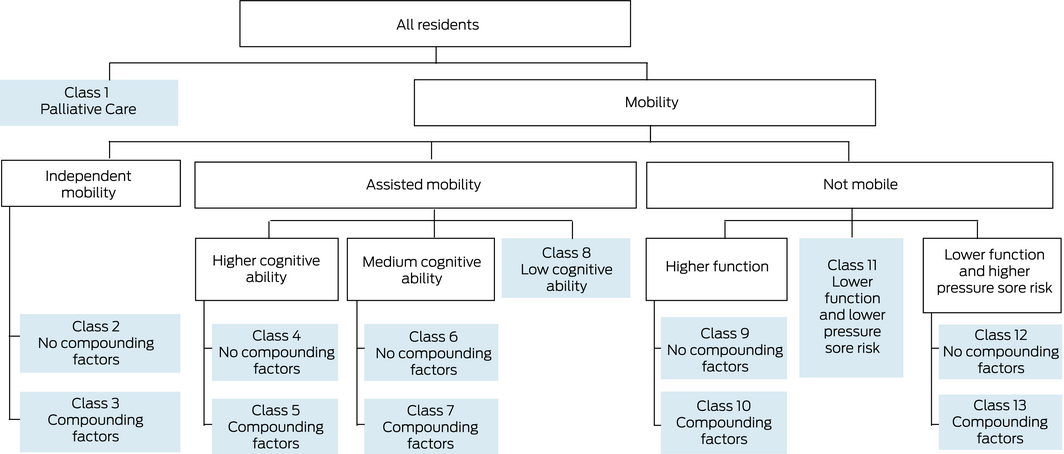
Classification and regression tree analysis produced a regression tree in which the first branching was determined by resident mobility classification, measured with the modified de Morton Mobility Index (DEMMI): independent, assisted and non‐mobile.12 Each branch was then split into further classes based on other clinical measures, such as cognitive and physical function and pressure injury risk (Box 1), producing a classification with 13 classes, the Australian National Aged Care Classification (AN‐ACC) (Box 2; Supporting Information).
The AN‐ACC includes a single class for people admitted for palliative care, based on clinical advice that these residents comprise a clinically discrete class and require considerable levels of additional resources. As insufficient data were available to calculate resource use for this group of residents, a relative value was imputed on the basis of clinical advice. Residents who required palliative care after admission to residential care can be re‐assessed and re‐assigned to a different class as their needs change.
Each of the other branches of the clinically informed regression tree model includes classes defined by whether a resident has compounding factors. These factors reflect the combined incremental resource use associated with other independent variables, such as frailty, falls, daily injections and wound management, and their impact was estimated by multiple regression analysis (summarised in Box 1).
The independent mobility branch has two classes defined by the combined effects of the compounding factors Resource Utilisation Group: activities of daily living (RUG‐ADL), Australian modified functional independence measure (AM‐FIM): cognition, Australia‐modified Karnofsky performance status (AKPS), behaviour resource utilisation assessment (BRUA), and daily injections.
The assisted mobility branch has five classes, defined by cognitive ability, and then by the combined effects of the compounding factors Braden activity item, RUG‐ADL, AM‐FIM: motor, AM‐FIM: social cognition, AM‐FIM: communication, AKPS, Rockwood score, BRUA, falls during the past 12 months, daily injections, and complex wound management.
The not mobile branch has five classes defined by function and pressure sore risk, and then by the combined effects of the compounding factors Braden total score, AM‐FIM: eating, AM‐FIM: transfers, BRUA, falls during the past 12 months, obesity flag, daily injections, and complex wound management.
The RIV for the test dataset was 0.52, indicating that the classification performs well in explaining the variation in daily care costs between classes of residents. The RIV for the re‐test dataset was 0.48; the similarity of the two values indicates that the classification model is reliable. The coefficient of variation for each class was quite small (less than 1.0: range, 0.34–0.62), indicating that each class is relatively homogenous with respect to resource use (Supporting Information, figure).
Relative value units for individual AN‐ACC classes (that is, the ratio of mean costs for the class to mean costs for all residents) ranged from 0.37 (class 2) to 1.95 (classes 1 and 13).
Discussion
We report the first study to produce a useful casemix classification for people in residential aged care in Australia. An important feature of our study was that a resident's specific medical diagnoses (including dementia, mental health disorders, and physical disorders) are not captured as cost drivers per se. This is because underlying medical conditions result in frailty, impaired mobility, functional and cognitive decline, behavioural disturbance, and technical nursing needs. The care burden arising from these outcomes determines residential aged care costs. As the age and frailty of people entering residential age care are increasing, the prevalence of these cost drivers will increase in future and substantial increases in residential care funding will be required.
