The known: Each year, more than 180 000 people are admitted to Australian hospitals with heart failure. It is not known whether treatment advances over the past two decades have improved in‐hospital survival for people living outside major cities.
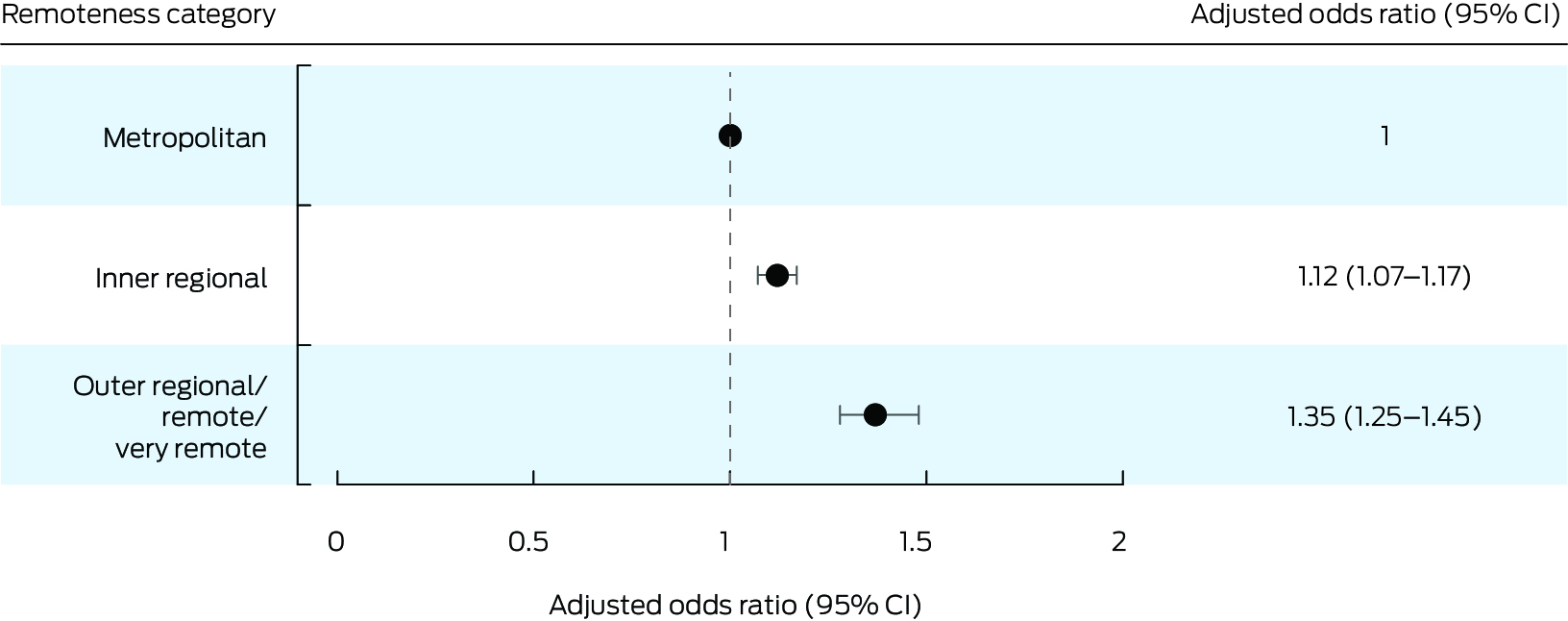
The new: During 2002–21, in‐hospital survival for people admitted with heart failure to New South Wales public hospitals improved, but the likelihood of dying in hospital was 12% higher for people from inner regional areas than for people from major cities, and 35% higher for people from outer regional or remote NSW.
The implications: Determining the reasons for these differences would enable targeted programs for improving outcomes for people in regional and remote Australia with heart failure.
Cardiovascular disease is the leading cause of death in Australia.1 Heart failure, second only to coronary artery disease as a cardiovascular cause of illness and death, is the main reason for 180 000 hospital admissions in Australia each year.1 The rates of hospitalisation with and death from heart failure increase with geographic remoteness,1,2 but the reasons for the differences, and changes over time, have not been investigated in detail.
Almost one‐third of people in Australia do not live in metropolitan areas,3 but only 2.4% of National Health and Medical Research Council funding is for research that specifically benefits people living in regional or remote Australia.4 Further, people living in regional and remote areas do not have adequate access to specialist cardiology care, which is very important for both inpatient and outpatient follow‐up care. Treatment of cardiovascular disease guided by a cardiologist is associated with lower risk of death from heart failure.5,6 People in regional Australia have less access to specialist heart failure care and are more likely to have general practitioners as their primary heart failure physicians than people in metropolitan areas,7,8,9 and their clinical outcomes are poorer.10,11,12 The management of heart failure has markedly improved over the past two decades, and updates are regularly published by Australian13 and overseas cardiology societies14,15 to guide physicians managing patients with heart failure.
Whether the geographic differences in outcomes for people with heart failure in Australia have changed with these improvements is unclear. We therefore examined associations between remoteness of region of residence and in‐hospital mortality for people admitted to hospital with heart failure in New South Wales during 2002–21.
Methods
Established in 2006, the Centre for Health Record Linkage (CheReL; https://www.cherel.org.au) maintains a large data linkage system for health‐related data for New South Wales residents; it includes hospitals administrative data since 31 July 2001. It includes the Admitted Patient Data Collection (APDC), which includes data for more than 97% of hospital admissions in NSW.16 For our retrospective observational cohort study, we identified all admissions with primary diagnoses of heart failure during 1 January 2002 – 30 September 2021, as described previously.17,18,19,20 De‐identified data for cases that met the inclusion criteria were provided to the research team by CheReL. We analysed data for NSW residents aged 16 years or older at the time of admission with heart failure to public hospitals. We excluded patients without documented area of residence; for people admitted more than once with heart failure during the study period, we included only the first admission. We excluded private hospital admissions to reduce geographic bias, as most private hospitals are in metropolitan areas. We report our study in concordance with the STROBE guidelines for reporting observational studies.21
Data sources and study outcome
For each heart failure admission, we extracted the admission date, region of residence (Statistical Area Level 2 [SA2] code), age, sex (male, female), hospital length of stay, and whether the person died in hospital (the primary outcome). The primary diagnosis and all background diagnoses were coded in the APDC according to the International Statistical Classification of Diseases, tenth revision, Australian modification (ICD‐10‐AM) (Supporting Information, table 1). The number of medical conditions other than heart failure was quantified using the Charlson comorbidity index (CCI). Socio‐economic status (Index of Relative Socioeconomic Advantage and Disadvantage, IRSAD22) was based on SA2 region of residence;23 a higher IRSAD score indicates lower disadvantage and greater advantage.
