The known: Iodine deficiency re‐emerged in Australia in the 1990s, motivating mandatory fortification of bread with iodised salt in 2009.
The new: The median urinary iodine concentration of 368 young Northern Territory residents increased from 58 μg/L (interquartile range [IQR], 35–83 μg/L) to 101 μg/L (IQR, 66–163 μg/L) after fortification became mandatory. Urban Indigenous and non‐Indigenous participants achieved adequate iodine levels, but remote Indigenous and urban non‐Indigenous women were still mildly iodine‐deficient.
The implications: Although iodine fortification has generally been successful, targeted interventions are needed to improve intake by some Australians, particularly women of child‐bearing age.
Iodine deficiency returned as a significant public health problem in Australia during the 1990s.1 It had historically existed in the southeast of the mainland and in Tasmania,2 but deliberate strategies2 and unintentional iodine supplementation1 had led to its disappearance until it re‐emerged in some parts of Australia.3
Adding iodised salt to bread has been a strategy for improving population iodine levels at various times and locations since the mid‐20th century.2 In response to national data that indicated Australian children were mildly iodine‐deficient, fortification of salt used in bread has been mandatory across Australia since October 2009.4 Subsequently, several surveys of urinary iodine concentration (UIC) have indicated that this initiative improved the iodine status of children aged 8–10 years (internationally the sentinel age group for population iodine status assessment5). In the mainland states, national surveys found that the median UIC for younger children was higher in 2011–12 (177 μg/L)6 than in 2003 (104 μg/L).3 In Tasmania, the median UIC increased after voluntary replacement of salt in bread with iodised salt was introduced, and still further after it became mandatory.7
Prior to mandatory fortification, national data on the iodine status of the Australian adult population were limited to data for pregnant women.8 Iodine status was inferred from dietary data, as were the predicted effects of fortification options for adults.4 After fortification was introduced, biomedical data collected in national health surveys indicated that both the general Australian and the Indigenous adult populations had adequate iodine levels.6,9
We have previously reported that Indigenous young people in the Top End of the Northern Territory were classified as mildly to moderately iodine‐deficient prior to fortification.10 We now report the iodine status of this Indigenous population following fortification, and also include data on the pre‐ and post‐fortification iodine status of non‐Indigenous Territorians of the same age. We aimed to provide insights into the impact of mandatory fortification on the iodine status of young adults in the NT, particularly young women of reproductive age.
Methods
The Life Course Program based in Darwin includes two complementary prospective cohorts: the Aboriginal Birth Cohort (ABC) and the non‐Indigenous Top End Cohort (TEC). The recruitment of the two cohorts has been described previously.11,12 Briefly, the ABC consists of 686 people recruited at birth, born to Indigenous Australian mothers at the Royal Darwin Hospital between January 1987 and March 1990.11 This group was followed up during 2006–200713 and 2013–15.14 The TEC comprises 196 non‐Indigenous people recruited and assessed during November 2007 – September 2009.12 Eligibility criteria were birth during 1987–1991 (ie, age‐matched with the ABC) in Darwin to a non‐Indigenous mother and residing in Darwin at the time of recruitment. The TEC participants were followed up during 2013–15, parallel to the follow‐up of ABC participants.15
The iodine status of the two cohorts was assessed before and after the implementation date for mandatory fortification. In this article, “pre‐fortification” refers to data from the 2006–2007 follow‐up of the Indigenous ABC group and the first assessment of the non‐Indigenous TEC group during 2007–2009, and “post‐fortification” to the 2013–15 follow‐up of both groups.
Comprehensive health assessments with the same procedures were undertaken in the participants’ communities of residence. Barefoot height was measured to the nearest millimetre with a portable calibrated wall‐mounted stadiometer, and weight in light clothing was measured to 0.1 kg with a digital electronic scale (Tanita TBF‐521) for calculating body mass index (BMI; kg/m2).
A random spot urine sample was collected and kept cool (on ice or in a refrigerator) until aliquoted into labelled microtubes and frozen (within 2 hours of collection); it was then transported to Darwin and stored at –80°C, before being transported on dry ice to the Institute of Clinical Pathology and Medical Research (ICPMR) at Westmead Hospital in Sydney. The ICPMR iodine laboratory participates in the External Quality Assurance Program, the Centers for Disease Control (United States) standardisation program for providing urinary iodine laboratories with independent assessment of their analytic performance, and is the regional reference laboratory for iodine assays in the Asia–Pacific region. Samples were subjected to ammonium persulfate digestion prior to assessment of iodine levels with the Sandell–Kolthoff reaction in microtitre plates.
