Clinical record
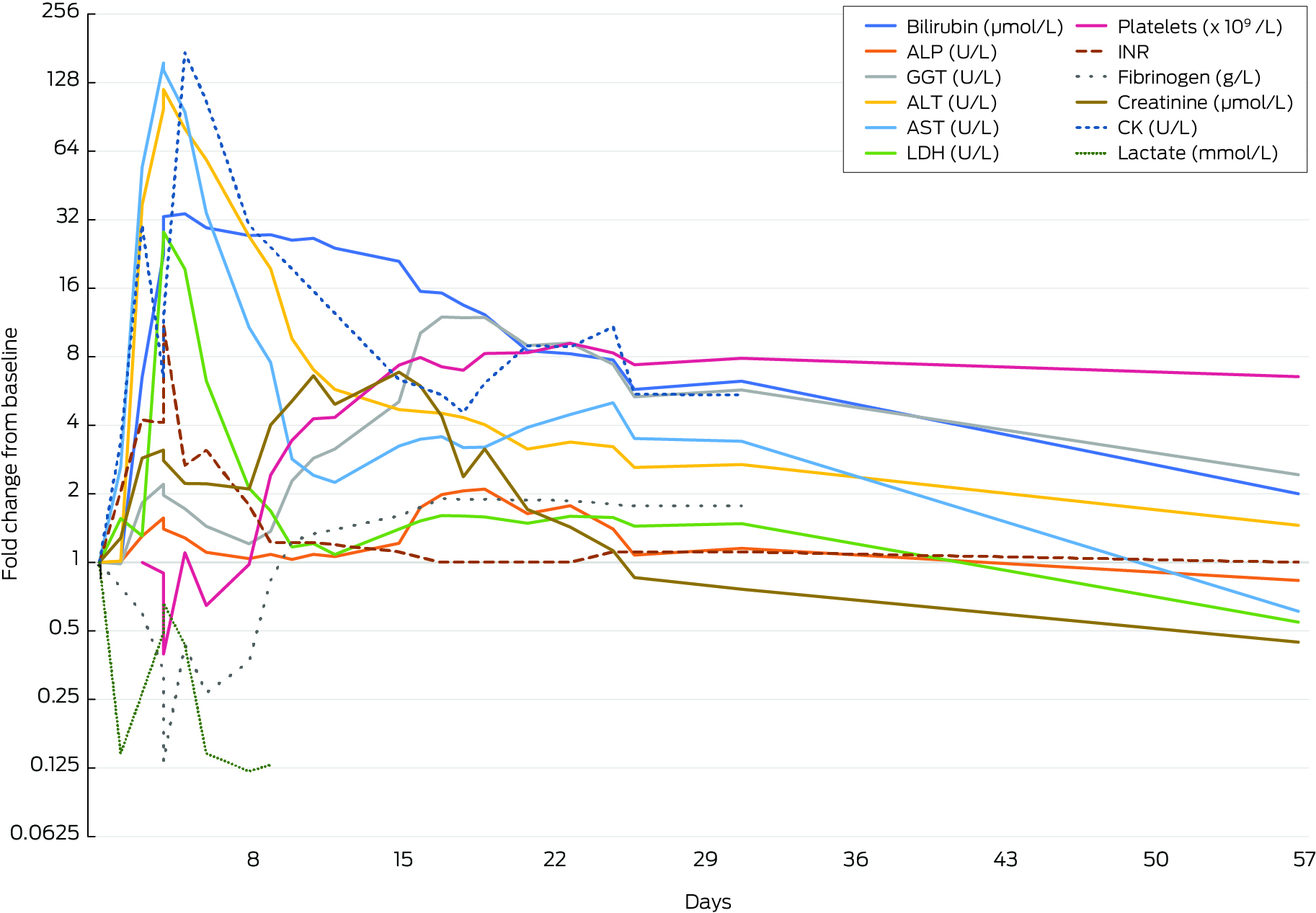
A 26‐year‐old man with central obesity (body mass index, 32.7 kg/m2) and a history of drinking up to 22 standard drinks over weekends, collapsed 5 minutes following a 5 km run in hot and humid conditions in Brisbane, Australia. He was not on any regular medications or supplements and had been running 3 km, four times weekly, for the previous four months. He presented to a tertiary hospital with a Glasgow Coma Score of 10, hyperthermia (40.6°C), acute kidney injury and rhabdomyolysis. After resuscitation, cooling and intubation, he was transferred to the Intensive Care Unit (ICU) and treated with noradrenaline to maintain mean arterial pressure over 65 mmHg and broad‐spectrum antibiotics. The patient was extubated on Day 2 with a stable Glasgow Coma Score of 14. From Day 3, his creatinine level rose to 482 μmol/L (reference interval [RI], 60–110 μmol/L), requiring renal replacement therapy and his liver function markedly worsened (see Box 1 and Box 2). Common causes of acute hepatitis (viral, autoimmune, drug‐induced) were excluded with laboratory testing and further history.