Statistical analysis
We stratified patients by region of residence (SA2) at the time of heart failure admission. We classified remoteness according to the Australian Statistical Geography Standard, a measure of relative access to services, with five categories;23 for this study, we defined three categories: metropolitan (= major cities; the reference group), inner regional, and outer regional/remote/very remote.
We summarise continuous variables as means with standard deviations (SDs) or medians with interquartile ranges (IQRs); the statistical significance of between‐group differences was assessed using one‐way analysis of variance (ANOVA; parametric variables) or Kruskal–Wallis tests (non‐parametric variables). We summarise categorical variables as numbers and proportions; the statistical significance of between‐group differences was assessed in χ2 tests. We examined associations of variables with in‐hospital mortality using binary logistic regression; the variables assessed were remoteness category, age (with respect to median), sex, IRSAD score (with respect to median), other diagnoses, hospital length of stay, and calendar year of admission (by 4‐year group, to reduce variability by year); we report odds ratios (ORs) with 95% confidence intervals (CIs). We performed a separate multivariable model that incorporated CCI to assess the impact of morbidity burden on in‐hospital mortality and to assess the robustness of our results. To reduce potential multicollinearity, tolerance was set at greater than 0.4 (ie, variance inflation factor of 2.5). Variables for which P < 0.05 were included in the multivariable analysis; we report adjusted ORs (aORs) with 95% CIs. All analyses were performed in SPSS 23 (IBM) and Prism 8 (GraphPad). P < 0.05 (two‐tailed) was deemed statistically significant.
Ethics approval
The NSW Population and Health Services Research Ethics Committee approved the study and waived the requirement for individual consent to use health information (2013/09/479). All patient‐related data were de‐identified and analysed anonymously. The study protocol conformed with the 2013 Declaration of Helsinki.
Results
Our analysis included 154 853 people admitted to hospital with heart failure during 1 January 2002 – 30 September 2021 (Supporting Information, figure 1); 99 687 lived in metropolitan areas (64.4%), 41 953 in inner regional areas (27.1%), and 13 213 in outer regional/remote/very remote areas (8.5%). The median age at admission was 80.3 years (IQR, 71.2–86.8 years), and 78 591 were men (50.8%); the proportion