The known: The prevalence of heavy menstrual bleeding among women of reproductive age in Australia, and its change across the reproductive lifespan, are uncertain.
The new: Serial surveys of a cohort of Australian women found that at age 22 years 17.6% reported heavy bleeding during the preceding twelve months, rising to 39.3% of women aged 48 years who menstruated. Higher body mass index, iron deficiency, and endometriosis were associated with heavy bleeding. Health‐related quality of life was poorer for women who experienced heavy menstrual bleeding.
The implications: Given the burden of the condition, it is important that Australian women are aware of and have access to effective care for heavy menstrual bleeding.
The impact of heavy menstrual bleeding on the physical and mental wellbeing of women is increasingly recognised.1,2 The estimated prevalence ranges between 4% and 52%,3 the broad variation in estimates explained by differences in the methods and instruments used to assess heavy bleeding, the cultural and social context of the studies, whether women not currently menstruating were excluded, and the ages of the study participants.3
Until the early 2000s, heavy menstrual bleeding was defined as menstrual blood loss exceeding 80mL per cycle;4 however, this criterion did not reflect individual perceptions of “heavy” bleeding.1 Most countries have now moved to a more person‐centred approach, as outlined in the National Institute for Health and Care Excellence (NICE) guidelines5 and adopted by the Australian Commission on Safety and Quality in Health Care Clinical Standards,6 in which heavy menstrual bleeding is based on self‐report and defined as “excessive menstrual blood loss which interferes with a woman's physical, social, emotional and/or material quality of life. It can occur alone or in combination with other symptoms.”5 This change in definition also reorients treatment options from minimising blood loss to improving quality of life.5
In Australia, little is known about the prevalence of heavy menstrual bleeding across the reproductive lifespan, nor about the characteristics of women who experience this condition. The Australian Longitudinal Study on Women's Health (ALSWH) could investigate these questions, as participants have been asked to report their experiences of heavy periods in nine surveys across more than two decades, allowing us to track heavy menstrual bleeding in a cohort of women born during 1973–1978 from young adulthood to midlife.
The objectives of our study were to estimate the prevalence of self‐reported heavy menstrual bleeding from young adulthood to midlife in Australia, to investigate the characteristics of women who experience this condition, and to investigate the relationship of heavy menstrual bleeding with health‐related quality of life.
Methods
The ALSWH is a longitudinal population‐based study that recruited three cohorts of women in 1996: women born during 1973–1978, 1946–1951, or 1921–1926. Women invited to participate had been randomly selected from people identified as “female” in the Medicare database; women living in rural and remote areas were sampled at twice the rate of women in urban areas to facilitate statistical comparisons.7
For the study we report in this article, we analysed survey and linked administrative health records data for women in the 1973–1978 ALSWH cohort, followed up approximately every three years; participants completed surveys 2 to 9 during 2000–2021, and were aged 43–48 years at the most recent survey (survey 9). We analysed data for women who consented to linkage of their survey responses with data on health service use (Pharmaceutical Benefits Scheme [PBS] and Medicare Benefits Schedule [MBS] databases).
The Australian Longitudinal Study on Women's Health data recruited participants who were identified as female in the Medicare database in 1996. In this article, “woman” is defined as any person with a uterus, including transgender and binary people who do not identify as women.
Data collection
At each survey, participants were asked: “In the last 12 months have you had heavy periods?”; the response options were “never”, “rarely”, “sometimes”, “often”. The women were not provided with any guidance about the levels of severity or frequency corresponding to these response options. As our focus was women who reported frequent heavy menstrual bleeding, for this study we grouped the responses as never/rarely, sometimes, and often.
We extracted data on age, remoteness of residence,8 highest educational attainment, labour force participation, smoking status, and level of physical activity. We also collected data on body mass index (BMI; derived from self‐reported height and weight), depressive symptoms (Center for Epidemiological Studies Depression Scale [CESD‐10]; score of 10 or more indicates significant level of depressive symptoms),9 and self‐reported diagnoses of hypertension (other than during pregnancy), low iron levels, endometriosis, and polycystic ovary syndrome (PCOS).
The reproduction‐related characteristics we included were the number of times the woman had given birth, and the use of progestogen implants or levonorgestrel‐releasing intrauterine devices (IUDs) as ascertained in linked PBS and MBS data. The recorded date of supply was used as a proxy for the date the implant or IUD was inserted; we assumed that implant use was for three years (1.5 years in a post hoc sensitivity analysis), IUD use for five years (3.3 years in a sensitivity analysis, based on mean duration of use10). We also included as a dichotomous variable the self‐reported use of other hormonal contraceptives at each survey (oral contraceptives, combined or progestogen‐containing only; injection [eg, Depo‐Provera]; vaginal ring [eg, Nuvaring]). Whether women had had a hysterectomy or bilateral oophorectomy or had experienced menopause was also asked in each survey (further details: Supporting Information, part 1).
In each survey, health‐related quality of life was assessed with the Medical Outcomes Study 36‐item short form health survey (SF‐36),11 which comprises eight domains (physical functioning, role‐limiting physical problems, bodily pain, general health, vitality, social functioning, role‐limiting emotional problems, mental health) and two component summary scores (physical health, mental health). Scores for each of the domains and the two summary scores range from 0 to 100, with higher scores indicating better health‐related quality of life.
