The uneven distribution of essential primary health care services between rural and metropolitan communities is a challenge in Australia1 and overseas.2 More than 7 million Australians (29% of the population) live in regional and remote areas.3 Despite recent increases in the number of general practitioners in these communities, differences in service delivery models and higher levels of service demand in some rural areas (related to the broader scope of practice and the low numbers of other health practitioners) contribute to the shortage of GPs in rural areas. In very remote areas, the number of GP services per capita is about half that of major cities.4 Rural Australians have higher rates of health risk behaviours (including smoking, excessive alcohol consumption, physical inactivity, overweight and obesity) and mortality (predominantly from heart disease and diabetes).3 An effective rural GP workforce is essential for meeting the health needs of our rural and remote communities, particularly those of more vulnerable Aboriginal and Torres Strait Islander Australians.5
Recruiting international medical graduates to work in rural and remote areas has provided a temporary solution to the rural GP workforce problem.5 The Australian government has also funded several programs that strengthen and support the recruitment and retention of rural primary care workers, including regionalised education and training programs, and has also implemented regulatory and legislative measures (eg, compulsory service requirements and scholarships) and provided financial incentives and personal and professional support recommendations (such as outreach support and supervision).2 The Stronger Rural Health Strategy6 provides further incentives, targeted funding, and bonding arrangements with the aim of improving opportunities for training and practice in rural Australia. However, evidence for the effectiveness of government interventions is limited.7,8
Several reviews9,10,11 have reported the effects of rural background and rural experience during undergraduate or postgraduate medical training (rural pipeline factors12) on where doctors later practice. These reviews, however, included other medical, specialist, and allied health practitioners for whom the likelihood of working in a metropolitan or rural area may be influenced by service obligations.
Understanding the effects of rural pipeline factors — including the recruitment of rural students and providing opportunities for rural placement during medical school and residency and vocational training12,13,14,15 — should inform strategies and national policies for attracting GPs to rural clinical practice. The aim of our review was to synthesise quantitative data on the effects of rural background and of experience in rural areas during medical training or during postgraduate GP training on the likelihood of GPs practising and remaining in rural areas.
Methods
The protocol for this systematic review was registered with the International Prospective Register of Systematic Reviews (PROSPERO) on 21 August 2017 (CRD42017074943; updated 1 February 2018).
Types of study and participants
We included studies that reported quantitative comparisons of associations between rural pipeline factors and the location or duration of later clinical practice for GPs or family physicians. We excluded qualitative studies, case reports and series, abstracts, education articles, and opinion pieces. Studies were excluded if data for GPs or family physicians could not be separated from data for other medical specialists and health professionals, clinicians had not completed postgraduate or vocational general practice training, or the study outcome was a proxy measure of recruitment to rural practice rather than actual practice location (eg, attitudes toward rural practice, rural practice intention).
Types of rural experience
Rural background was defined as having either lived in a rural area for at least one year before the age of 18 years or graduated from a rural high school. Rural experience during medical training was defined as completing short term traditional block rotations in rural areas or attending a rural clinical school for at least one academic year. Rural clinical school clinical placements are generally either traditional block rotations in hospitals and general practice or longitudinal integrated clerkships in hospitals, general practices, or remote community clinics. Postgraduate rural medical experience (during internship, residency or vocational training) was defined as a rural placement of any duration during postgraduate training, bonded scholarships in rural hospitals, or rural pathway GP vocational or family physician residency training.
Outcome variables
The primary outcomes were current practice location and duration of rural clinical practice (number of consecutive years in rural general practice).
Information sources and search strategy
We searched the MEDLINE, EMBASE, Informit Health Collection, and ERIC (Educational Resources Information Center) databases for records published to September 2018; MeSH headings and key search terms (and their synonyms) were combined with Boolean operators (Supporting Information, table 1). The reference lists of retrieved articles and published reviews were examined for additional studies, and we also searched grey literature resources for relevant electronic theses and conference proceedings.
Selection process
Search results were merged in the Endnote X9 reference manager (Clarivate) and duplicates removed. Two authors (JO, PC) independently screened the titles and abstracts in the records and then reviewed the full text of potentially relevant articles. We excluded studies for which the full text could not be retrieved. We contacted the corresponding author of one study to clarify their report. The final list of included studies was confirmed after discussion by the five review authors.
Data extraction, synthesis, and analysis
Study data related to GPs or family physicians were extracted by the five review authors into a specially designed electronic data extraction form. We extracted data on author, year of publication, study design, country, study setting, data sources, participant characteristics, exposure variables, relevant outcome variables, results, and study strengths and limitations.
Attrition rates were adequately disclosed in all included publications. Primary outcome data included dichotomous effect measures (odds ratios [ORs], risk ratios [RRs], χ2 test results, proportions). Our meta‐analysis was limited to studies reporting ORs adjusted for confounders in multi‐level regression analyses. Data were pooled in RevMan 5 (Cochrane Collaboration) to calculate weighted effects and 95% confidence intervals (CIs) for each outcome, applying a random effects model because of expected heterogeneity. We narratively report study data that could not be pooled for meta‐analysis.