of men was larger for outer regional/remote/very remote areas (52.2%) than metropolitan areas (50.2%). The most frequent other cardiac conditions were atrial fibrillation or flutter (39 763 people, 25.7%) and ischaemic heart disease (31 949, 20.6%); the most frequent cardiovascular risk factors were diabetes (42 435 people, 27.4%) and hypertension (41 146, 26.6%). The median CCI score for people living in metropolitan areas was 1 (IQR, 0–2), for those in inner regional it was 1 (IQR, 0–2), and for those in outer regional/remote/very remote areas it was 0 (IQR, 0–1). The median IRSAD score was higher for people from metropolitan (1000; IQR, 940–1064) than those from inner regional (934; IQR, 924–981 and outer regional/remote/very remote areas (930; IQR, 905–936) (Box 1).
In‐hospital mortality and hospital length of stay
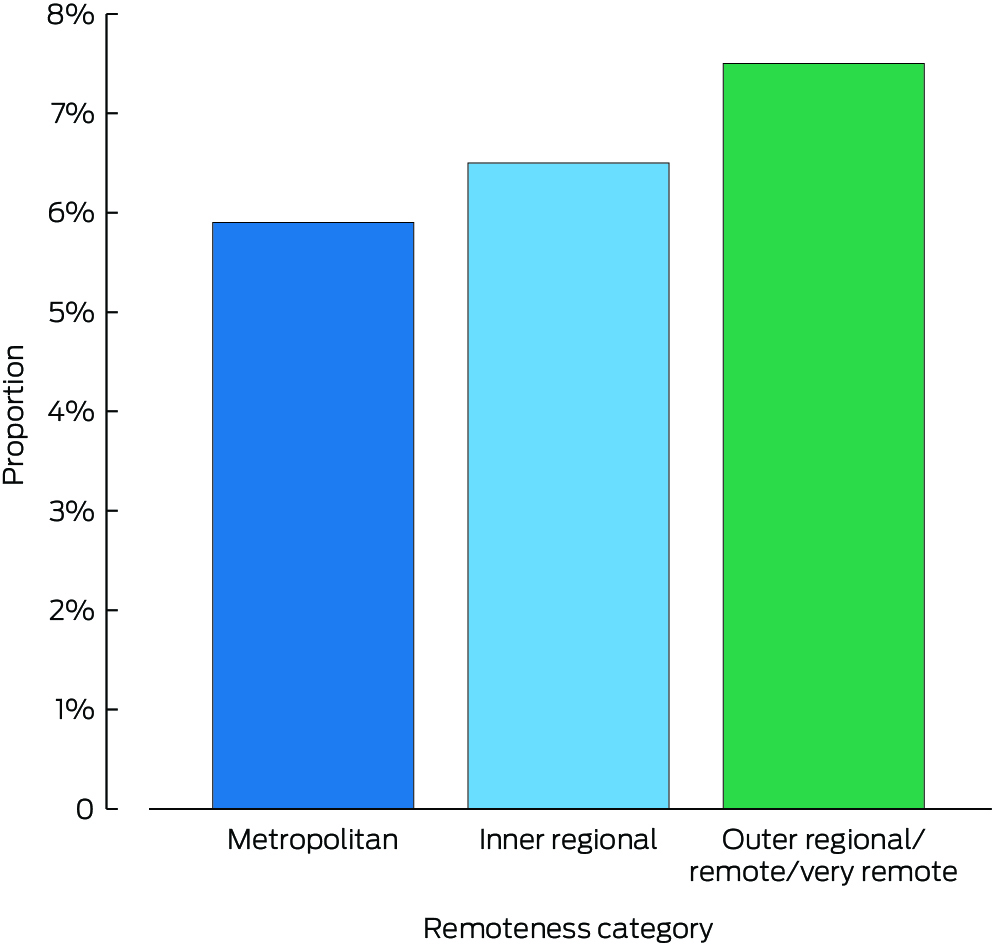
During 2002–21, 9621 people admitted to hospital with heart failure (6.2%) died during their admissions; the proportion was 8.0% in 2002, and 4.9% in 2021 (Supporting Information, figure 2). By remoteness category, 5887 patients from metropolitan areas (5.9%), 2740 from inner regional areas (6.5%), and 994 people from outer regional/remote/very remote areas (7.5%) died in hospital (Box 2). By sex, 5005 women (6.6%) and 4615 men (5.9%) had died in hospital; the proportion of women who died in hospital exceeded that of men in all three remoteness categories: metropolitan, 3006 women (6.1%) and 2880 men (5.8%); inner regional, 1449 women (7.1%) and 1291 men (6.0%); outer regional/remote/very remote, 550 women (8.7%) and 444 men (6.4%) (Supporting Information, figure 3). In the multivariable analysis, the association of sex with in‐hospital mortality was not statistically significant (aOR, 0.98, 95% CI, 0.94–1.02) (Box 3).
The median hospital length of stay was five days (IQR, 2–8 days); it was five days (IQR, 2–9 days) for patients from metropolitan areas, and four days (IQR, 2–8 days) for patients from both inner regional and outer regional/remote/very remote areas (Box 1).
Change in in‐hospital all‐cause mortality during admissions with heart failure
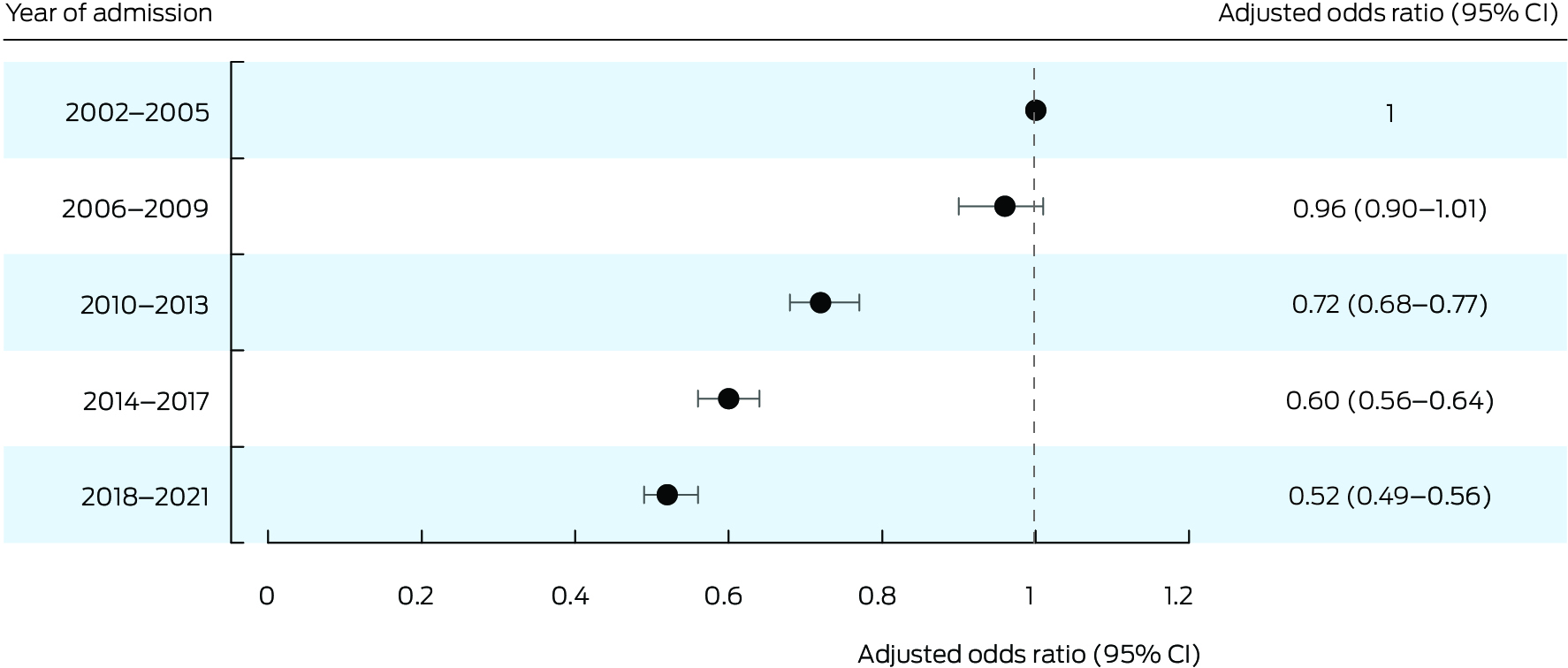
In‐hospital all‐cause mortality was lower during 2018–21 than during 2002–2005, both overall (aOR, 0.52; 95% CI, 0.49–0.56) (Box 3; Box 4) and for patients from metropolitan areas (aOR, 0.50; 95% CI, 0.46–0.55), inner regional areas (aOR, 0.53; 95% CI, 0.47–0.61), and outer regional/remote/very remote areas (aOR, 0.55; 95% CI, 0.44–0.69) (Supporting Information, figure 4).