On Day 4, he developed disseminated intravascular coagulation marked by an international normalised ratio exceeding 10 (RI, 0.9–1.2), clottable fibrinogen below 0.04 g/L (RI, 2.0–4.5 g/L), D‐dimer level over 128 mg/L (RI, 0.02–0.48 mg/L) and platelet count of 19 × 109/L (RI, 140–400 × 109/L). His lactate dehydrogenase level peaked on Day 4 at 11 914 U/L (RI, 120–250 U/L). He had evidence of asterixis with a venous ammonia level of 110 μmol/L (RI, < 50 μmol/L) and altered cognition consistent with acute liver failure (ALF). Treatment included N‐acetyl cysteine infusion, rifaximin and lactulose. His coagulation profile was supported with cryoprecipitate, fresh frozen plasma and three‐factor (II, IX and X) prothrombin complex concentrate (Prothrombinex‐VF, CSL Behring). His creatinine kinase concentration peaked on Day 5 at 74 100 U/L (RI, 46–171 U/L). He was transferred to the ICU at the local liver transplant centre on Day 5.
With supportive care, he avoided transplantation and his liver function steadily improved (encephalopathy resolved on Day 6, international normalised ratio stabilised on Day 9). He was discharged from the ICU on Day 8 but his cholestatic enzymes began to rise reaching a peak alkaline phosphatase concentration of 277 U/L (RI, < 110 U/L) and γ‐glutamyltransferase concentration of 810 U/L (RI, < 55 U/L) on Day 19. A magnetic resonance cholangiopancreatogram showed a diffuse reduction in intrahepatic bile duct calibre. Cholestasis improved with ursodeoxycholic acid and his bilirubin level normalised by Day 57. Dialysis had ceased on Day 20. At the four‐month follow‐up, he remained fatigued but otherwise well. His metabolic screen was negative.