Study quality
Pairs of review authors (JO, RP, RO, PC) independently assessed the risk of bias of each included study, with disagreements resolved by a third reviewer (SP). Risk of bias was scored with the Newcastle–Ottawa Scale:16 7–8, very good; 5–6, good; 4, satisfactory; 0–3, unsatisfactory.
Results
Study selection
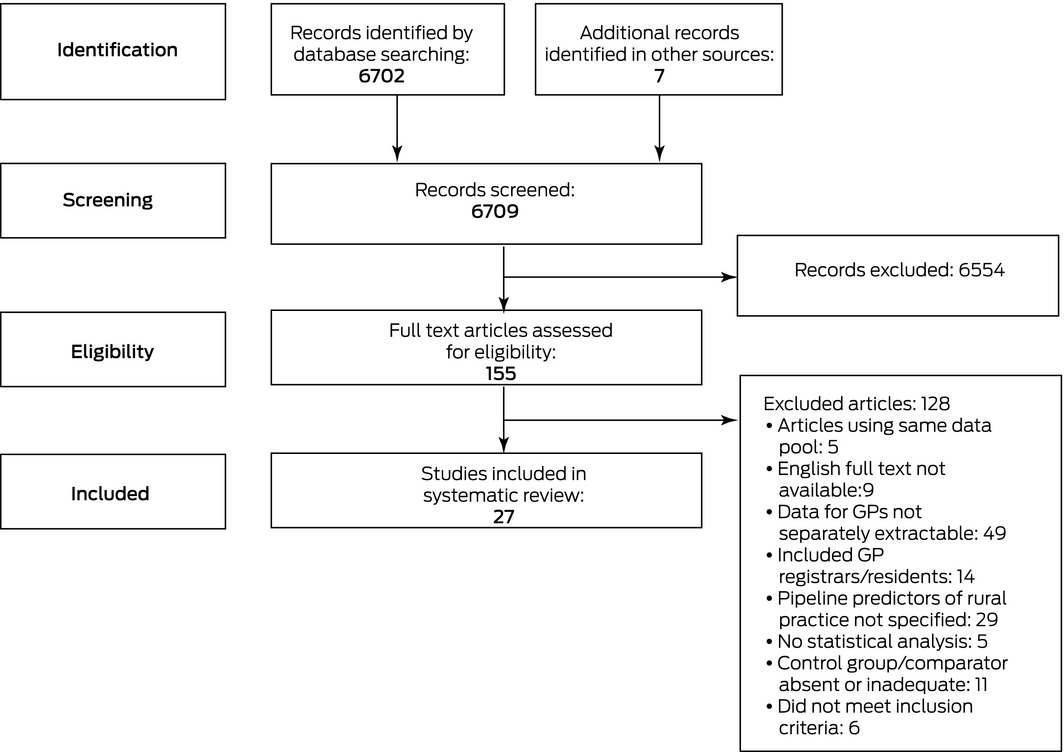
We identified 6702 potentially relevant items by electronic database searching, and seven further items from other sources. We excluded 6554 duplicates and irrelevant records after title and abstract screening. After screening the full text of 155 articles, 27 eligible studies were included in our review (Box 1).
Study characteristics
Twelve included studies had cohort designs, four were case–control studies, and eleven were cross‐sectional studies. Eleven studies were conducted in the United States, eight in Canada, and eight in Australia. Study sample sizes ranged from 68 to about 27 800 GPs or family practitioners. All included studies reported current rural practice location as a study outcome; four studies20,21,40,41 reported rural retention. The definition of rural location differed substantially between studies. The time at which “current” practice location was determined ranged from shortly after graduation to 31 years after graduation. The time spent in rural areas varied, as many studies followed up at a single time point students who had graduated in different years. Definitions of retention in rural practice required periods of practice ranging between one and 25 years (Box 2).
Study quality
We scored ten studies as very good, 14 as good, two as satisfactory, and one as unsatisfactory. In the three studies with the lowest scores,26,31,34 adjustment for confounding variables was not undertaken and information about rural experience and practice was self‐reported (Box 2; Supporting Information, table 2).