Associations of patient factors with in‐hospital mortality
Compared with patients from metropolitan areas, the odds of in‐hospital death were higher for patients from inner regional (aOR, 1.12; 95% CI, 1.07–1.17) and outer regional/remote/very remote areas (aOR, 1.35; 95% CI, 1.25–1.45) (Box 5). Similar results were yielded by a multivariable model that additionally included CCI as a variable: inner regional: aOR, 1.15 (95% CI, 1.10–1.21); outer regional/remote/very remote areas: aOR, 1.37 (95% CI, 1.28–1.48) (Supporting Information, table 4). The odds of in‐hospital mortality were greater for people with a history of stroke (aOR, 3.47; 95% CI, 3.07–3.92) or malignancy (aOR, 3.06; 95% CI, 2.81–3.33) (Box 3).
Discussion
We found that all‐cause in‐hospital mortality among people admitted to NSW public hospitals with heart failure during 2002–21 declined significantly during the study period, but that it was higher among patients from regional or remote areas than people from metropolitan areas.
A 2018 meta‐analysis found few studies that had examined differences in outcomes of hospitalisations with heart failure for people from metropolitan and regional areas.24 We report the largest published study of in‐hospital mortality among people admitted to hospital with heart failure in Australia, and our 20‐year study period facilitated a comprehensive analysis of statewide changes in admissions and outcomes for a geographically diverse population.
We found that overall in‐hospital mortality for people hospitalised with heart failure during 2002–21 was 6.2%, but ranged from 5.9% for metropolitan area residents to 7.5% for people from outer regional/remote/very remote areas. The NSW Heart Failure Snapshot study, a four‐week audit of heart failure admissions to 24 participating NSW and Australian Capital Territory hospitals in mid‐2013, found that in‐hospital mortality was 6%;25 the authors did not state how many patients were from metropolitan and regional areas. A retrospective study found that in‐hospital mortality was 10.5% among people admitted with heart failure to hospitals in the Hunter New England Local Health District during 2005–2014, 40% of whom had been admitted to regional or remote hospitals.26 This earlier study was not statewide and was undertaken prior to recent therapeutic advances, but it was closer in design to our study than the NSW Heart Failure Snapshot study. Other Australian studies have examined 30‐day mortality for people from metropolitan and regional areas admitted to hospital with heart failure. In a 2014 Western Australian study, adjusted 30‐day mortality was higher among people from regional areas than those from metropolitan areas (OR, 1.16, 95% CI, 1.01–1.33);11 a 2022 Victorian study did not find any difference in 30‐day mortality, but fewer than 100 of the 1357 included patients were from regional areas.27
Our study was unique in that we assessed in detail temporal changes in in‐hospital mortality among people admitted with heart failure over twenty years. No other Australian study has examined statewide heart failure outcomes for such a long period. We found that all‐cause in‐hospital mortality was 48% lower for people admitted during 2018–21 than for those admitted during 2002–2005; the reduction was similar for people from metropolitan, inner regional, and outer regional/remote/very remote areas. Several factors are likely to have contributed to this change. Guideline‐directed medical therapies are important for minimising in‐hospital mortality among patients admitted with acute heart failure,28,29 and non‐pharmacological measures, such as appropriate heart failure care pathways, also improve survival.30 We had no information about in‐hospital therapy, but the reduction in in‐hospital mortality could be partially attributable to improved pharmacological and non‐pharmacological management of heart failure in both metropolitan and regional areas.
We found that the likelihood of dying in hospital was higher for patients with heart failure from non‐metropolitan areas: 12% higher for inner regional residents, and 35% higher for people in outer regional/remote/very remote areas after adjusting for baseline characteristics, year of admission, socio‐economic status, and other medical conditions. Clinical outcomes are likely to be more favourable for people with heart failure if they receive care from a cardiologist rather than a general physician or general practitioner.5,6 In the NSW Heart Failure Snapshot study, 8% of patients were in the care of heart failure physicians, 62% in the care of cardiologists, and 40% in the care of general physicians.25 A 2014 study found that general physicians or practitioners were more likely to provide inpatient heart failure care for people from regional areas than those from metropolitan Western Australia,11 and similar results were found by a study in Victoria.27 We did not have information about whether patients received specialist cardiology care at the 242 admitting hospitals in our study; 81 934 admissions (52.9%) were to twenty tertiary or quaternary hospitals and 15 017 (9.7%) to seventeen metropolitan district hospitals; 27 899 people (18.0%) were admitted to fifteen large regional hospitals and 30 003 (19.4%) to smaller district‐level or lower tier hospitals in outer regional/remote/very remote areas, which presumably did not have access to the cardiology services available in larger centres. More comprehensive information about admitting physicians at each institution would be needed to assess the influence of care type on outcomes for patients with heart failure from outside metropolitan areas.
As an analysis of population‐level data for the most populous Australian state, our findings provide a useful benchmark for in‐hospital mortality during admissions with heart failure. It could support assessment of the impact of inpatient heart failure care programs in regional Australia. Linking patient‐level admission and discharge medications information, outpatient follow‐up via Medicare Benefits Schedule billing codes, and individual echocardiographic data would facilitate a more comprehensive investigation of why in‐hospital mortality is higher for people from regional and remote areas with heart failure than for metropolitan patients.
Limitations
The findings of our retrospective analysis of observational data can be used to generate hypotheses and could assist prospective studies of heart failure outcomes for people living in regional and remote areas. We did not apply a look‐back strategy to identify lifetime index heart failure admissions. It is likely that our reference group of people admitted during 2002–2005 included patients who had previously been admitted to hospital with heart failure; people with recurrent heart failure admissions are at greater risk of in‐hospital death. The continuous decline in‐hospital mortality during the study period suggests that this factor is unlikely to fully explain the improvement in survival at the end of the study period. The APDC does not include information about ejection fraction, medical therapy, haemodynamic profile, or blood pathology findings for individual patients.