For men and non‐pregnant women, median UICs were interpreted according to World Health Organization criteria: the iodine status of a population is defined as adequate if the median UIC is 100–199 μg/L, as mildly deficient with a median UIC of 50–99 μg/L, moderately deficient with a median UIC of 20–49 μg/L, and severely deficient if the median UIC is less than 20 μg/L.5 For pregnant women, a median UIC of at least 150 μg/L is deemed adequate.5
Residence at the date of collection was classified as remote (remote community with an Aboriginal council) or urban (Darwin and rural towns). Women were classified as pregnant if they had reported they were pregnant when assessed or a birth was recorded in the NT Perinatal Collection registry up to 9 months after the assessment.
Statistical analysis
Median UICs (with interquartile ranges [IQRs]) were calculated for men and non‐pregnant women seen at either assessment time point, and separately for the subset of participants assessed on both occasions. The characteristics of this subset were compared with those of all available Indigenous and non‐Indigenous participants in Mann–Whitney U tests. UICs were log‐transformed as the distribution of values was skewed. The association between Indigenous status and area of residence was modelled by linear regression, with log‐normal iodine concentration the outcome variable, and Indigenous status, remoteness of residence, sex, and BMI the explanatory variables.
Unadjusted differences in non‐transformed median UIC between periods were assessed in Wilcoxon signed‐rank tests; P < 0.05 was deemed statistically significant. Statistical analyses were performed in Stata 15.1 (StataCorp).
Ethics approval
This study was approved by the Human Research Ethics Committee of the NT Department of Health and Menzies School of Health Research; this includes approval by the Aboriginal Ethics Subcommittee, which has the power of veto (ABC reference, 2013‐2022; TEC reference, 2013‐1986).
Results
Urinary iodine concentrations (UICs) of 25 pre‐fortification samples (24 Indigenous participants, one non‐Indigenous participant) and three post‐fortification samples (all Indigenous participants) below the limit of detection (10 μg/L) were assigned values of 5 μg/L for the purposes of our analyses.
Median UIC values were similar whether analysis was restricted to men and non‐pregnant women who were assessed both pre‐ and post‐fortification (368 participants) or all available data were analysed (pre‐fortification, 589 participants; post‐fortification, 508 participants) (Box 1). Most Indigenous participants (80%) lived in remote areas at both assessments; the number in each location type varied with time because of movement between remote and urban locations, but the numbers were small (post‐ v pre‐fortification: 19 remote participants moved to urban areas [7%] and 11 urban participants to remote areas [4%]).
Pre‐fortification median urinary iodine concentrations
The pre‐fortification median UIC for all participants assessed at both time points was 58 μg/L (IQR, 35–83 μg/L; Box 1). The values for each group were substantially below the minimum desirable level of 100 μg/L: for remote Indigenous participants, 53.0 μg/L (IQR, 28–75 μg/L); for urban Indigenous participants, 67.0 μg/L (IQR, 51–90 μg/L); and for urban non‐Indigenous participants, 73.0 μg/L (IQR, 40–107 μg/L) (Box 2). Levels were significantly lower for Indigenous participants in remote locations than for urban Indigenous (P = 0.001) and urban non‐Indigenous participants (P < 0.001), and this difference remained after adjusting for sex and BMI (v urban non‐Indigenous participants: P = 0.006; v urban non‐Indigenous participants: P = 0.001). The median UICs for Indigenous and non‐Indigenous urban participants were not significantly different (P = 0.60).
Among non‐Indigenous urban participants, the median UIC was significantly lower for non‐pregnant women than for men (P = 0.001); sex differences were not significant for remote (P = 0.08) or urban Indigenous participants (P = 0.07) (Box 3).