Statistical analysis
We estimated the prevalence of heavy menstrual bleeding from responses to surveys 2 to 9. As in earlier ALSWH studies, we omitted survey 1 data from this analysis because several symptoms were reported more frequently than in subsequent surveys, possibly indicating a telescoping effect; that is, when women were first asked to report symptoms, they may have underestimated how recently they occurred.12
We estimated the prevalence of heavy menstrual bleeding by year of age, using the three frequency categories, for all survey respondents. We then estimated the prevalence after excluding women who had hysterectomies or bilateral oophorectomies or who had completed menopause (ie, were no longer at risk of heavy menstrual bleeding). All prevalence estimates were weighted by residential remoteness category to adjust for the oversampling of women from rural and remote areas at the time of ALSWH recruitment.
We assessed associations of socio‐demographic, behavioural, health, and reproduction‐related characteristics with heavy menstrual bleeding for respondents to at least one of surveys 3 (2003) to 9 (2021); we did not include survey 2 in this analysis because questions on labour force participation were first included in survey 3. We summarise the characteristics of participants at survey 3 (analysis baseline) by heavy menstrual bleeding frequency category as numbers and proportions weighted by residential remoteness category. Given the three categories of the heavy bleeding outcome, and that the outcome was not rare, we assessed associations between each characteristic and sometimes or often experiencing heavy bleeding using log‐multinomial regression,13 weighted by residential remoteness category, using the cluster option to account for repeated measures; we report risk ratios (RRs) with 95% confidence intervals (CIs). This was a time‐varying analysis, as the exposure and outcome category for individuals could differ at each survey. Women no longer at risk of heavy bleeding (women who reported hysterectomy or bilateral oophorectomy, or had experienced menopause) were excluded from this analysis at subsequent survey time points.
Finally, we assessed the differences between heavy menstrual bleeding frequency categories in the mean SF‐36 domain and summary component scores for surveys 2 to 9, excluding women who had reported hysterectomy, bilateral oophorectomy, or menopause, using analysis of variance (ANOVA). As differences between the three heavy menstrual bleeding frequency categories in mean scores were all statistically significant at each survey, and the magnitude of these differences did not markedly differ between surveys, we report results (means with 95% CIs) only for survey 9 (when participants were aged 43–48 years).
Descriptive and ANOVA analyses were undertaken in SAS 9.4 TS1M, log‐multinomial regression analyses in Stata/SE 14.2 for Windows.
Ethics approval
The ALSWH survey program has ongoing ethics approval from the human research ethics committees of the University of Newcastle (H‐076‐0795) and the University of Queensland (2004/HE000224). The ALSWH also has institutional human research ethics committee approval for external record linkage (University of Newcastle, H‐2011‐0371; University of Queensland, 2012/HE000132). Access to MBS and PBS data collections was approved by the Australian Institute of Health and Welfare human research ethics committee (EC00103), protocol EO2020/3/1115).
Results
Prevalence of heavy menstrual bleeding and hormonal contraception use (ALSWH surveys 2–9)
Of the 14 247 women in the ALSWH 1973–1978 cohort, we excluded 746 women (5.2%) who did not consent to data linkage, 2178 (15.3%) who responded only to the initial survey, and twelve women (0.1%) who did not respond to questions about heavy menstrual bleeding in surveys 2 to 9. Data for 11 311 participants were included in the prevalence analysis (Supporting Information, figure 1).
The proportion of participants who reported often experiencing heavy menstrual bleeding increased from 6.1% (45 of 691 participants) at 22 years of age to 12.1% (136 of 1132 participants) at 48 years; the proportion who reported sometimes experiencing heavy menstrual bleeding increased from 11.5% (79 participants) to 20.0% (223 participants) (Box 1). By the age of 48 years, 112 women (8.6%) had had hysterectomies or bilateral oophorectomies, and 107 (9.6%) had experienced menopause; after excluding these women, 14.8% of 48‐year‐old women (136 of 913 participants) reported experiencing heavy bleeding often and 24.5% (223 of 913 participants) sometimes (Supporting Information, figure 2).
The proportion of women who used levonorgestrel‐releasing IUDs increased from 0.3% in 2000 (24 of 9124 women aged 22–27 years) to 19.4% in 2021 (1271 of 6547 women aged 43–48 years); the proportions who reported using progestogen implants was 3–4% at each survey, and the proportion using other hormonal contraception declined from 55.6% (5069 women) to 9.5% (621 women) (Supporting Information, table 2).
Characteristics associated with heavy menstrual bleeding (ALSWH surveys 3–9)
After excluding 699 participants who did not respond to surveys after survey 2, and 1213 women for whom covariate information was missing, we included 9399 participants in the analysis of factors associated with heavy menstrual bleeding (Supporting Information, figure 1). The likelihood of often experiencing heavy menstrual bleeding increased with BMI (40 kg/m2 or greater v 18.5–24.9 kg/m2: RR, 2.27; 95% CI, 1.93–2.67), and was greater for respondents who reported low iron levels (RR, 2.26; 95% CI, 2.03–2.51) or endometriosis (RR, 2.29; 95% CI, 2.06–2.54). It was also greater for women who did not have university degrees, formerly or currently smoked, reported no or low levels of physical activity, had given birth two or more times, had depressive symptoms, or reported diagnoses of hypertension or PCOS than for respondents in the respective comparator groups. The likelihood of often experiencing heavy menstrual bleeding was not significantly influenced by IUD use, either when assuming duration of use to be five years (RR, 0.93; 95% CI 0.83–1.04) or 3.3 years (RR, 1.05; 95% CI, 0.93–1.18); it was lower for women who used progestogen implants (three years: RR, 0.58; 95% CI, 0.46–0.73; 1.5 years: RR, 0.59; 95% CI, 0.44–0.80) or other hormonal contraceptives (RR, 0.36; 95% CI, 0.33–0.41). Associations for the likelihood of reporting heavy menstrual bleeding sometimes were similar (Box 2).