Rural background
Seventeen studies17,18,19,20,22,23,24,26,27,28,30,31,32,33,36,37,38 investigated associations between living in a rural community before adulthood and practising as a rural GP or family practitioner. Data from ten studies could be pooled for meta‐analysis; three studies17,26,28 were omitted from the meta‐analysis because of the nature of their reported results and four22,23,24,36 because of differences in reported outcomes, including multiple outcomes derived from a common database. Living in a rural area for any period before the age of 18 years increased the odds of practising in a rural location (OR, 2.71; 95% CI, 2.12–3.46) (Box 3). Being raised in a rural community was associated with increased likelihood of rural practice in most studies,19,20,24,26,30,32,33 but not all.18,22 Residing in a rural community for at least one year before the age of 18 years increased the odds of current rural practice in one study (OR, 2.14; 95% CI, 1.13–4.03)31 but not in another (OR, 1.51; 95% CI, 0.82–2.76).38 Living in an Australian rural community for 6–10 years (OR, 2.28; 95% CI, 1.69–3.08) or 11–18 years (OR, 2.35; 95% CI, 1.93–2.87), but not for 1–5 years (OR, 1.20; 95% CI, 0.89–1.63), increased the likelihood of rural practice.36 Similarly, GPs in rural practice were more likely to have lived in rural areas for at least 5 consecutive or 8 cumulative years (OR, 2.50; 95% CI, 1.97–3.18)27 or for more than 10 years during childhood (rural GPs, 30–33%; suburban GPs, 11%).17 In an Australian study, rural primary school education (OR, 2.43; 95% CI, 1.09–5.56) but not rural secondary school (OR, 1.50; 95% CI, 0.74–3.05) was associated with later rural practice;22 a subsequent Australian study found that rural attendance was significantly associated with later rural practice for both school levels.23 Other studies found that attending (OR, 4.03; 95% CI, 1.05–15.4)37 or graduating from a rural secondary school (OR, 5.27; 95% CI, 1.96–14.2)28 increased the odds of later rural practice. The likelihood of rural practice increased if students completed their final year at a rural secondary school (OR, 3.18; 95% CI, 0.99–10.2)24 or students were rural residents for the duration of primary or secondary school.23
Rural clinical experience during medical school
Seven studies20,24,28,30,37,38,42 investigated the relationship between rural undergraduate clinical training and rural practice location; adjusted ORs from five20,24,28,30,38 were pooled for meta‐analysis. Rural clinical experience during undergraduate training increased the likelihood of practising in a rural area (OR, 1.75; 95% CI, 1.48–2.08). One small Canadian study42 found a significant association between rural clinical experience during medical school and practice location; another37 found the odds of rural practice for students undertaking a third year community‐based clerkship in non‐rural areas were less than half those for undergraduates with placements in rural areas (OR, 0.40; 95% CI, 0.17–0.93). Rural undergraduate training increased the odds of rural practice in two studies,24,30 as did a specifically rural curriculum in one study,28 but not in two others20,38 (Box 4).
Rural clinical experience during postgraduate training
Thirteen studies17,20,24,25,28,29,30,33,34,35,38,39,43 investigated the relationship between postgraduate clinical training in rural settings and rural clinical practice; adjusted ORs from eight studies20,24,28,30,33,38,39,43 were pooled for meta‐analysis. Rural residency training increased the likelihood of practising in a rural community (OR, 4.57; 95% CI, 2.80–7.46). One study found that the likelihood of practising in a rural location increased with the proportion of rural postgraduate training (v no rural training, OR: 0.1–25%, 1.9 [95% CI, 1.5–2.5]; 25.1–50%, 4.1 [95% CI, 2.8–6.0]; 50.1–99.9%, 10 [95% CI, 5.4–20]; 100%, 8.3 [95% CI, 4.5–15]).24 Four studies17,25,29,34 found that the proportion of doctors in rural practice was higher among those with rural clinical experience during residency training, and one35 that rural family medicine graduates were almost three times as likely as non‐rural graduates to practise in rural locations (RR, 2.8; 95% CI, 1.52–5.17). Seven of the eight pooled studies found that the likelihood of rural practice was higher for doctors who had at least some rural postgraduate training (OR [range], 2.6–15.5); the exception was a Canadian study which found only a statistically non‐significant increase (OR, 2.47; 95% CI, 0.91–6.73)20 (Box 5).
Studies examining multiple rural experience variables
Four studies21,24,40,41 examined the effects of two or more rural pipeline factors on practice location, but were not sufficiently similar to permit meta‐analysis. One Australian study41 found significant associations between combined rural origin and training (v metropolitan origin and training: OR, 52; 95% CI, 24–111), metropolitan origin and rural training (OR, 24; 95% CI, 13–43), and rural origin and metropolitan training (OR, 3.5; 95% CI, 1.5–7.9) on sustained rural practice for 5 years after vocational registration. In a small United States study, 70% of family physician graduates who had been raised in rural areas and completed rural family medicine clerkships (year 3) and rural preceptorships (year 4) practised in the same rural area as their first rural practice after 20–25 years, but only 46% of those who had not participated in the rural program.40 The same group had previously reported that 21% of such graduates practised family medicine in rural areas, compared with 2% of other Pennsylvania medical graduates.21 The combined effects of rural undergraduate and postgraduate training increased the odds of GPs practising in Australian rural areas (OR, 3.73; 95% CI, 2.88–4.83) compared with those who completed rural undergraduate or postgraduate training alone.24
Discussion
Attracting GPs to practise in rural and remote areas is critical for effective, coordinated health care.8,11 It is recognised that rural pipeline factors are important when recruiting and retaining rural GPs,47 and this has motivated efforts to recruit and retain domestic medical graduates in Australia,41 the US,48 and Canada.49
We found that rural background is an important predictor of later rural practice. Most studies also found a relationship between clinical experience during medical school and later rural practice, particularly the longer rural experience provided by rural longitudinal integrated clerkships,42 rural rotations of longer than three months,30 and programs with specialised rural curricula.28 These interventions may facilitate positive experience of rural practice by increasing the sense of integration into rural communities and contact with supervisors committed to rural practice.50 Providing medical undergraduates with rural training opportunities may assist skills development and knowledge acquisition as well as encouraging future rural practice.9
GPs who completed rural rotations during postgraduate training were more likely to enter rural practice than those who did not. The likelihood of practising in rural locations was correlated with increasing experience in rural areas during training.24,30 Moreover, in one recent Australian study the location of final year training was particularly influential on future practice location,41 and longer term rural training may help integrate the GP (and their family) into the community,47 consistent with our finding of an association between likelihood of rural practice and duration of rural vocational training.