Discussion
In Australia from 2006 to 2019, extreme heat caused 252 deaths, with an additional 170 deaths contributed to by extreme heat.1 Heatstroke is a life‐threatening condition associated with an uncontrolled rise in core body temperature above 40°C. This occurs due to the failure of the body's compensatory mechanisms required to maintain thermal homeostasis. Classic heatstroke results from passive exposure to high temperatures and humidity, often during heatwaves and primarily affects the older population. Exertional heatstroke (EHS) tends to affect younger, healthier individuals during vigorous exercise. The prevalence of EHS is unknown and often underestimated.2
The pathophysiology of heatstroke is complex, resulting most commonly in brain dysfunction; however, in severe cases, patients may develop disseminated intravascular coagulation, circulatory shock, pulmonary oedema and acute kidney injury.3 Muscle breakdown in rhabdomyolysis causes elevated concentrations of transaminases, potentially obscuring the early signs of underlying liver injury. ALF is a rare but life‐threatening complication of EHS, resulting from severe hyperthermia‐induced direct liver injury, ischaemia, systemic inflammatory response, coagulopathy and multiorgan dysfunction. Management of EHS involves rapid implementation of cooling protocols and supportive care, including stabilising vital signs, maintaining adequate hydration and providing respiratory and circulatory support. The management of EHS complications involves organ support similar to that used in trauma or sepsis with liver transplantation used in cases of fulminant liver failure.4
The literature on EHS‐induced ALF and its treatment is primarily based on heterogenous case reports, making it challenging to predict which patients will not survive with supportive management alone. Although liver transplantation is a preferred treatment option in selected cases, some patients who meet the transplant criteria, such as the patient discussed herein, also recover spontaneously.5,6 The use of King's College criteria to identify severe cases with poor prognosis without liver transplantation is limited due to unique pathophysiology of EHS‐induced ALF. Liver transplantation alone does not address other organ failures, emphasising the importance of ongoing ICU care and raising considerations about the timing of transplantation decisions.7 With climate change potentially leading to a rise in such incidents,8 it is imperative to address heatstroke‐induced liver failure from both medical and public health perspectives.
From a medical standpoint, the focus should be in improving the understanding of this condition, prompt recognition of cases, prioritisation of comprehensive patient care in ICU and development of enhanced risk stratification tools to ensure favourable patient outcomes.
Lessons from practice
- Heatstroke is a life‐threatening condition that occurs when the body temperature rises above 40°C due to failed thermal regulation.
- Heatstroke can lead to extreme and life‐threatening complications, such as acute liver failure, which requires comprehensive management, including liver transplant in severe cases.
- The King's College criteria for severe cases may not apply to heatstroke‐induced acute liver failure due to multiorgan involvement, highlighting the need for better risk stratification.
- Climate change may increase the incidence of these cases, necessitating a better understanding of the condition, prompt management and improved public health strategies.
Box 1 – Laboratory findings and timeline
|
|
Bilirubin (μmol/L) |
ALP (U/L) |
GGT (U/L) |
ALT (U/L) |
AST (U/L) |
LDH (U/L) |