Indigenous people have poorer heart failure outcomes than non‐Indigenous Australians,24,31 and a larger proportion live in regional and remote areas.3 In‐hospital heart failure mortality among Australia Indigenous patients have not been published. The larger proportion of Indigenous patients in regional and remote areas may have influenced our findings, but the APDC does not include information about ethnic background.
The findings of our analysis of statewide data for the most populous Australian state should be generalisable to the entire country, but analysis of national data would be preferable. We limited our study to only people admitted with heart failure to public hospitals, excluding 13% of all heart failure admissions during the study period. Finally, we examined only in‐hospital death as an outcome for people admitted with heart failure, not the full spectrum of heart failure presentations, nor outcomes after leaving hospital.
Conclusion
In‐hospital mortality is higher among people living in inner regional and outer regional/remote/very remote areas of NSW admitted to public hospitals with heart failure than for people living in metropolitan areas. Detailed patient‐level information is needed to identify the reasons for this difference, enabling targeted programs for improving outcomes for people with heart failure in regional and remote Australia.
Box 1 – Characteristics of people aged 16 years or older admitted with heart failure to New South Wales public hospitals, 1 January 2002 – 30 September 2021, by remoteness of residence*
|
Parameters |
All patients |
Metropolitan |
Inner regional |
Outer regional/remote/very remote |
|||||||||||
|
|
|||||||||||||||
|
Number of patients |
154 853 |
99 687 (64.4%) |
41 953 (27.1%) |
13 213 (8.5%) |
|||||||||||
|
Age (years), median (IQR) |
80.3 (71.2–86.8) |
80.6 (71.4–87.0) |
80.0 (71.2–86.5) |
79.0 (70.0–86.1) |
|||||||||||
|
Sex (men) |
78 591 (50.8%) |
50 034 (50.2%) |
21 664 (51.6%) |
6893 (52.2%) |
|||||||||||
|
IRSAD score, median (IQR) |
973 (926–1032) |
1000 (940–1064) |
934 (924–981) |
930 (905–936) |
|||||||||||
|
Other medical conditions |
|
|
|
|
|||||||||||
|
Atrial fibrillation/flutter |
39 763 (25.7%) |
27 280 (27.4%) |
9944 (23.7%) |
2539 (19.2%) |
|||||||||||
|
Ischaemic heart disease |
31 949 (20.6%) |
21 368 (21.4%) |
8381 (20.0%) |
2200 (16.7%) |
|||||||||||
|
Prior percutaneous coronary interventions/coronary artery bypass graft |
10 921 (7.1%) |
7468 (7.5%) |
2718 (6.5%) |
735 (5.6%) |
|||||||||||
|
Peripheral vascular disease |
6880 (4.4%) |
4779 (4.8%) |
1707 (4.1%) |
394 (3.0%) |
|||||||||||
|
Prior valve replacement |
2414 (1.6%) |
1588 (1.6%) |
657 (1.6%) |
169 (1.3%) |
|||||||||||
|
Stroke |
1030 (0.7%) |
673 (0.7%) |
278 (0.7%) |
79 (0.6%) |
|||||||||||
|
Chronic pulmonary disease |
21 769 (14.1%) |
13 368 (13.4%) |
6318 (15.1%) |
2083 (15.8%) |
|||||||||||
|
Chronic kidney disease |
17 480 (11.3%) |
11 999 (12.0%) |
4390 (10.5%) |
1091 (8.3%) |
|||||||||||
|
Neurodegenerative disease† |
7310 (4.7%) |
4950 (5.0%) |
1857 (4.4%) |
503 (3.8%) |
|||||||||||
|
Malignancy |
3301 (2.1%) |
2113 (2.1%) |
943 (2.2%) |
245 (1.9%) |
|||||||||||
|
Cardiac risk factors |
|
|
|
|
|||||||||||
|
Diabetes |
42 435 (27.4%) |
29 013 (29.1%) |
10 279 (24.5%) |
3143 (23.8%) |
|||||||||||
|
Hypertension |
41 146 (26.6%) |
28 783 (28.9%) |
9561 (22.8%) |
2802 (21.2%) |
|||||||||||
|
Hyperlipidaemia |
8412 (5.4%) |
6837 (6.9%) |
1259 (3.0%) |
316 (2.4%) |
|||||||||||
|
Charlson comorbidity index,‡ median (IQR) |
1.0 (0–2) |
1.0 (0–2) |
1.0 (0–2) |
0.0 (0–1) |
|||||||||||
|
Hospital length of stay (days),§ median (IQR) |
5.0 (2–8) |
5 (2–9) |
4 (2–8) |
4 (2–8) |
|||||||||||
|
Year group |
|
|
|
|
|||||||||||
|
2002–2005 |
31 124 |
19 820 (63.7%) |
8329 (26.8%) |
2975 (9.6%) |
|||||||||||
|
2006–2009 |
28 345 |
17 970 (63.4%) |
7814 (27.6%) |
2561 (9.0%) |
|||||||||||
|
2010–2013 |
30 665 |
19 859 (64.8%) |
8205 (26.8%) |
2601 (8.5%) |
|||||||||||
|
2014–2017 |
33 028 |
21 513 (65.1%) |
8923 (27.0%) |
2592 (7.8%) |
|||||||||||
|
2018–2021 |
31 691 |
20 525 (64.8%) |
8682 (27.4%) |
2484 (7.8%) |
|||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range; IRSAD = Index of Relative Social Advantage and Disadvantage; SD = standard deviation. * First admissions during the study period only. † Includes dementia, central nervous systemic atrophies, Parkinson disease, basal ganglia degeneration, nervous systemic degenerative diseases. ‡ Includes myocardial infarction, heart failure, peripheral vascular disease, stroke, dementia, chronic pulmonary disease, connective tissue disease, peptic ulcer disease, liver disease (mild or moderate to severe), diabetes (with or without organ damage), hemiplegia, moderate to severe renal disease, any tumour (within past five years), lymphoma, leukaemia, metastatic solid tumour, acquired immunodeficiency syndrome. § Length of stay by 4‐year admission period is reported in the Supporting Information, table 3. |