Post‐fortification median urinary iodine concentrations
The post‐fortification median UIC for all participants assessed at both time points was 101.0 μg/L (IQR, 66–163 μg/L), significantly higher than the pre‐fortification value (P < 0.001). Values for urban Indigenous (127.0 μg/L; IQR, 94–203 μg/L) and non‐Indigenous participants (117.0 μg/L; IQR, 65–160 μg/L) were now within the desirable range; the median UIC for remote Indigenous participants (94.0 μg/L; IQR 63–152 μg/L) was slightly lower than the recommended 100 μg/L (mildly deficient) (Box 2). After adjusting for sex, the median UIC for remote Indigenous participants was significantly lower than that for urban Indigenous participants (P = 0.015) but not that of non‐Indigenous urban participants (P = 0.28). The difference between remote and urban Indigenous participants was not significant after also adjusting for BMI.
Among non‐Indigenous urban participants, the median UIC for non‐pregnant women was significantly lower than for men (P < 0.001); sex differences were not significant for remote (P = 0.33) or urban Indigenous participants (P = 0.90). After stratifying by sex, the post‐fortification median UIC was significantly higher than the pre‐fortification levels for remote (P < 0.001) and urban Indigenous participants (P = 0.004), but not for urban non‐Indigenous participants (P = 0.99) (Box 3).
Urinary iodine concentrations in pregnant women
Urinary iodine was assessed in 22 pregnant women pre‐fortification (18 remote Indigenous, four urban Indigenous participants) and in 24 women post‐fortification (14 remote Indigenous, seven urban Indigenous, three urban non‐Indigenous participants). Given the importance of iodine during pregnancy, we calculated the median UIC of pregnant women, despite the small numbers of participants: the median pre‐fortification concentration was 48.0 μg/L (IQR, 36–67 μg/L), the median post‐fortification level 93.0 μg/L (IQR, 62–171 μg/L); both values were below the recommended minimum of 150 μg/L (Box 4).
Discussion
The median UIC among remote and urban Indigenous young people and urban non‐Indigenous young people in the NT Top End increased substantially after mandatory iodine fortification was introduced. However, the median UICs for remote Indigenous men and non‐pregnant women and for urban non‐Indigenous non‐pregnant women were still slightly below recommended levels. Our pre‐fortification data for the two cohorts are the only Australian data on the iodine status of non‐clinical adult populations.
Iodine fortification of salt used in bread is the most likely explanation for the increased urinary iodine levels. Our results are consistent with the change in urinary concentration predicted on the basis of the iodine concentrations in bread after fortification and the bread intake in remote areas reported in national surveys.16 The increase in dietary iodine intake by a non‐pregnant adult can be estimated from their body weight with a standard formula.17 For example, the estimated median intake by remote Indigenous women rose from 72 μg to 132 μg per day after fortification. Other possible explanations for increased urinary iodine levels include increased iodide levels in drinking water, greater consumption of dairy products and fish, and increased use of iodised salt. We did not assess fish or iodised salt consumption, but there were no changes in water sources in Top End communities during the study period. Bread consumption varies widely between individuals, and lower consumption could explain the smaller increases in some population groups.
The UIC interquartile range was generally broader after fortification became mandatory. This is expected, as the intervention added iodine to a dietary component that is not eaten in the same amounts each day. A similar phenomenon was observed in Tasmania during the voluntary iodine fortification program.18 Signs of iodine deficiency, such as intellectual impairment, are generally not evident in people with a mild deficiency. The UIC, however, is not an appropriate measure of the iodine status of an individual because it varies considerably according to time of day and recent intake, for example. Physical examinations and thyroid functions tests conducted as part of the comprehensive health check in our study did not find any abnormalities in participants (data not shown).
Despite the rises in median UIC with mandatory fortification, the values for women of child‐bearing age remained in the mildly deficient range; further, the median UIC for pregnant women was low, and the median UIC for pregnant Indigenous women in remote locations was less than half the recommended level for pregnant women, suggesting that iodine supplementation — recommended by the National Health and Medical Research Council for all pregnant and breastfeeding women19 — was not being practised. National surveys in Australia do not oversample pregnant women, so their characteristics cannot be explored in specific analyses. However, our limited data suggest that pregnant women living in previously iodine‐deficient parts of Australia may still be iodine‐deficient; this question requires further investigation.