The AN‐ACC is based on these key cost drivers, reflecting the functional consequences of health conditions rather than the conditions themselves. It captures not what a resident does, but rather their physical capacity (including pain), cognitive capacity (including ability to communicate, sequence, interact socially, and solve problems, and memory), mental health problems (including depression and anxiety), and behaviour (including cooperation, physical agitation, wandering, passive resistance, verbal aggression).
The statistical performance and clinical acceptability of the AN‐ACC are adequate for its application for funding purposes. With only 13 classes and an RIV of 0.52, it compares favourably with related casemix classifications, including the Australian National Subacute and Non‐Acute Patient (AN‐SNAP) classification (83 classes; RIV, 0.55),19 the ACFI (64 classes; RIV, 0.20), the RUG‐IV classification used in the US (66 classes; RIV, 0.62), and other variants of the RUG classification used overseas (34–53 classes; RIV, 0.12–0.56).7
Implementing the AN‐ACC is now being considered by the Australian government in the context of the major structural and funding aged care reforms expected after the Royal Commission into Aged Care Quality and Safety publishes its final report in late 2020. In our final Resource Utilisation and Classification Study report, we recommended the AN‐ACC not only for residential aged care but also in other aged care settings; we also proposed an ongoing aged care research and development agenda that builds on this study, including assessment, classification, costing, and outcome studies.20
The AN‐ACC is not an end in itself, but an essential element in the broader reform of the national aged care funding system. This includes protocols for re‐assessment that allow a resident to be assigned to a different class as their needs change.
The AN‐ACC could provide a meaningful system for measuring and benchmarking both input measures (staff ratios) and resident outcome measures. Staffing requirements, mortality rates, and outcome rates (such as numbers of falls) vary markedly between AN‐ACC classes. Reporting resident outcome measures by AN‐ACC class would facilitate routine evaluation of residential aged care outcomes, taking into account the mix of residents in a facility.
Strengths and limitations
Strengths of our study include the strong clinical and residential care staff engagement in study design, data collection, and data interpretation, the use of independent clinical assessors, and the use of barcode technology to maximise the accuracy of staff time data.
A further strength was the representativeness of the sample, confirmed by the follow‐up study. The results of the verification study reflected those of the original study sample, indicating both the robustness of the classification and the representativeness of the original sample.9 A further measure of the stability and reliability of the classification model was the fact that the characteristics of the validation dataset mirrored those of the dataset with which the classification was developed.
Limitations include our excluding respite care residents, and the small number of residents included in class 1 (palliative care); the latter problem was mitigated by combining class 1 and class 13 for funding purposes. We could not adequately investigate residents with special care needs (oxygen, enteral feeding, tracheostomy, catheter, stoma, dialysis) because of their very small numbers.
Conclusion
The AN‐ACC enables the community, care providers, and governments to make meaningful judgements about the quality and outcomes of residential aged care and to fairly compare the quality of care provided at different facilities.