Platelets (x109/L) |
INR |
Fibrinogen (g/L) |
Creatinine (μmol/L) |
CK (U/L) |
Lactate (mmol/L) |
|||
|
|
|||||||||||||||
|
Reference interval |
< 20 |
30–110 |
< 55 |
< 45 |
< 35 |
120–250 |
140–400 |
0.9–1.2 |
2.0–4.5 |
60–110 |
46–171 |
0.5–2.2 |
|||
|
Day |
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
1 |
4 |
132 |
68 |
77 |
82 |
421 |
|
0.9 |
3.0 |
168 |
426 |
12.4 |
|||
|
2 |
4 |
133 |
67 |
78 |
216 |
656 |
|
|
|
215 |
1450 |
1.8 |
|||
|
3 |
26 |
172 |
124 |
2860 |
4450 |
550 |
48 |
3.8 |
1.8 |
482 |
12 900 |
3.3 |
|||
|
4 (am) |
90 |
207 |
150 |
7550 |
12 800 |
11 015 |
43 |
3.7 |
1.0 |
523 |
2750 |
6.1 |
|||
|
4 (pm) |
132 |
185 |
134 |
9200 |
11 900 |
11 914 |
19 |
> 10 |
< 0.4 |
470 |
5110 |
8.2 |
|||
|
5 |
136 |
169 |
117 |
6170 |
7800 |
8174 |
53 |
2.4 |
1.3 |
373 |
74 100 |
5.4 |
|||
|
6 |
118 |
146 |
98 |
4520 |
2810 |
2641 |
31 |
2.8 |
0.8 |
372 |
45 200 |
1.8 |
|||
|
8 |
109 |
137 |
82 |
2080 |
883 |
891 |
47 |
1.6 |
1.1 |
353 |
12 900 |
1.5 |
|||
|
9 |
110 |
143 |
93 |
1500 |
620 |
708 |
116 |
1.1 |
2.5 |
674 |
|
1.6 |
|||
|
10 |
104 |
136 |
155 |
739 |
233 |
492 |
165 |
1.1 |
3.7 |
858 |
|
|
|||
|
11 |
106 |
143 |
195 |
541 |
198 |
509 |
205 |
1.1 |
4.0 |
1110 |
|
|
|||
|
12 |
96 |
140 |
214 |
443 |
184 |
456 |
208 |
|
|
830 |
|
|
|||
|
15 |
84 |
160 |
345 |
361 |
266 |
589 |
353 |
1.0 |
4.8 |
1150 |
2710 |
|
|||
|
16 |
62 |
230 |
690 |
354 |
285 |
640 |
381 |
|
|
1000 |
|
|
|||
|
17 |
61 |
262 |
813 |
348 |
292 |
676 |
347 |
0.9 |
5.7 |
736 |
2320 |
|
|||
|
18 |
54 |
272 |
807 |
333 |
262 |
673 |
335 |
|
|
399 |
1940 |
|
|||
|
19 |
49 |
277 |
810 |
310 |
263 |
666 |
397 |
|
|
529 |
2610 |
|
|||
|
21 |
34 |
216 |
609 |
242 |
321 |
625 |
400 |
|
|
287 |
3820 |
|
|||
|
23 |
33 |
234 |
625 |
260 |
366 |
671 |
440 |
0.9 |
5.6 |
240 |
3760 |
|
|||
|
25 |
31 |
185 |
504 |
248 |
412 |
663 |
399 |
1 |
5.4 |
189 |
4610 |
|
|||
|
26 |
23 |
142 |
363 |
201 |
287 |
607 |
354 |
1 |
5.3 |
144 |
2330 |
|
|||
|
31 |
25 |
152 |
389 |
207 |
279 |
623 |
378 |
1 |
5.3 |
128 |
2320 |
|
|||
|
57 |
8 |
110 |
165 |
112 |
50 |
230 |
314 |
0.9 |
|
75 |
|
|
|||
|
|
|||||||||||||||
|
ALP = alkaline phosphatase; ALT = alanine aminotransferase; AST = aspartate aminotransferase; CK = creatine kinase; GGT = γ‐glutamyltransferase; INR = international normalised ratio; LDH = lactate dehydrogenase. |
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
- 1. Peden AE, Heslop D, Franklin RC. Weather‐related fatalities in Australia between 2006 and 2019: applying an equity lens. Sustainability 2023; 15: 813.
- 2. Garcia CK, Renteria LI, Leite‐Santos G, et al. Exertional heat stroke: pathophysiology and risk factors. BMJ Med 2022; 1: e000239.
- 3. Bouchama A, Abuyassin B, Lehe C, et al. Classic and exertional heatstroke. Nat Rev Dis Primers 2022; 8: 8.
- 4. Bi X, Deising A, Frenette C. Acute liver failure from exertional heatstroke can result in excellent long‐term survival with liver transplantation. Hepatology 2020; 71: 1122‐1123.
- 5. Figiel W, Morawski M, Grąt M, et al. Fulminant liver failure following a marathon: five case reports and review of literature. World J Clin Cases 2019; 7: 1467‐1474.
- 6. Davis BC, Tillman H, Chung RT, et al. Heat stroke leading to acute liver injury and failure: a case series from the Acute Liver Failure Study Group. Liver Int 2017; 37: 509‐513.
- 7. Berger J, Hart J, Millis M, Baker AL. Fulminant hepatic failure from heat stroke requiring liver transplantation. J Clin Gastroenterol 2000; 30: 429‐431.
- 8. Ebi KL, Capon A, Berry P, et al. Hot weather and heat extremes: health risks. Lancet 2021; 398: 698‐708.





Patient consent:
The patient provided written consent for publication.
No relevant disclosures.