Mean health‐related quality of life scores for women who reported heavy menstrual bleeding were lower in all domains and for the summary mental health and physical health scores at survey 9 (age 43–48 years) than for women who reported never or rarely experiencing the condition. Further, mean quality of life scores were lower for women who often experienced heavy menstrual bleeding than for women who sometimes experienced heavy bleeding (Box 3). The differences in mean scores by frequency category were similar across surveys 3 to 9 (data not shown).
Discussion
A considerable proportion of our cohort of Australian women born during 1973–1978 reported experiencing heavy menstrual bleeding often or sometimes during the preceding twelve months; the overall proportion increased from 17.6% at age 22 years to 32.1% at 48 years. After excluding the 18.2% of women aged 48 years no longer at risk of heavy menstrual bleeding because they had had hysterectomies or bilateral oophorectomies or had experienced menopause, 39.3% of participants aged 48 years reported heavy menstrual bleeding. At each survey, experiencing heavy menstrual bleeding was associated with lower mean levels of both physical and mental health‐related quality of life.
Our estimates of the prevalence of heavy menstrual bleeding are broadly consistent with those of other studies, including cross‐sectional surveys of 1575 Australian women aged 20–39 years (28% perceived their periods to be heavy or very heavy),2 4610 Scottish women aged 25–44 years (35%),14 and 865 Brazilian women aged 18–45 years (35%).15 Our findings also confirm the increasing prevalence of heavy menstrual bleeding as women move into the late pre‐menopause–menopause transition.16,17 Increasing prevalence with age and differences between studies in the frequency of use of treatments such as long‐acting reversible contraception and hysterectomy need to be considered when comparing estimates of prevalence in different studies.
Women who reported endometriosis, PCOS, or depressive symptoms were more likely to report that they often experienced heavy menstrual bleeding. While other studies have found that women with endometriosis are more likely to experience the condition,18,19 the only study to assess the association of PCOS with heavy bleeding (a cross‐sectional study of 940 women in China) did not find one.19 The direction of effect between depressive symptoms and heavy menstrual bleeding is unclear. A recent study found genetic correlations of depression and many reproductive disorders, including heavy menstrual bleeding, suggesting a shared biological pathway.20 Similar to other studies, we also found that women who had lower education levels,15 currently smoked,16 were less physically active,21 had higher BMI values,16 or reported hypertension12 were more likely to report heavy menstrual bleeding, while low iron levels are a consequence of this condition.22 Other studies have also found associations between increasing number of births and heavy menstrual bleeding.14,23 Pregnancy and birth may cause anatomic changes and disruption to the endometrial lining that contribute to changes in menstrual bleeding.23
Our findings that mean health‐related quality of life scores in all physical and mental health‐related domains were lower for women who reported heavy menstrual bleeding are consistent with the findings of a systematic review that included eight studies (total of 1465 women) in which health‐related quality of life was assessed with the SF‐36 prior to any treatment for heavy bleeding.1 As women in our study who reported heavy periods during the preceding twelve months may also have been treated for the condition (eg, levonorgestrel‐releasing IUDs or surgical treatments) before completing the SF‐36, we probably underestimated associations between untreated heavy menstrual bleeding and health‐related quality of life.
Limitations
Our study included a large community‐based sample of women, and our analysis was longitudinal in nature, based on responses to questions about heavy periods and time‐dependent covariates repeated at each survey. However, while we surveyed participants’ opinion on the quantity and frequency of their menstrual blood loss, we did not ask whether women considered heavy menstrual bleeding to be a problem, reducing the alignment of our definition with the NICE guideline definition. In the 2005 Scottish survey, 43% of women who reported heavy periods described them as marked or severe problems.14 The ALSWH survey question about heavy menstrual bleeding has not been validated for assessing this condition. Despite the recent shift to patient‐reported outcome measures for assessing heavy menstrual bleeding, no patient‐reported outcome is considered the gold standard for defining this condition.24 Further, most covariate data in our study were derived from survey responses, which are subject to recall bias, resulting in some misclassification of participants, including with respect to menopause status; women who experienced amenorrhea for twelve or more months for reasons other than menopause (eg, lactational amenorrhoea) could have been misclassified as having experienced menopause.
Our analyses took reported diagnoses of endometriosis and PCOS into account, but not other conditions that could contribute to heavy menstrual bleeding, such as uterine fibroids and adenomyosis. Although we undertook sensitivity analyses with respect to the duration of IUD and implant use, the uncertainty of our assumptions may have biased our findings for these variables. Further, we relied on survey responses to ascertain the use of other hormonal contraceptives, as many contraceptive prescriptions are not recorded in the PBS databank.25 Differences between surveys in the wording of questions prevented our separately assessing the influence of combined oral contraceptives, progestogen injections, and vaginal rings. Individuals’ knowledge about and their perceptions of heavy menstrual bleeding may have changed over time, together with their likelihood of reporting it. Finally, the proportions of women in our study who had university educations or were born in Australia were larger than for all Australian women, which may limit the generalisability of our findings.7
Conclusions
Heavy menstrual bleeding was reported in our survey study by large minorities of women of reproductive age, and the proportion increased with age. Many women experience symptoms that have a substantial impact on their physical and mental health‐related quality of life. Despite the availability of effective treatments for heavy menstrual bleeding, which also improve health‐related quality of life,26 many women continue to live with symptoms. All women should be made aware of the range of treatments available, and provided access to care that is effective, empathetic, and reflects their values and preferences.