|||||||||||||||
Box 2 – Proportions of people aged 16 years or older who died during admissions to New South Wales public hospitals, 1 January 2002 – 30 September 2021, by remoteness of residence
Box 3 – In‐hospital mortality during admissions with heart failure of people aged 16 years or older to New South Wales public hospitals, 1 January 2002 – 30 September 2021: logistic regression analysis
|
Parameter |
Deaths |
Missing cases |
Univariable odds ratio (95% CI) |
Multivariable odds ratio (95% CI) |
|||||||||||
|
|
|||||||||||||||
|
Remoteness category |
|
|
|
|
|||||||||||
|
Metropolitan |
5887 (5.9%) |
0 |
1 |
1 |
|||||||||||
|
Inner regional |
2740 (6.5%) |
0 |
1.11 (1.06–1.17) |
1.12 (1.07–1.17) |
|||||||||||
|
Outer regional/remote/very remote |
994 (7.5%) |
0 |
1.30 (1.21–1.39) |
1.35 (1.25–1.45) |
|||||||||||
|
Age (years)* |
|
|
|
|
|||||||||||
|
Older than 80.3 years old |
6672 (8.6%) |
0 |
2.32 (2.28–2.49) |
2.21 (2.11–2.31) |
|||||||||||
|
80.3 years or younger |
2949 (3.8%) |
0 |
1 |
1 |
|||||||||||
|
Sex |
|
|
|
|
|||||||||||
|
Men |
4615 (5.9%) |
0 |
0.89 (0.85–0.93) |
0.98 (0.94–1.02) |
|||||||||||
|
Women |
5005 (6.6%) |
0 |
1 |
1 |
|||||||||||
|
IRSAD score* |
|
|
|
|
|||||||||||
|
More than 973 |
4690 (6.1%) |
0 |
0.96 (0.81–0.99) |
0.96 (0.91–1.00) |
|||||||||||
|
973 or less |
4931 (6.4%) |
25 |
1 |
1 |
|||||||||||
|
Ischaemic heart disease |
|
|
|
|
|||||||||||
|
Yes |
3131 (9.8%) |
0 |
1.95 (1.86–2.04) |
1.90 (1.81–1.98) |
|||||||||||
|
No |
6490 (5.3%) |
0 |
1 |
1 |
|||||||||||
|
Prior percutaneous coronary interventions/coronary artery bypass graft |
|
|
|
|
|||||||||||
|
Yes |
514 (4.7%) |
0 |
0.73 (0.67–0.80) |
0.60 (0.54–0.65) |
|||||||||||
|
No |
9107 (6.3%) |
0 |
1 |
1 |
|||||||||||
|
Stroke |
|
|
|
|
|||||||||||
|
Yes |
265 (25.7%) |
0 |
5.35 (4.64–6.16) |
3.47 (3.07–3.92) |
|||||||||||
|
No |
9356 (6.1%) |
0 |
1 |
1 |
|||||||||||
|
Peripheral vascular disease |
|
|
|
|
|||||||||||
|
Yes |
666 (9.7%) |
0 |
1.66 (1.53–1.81) |
1.53 (1.41–1.66) |
|||||||||||
|
No |
8955 (6.1%) |
0 |
1 |
1 |
|||||||||||
|
Atrial fibrillation/flutter |
|
|
|
|
|||||||||||
|
Yes |
2800 (7.0%) |
0 |
1.20 (1.15–1.26) |
1.05 (1.01–1.10) |
|||||||||||
|
No |
6821 (5.9%) |
0 |
1 |
1 |
|||||||||||
|
Prior valve replacement |
|
|
|
|
|||||||||||
|
Yes |
148 (6.1%) |
0 |
0.99 (0.83–1.17) |
— |
|||||||||||
|
No |
9473 (6.2%) |
0 |
1 |
— |
|||||||||||
|
Chronic pulmonary disease |
|
|
|
|
|||||||||||
|
Yes |
1839 (8.4%) |
0 |
1.49 (1.41–1.57) |
1.44 (1.37–1.52) |
|||||||||||
|
No |
7782 (5.8%) |
0 |
1 |
1 |
|||||||||||
|
Chronic kidney disease |
|
|
|
|
|||||||||||
|
Yes |
1637 (9.4%) |
0 |
1.68 (1.58–1.77) |
1.97 (1.86–2.08) |
|||||||||||
|
No |
7894 (5.8%) |
0 |
1 |
1 |
|||||||||||
|
Malignancy |
|
|
|
|
|||||||||||
|
Yes |
581 (17.6%) |
0 |
3.37 (3.07–3.69) |
3.06 (2.81–3.33) |
|||||||||||
|
No |
9040 (6.0%) |
0 |
1 |
1 |
|||||||||||
|
Neurodegenerative disease† |
|
|
|
|
|||||||||||
|
Yes |
1051 (14.4%) |
0 |
2.73 (2.54–2.92) |
1.85 (1.73–1.97) |
|||||||||||
|
No |
8570 (5.8%) |
0 |
1 |
1 |
|||||||||||
|
Hypertension |
|
|
|
|
|||||||||||
|
Yes |
2506 (6.1%) |
0 |
0.97 (0.93–1.02) |
— |
|||||||||||
|
No |
7115 (6.3%) |
0 |
1 |
— |
|||||||||||
|
Hyperlipidaemia |
|
|
|
|
|||||||||||
|
Yes |
412 (4.9%) |
0 |
0.77 (0.69–0.85) |
0.66 (0.60–0.73) |
|||||||||||
|
No |
9209 (6.3%) |
0 |
1 |
1 |
|||||||||||
|
Diabetes |
|
|
|
|
|||||||||||
|
Yes |
2223 (5.2%) |
0 |
0.79 (0.75–0.82) |
0.85 (0.81–0.89) |
|||||||||||
|
No |
7398 (6.6%) |
0 |
1 |
1 |
|||||||||||
|
Hospital length of stay, per day |
9621 (6.2%) |
0 |
1.01 (1.01–1.01) |
1.00 (1.00–1.00) |
|||||||||||
|
Year groups |
|
|
|
|
|||||||||||
|
2002–2005 |
2584 (8.3%) |
0 |
1 |
1 |
|||||||||||
|
2006–2009 |
2209 (7.8%) |
0 |
0.93 (0.88–0.99) |
0.96 (0.90–1.01) |
|||||||||||
|
2010–2013 |
1852 (6.0%) |
0 |
0.71 (0.67–0.76) |
0.72 (0.68–0.77) |
|||||||||||
|
2014–2017 |
1631 (4.9%) |
0 |
0.57 (0.54–0.61) |
0.60 (0.56–0.64) |
|||||||||||
|
2018–2021 |
1345 (4.2%) |
0 |
0.49 (0.46–0.52) |
0.52 (0.49–0.56) |
|||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; IRSAD = Index of Relative Social Advantage and Disadvantage. * Categories based on median values for all patients. † Includes dementia, central nervous systemic atrophies, Parkinson disease, basal ganglia degeneration, nervous systemic degenerative diseases. |