The authors of a Canadian study noted that procedural skills and minor surgery types received greater emphasis during family medicine residency placements in rural and regional areas than during urban placements.38 General practice training in rural areas may therefore assist future GPs gain the generalist skills specifically required for rural practice and alleviate some of the problems that can lead to burnout (eg, professional isolation, lack of specialty support).51 Finally, several studies21,24,40,41 reported increased likelihood of rural practice for doctors with multiple rural pipeline experiences, although their individual contributions were unclear.
Our findings support the Stronger Rural Health Strategy recently announced by the Australian government,6 which includes a range of incentives and targeted funding that promote rural training for medical students and doctors, including the Rural Junior Doctor Training Innovation Fund52 and the Murray–Darling Medical Schools Network.53
Limitations
The included studies were all observational studies. The heterogeneity of investigations of rural background and rural postgraduate training was considerable, largely because of the diversity of rural definitions and the type and duration of postgraduate rural training. Many studies relied on self‐reported information, and students with pre‐existing interest in rural practice who participated in rural rotations or programs would cause self‐selection bias. Many studies did not closely define the rural environment (eg, degree of rurality, community type, duration of experience) or used different classifications of rural area for exposure and outcome. Applying binary definitions of remoteness (ie, rural v urban) may obscure important differences between regional and remote areas. Several studies adjusted their analyses for other variables, but only one24 accounted for the influence of undergraduate rural medical experience when assessing the influence of postgraduate rural experience. Similarly the influence of rural postgraduate training on the effect of undergraduate rural experience could not be assessed.
Implications for practice
Our findings support strategies that promote selecting GP registrars with rural backgrounds. While some studies suggest that rural background is the most important predictor of later rural practice,45 most GPs do not have rural backgrounds and selection on this criterion can only be part of the solution for relieving the lack of GPs in rural areas.36 Longer rural placements at both the undergraduate and postgraduate medical levels may influence commitment to rural practice. The final year of training may be particularly important for enhancing community integration and for essential clinical skills development, better preparing GPs for rural practice. Providing students and doctors with extended rural opportunities throughout training should be components of government strategies for solving rural workforce problems.
Conclusion
GPs and family physicians with rural backgrounds and rural experience during undergraduate and postgraduate medical education are more likely to enter rural practice. At the individual level, GPs working in rural areas are more likely to have rural backgrounds than those in metropolitan practices. GPs who have completed any form of rural placement or training program are more likely to work in rural practices, including GPs without rural backgrounds, showing the value for rural GP recruitment of rural clinical education for all medical students and postgraduate GP trainees.