Box 1 – Proportions of Australian Longitudinal Study on Women's Health survey respondents who reported frequency of heavy menstrual bleeding during the preceding twelve months (never or rarely, sometimes, or often), hysterectomies or bilateral oophorectomies, or menopause, by age at survey
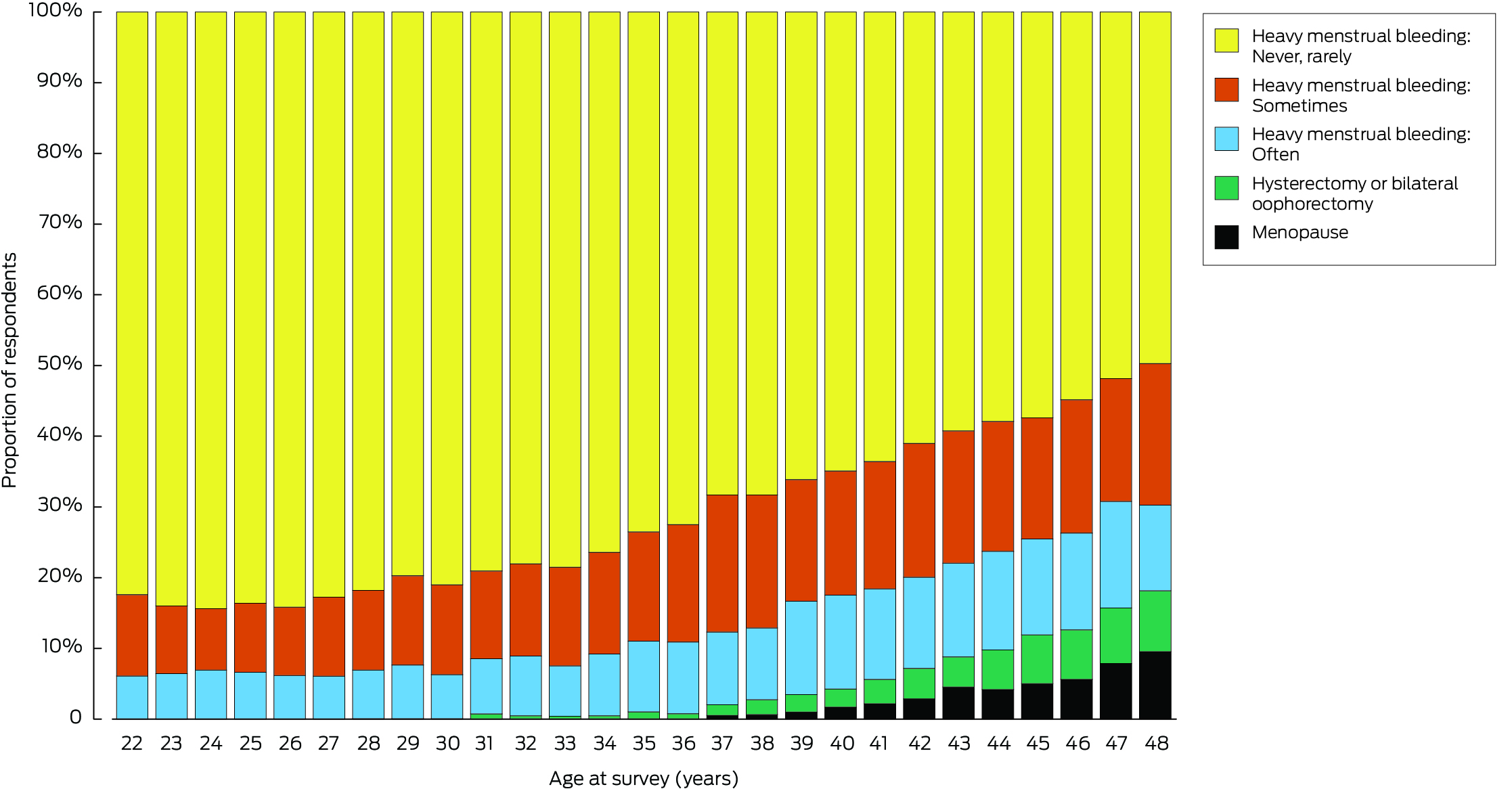
* The raw numbers underlying this graph are reported in the Supporting Information, table 1.