Box 1 – Independent variables included in the Australian National Aged Care Classification, version 1
|
|
|
Primary branch |
|||||||||||||
|
Independent variable |
Description |
Independent mobility |
Assisted mobility |
Not mobile |
|||||||||||
|
|
|||||||||||||||
|
Modified De Morton mobility index (DEMMI)12 |
12 items, four subscales (bed, chair, static balance, walking); questions 13–15 of standardised DEMMI excluded. Used to assign resident to a mobility branch |
|
|
|
|||||||||||
|
Australian modified functional independence measure (AM‐FIM)13,14 |
17 items, two subscales (motor and cognition) and six domains (self‐care, sphincter control, transfers, location, communication, social cognition) |
|
|
|
|||||||||||
|
Motor |
Self‐care, sphincter control, transfers, location domains (12 items) |
|
|
|
|||||||||||
|
Transfers |
Three items (bed/chair, toilet, shower) |
|
|
|
|||||||||||
|
Eating |
Single item |
|
|
|
|||||||||||
|
Cognition |
Communication and social cognition domains (five items) |
|
|
|
|||||||||||
|
Communication |
Two items (comprehension and expression) |
|
|
|
|||||||||||
|
Social cognition |
Three items (social interaction, problem solving and memory) |
|
|
|
|||||||||||
|
Resource Utilisation Group: activities of daily living (RUG‐ADL)15 |
Four items originally included in RUG classification. Total score is used in AN‐ACC |
|
|
|
|||||||||||
|
Braden scale for predicting pressure sore risk16 |
Seven item scale |
||||||||||||||
|
Total score |
All seven items |
|
|
|
|||||||||||
|
Activity item |
The activity item in the Braden scale |
|
|
|
|||||||||||
|
Australia‐modified Karnofsky performance status (AKPS)17 |
Single score rating |
|
|
|
|||||||||||
|
Rockwood clinical frailty scale18 |
Single score rating |
|
|
|
|||||||||||
|
Behaviour resource utilisation assessment (BRUA)10 |
Five items (problem wandering or intrusive behaviour; verbal disruption; physical aggression; emotional dependence; and danger to self and others) |
|
|
|
|||||||||||
|
Obesity |
Flag to identify requirement for bariatric care |
|
|
|
|||||||||||
|
Falls during past 12 months |
Flag to indicate number of falls in previous year |
|
|
|
|||||||||||
|
Daily injections |
Proxy indicator of need for complex nursing |
|
|
|
|||||||||||
|
Complex wound management |
Proxy indicator of need for complex nursing |
|
|
|
|||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 8 January 2020, accepted 14 May 2020
- Kathy Eagar1
- Rob Gordon1
- Milena F Snoek1
- Carol Loggie1
- Anita Westera1
- Peter David Samsa1
- Conrad Kobel1
- Australian Health Services Research Institute, University of Wollongong, Wollongong, NSW
We thank the participating aged care homes, the residents, the clinicians and care staff who assessed residents and collected resource use data, and the Resource Utilisation and Classification Study project team. The project was funded by the Australian Department of Health (Health/16‐17/02638).
No relevant disclosures.
- 1. Australian Productivity Commission. Report on Government Services 2019. Part F, chapter 14: Aged care services. Feb 2019. https://www.pc.gov.au/research/ongoing/report-on-government-services/2019/community-services/aged-care-services (viewed Nov 2019).
- 2. Aged Care Financing Authority. Attributes for sustainable aged care: a funding and financing perspective. Oct 2019. https://www.health.gov.au/resources/publications/acfa-report-on-attributes-for-sustainable-aged-care (viewed Dec 2019).
- 3. Royal Commission into Aged Care Quality and Safety. Interim report: Neglect. Volume 2: hearing overviews and case studies. Adelaide: Royal Commission into Aged Care Quality and Safety, 2019. https://agedcare.royalcommission.gov.au/sites/default/files/2019-12/interim-report-volume-2_0.pdf (viewed Nov 2019).
- 4. Australian Department of Health. 2018–19 Report on the operation of the Aged Care Act 1997. 2019. https://www.gen-agedcaredata.gov.au/www_aihwgen/media/ROACA/2018-19-ROACA.pdf (viewed Oct 2019).
- 5. Australian Institute of Health and Welfare. GEN aged care data. Updated 30 June 2018. https://www.gen-agedcaredata.gov.au/Topics/People-leaving-aged-care; https://www.gen-agedcaredata.gov.au/Topics/Admissions-into-aged-care (viewed Oct 2019).
- 6. McNamee J, Poulos C, Seraji H, et al. Alternative aged care assessment, classification system and funding models: final report, volume one. Wollongong: Centre for Health Service Development, Australian Health Services Research Institute, University of Wollongong, 2017. https://www.health.gov.au/resources/publications/alternative-aged-care-assessment-classification-system-and-funding-models-report (viewed Nov 2019).
- 7. Turcotte LA, Poss J, Fries B, Hirdes JP. An overview of international staff time measurement validation studies of the RUG‐III case–mix system. Health Serv Insights 2019; 12: 1178632919827926.
- 8. Eagar K, McNamee J, Gordon R, et al. The Australian National Aged Care Classification (AN‐ACC). The Resource Utilisation and Classification Study: report 1. Australian Health Services Research Institute, University of Wollongong, 2019. https://www.health.gov.au/sites/default/files/documents/2019/12/resource-utilisation-and-classification-study-rucs-reports-report-1-the-australian-national-aged-care-classification-an-acc_0.pdf (viewed Nov 2019).