Box 1 – Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram of study selection
Box 2 – Characteristics of the included studies
|
Study (nation) |
Design |
Population and data sources |
Geographic definitions |
Estimated effect of rural experience on practice location |
Study quality* |
||||||||||
|
|
|||||||||||||||
|
Strasser 199217 (AU) |
Cross‐sectional |
|
|
Rural upbringing, by practice location: 11.0% v 21.6% v 33.3% v 30.1% (P < 0.05‡) |
5 (good) |
||||||||||
|
Potter 199518 (US) |
Cross‐sectional |
|
|
Lived in rural community v between urban and rural/rural community (by age groups): |
5 (good) |
||||||||||
|
Fryer 199719 (US) |
Cross‐sectional |
|
|
Raised in rural community: OR, 1.68 (95% CI, 1.12–2.52) |
5 (good) |
||||||||||
|
Easterbrook 199920 (CA) |
Cross‐sectional |
|
|
Rural hometown: OR, 4.92 (95% CI, 1.98–12.1) |
5 (good) |
||||||||||
|
Rabinowitz 199921 (US) |
Cohort |
|
Practice location: rural defined as non‐standard MSA |
PSAP v non‐PSAP graduates: 21% v 2% |
6 (good) |
||||||||||
|
Wilkinson 200022 (AU) |
Case–control |
|
|
Rural background: OR, 0.82 (95% CI, 0.40–1.66) |
7 (very good) |
||||||||||
|
Laven 200323 (AU) |
Case–control |
|
|
All rural residence during primary school v none: OR, 2.89 (95% CI, 2.05–4.09) |
5 (good) |
||||||||||
|
Wilkinson 200324 (AU) |
Case–control |
|
|
Rural high school: OR, 3.18 (95% CI, 0.99–10.2) |
5 (good) |
||||||||||
|
Peach 200425 (AU) |
Cohort |
|
|
Ballarat graduates v control: 44% v 13% (P < 0.001) |
7 (very good) |
||||||||||
|
Woloschuk 200426 (CA) |
Cohort |
|
|
Raised in rural community: RR, 2.55 (95% CI, 1.01–6.42) |
2 (unsatisfactory) |
||||||||||
|
Laven 200527 (AU) |
Case–control |
|
|
Residing in rural area for 5 consecutive or 8 cumulative years (RAMUS criteria): OR, 2.50 (95% CI, 1.97–3.18) |
7 (very good) |
||||||||||
|
Nocella 200528 (US) |
Cross‐sectional |
|
|
Graduated from rural high school: OR, 5.27 (95% CI, 1.96‐14.2); P < 0.001¶ |
7 (very good) |
||||||||||
|
Pacheco 200529 (US) |
Cross‐sectional |
|
|
Rural 1+2 programs (one year in metropolitan area and two years in mixture of rural and metropolitan sites): 65.1% v 25.8% (P < 0.001‡) |
6 (good) |
||||||||||
|
Rourke 200530 (CA) |
Cross‐sectional |
|
|
Rural background: OR, 3.31 (95% CI, 1.87–5.86) |
6 (good) |
||||||||||
|
Woloschuk 200531 (CA) |
Cross‐sectional |
|
|
Rural background: OR, 2.14 (95% CI, 1.13–4.03) |
4 (satisfactory) |
||||||||||
|
Wade 200732 (US) |
Cohort |
|
|
Rural hometown: OR, 4.43 (95% CI, 2.51–7.82) |
8 (very good) |
||||||||||
|
Mathews 200833 (CA) |
Cross‐sectional |
|
|
Rural background: OR, 3.08 (95% CI, 1.79–5.29) |
7 (very good) |
||||||||||
|
Ferguson 200934 (US) |
Cross‐sectional |
|
|
Rural residency training v community health centre or urban centre: OR, 2.17 (95% CI, 1.25–3.75)‡ |
4 (satisfactory) |
||||||||||
|
Chen 201035 (US) |
Cross‐sectional |
|
|
Rural family medicine residency training program: RR, 2.8 (95% CI, 1.52–5.17) (P < 0.001¶) |
6 (good) |
||||||||||
|
McGrail 201136 (AU) |
Cohort |
|
|
1–5 years: OR, 1.20 (95% CI, 0.89–1.63) |
7 (very good) |
||||||||||
|
Orzanco 201137 (CA) |
Cohort |
|
|
Rural high school: OR, 4.03 (95% CI, 1.05–15.4) |
7 (very good) |
||||||||||
|
Jamieson 201338 (CA) |
Cohort |
|
|
Rural upbringing: OR, 1.51 (95% CI, 0.82–2.76) |
5 (good) |
||||||||||
|
Petrany 201339 (US) |
Cohort |
|
|
Rural track residency v traditional track: OR, 7.54 (95% CI, 1.50–37.9) |
6 (good) |
||||||||||
|
Rabinowitz 201340 (US) |
Cohort |
|
|
Rural background and completion of a 6‐week clerkship in family medicine in a small town (year 3) and a rural preceptorship (year 4): 70% v 46% for non‐PSAP graduates (P = 0.02‡) |
6 (good) |
||||||||||
|
McGrail 201641 (AU) |
Cohort |
|
|
v Metropolitan origin and training: |
7 (very good) |
||||||||||
|
Myhre 201642 (CA) |
Cohort |
|
|
For rural LIC graduates: |
7 (very good) |
||||||||||
|
Nelson 201743 (US) |
Cohort |
|
|
Rural residency: OR, 14.0 (95% CI, 2.90–67.4) (P < 0.01¶) |
6 (good) |
||||||||||
|
|
|||||||||||||||
|
AU = Australia; CA = Canada; US = United States. AMA = American Medical Association; ASGC‐RA = Australian Standard Geographic Classification Remoteness Areas;44 CI = confidence interval; DO = Doctor of Osteopathy; MABEL = Medicine in Australia: Balancing Employment and Life study; MD = Doctor of Medicine; MSA = metropolitan statistical area; OR = odds ratio; PSAP = Physician Shortage Area Program; RACGP = Royal Australian College of General Practitioners; RAMUS = Rural Australia Medical Undergraduate Scholarship; RR = rate ratio; RRMA = Rural and Remote Metropolitan Areas classification;45 RUCA = Rural–Urban Commuting Area;46 UdeS = Université de Sherbrooke; UMMS = University of Massachusetts Medical School; USDA = US Department of Agriculture. * Newcastle–Ottawa scale score. † Calculated from reported denominator (n = 1128) and overall response rate (74.6%). ‡ Calculated from article data. § Medical school rural program for students with rural backgrounds; they complete a 6‐week clerkship in family medicine in a small town (year 3) and a rural preceptorship (year 4). ¶ 95% CI calculated from reported P value, or upper estimate when P < 0.001. ** Calculated from reported numerators and proportions. |
|||||||||||||||
Box 3 – Studies comparing influence of background (rural v urban) on likelihood of general practitioners or family physicians practising in rural locations

CI = confidence interval; OR = odds ratio (instrumental variability, random); SE = standard error.