Box 2 – Socio‐demographic, behaviour, health, and reproduction‐related characteristics for 9399 respondents to at least one of Australian Longitudinal Study on Women's Health surveys 3 (2003) to survey 9 (2021) and frequency of heavy menstrual bleeding during the preceding twelve months: log‐multinomial regression analysis*
|
|
|
Heavy menstrual bleeding: risk ratio (95% CI)† |
|||||||||||||
|
Characteristic |
Number in category (survey 3)† |
Sometimes |
Often |
||||||||||||
|
|
|||||||||||||||
|
Respondents to survey 3 |
5784 |
|
|
||||||||||||
|
Age (years), mean (standard deviation) |
27.1 (1.5) |
— |
— |
||||||||||||
|
Age, per year at survey |
— |
1.03 (1.03–1.03) |
1.05 (1.04–1.05) |
||||||||||||
|
Residential remoteness8 |
|
|
|
||||||||||||
|
Major cities |
3319 (69.1%) |
1 |
1 |
||||||||||||
|
Inner regional |
1485 (18.1%) |
1.02 (0.95–1.09) |
1.07 (0.97–1.18) |
||||||||||||
|
Outer regional/rural/remote |
980 (12.8%) |
0.91 (0.83–0.99) |
0.97 (0.85–1.10) |
||||||||||||
|
Educational qualification (highest) |
|
|
|
||||||||||||
|
Degree or higher |
2746 (52.3%) |
1 |
1 |
||||||||||||
|
Trade/diploma |
1459 (24.2%) |
1.18 (1.10–1.26) |
1.29 (1.17–1.42) |
||||||||||||
|
High school or less |
1579 (23.5%) |
1.09 (1.01–1.18) |
1.28 (1.14–1.43) |
||||||||||||
|
Labour force status |
|
|
|
||||||||||||
|
Employed |
4852 (85.2%) |
1 |
1 |
||||||||||||
|
Unemployed |
241 (3.6%) |
1.13 (0.99–1.28) |
1.34 (1.15–1.57) |
||||||||||||
|
Not in labour force‡ |
691 (11.2%) |
0.85 (0.78–0.93) |
0.86 (0.76–0.96) |
||||||||||||
|
Smoking status |
|
|
|
||||||||||||
|
Never smoked |
3409 (59.7%) |
1 |
1 |
||||||||||||
|
Formerly smoked |
1024 (17.5%) |
1.13 (1.05–1.20) |
1.28 (1.17–1.41) |
||||||||||||
|
Currently smokes |
1351 (22.8%) |
1.17 (1.08–1.27) |
1.22 (1.09–1.38) |
||||||||||||
|
Physical activity level (METmin/week) |
|
|
|
||||||||||||
|
High (1000 or more) |
2116 (36.8%) |
1 |
1 |
||||||||||||
|
Moderate (500–999) |
1415 (24.8%) |
1.09 (1.02–1.17) |
1.04 (0.95–1.14) |
||||||||||||
|
Low (33.3–499) |
1832 (31.4%) |
1.04 (0.97–1.11) |
1.16 (1.06–1.27) |
||||||||||||
|
None/sedentary (less than 33.3) |
421 (7.0%) |
1.12 (1.03–1.122) |
1.45 (1.30–1.62) |
||||||||||||
|
Body mass index (kg/m2) |
|
|
|
||||||||||||
|
Below 18.5 |
245 (4.5%) |
1.09 (0.91–1.31) |
1.14 (0.88–1.48) |
||||||||||||
|
18.5–24.9 |
3354 (59.7%) |
1 |
1 |
||||||||||||
|
25.0–29.9 |
1318 (21.7%) |
1.13 (1.06–1.21) |
1.27 (1.15–1.40) |
||||||||||||
|
30.0–34.9 |
549 (9.0%) |
1.32 (1.22–1.43) |
1.67 (1.49–1.87) |
||||||||||||
|
35.0–39.9 |
201 (3.3%) |
1.38 (1.25–1.54) |
1.94 (1.69–2.22) |
||||||||||||
|
40 or higher |
117 (1.7%) |
1.52 (1.36–1.71) |
2.27 (1.93–2.67) |
||||||||||||
|
Self‐reported hypertension |
|
|
|
||||||||||||
|
No |
5658 (97.9%) |
1 |
1 |
||||||||||||
|
Yes |
126 (2.1%) |
1.20 (1.06–1.35) |
1.62 (1.39–1.88) |
||||||||||||
|
Self‐reported low iron (deficiency or anaemia) |
|
|
|
||||||||||||
|
No |
4900 (84.7%) |
1 |
1 |
||||||||||||
|
Yes |
884 (15.3%) |