The median UIC values for our populations were lower than reported by national surveys: the median UIC for adults aged 18–24 years in the general Australian population (2011–12) was 138 μg/L,5 for the Indigenous Australian population (2012–13), 135 μg/L.9 Median UIC was similar for Indigenous men and women (135 v 134 μg/L),9 but was higher for men than women in the general Australian population (131 v 118 μg/L).6 It was higher for remote than urban Indigenous adults, but the proportion of people with low iodine values did not vary by remoteness. Unlike the national data, we found that the median UIC for some population groups is still below the recommended level of 100 μg/L. The sex difference in median UIC was greater for non‐Indigenous than Indigenous participants, regardless of remoteness of residence. Median UICs for urban Indigenous and non‐Indigenous young adults were similar, but the median UIC for remote Indigenous participants was lower than both.
The differences between our results and those of national surveys are probably explained by differences in the characteristics of participants in our Life Course Program, reflecting the fact that national and state‐level results can mask local variations. Most Indigenous people in the ABC live remotely (76%), and many reside either in remote communities with small populations (fewer than 500 people) or on outstations (fewer than 50 people). In the 2012–13 national study, only 40% of participants completed the biomedical component of the survey;20 further, the national study excluded some Indigenous communities “in the NT, in remote areas with a small number of Aboriginal and Torres Strait Islander households.”21
Conclusions
We found that the median urinary iodine concentrations of young people in the Top End of the NT increased following the introduction of mandatory fortification of bread in Australia. However, median levels for some groups, particularly pregnant women and women of child‐bearing age, remain in the mildly deficient range. Iodine requirements are greatest during pregnancy when the fetus is most vulnerable to the deleterious effects of iodine deficiency. Targeted interventions are needed to improve iodine intake in some sections of the Australian population, particularly women of child‐bearing age, to complement the broad population strategy.
Box 1 – Median urine iodine concentrations of non‐pregnant participants, pre‐ and post‐fortification
|
|
Pre‐fortification* |
Post‐fortification† |
|||||||||||||
|
|
|||||||||||||||
|
All non‐pregnant participants |
|
|
|||||||||||||
|
Number of participants |
589 |
508 |
|||||||||||||
|
Sex (men) |
277 (47%) |
229 (45%) |
|||||||||||||
|
Urinary iodine (μg/L), median (IQR) |
58 (36–88) |
103 (67–167) |
|||||||||||||
|
Non‐pregnant participants assessed at both time points |
|
|
|||||||||||||
|
Number of participants |
368 |
368 |
|||||||||||||
|
Sex (men) |
180 (49%) |
180 (49%) |
|||||||||||||
|
Urinary iodine (μg/L), median (IQR) |
58 (35–83) |
101 (66–163) |
|||||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range. * Indigenous participants: 2006–2007; non‐Indigenous participants: 2007–2009. † Both groups: 2013–2015. |
|||||||||||||||
Box 2 – Characteristics of men and non‐pregnant women who were assessed both pre‐ and post‐fortification, by Indigenous identification and location
|
|
Indigenous Australians |
Non‐Indigenous |
|||||||||||||
|
Remote |
Urban |
Urban |
|||||||||||||
|
|
|||||||||||||||
|
Pre‐fortification* |
|
|
|
||||||||||||
|
Total number |
233 |
49 |
86 |
||||||||||||
|
Sex (men) |
123 (53%) |
25 (51%) |
33 (38%) |
||||||||||||
|
Age (years), mean (SD) |
17.8 (1.1) |