Heterogeneity: τ2 = 0.06; χ2 = 16.7 (P = 0.05); l2 = 46%. Test for overall effect: Z = 7.95 (P < 0.001).
Box 4 – Studies comparing influence of location of undergraduate medical training (rural v urban) on likelihood of general practitioners or family physicians practising in rural locations

CI = confidence interval; OR = odds ratio (instrumental variability, random); SE = standard error.
Heterogeneity: τ2 = 0.00; χ2 = 3.94 (P = 0.41); l2 = 0%. Test for overall effect: Z = 6.42 (P < 0.001).
Box 5 – Studies comparing influence of location of postgraduate medical training (rural v urban) on likelihood of general practitioners or family physicians practising in rural locations

CI = confidence interval; OR = odds ratio (instrumental variability, random); SE = standard error.
Heterogeneity: τ2 = 0.28; χ2 = 23.6 (P = 0.001); l2 = 70%. Test for overall effect: Z = 6.08 (P < 0.001).
Received 12 February 2019, accepted 24 March 2020
- Jessica Ogden1
- Scott Preston1
- Riitta L Partanen2
- Remo Ostini3
- Peter Coxeter1
- 1 General Practice Training Queensland, Brisbane, QLD
- 2 Rural Clinical School, University of Queensland, Hervey Bay, QLD
- 3 Rural Clinical School, University of Queensland, Toowoomba, QLD
No relevant disclosures.
- 1. Standing Council on Health. National strategic framework for rural and remote health. Updated Apr 2016. http://www.health.gov.au/internet/main/publishing.nsf/Content/national-strategic-framework-rural-remote-health (viewed Mar 2020).
- 2. World Health Organization. Increasing access to health workers in remote and rural areas through improved retention: global policy recommendations. Geneva: WHO, 2010. https://www.who.int/hrh/retention/guidelines/en (viewed Mar 2020).
- 3. Australian Institute of Health and Welfare. Australia's health 2018 (Cat no. AUS 221; Australia's health series, no. 16.). Canberra: AIHW, 2018.
- 4. Australian Institute of Health and Welfare. Rural and remote health [web report]. Updated Oct 2019. https://www.aihw.gov.au/reports/rural-health/rural-remote-health/contents/rural-health (viewed Mar 2020).
- 5. Mason J. Review of Australian Government health workforce programs. Updated May 2013. http://www.health.gov.au/internet/main/publishing.nsf/Content/review-australian-government-health-workforce-programs (viewed Mar 2020).
- 6. Australian Department of Health. Stronger Rural Health Strategy: factsheets. Updated Nov 2019. http://www.health.gov.au/internet/main/publishing.nsf/Content/stronger-rural-health-strategy-factsheets (viewed Mar 2020).
- 7. Duckett S, Breadon P, Ginnivan L. Access all areas: new solutions for GP shortages in rural Australia. Melbourne: Grattan Institute, 2013. https://grattan.edu.au/wp-content/uploads/2014/04/196-Access-All-Areas.pdf (viewed Mar 2020).
- 8. Soles TL, Ruth Wilson C, Oandasan IF. Family medicine education in rural communities as a health service intervention supporting recruitment and retention of physicians: Advancing Rural Family Medicine: the Canadian Collaborative Taskforce. Can Fam Physician 2017; 63: 32–38.
- 9. Barrett FA, Lipsky MS, Lutfiyya MN. The impact of rural training experiences on medical students: a critical review. Acad Med 2011; 86: 259–263.
- 10. Laven G, Wilkinson D. Rural doctors and rural backgrounds: how strong is the evidence? A systematic review. Aust J Rural Health 2003; 11: 277–284.
- 11. Russell DJ, McGrail MR, Humphreys JS. Determinants of rural Australian primary health care worker retention: a synthesis of key evidence and implications for policymaking. Aust J Rural Health 2017; 25: 5–14.
- 12. Wenghofer EF, Hogenbirk JC, Timony PE. Impact of the rural pipeline in medical education: practice locations of recently graduated family physicians in Ontario. Hum Resour Health 2017; 15: 16.
- 13. Fisher KA, Fraser JD. Rural health career pathways: research themes in recruitment and retention. Aust Health Rev 2010; 34: 292–296.