1.24 (1.13–1.35) |
2.26 (2.03–2.51) |
||||||||||||
|
Depressive symptoms9 |
|
|
|
||||||||||||
|
No (CESD‐10 score 10 or less) |
4288 (74.5%) |
1 |
1 |
||||||||||||
|
Yes (CESD‐10 score greater than 10) |
1496 (25.5%) |
1.31 (1.24–1.39) |
1.81 (1.68–1.95) |
||||||||||||
|
Number of births |
|
|
|
||||||||||||
|
None |
4116 (74.5%) |
1 |
1 |
||||||||||||
|
One |
791 (12.8%) |
1.09 (1.00–1.19) |
1.09 (0.96–1.24) |
||||||||||||
|
Two |
641 (9.4%) |
1.21 (1.13–1.30) |
1.41 (1.27–1.57) |
||||||||||||
|
Three or more |
236 (3.3%) |
1.30 (1.20–1.40) |
1.87 (1.66–2.09) |
||||||||||||
|
Self‐reported endometriosis |
|
|
|
||||||||||||
|
No |
5441 (94.3%) |
1 |
1 |
||||||||||||
|
Yes |
343 (5.7%) |
1.23 (1.12–1.34) |
2.29 (2.06–2.54) |
||||||||||||
|
Self‐reported polycystic ovary syndrome |
|
|
|
||||||||||||
|
No |
5473 (94.3%) |
1 |
1 |
||||||||||||
|
Yes |
311 (5.7%) |
1.25 (1.14–1.37) |
1.90 (1.69–2.15) |
||||||||||||
|
Uses levonorgestrel‐releasing intrauterine device (5 years) |
|
|
|
||||||||||||
|
No |
5768 (99.8%) |
1 |
1 |
||||||||||||
|
Yes |
16 (0.2%) |
0.59 (0.53–0.65) |
0.93 (0.83–1.04) |
||||||||||||
|
Uses levonorgestrel‐releasing intrauterine device (3.3 years)† |
|
|
|
||||||||||||
|
No |
5770 (99.8%) |
1 |
1 |
||||||||||||
|
Yes |
15 (0.2%) |
0.60 (0.53–0.67) |
1.05 (0.93–1.18) |
||||||||||||
|
Uses progestogen implant (3 years) |
|
|
|
||||||||||||
|
No |
5625 (97.5%) |
1 |
1 |
||||||||||||
|
Yes |
159 (2.5%) |
0.82 (0.70–0.97) |
0.58 (0.46–0.73) |
||||||||||||
|
Uses progestogen implant (1.5 years)§ |
|
|
|
||||||||||||
|
No |
5627 (97.5%) |
1 |
1 |
||||||||||||
|
Yes |
157 (2.5%) |
0.77 (0.62–0.95) |
0.59 (0.44–0.80) |
||||||||||||
|
Uses other hormonal contraception¶ |
|
|
|
||||||||||||
|
No |
2793 (48.4%) |
1 |
1 |
||||||||||||
|
Yes |
2991 (51.6%) |
0.60 (0.56–0.64) |
0.36 (0.33–0.41) |
||||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; CESD‐10 = Center for Epidemiological Studies Depression Scale – 10‐item;9 METmin = metabolic minutes. * Women who reported a hysterectomy or bilateral oophorectomy, or had experienced menopause were excluded from the analysis at subsequent survey time points. † Proportions and risk ratios weighted for residential remoteness to adjust for oversampling in rural and remote areas. ‡ That is, not in or seeking paid employment. § Post hoc sensitivity analyses. ¶ Used an oral contraceptive (combined or progestogen only), injection, or vaginal ring, but not a levonorgestrel‐releasing intrauterine device or implant. |
|||||||||||||||
Box 3 – Health‐related quality of life scores (36‐item Short Form health survey, SF‐36) for the 5476 women who responded to the 2021 Australian Longitudinal Study on Women's Health survey (age range, 43–48 years), by frequency of heavy menstrual bleeding during the preceding twelve months*
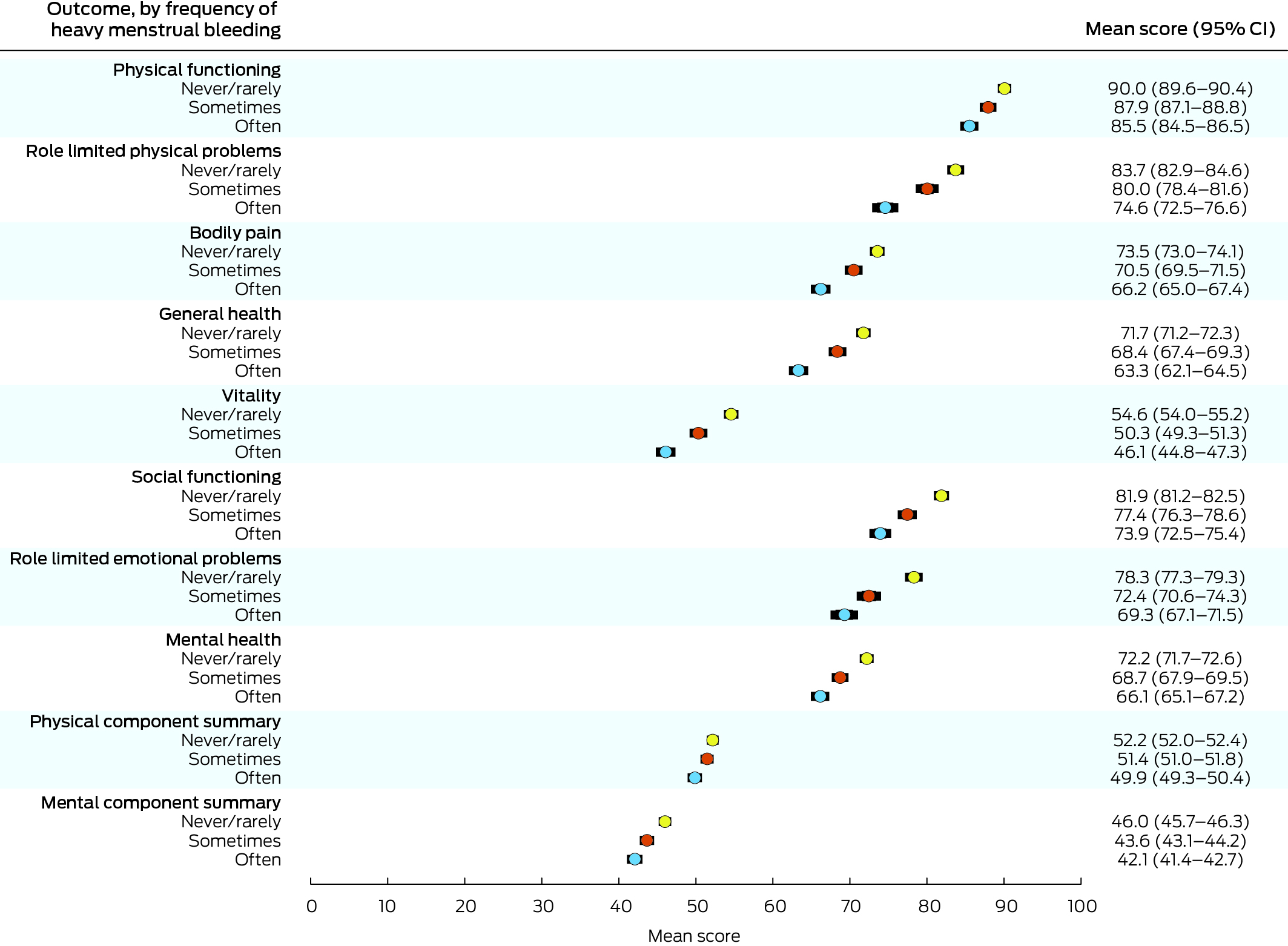
CI = confidence interval, denoted by error bars.* Excludes 1071 women who had reported hysterectomy/bilateral oophorectomy or menopause.