17.9 (1.1) |
18.2 (1.4) |
||||||||||||
|
Height (cm), median (IQR) |
166.5 (161–173) |
169.4 (164–176) |
169.1 (163–178) |
||||||||||||
|
Weight (kg), median (IQR) |
54.0 (49–63) |
65.4 (55–81) |
63.9 (57–75) |
||||||||||||
|
BMI (kg/m2), median (IQR) |
19.0 (17–23) |
22.7 (19–27) |
21.8 (20–24) |
||||||||||||
|
Urinary iodine (μg/L), median (IQR) |
53.0 (28–75) |
67.0 (51–90) |
73.0 (40–107) |
||||||||||||
|
Post‐fortification† |
|
|
|
||||||||||||
|
Total number |
225 |
57 |
86 |
||||||||||||
|
Age (years), mean (SD) |
25.2 (1.1) |
25.4 (1.2) |
23.8 (1.4) |
||||||||||||
|
Sex (men) |
118 (52%) |
30 (53%) |
33 (38%) |
||||||||||||
|
Height (cm), median (IQR) |
167.0 (161–173) |
169.5 (164–178) |
170.0 (164–179) |
||||||||||||
|
Weight (kg), median (IQR) |
62.0 (52–72) |
76.2 (64–89) |
69.4 (60–85) |
||||||||||||
|
BMI (kg/m2), median (IQR) |
22.7 (19–26) |
26.6 (22–29) |
23.5 (22–27) |
||||||||||||
|
Urinary iodine (μg/L), median (IQR) |
94.0 (63–152) |
127.0 (94–203) |
117.0 (65–160) |
||||||||||||
|
|
|||||||||||||||
|
BMI = body mass index; IQR = interquartile range; SD = standard deviation. * Indigenous participants: 2006–2007; non‐Indigenous participants: 2007–2009. † Both groups: 2013–2015. |
|||||||||||||||
Box 3 – Distribution of urine iodine concentration values by sex, Indigenous identification, and location of residence, pre‐ and post‐fortification
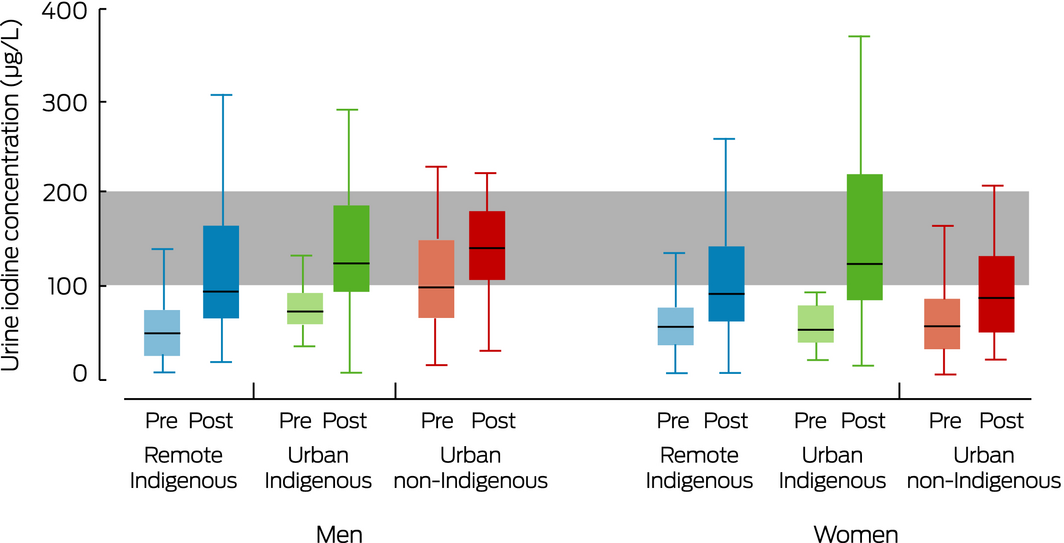
The shaded area indicates the adequate population iodine concentration range (100–199 μg/L).5 Box and whisker plot definitions: the centre line marks the median value, the box marks the interquartile range (IQR), the whiskers mark the most extreme values within the upper (Q3 + 1.5 × IQR) and lower (Q1 – 1.5 × IQR) adjacent value limits.
Box 4 – Median urine iodine concentrations of pregnant women, pre‐ and post‐fortification
|
|
Pre‐fortification* |
Post‐fortification† |
|||||||||||||
|
|
|||||||||||||||
|
Indigenous (remote) |
|
|
|||||||||||||
|
Number of women |
18 |
14 |
|||||||||||||
|
Urinary iodine (μg/L), median (IQR) |
46 (32–53) |
64 (41–89) |
|||||||||||||
|
Indigenous (urban) |
|
|
|||||||||||||
|
Number of women |
4 |
7 |
|||||||||||||
|
Urinary iodine (μg/L), median (IQR) |
72 (58–105) |
122 (101–254) |
|||||||||||||
|
Non‐Indigenous (urban) |
|
|
|||||||||||||
|
Number of women |
0 |
3 |
|||||||||||||
|
Urinary iodine (μg/L), median (IQR) |
— |
165 (82–169) |
|||||||||||||
|
All pregnant women |
|
|
|||||||||||||
|
Number of women |
22 |
24 |
|||||||||||||
|
Urinary iodine (μg/L), median (IQR) |
48 (36–67) |
93 (62–171) |
|||||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range. * Indigenous participants: 2006–2007; non‐Indigenous participants: 2007–2009. † Both groups: 2013–2015. |
|||||||||||||||
Received 22 March 2018, accepted 1 August 2018
- Gurmeet R Singh1
- Belinda Davison1
- Gary Y Ma2
- Creswell J Eastman3,4
- Dorothy EM Mackerras5
- 1 Menzies School of Health Research, Darwin, NT
- 2 Western Sydney University School of Medicine, Penrith, NSW
- 3 Sydney Thyroid Clinic, Sydney, NSW
- 4 Sydney Medical School, Sydney, NSW
- 5 Food Standards Australia New Zealand, Canberra, ACT
This investigation was supported by the National Health and Medical Research Council (APP1046391). We acknowledge past and present study teams who traced participants and collected the data, particularly the late Susan Sayers, founder of the ABC study. We thank Victor Uguoma for his statistical advice. We especially thank the young adults in the Aboriginal Birth and Top End Cohorts and their families and communities for their cooperation and support, and all the individuals who helped in urban and rural locations.