- 14. Henry JA, Edwards BJ, Crotty B. Why do medical graduates choose rural careers? Rural Remote Health 2009; 9: 1083.
- 15. Tesson G, Strasser R, Pong RW, Curran V. Advances in rural medical education in three countries: Canada, the United States and Australia. Rural Remote Health 2005; 5: 397.
- 16. Wells GA, Shea B, O'Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. Updated July 2000. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (viewed Mar 2020).
- 17. Strasser R. Attitudes of Victorian rural GPs to country practice and training. Aust Fam Physician 1992; 21: 808–812.
- 18. Potter J. Characteristics of Alaskan family physicians as determinants of practice location. Alaska Med 1995; 37: 49–52.
- 19. Fryer GE, Stine C, Vojir C, Miller M. Predictors and profiles of rural versus urban family practice. Fam Med 1997; 29: 115–118.
- 20. Easterbrook M, Godwin M, Wilson R, et al. Rural background and clinical rural rotations during medical training: effect on practice location. CMAJ 1999; 160: 1159–1163.
- 21. Rabinowitz HK, Diamond JJ, Markham FW, Hazelwood CE. A program to increase the number of family physicians in rural and underserved areas: impact after 22 years. JAMA 1999; 281: 255–260.
- 22. Wilkinson D, Beilby JJ, Thompson DJ, et al. Associations between rural background and where South Australian general practitioners work. Med J Aust 2000; 173: 137–140.
- 23. Laven GA, Beilby JJ, Wilkinson D, McElroy HJ. Factors associated with rural practice among Australian‐trained general practitioners. Med J Aust 2003; 179: 75–79. https://www.mja.com.au/journal/2003/179/2/factors-associated-rural-practice-among-australian-trained-general-practitioners
- 24. Wilkinson D, Laven G, Pratt N, Beilby J. Impact of undergraduate and postgraduate rural training, and medical school entry criteria on rural practice among Australian general practitioners: national study of 2414 doctors. Med Educ 2003; 37: 809–814.
- 25. Peach HG, Trembath M, Fensling B. A case for more year‐long internships outside metropolitan areas? Med J Aust 2004; 180: 106–108. https://www.mja.com.au/journal/2004/180/3/case-more-year-long-internships-outside-metropolitan-areas
- 26. Woloschuk W, Tarrant M. Do students from rural backgrounds engage in rural family practice more than their urban‐raised peers? Med Educ 2004; 38: 259–261.
- 27. Laven GA, Wilkinson D, Beilby JJ, McElroy HJ. Empiric validation of the rural Australian Medical Undergraduate Scholarship “rural background” criterion. Aust J Rural Health 2005; 13: 137–141.
- 28. Nocella IC. Recruitment of family physicians into rural California: predictors and possibilities. Thesis [PhD]: University of Southern California, 2005. http://digitallibrary.usc.edu/cdm/ref/collection/p15799coll16/id/613977 (viewed Mar 2020).
- 29. Pacheco M, Weiss D, Vaillant K, et al. The impact on rural New Mexico of a family medicine residency. Acad Med 2005; 80: 739–744.
- 30. Rourke JT, Incitti F, Rourke LL, Kennard M. Relationship between practice location of Ontario family physicians and their rural background or amount of rural medical education experience. Can J Rural Med 2005; 10: 231–240.
- 31. Woloschuk W, Crutcher R, Szafran O. Preparedness for rural community leadership and its impact on practice location of family medicine graduates. Aust J Rural Health 2005; 13: 3–7.
- 32. Wade ME, Brokaw JJ, Zollinger TW, et al. Influence of hometown on family physicians’ choice to practice in rural settings. Fam Med 2007; 39: 248–254.
- 33. Mathews M, Rourke JT, Park A. The contribution of Memorial University's medical school to rural physician supply. Can J Rural Med 2008; 13: 15–21.
- 34. Ferguson WJ, Cashman SB, Savageau JA, Lasser DH. Family medicine residency characteristics associated with practice in a health professions shortage area. Fam Med 2009; 41: 405–410.
- 35. Chen F, Fordyce M, Andes S, Hart LG. Which medical schools produce rural physicians? A 15‐year update. Acad Med. 2010; 85: 594–598.
- 36. McGrail MR, Humphreys JS, Joyce CM. Nature of association between rural background and practice location: a comparison of general practitioners and specialists. BMC Health Serv Res 2011; 11: 63.
- 37. Orzanco MG, Lovato C, Bates J, et al. Nature and nurture in the family physician's choice of practice location. Rural Remote Health 2011; 11: 1849.
- 38. Jamieson JL, Kernahan J, Calam B, Sivertz KS. One program, multiple training sites: does site of family medicine training influence professional practice location? Rural Remote Health 2013; 13: 2496.
- 39. Petrany SM, Gress T. Comparison of academic and practice outcomes of rural and traditional track graduates of a family medicine residency program. Acad Med 2013; 88: 819–823.