Received 17 April 2024, accepted 22 July 2024
- Louise Wilson1
- Tessa Copp2
- Martha Hickey3,4
- Bec Jenkinson1
- Susan J Jordan1
- Rachel Thompson2
- Gita D Mishra1
- Jenny A Doust1
- 1 Australian Women and Girls’ Health Research Centre, the University of Queensland, Brisbane, QLD
- 2 The University of Sydney, Sydney, NSW
- 3 The University of Melbourne, Melbourne, VIC
- 4 The Royal Women's Hospital, Melbourne, VIC
Open access:
Open access publishing facilitated by the University of Queensland, as part of the Wiley – the University of Queensland agreement via the Council of Australian University Librarians.
Data Sharing:
The Australian Longitudinal Study on Women's Health (ALSWH) survey data are owned by the Australian Department of Health and Aged Care. Because of the personal nature of the data collected, release by the ALSWH is subject to strict contractual and ethical restrictions. De‐identified data are available to researchers when a formal request to make use of the material has been approved by the ALSWH data access committee. The committee is receptive to requests about studies related to ALSWH investigations. Information on applying for access to ALSWH data is available at https://alswh.org.au/for‐data‐users/applying‐for‐data. For access to the linked administrative data provided by the Australian Institute of Health and Welfare, each data user must be added to the applicable data use agreements and human research ethics committee protocols.
Louise Wilson was supported by the HCF Research Foundation (2024/HE000399). Jenny Doust and Bec Jenkinson were supported by a National Health and Medical Research Council (NHMRC) Centres for Research Excellence grant (APP1153420). Gita Mishra was supported by an NHMRC Leadership Fellowship (APP2009577), and Tessa Copp by an NHMRC Emerging Leader Research Fellowship (2009419). The funding bodies played no role in the design, collection, analysis, or interpretation of data, in the writing of the manuscript, or in the decision to submit the manuscript for publication.
We thank the HCF Research Foundation for supporting this research. The investigation was conducted as part of the Australian Longitudinal Study on Women's Health by the University of Queensland and the University of Newcastle. We are grateful to the Australian Department of Health and Aged Care for funding and to the women who participated in the surveys. We acknowledge the Australian Department of Health and Aged Care for providing Medical Benefits Schedule and Pharmaceutical Benefits Scheme data, and the Australian Institute of Health and Welfare as the integrating authority. We also acknowledge the members of the Heavy Menstrual Bleeding consumer advisory group (six women with lived experience of heavy menstrual bleeding who provide advice for the HCF Research Foundation‐funded project on heavy menstrual bleeding) for their input; their questions and comments helped shape our analysis and opened up new lines of inquiry.
No relevant disclosures.
- 1. Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health‐related quality of life, work impairment, and health‐care costs and utilization in abnormal uterine bleeding. Value Health 2007; 10: 183‐194.
- 2. Weisberg E, McGeehan K, Fraser IS. Effect of perceptions of menstrual blood loss and menstrual pain on women's quality of life. Eur J Contracept Reprod Health Care 2016; 21: 431‐435.
- 3. Fraser IS, Langham S, Uhl‐Hochgraeber K. Health‐related quality of life and economic burden of abnormal uterine bleeding. Expert Rev Obstet Gynecol 2009; 4: 179‐189.
- 4. Hallberg L, Högdahl AM, Nilsson L, Rybo G. Menstrual blood loss: a population study. Variation at different ages and attempts to define normality. Acta Obstet Gynecol Scand 1966; 45: 320‐351.
- 5. National Institute for Health and Care Excellence. Heavy menstrual bleeding: assessment and management [NICE Guideline NG88]. Updated 24 May 2021. http://www.nice.org.uk/guidance/ng88 (viewed Nov 2023).
- 6. Australian Commission on Safety and Quality in Health Care. Heavy menstrual bleeding clinical care standard. June 2024. https://www.safetyandquality.gov.au/standards/clinical‐care‐standards/heavy‐menstrual‐bleeding‐clinical‐care‐standard (viewed June 2024).
- 7. Dobson AJ, Hockey R, Brown WJ, et al. Cohort profile update: Australian Longitudinal Study on Women's Health. Int J Epidemiol 2015; 44: 1547.
- 8. Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS), volume 5: remoteness structure, July 2016 (1270.0.55.005). 16 Mar 2018. https://www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005 (viewed Aug 2024).
- 9. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES‐D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med 1994; 10: 77‐84.
- 10. Teunissen AM, Merry AHH, Devies IEC, Roumen FJME. Differences in continuation rates and early removal between contraceptive and therapeutic use of the levonorgestrel‐releasing intrauterine system 52 mg. Eur J Contracept Reprod Health Care 2019; 24: 449‐456.
- 11. Ware JE, Snow KK, Kosinski M, Gandek B. SF‐36 health survey manual and interpretation guide. Boston: The Health Institute, New England Medical Center, 1993.