Dorothy Mackerras is employed by Food Standards Australia New Zealand, the agency that introduced mandatory iodine fortification.
- 1. Li M, Waite KV, Ma G, Eastman CJ. Declining iodine content of milk and re‐emergence of iodine deficiency in Australia. Med J Aust 2006; 184: 307. https://www.mja.com.au/journal/2006/184/6/declining-iodine-content-milk-and-re-emergence-iodine-deficiency-australia
- 2. Clements F, Gibson H, Howeler‐Coy J. Goitre prophylaxis by addition of potassium iodate to bread: experience in Tasmania. Lancet 1970; 295: 489–492.
- 3. Li M, Eastman CJ, Waite KV, et al. Are Australian children iodine deficient? Results of the Australian National Iodine Nutrition Study. Med J Aust 2006; 184: 165–169. https://www.mja.com.au/journal/2006/184/4/are-australian-children-iodine-deficient-results-australian-national-iodine
- 4. Food Standards Australia New Zealand. Proposal P1003. Mandatory iodine fortification for Australia: approval report. 6 Aug 2008. http://www.foodstandards.gov.au/code/proposals/documents/AppR_P1003_Mandatory_Iodine_Fortification_Aust%20AppR.pdf (viewed Feb 2018).
- 5. World Health Organization. Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers. Third edition. Geneva: WHO, 2007. http://www.who.int/nutrition/publications/micronutrients/iodine_deficiency/9789241595827/en/ (viewed Feb 2018).
- 6. Australian Bureau of Statistics. 4364.0.55.006. Australian Health Survey: biomedical results for nutrients, 2011–12. Iodine. Dec 2013. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.006Chapter1202011-12 (viewed Sept 2018).
- 7. Hynes KL, Seal JA, Otahal P, et al. Iodine adequacy in Tasmania sustained after 7 years of mandatory bread fortification. Med J Aust 2018; 208: 126. https://www.mja.com.au/journal/2018/208/3/iodine-adequacy-tasmania-sustained-after-7-years-mandatory-bread-fortification
- 8. Rahman A, Savige GS, Deacon NJ, et al. Urinary iodine deficiency in Gippsland pregnant women: the failure of bread fortification. Med J Aust 2011; 194: 240–243. https://www.mja.com.au/journal/2011/194/5/urinary-iodine-deficiency-gippsland-pregnant-women-failure-bread-fortification
- 9. Australian Bureau of Statistics. 4727.0.55.003. Australian Aboriginal and Torres Strait Islander Health Survey: biomedical results, 2012–13. Iodine. Sept 2014. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4727.0.55.003~2012-13~Main%20Features~Iodine~117 (viewed Sept 2018).
- 10. Mackerras DE, Singh GR, Eastman CJ. Iodine status of Aboriginal teenagers in the Darwin region before mandatory iodine fortification of bread. Med J Aust 2011; 194: 126–130. https://www.mja.com.au/journal/2011/194/3/iodine-status-aboriginal-teenagers-darwin-region-mandatory-iodine-fortification
- 11. Sayers SM, Powers JR. Birth size of Australian Aboriginal babies. Med J Aust 1993; 159: 586–591.
- 12. Davison B, Cunningham T, Singh G. Engaging adolescents and young adults in a longitudinal health study: experience from the Top End cohort. Aust N Z J Public Health. 2011; 35: 86–87.