|||||||||||||||
Received 6 February 2024, accepted 18 October 2024
- Imants Rubenis1
- Gregory Harvey1
- Karice Hyun2
- Vincent Chow1
- Leonard Kritharides1,2,3
- Andrew P Sindone1,2
- David B Brieger1,2
- Austin CC Ng1,2
- 1 Concord Repatriation General Hospital, Sydney, NSW
- 2 The University of Sydney, Sydney, NSW
- 3 ANZAC Research Institute, Sydney, NSW
Correspondence: imants.rubenis@sydney.edu.au
Open access:
Open access publishing facilitated by the University of Sydney, as part of the Wiley – the University of Sydney agreement via the Council of Australian University Librarians.
Data Sharing:
The NSW Population and Health Services Research Ethics Committee (PHSREC) prohibits authors from making the minimal data set publicly available. Interested researchers may contact the ethics coordinator (
No relevant disclosures.
- 1. Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts (cat. no. CVD 92). Updated 12 Dec 2024. https://www.aihw.gov.au/reports/heart‐stroke‐vascular‐diseases/hsvd‐facts/contents/about (viewed Dec 2024).
- 2. Australian Commission on Safety and Quality in Health Care. Heart failure. In: The fourth Australian atlas of healthcare variation. Sydney: Australian Commission on Safety and Quality in Health Care, 2021; pp. 87‐108. https://www.safetyandquality.gov.au/publications‐and‐resources/resource‐library/fourth‐atlas‐2021‐22‐heart‐failure (viewed Dec 2023).
- 3. Baxter J, Gray M, Hayes A; Australian Institute of Family Studies. Families in regional, rural and remote Australia. Mar 2011. https://aifs.gov.au/research/research‐reports/families‐regional‐rural‐and‐remote‐australia (viewed Dec 2023).
- 4. Barclay L, Phillips A, Lyle D. Rural and remote health research: does the investment match the need? Aust J Rural Health 2018; 26: 74‐79.
- 5. Jong P, Gong Y, Liu PP, et al. Care and outcomes of patients newly hospitalized for heart failure in the community treated by cardiologists compared with other specialists. Circulation 2003; 15: 184‐191.
- 6. Masters J, Morton G, Anton I, et al. Specialist intervention is associated with improved patient outcomes in patients with decompensated heart failure: evaluation of the impact of a multidisciplinary inpatient heart failure team. Open Heart 2017; 8: e000547.
- 7. Taylor CJ, Valenti L, Britt H, et al. Management of chronic heart failure in general practice in Australia. Aust Fam Physician 2016; 45: 734‐739.
- 8. Audehm RG, Neville AM, Piazza P, et al. Healthcare services use by patients with heart failure in Australia: findings from the SHAPE study. Aust J Gen Prac 2022; 51: 713‐720.
- 9. Clark RA, Driscoll A, Nottage J, et al. Inequitable provision of optimal services for patients with chronic heart failure: a national geo‐mapping study. Med J Aust 2007; 186: 169‐173. https://www.mja.com.au/journal/2007/186/4/inequitable‐provision‐optimal‐services‐patients‐chronic‐heart‐failure‐national
- 10. Sahle BW, Owen AJ, Mutowo MP, et al. Prevalence of heart failure in Australia: a systematic review. BMC Cardiovasc Disord 2016; 16: 32.
- 11. Teng THK, Katzenellenbogen JM, Hung J, et al. Rural–urban differentials in 30‐day and 1‐year mortality following first‐ever heart failure hospitalisation in Western Australia: a population‐based study using data linkage. BMJ Open 2014; 4: e004724.
- 12. Al‐Omary MS, Davies AJ, Khan AA, et al. Heart failure hospitalisations in the Hunter New England area over 10 years. A changing trend. Heart Lung Circ 2017; 26: 627‐630.
- 13. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2022; 79: e263‐e421.
- 14. McDonagh TA, Metra M, Adamo M, et al; ESC Scientific Document Group. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021; 42: 3599‐3726.
- 15. NHFA CSANZ Heart Failure Guidelines Working Group; Atherton JJ, Sindone A, Pasquale CGD, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Guidelines for the prevention, detection, and management of heart failure in Australia 2018. Heart Lung Circ 2018; 27: 1123‐1208.
- 16. Centre for Health Record Linkage. NSW Admitted Patient Data Collection: legacy data dictionary for data to 30 June 2023. Apr 2024. https://www.cherel.org.au/media/38875/nsw‐apdc‐data‐dictionary‐april‐2024.pdf (viewed Jan 2024).
- 17. Brieger DB, Ng ACC, Chow V, et al. Falling hospital and postdischarge mortality following CABG in New South Wales from 2000 to 2013. Open Heart 2019; 6: e000959.
- 18. Cheng YY, Chow V, Brieger D, et al. Outcomes of 16 436 patients requiring isolated aortic valve surgery: a statewide cohort study. Int J Cardiol 2021; 326: 55‐61.