- 12. Chung HF, Ferreira I, Mishra GD. The association between menstrual symptoms and hypertension among young women: a prospective longitudinal study. Maturitas 2021; 143: 17‐24.
- 13. Blizzard L, Hosmer DW. The log multinomial regression model for nominal outcomes with more than two attributes. Biom J 2007; 49: 889‐902.
- 14. Santer M, Warner P, Wyke S. A Scottish postal survey suggested that the prevailing clinical preoccupation with heavy periods does not reflect the epidemiology of reported symptoms and problems. J Clin Epidemiol 2005; 58: 1206‐1210.
- 15. Santos IS, Minten GC, Valle NC, et al. Menstrual bleeding patterns: a community‐based cross‐sectional study among women aged 18–45 years in Southern Brazil. BMC Womens Health 2011; 11: 26.
- 16. Paramsothy P, Harlow SD, Greendale GA, et al. Bleeding patterns during the menopausal transition in the multi‐ethnic Study of Women's Health Across the Nation (SWAN): a prospective cohort study. BJOG 2014; 121: 1564‐1173.
- 17. Shapley M, Jordan K, Croft PR. An epidemiological survey of symptoms of menstrual loss in the community. Br J Gen Pract 2004; 54: 359‐363.
- 18. Ballard KD, Seaman HE, de Vries CS, Wright JT. Can symptomatology help in the diagnosis of endometriosis? Findings from a national case‐control study: part 1. BJOG 2008; 115: 1382‐1391.
- 19. Bigambo FM, Wang D, Zhang Y, et al. Current situation of menstruation and gynecological diseases prevalence among Chinese women: a cross‐sectional study. BMC Womens Health 2022; 22: 270.
- 20. Kiewa J, Mortlock S, Meltzer‐Brody S, et al. A common genetic factor underlies genetic risk for gynaecological and reproductive disorders and is correlated with risk to depression. Neuroendocrinology 2023; 113: 1059‐1075.
- 21. Mena GP, Mielke GI, Brown WJ. Prospective associations between physical activity and BMI with irregular periods and heavy menstrual bleeding in a large cohort of Australian women. Hum Reprod 2021; 36: 1481‐1491.
- 22. Munro MG, Mast AE, Powers JM, et al. The relationship between heavy menstrual bleeding, iron deficiency, and iron deficiency anemia. Am J Obstet Gynecol 2023; 229: 1‐9.
- 23. Abenhaim HA, Harlow BL. Live births, cesarean sections and the development of menstrual abnormalities. Int J Gynaecol Obstet 2006; 92: 111‐116.
- 24. Critchley HOD, Babayev E, Bulun SE, et al. Menstruation: science and society. Am J Obstet Gynecol 2020; 223: 624‐664.
- 25. Kemp A, Paige E, Banks E. Beginner's guide to using pharmaceutical benefits scheme data. Tips and pitfalls. Updated Aug 2012. https://nceph.anu.edu.au/files/Guide_to_Using_PBS_Data_20131125_0.pdf (viewed Aug 2023).
- 26. Kai J, Dutton B, Vinogradova Y, et. al. Rates of medical or surgical treatment for women with heavy menstrual bleeding: the ECLIPSE trial 10‐year observational follow‐up study. Health Technol Assess 2023; 27: 1‐50.






Abstract
Objectives: To estimate the prevalence of heavy menstrual bleeding among Australian women from young adulthood to midlife (22–48 years) and investigate the characteristics of women who experience this condition; to investigate the relationship of heavy menstrual bleeding and health‐related quality of life.
Study design: Longitudinal cohort survey study (Australian Longitudinal Study on Women's Health, ALSWH).
Setting, participants: Australia; baseline cohort of 14 247 women born during 1973–1978, recruited in 1996; eight post‐baseline surveys undertaken at 3‐year intervals, 2000–2021.
Main outcome measures: Self‐reported frequency of heavy menstrual bleeding during the preceding twelve months (never/rarely, sometimes, often); frequency of heavy menstrual bleeding by socio‐demographic, behavioural, health, and reproduction‐related characteristics; mean physical and mental health‐related quality of life scores (36‐item Short Form health survey, SF‐36) by frequency of heavy menstrual bleeding. Results are weighted to adjust for oversampling of participants from rural and remote areas.
Results: Data for 11 311 respondents to at least one ALSWH post‐baseline survey were included in our prevalence analysis. The prevalence of sometimes or often experiencing heavy menstrual bleeding increased from 17.6% at age 22 years (124 of 691 respondents) to 32.1% at 48 years (359 of 1132 respondents); the proportion who reported often experiencing the condition increased from 6.1% (45 participants) to 12.1% (136 participants). The likelihood of often experiencing heavy menstrual bleeding increased with body mass index (40 kg/m2 or greaterv 18.5–24.9 kg/m2: risk ratio [RR], 2.27; 95% confidence interval [CI], 1.93–2.67), and was greater for respondents who reported low iron levels (RR, 2.26; 95% CI, 2.03–2.51) or endometriosis (RR, 2.29; 95% CI, 2.06–2.54). Similar associations were seen for sometimes experiencing heavy bleeding. Mean health‐related quality of life scores for women who reported heavy menstrual bleeding were lower in all domains and for the summary mental health and physical health scores than for women who reported never or rarely experiencing the condition; the differences were greater for women who often experienced heavy menstrual bleeding.
Conclusions: Heavy menstrual bleeding was reported by large minorities of women of reproductive age, and the proportion increased with age. Many women experience symptoms that have a substantial impact on their physical and mental health‐related quality of life.