- 13. Sayers S, Singh G, Mackerras D, et al. Australian Aboriginal Birth Cohort study: follow‐up processes at 20 years. BMC Int Health Hum Rights 2009; 9: 23.
- 14. Sayers SM, Mackerras D, Singh GR. Cohort profile: the Australian Aboriginal Birth Cohort (ABC) study. Int J Epidemiol 2017; 46: 1383–1383f.
- 15. Davison B, Nagel T, Singh G. Life, lifestyle and location: examining the complexities of psychological distress in young adult Indigenous and non‐Indigenous Australians. J Dev Orig Health Dis 2017; 8: 541–549.
- 16. Australian Institute of Health and Welfare. Monitoring the health impacts of mandatory folic acid and iodine fortification (Cat. No. PHE 208). Canberra: AIHW, 2016.
- 17. Zimmermann MB. Iodine deficiency. Endocr Rev 2009; 30: 376–408.
- 18. DePaoli KM, Seal JA, Burgess JR, Taylor R. Improved iodine status in Tasmanian schoolchildren after fortification of bread: a recipe for national success. Med J Aust 2013; 198: 492–494. https://www.mja.com.au/journal/2013/198/9/improved-iodine-status-tasmanian-schoolchildren-after-fortification-bread-recipe
- 19. National Health and Medical Research Council. Iodine supplementation for pregnant and breastfeeding women. NHMRC Public Statement [online], Jan 2010. Archived: https://web.archive.org/web/20180329041755/https://www.nhmrc.gov.au/guidelines-publications/new45 (viewed May 2018)
- 20. Australian Bureau of Statistics. 4727.0.55.003. Australian Aboriginal and Torres Strait Islander Health Survey: biomedical results, 2012–13. Explanatory notes. Sept 2014. http://www.abs.gov.au/AUSSTATS/abs@.nsf/Latestproducts/4727.0.55.003Explanatory%20Notes12012-13?opendocument&tabname=Notes&prodno=4727.0.55.003&issue=2012-13&num=&view (viewed May 2018).
- 21. Australian Bureau of Statistics. 4727.0.55.006. Australian Aboriginal and Torres Strait Islander Health Survey: updated results, 2012–13. June 2014. http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4727.0.55.006Explanatory%20Notes12012%E2%80%9313?OpenDocument (viewed May 2018).





Abstract
Objective: To assess the median urine iodine concentration (UIC) of young adults in the Top End of Northern Territory, before and after fortification of bread with iodised salt became mandatory.
Design, setting: Analysis of cross‐sectional data from two longitudinal studies, the Aboriginal Birth Cohort and the non‐Indigenous Top End Cohort, pre‐ (Indigenous participants: 2006–2007; non‐Indigenous participants: 2007–2009) and post‐fortification (2013–15).
Participants: Indigenous and non‐Indigenous Australian young adults (mean age: pre‐fortification, 17.9 years (standard deviation [SD], 1.20 years); post‐fortification, 24.9 years (SD, 1.34 years).
Main outcome measure: Median UIC (spot urine samples analysed by a reference laboratory), by Indigenous status, remoteness of residence, and sex.
Results: Among the 368 participants assessed both pre‐ and post‐fortification, the median UIC increased from 58 μg/L (interquartile range [IQR], 35–83 μg/L) pre‐fortification to 101 μg/L (IQR, 66–163 μg/L) post‐fortification (P < 0.001). Urban Indigenous (median IUC, 127 μg/L; IQR, 94–203 μg/L) and non‐Indigenous adults (117 μg/L; IQR, 65–160 μg/L) were both iodine‐replete post‐fortification. The median UIC of remote Indigenous residents increased from 53 μg/L (IQR, 28–75 μg/L) to 94 μg/L (IQR, 63–152 μg/L; p < 0.001); that is, still mildly iodine‐deficient. The pre‐fortification median UIC for 22 pregnant women was 48 μg/L (IQR, 36–67 μg/L), the post‐fortification median UIC for 24 pregnant women 93 μg/L (IQR, 62–171 μg/L); both values were considerably lower than the recommended minimum of 150 μg/L for pregnant women.
Conclusions: The median UIC of young NT adults increased following mandatory fortification of bread with iodised salt. The median UIC of pregnant Indigenous women in remote locations, however, remains low, and targeted interventions are needed to ensure healthy fetal development.