- 19. Hoskin S, Brieger D, Chow V, et al. Trends in acute pulmonary embolism admission rates and mortality outcomes in Australia, 2002–2003 to 2017–2018: a retrospective cohort study. Thromb Haemost 2021; 121: 1237‐1245.
- 20. Vijayarajan V, Kritharides L, Brieger D, et al. Sex differences in rates of permanent pacemaker implantation and in‐hospital complications: a statewide cohort study of over 7 million persons from 2009–2018. PLoS One 2022; 17: e0272305.
- 21. Von Elm E Altman D, Egger M, et al; STROBE initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453‐1457.
- 22. Australian Bureau of Statistics. Index of Relative Socio‐economic Advantage and Disadvantage (IRSAD). In: Socio‐Economic Indexes for Areas (SEIFA); 2021. 27 Apr 2023. https://www.abs.gov.au/statistics/people/people‐and‐communities/socio‐economic‐indexes‐areas‐seifa‐australia/latest‐release#index‐of‐relative‐socio‐economic‐advantage‐and‐disadvantage‐irsad‐ (viewed Dec 2023).
- 23. Australian Bureau of Statistics. Statistical Area Level 2. Australian Statistical Geography Standard (ASGS) edition 3, July 2021 – June 2026. 20 July 2021. https://www.abs.gov.au/statistics/standards/australian‐statistical‐geography‐standard‐asgs‐edition‐3/jul2021‐jun2026/main‐structure‐and‐greater‐capital‐city‐statistical‐areas/statistical‐area‐level‐2 (viewed Dec 2023).
- 24. Al‐Omary MS, Davies AJ, Evans TJ, et al. Mortality and readmission following hospitalisation for heart failure in Australia: a systematic review and meta‐analysis. Heart Lung Circ 2018; 27: 917‐927.
- 25. Newton PJ, Davidson PM, Reid CM, et al. Acute heart failure admissions in New South Wales and the Australian Capital Territory: the NSW HF Snapshot Study. Med J 2016; 204: 113. https://www.mja.com.au/journal/2016/204/3/acute‐heart‐failure‐admissions‐new‐south‐wales‐and‐australian‐capital‐territory
- 26. Al‐Omary MS, Khan AA, Davies AJ, et al. Outcomes following heart failure hospitalization in a regional Australian setting between 2005 and 2014. ESC Heart Fail 2018; 5: 271‐278.
- 27. Chan RK, Dinh DT, Hare DL, et al; VCOR‐HF Investigators. Management of acute decompensated heart failure in rural versus metropolitan settings: an Australian experience. Heart Lung Circ 2022; 31: 491‐498.
- 28. Tamaki Y, Yaku H, Morimoto T, et al; KCHF Study Investigators. Lower in‐hospital mortality with beta‐blocker use at admission in patients with acute decompensated heart failure. J Am Heart Assoc 2021; 10: e020012.
- 29. Koh HB, Quah WJ, Tey S, et al. Predictors of in‐hospital mortality due to heart failure hospitalisation and trends of guideline‐directed medical therapy usage [abstract: European Society of Cardiology congress, Barcelona, 26–29 August 2022]. Eur Heart J 2022; 43 (Suppl 2): ehac544.1074.
- 30. Panella M, Marchisio S, Demarchi ML, et al. Reduced in‐hospital mortality for heart failure with clinical pathways: the results of a cluster randomised controlled trial. Qual Saf Health Care 2009; 18: 369‐373.
- 31. Teng THK, Katzenellenbogen JM, Thompson SC, et al. Incidence of first heart failure hospitalisation and mortality in Aboriginal and non‐Aboriginal patients in Western Australia, 2000–2009. Int J Cardiol 2014; 173: 110‐117.






Abstract
Objective: To examine associations between remoteness of region of residence and in‐hospital mortality for people admitted to hospital with heart failure in New South Wales during 2002–21.
Study design: Retrospective observational cohort study; analysis of New South Wales Admitted Patient Data Collection data.
Setting, participants: Adult (16 years or older) NSW residents admitted with heart failure to NSW public hospitals, 1 January 2002 – 30 September 2021. Only first admissions with heart failure during the study period were included.
Main outcome measures: In‐hospital mortality, by remoteness of residence (Australian Statistical Geography Standard), adjusted for age (with respect to median), sex, socio‐economic status (Index of Relative Socioeconomic Advantage and Disadvantage [IRSAD], with respect to median), other diagnoses, hospital length of stay, and calendar year of admission (by 4‐year group).
Results: We included 154 853 admissions with heart failure; 99 687 people lived in metropolitan areas (64.4%), 41 953 in inner regional areas (27.1%), and 13 213 in outer regional/remote/very remote areas (8.5%). The median age at admission was 80.3 years (interquartile range [IQR], 71.2–86.8 years), and 78 591 patients were men (50.8%). The median IRSAD score was highest for people from metropolitan areas (metropolitan: 1000; IQR, 940–1064; inner regional: 934; IQR, 924–981; outer regional/remote/very remote areas: 930; IQR, 905–936). During 2002–21, 9621 people (6.2%) died in hospital; the proportion was 8.0% in 2002, 4.9% in 2021. In‐hospital all‐cause mortality was lower during 2018–21 than during 2002–2005 (adjusted odds ratio [aOR], 0.52; 95% confidence interval [CI], 0.49–0.56); the decline was similar for all three remoteness categories. Compared with people from metropolitan areas, the odds of in‐hospital death during 2002–21 were higher for people from inner regional (aOR, 1.12; 95% CI, 1.07–1.17) or outer regional/remote/very remote areas (aOR, 1.35; 95% CI, 1.25–1.45).
Conclusion: In‐hospital mortality during heart failure admissions to public hospitals declined across NSW during 2002–21. However, it was higher among people living in regional and remote areas than for people from metropolitan areas. The reasons for the difference in in‐hospital mortality should be investigated.