- 9. Eagar K, McNamee J, Kobel C, et al. Modelling the impact of the AN‐ACC in Australia. The Resource Utilisation and Classification Study: report 4. Wollongong: Australian Health Services Research Institute, University of Wollongong, 2019. https://www.health.gov.au/sites/default/files/documents/2019/12/resource-utilisation-and-classification-study-rucs-reports-report-4-modelling-the-impact-of-the-an-acc-in-australia_0.pdf (viewed Nov 2019).
- 10. Westera AB, Snoek M, Duncan C, et al. The AN‐ACC assessment model. The Resource Utilisation and Classification Study: report 2. Wollongong: Australian Health Services Research Institute, University of Wollongong, 2019. https://www.health.gov.au/sites/default/files/documents/2019/12/resource-utilisation-and-classification-study-rucs-reports-report-2-the-an-acc-assessment-model_0.pdf (viewed Nov 2019).
- 11. Breiman L, Friedman J, Stone CJ, Olshen RA. Classification and regression trees. Boca Raton (FL): CRC Press, 1984.
- 12. de Morton NA, Davidson M, Keating JL. The de Morton Mobility Index (DEMMI): an essential health index for an ageing world. Health Qual Life Outcomes 2008; 6: 63.
- 13. Granger CV, Brownscheidle CM. Outcome measurement in medical rehabilitation. Int J Technol Assess Health Care 1995; 11: 262–268.
- 14. Eagar K, Green J, Gordon R, et al. Functional assessment to predict capacity for work in a population of school‐leavers with disabilities. Int J Disabil Dev Ed 2006; 53: 331–349.
- 15. Williams BC, Fries BE, Foley WJ, et al. Activities of daily living and costs in nursing homes. Health Care Financ Rev 1994; 15: 117–135.
- 16. Bergstrom N, Braden BJ, Laguzza A, Holman V. The Braden Scale for predicting pressure sore risk. Nurs Res 1987; 36: 205–210.
- 17. Abernethy AP, Shelby‐James T, Fazekas BS, et al. The Australia‐modified Karnofsky Performance Status (AKPS) scale: a revised scale for contemporary palliative care clinical practice. BMC Palliat Care 2005; 4: 7.
- 18. Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173: 489–495.
- 19. Green J, Gordon R, Blanchard M, et al. Development of the Australian National Subacute and Non‐acute Patient Classification version 4: final report. Wollongong: Centre for Health Service Development, University of Wollongong, 2015. https://www.ihpa.gov.au/sites/default/files/Documents/an-snap_classification_version_4_final_report.pdf (viewed Nov 2019).
- 20. Eagar K, McNamee J, Gordon R, et al. AN‐ACC: A national classification and funding model for residential aged care: synthesis and consolidated recommendations. the Resource Utilisation and Classification Study: report 6. Wollongong: Australian Health Services Research Institute, University of Wollongong, 2019. https://www.health.gov.au/sites/default/files/documents/2019/12/resource-utilisation-and-classification-study-rucs-reports-report-6-an-acc-a-national-classification-and-funding-model-for-residential-aged-care-synthesis-and-consolidated-recommendations_0.pdf (viewed Nov 2019).






Abstract
Objective: To develop a casemix classification to underpin a new funding model for residential aged care in Australia.
Design, setting: Cross‐sectional study of resident characteristics in thirty non‐government residential aged care facilities in Melbourne, the Hunter region of New South Wales, and northern Queensland, March 2018 – June 2018.
Participants: 1877 aged care residents and 1600 residential aged care staff.
Main outcome measures: The Australian National Aged Care Classification (AN‐ACC), a casemix classification for residential aged care based on the attributes of aged care residents that best predict their need for care: frailty, mobility, motor function, cognition, behaviour, and technical nursing needs.
Results: The AN‐ACC comprises 13 aged care resident classes reflecting differences in resource use. Apart from the class that included palliative care patients, the primary branches were defined by the capacity for mobility; further classification is based on physical capacity, cognitive function, mental health problems, and behaviour. The statistical performance of the AN‐ACC was good, as measured by the reduction in variation statistic (RIV; 0.52) and class‐specific coefficients of variation. The statistical performance and clinical acceptability of AN‐ACC compare favourably with overseas casemix models, and it is better than the current Australian aged care funding model, the Aged Care Funding Instrument (64 classes; RIV, 0.20).
Conclusions: The care burden associated with frailty, mobility, function, cognition, behaviour and technical nursing needs drives residential aged care resource use. The AN‐ACC is sufficiently robust for estimating the funding and staffing requirements of residential aged care facilities in Australia.