- 40. Rabinowitz HK, Diamond JJ, Markham FW, Santana AJ. Retention of rural family physicians after 20–25 years: outcomes of a comprehensive medical school rural program. J Am Board Fam Med 2013; 26: 24–27.
- 41. McGrail MR, Russell DJ, Campbell DG. Vocational training of general practitioners in rural locations is critical for the Australian rural medical workforce. Med J Aust 2016; 205: 216–221. https://www.mja.com.au/journal/2016/205/5/vocational-training-general-practitioners-rural-locations-critical-australian
- 42. Myhre DL, Bajaj S, Woloschuk W. Practice locations of longitudinal integrated clerkship graduates: a matched‐cohort study. Can J Rural Med 2016; 21: 13–16.
- 43. Nelson GC, Gruca TS. Determinants of the 5‐year retention and rural location of family physicians: results from the Iowa Family Medicine Training Network. Fam Med 2017; 49: 473–476.
- 44. Australian Department of Health. Australian Standard Geographic Classification — Remoteness Areas. Updated July 2019. https://www.health.gov.au/health-workforce/health-workforce-classifications/australian-statistical-geographical-classification-remoteness-area (viewed Mar 2020).
- 45. Australian Department of Health. Rural, remote and metropolitan area. Updated Feb 2020. https://www.health.gov.au/health-workforce/health-workforce-classifications/rural-remote-and-metropolitan-area (viewed Mar 2020).
- 46. WWAMI Rural Health Research Center. RUCA data. Undated. https://depts.washington.edu/uwruca/ruca-uses.php (viewed Mar 2020).
- 47. Brooks RG, Walsh M, Mardon RE, et al. The roles of nature and nurture in the recruitment and retention of primary care physicians in rural areas: a review of the literature. Acad Med 2002; 77: 790–798.
- 48. Parlier AB, Galvin SL, Thach S, et al. The road to rural primary care: a narrative review of factors that help develop, recruit, and retain rural primary care physicians. Acad Med 2018; 93: 130–140.
- 49. Pong RW, Heng D. The link between rural medical education and rural medical practice location: literature review and synthesis. Sudbury [ON], Canada: Centre for Rural and Northern Health Research, Laurentian University, 2005. http://documents.cranhr.ca/pdf/Physician_Planning_Unit_report_Final.pdf (viewed Mar 2020).
- 50. Viscomi M, Larkins S, Gupta TS. Recruitment and retention of general practitioners in rural Canada and Australia: a review of the literature. Can J Rural Med 2013; 18: 13–23.
- 51. Cutchin MP, Norton JC, Quan MM, et al. To stay or not to stay: issues in rural primary care physician retention in eastern Kentucky. J Rural Health 1994; 10: 273–278.
- 52. Australian Department of Health. Stronger Rural Health Strategy: junior doctor training. Updated Dec 2018. http://www.health.gov.au/internet/main/publishing.nsf/Content/stronger-rural-health-strategy-junior-doctor-training (viewed Mar 2020).
- 53. Australian Department of Health. Stronger Rural Health Strategy: the Murray–Darling Medical Schools Network. Updated Dec 2018. http://www.health.gov.au/internet/main/publishing.nsf/Content/stronger-rural-health-strategy-the-murray-darling-medical-schools-network (viewed Mar 2020).





Abstract
Objective: To synthesise quantitative data on the effects of rural background and experience in rural areas during medical training on the likelihood of general practitioners practising and remaining in rural areas.
Study design: Systematic review and meta‐analysis of the effects of rural pipeline factors (rural background; rural clinical and education experience during undergraduate and postgraduate/vocational training) on likelihood of later general practice in rural areas.
Data sources: MEDLINE (Ovid), EMBASE, Informit Health Collection, and ERIC electronic database records published to September 2018; bibliographies of retrieved articles; grey literature.
Data synthesis: Of 6709 publications identified by our search, 27 observational studies were eligible for inclusion in our systematic review; when appropriate, data were pooled in random effects models for meta‐analysis. Study quality, assessed with the Newcastle–Ottawa scale, was very good or good for 24 studies, satisfactory for two, and unsatisfactory for one. Meta‐analysis indicated that GPs practising in rural communities was significantly associated with having a rural background (odds ratio [OR], 2.71; 95% CI, 2.12–3.46; ten studies) and with rural clinical experience during undergraduate (OR, 1.75; 95% CI, 1.48–2.08; five studies) and postgraduate training (OR, 4.57; 95% CI, 2.80–7.46; eight studies).
Conclusion: GPs with rural backgrounds or rural experience during undergraduate or postgraduate medical training are more likely to practise in rural areas. The effects of multiple rural pipeline factors may be cumulative, and the duration of an experience influences the likelihood of a GP commencing and remaining in rural general practice. These findings could inform government‐led initiatives to support an adequate rural GP workforce.
Protocol registration: PROSPERO, CRD42017074943 (updated 1 February 2018).