Australia's health care system is grappling with a mismatch of demand and capacity, with bottlenecks in access to, and transitions of, care and rising costs.1 Hospital‐in‐the‐home (HITH) models of care are suggested as sustainable patient‐centred, value‐based solutions.2
The opportunity
HITH is defined as a 24‐hour, 7‐days‐a‐week service of “acute inpatient equivalent care, utilising highly skilled staff, hospital technologies, equipment, medication, and safety and quality standards, to deliver hospital‐level care within a person's place of residence or preferred (non‐hospital) treatment location”.3 HITH models vary in clinical governance, combination and frequency of in‐person or telehealth visits, patient selection and clinician staffing.4,5,6 When HITH substitutes for hospital location of care (admission avoidance, AA) are compared to early supported discharge (ESD) or other hospital outreach services, clinical outcomes and patient satisfaction are comparable or improved, and care is cost‐effective.7,8 However, evidence describing those patients for whom HITH is optimal and processes to recognise and respond to deteriorating HITH patients remains limited.9,10
Existing patient safety and quality standards: the deteriorating patient
The Australian Commission on Safety and Quality in Health Care (ACSQHC) defines health service standards of care, including “recognising and responding to acute deterioration” in a patient's physical, cognitive or mental state.11 Currently, systems for managing deteriorating patients focus on hospital‐located patients with escalation when mismatches in “clinical needs and the local resources to manage them” are identified.12 In hospitals with rapid response teams, rates of activation of these teams vary considerably (1.35–71.3 per 1000 admissions).13 Mixed efficacy in improving patient outcomes is observed, with concern regarding cost‐effectiveness, sustainability, disruption to usual hospital routines, mortality as an outcome measure, deskilling of ward staff, and the impact on patient‐centred care and doctor–patient relationships, especially in end‐of‐life care.14 Relevant to the current context, evidence shows an increased reliance on systems for managing deteriorating patients with increasing patient complexity, economic and hospital capacity stress, and a focus on patient flow.14
The challenges: deteriorating patients at home
HITH models of care attached to Australian health services are subject to ACSQHC safety and quality accreditation standards.11,15 Despite HITH being available in Australia for many years, gaps remain in translation of hospital systems to manage deteriorating patients to HITH locations of care, standardised definitions, and data collection, making audit, research, benchmarking and policy difficult.8,16 The incidence of HITH patient deterioration and transfer back to hospital is difficult to establish because it is confused with post‐discharge readmission rates, reported within disease‐specific research and not model of care research, and impacted by variability in patient complexity and acuity.9,17,18,19
Systems to manage deteriorating patients rely on identification of patient deterioration, and safe, timely, appropriate responses. HITH models introduce geographical distance, variable contexts of care, altered opportunities for patient observation, and adjacent community‐based stakeholders including paid and unpaid caregivers and health care providers such as general practitioners, specialist physicians, nurses, allied health practitioners and paramedicine practitioners. Coordinating across these fragmented hospital and community services is complex without real‐time information sharing and communication systems.
Recognising deteriorating patients at home
HITH services rely on patient selection to mitigate risk.20 Services that achieve safe, earlier diversion of higher acuity, more complex patients offer more value.4 Geographical distance offers opportunities for innovative digital adjuncts such as wearable and continuous monitoring devices and video telehealth.21,22 However, the sensitivity, specificity, noise to signal ratio for clinical deterioration remains unclear. Also, the cost‐effectiveness, utility in risk assessment, and value of digital adjuncts to clinicians, patients and caregivers need clarification. Current evidence suggests that HITH nurses use clinical cues in collaboration with patients and caregivers along with context‐specific social and environmental factors, such as safety in the home for patients, workforce and caregivers to identify and respond to clinical deterioration.23,24
HITH offers unique opportunities to incorporate nuanced qualitative observation tools, such as caregiver assessment and escalation, proven effective in paediatric cohorts.25 Similar systems are evolving in adult care to detect deterioration in adults living with multimorbidity, cognitive impairment and frailty.26 Situations with appropriate limitations on futile care or palliative intent, coupled with deficiencies in community aged care services, ageism, poor shared understanding of HITH capabilities and risks of hospital‐based care increase complexity in HITH systems managing deteriorating patients.27 Co‐designing integrated care that includes effective systems to manage deteriorating patients with patients, caregivers and stakeholders across hospital and community services is crucial to optimise patient‐centred outcomes and maintain trust in the health care system. When poorly implemented, unintended consequences include caregiver burden to recognise, escalate and observe deteriorating patient events.28
Responding to deteriorating patients at home
After recognition, HITH systems to manage deteriorating patients should provide clear options in terms of what happens next, including the timing, people involved and location. Clinicians must be skilled in weighing up and accepting risk across individualised thresholds and timeframes for in‐person or telehealth assessment, access to diagnostic and intervention resources, in community or hospital locations, with safety‐netting in observation and care during and after recognition, assessment and response to deteriorating patients. When relocating patients to hospital, clinicians must establish when, by which mode of transport, to which resourced patient reception area for assessment and management, under governance of which accountable unit and using which communication strategies for patients, caregivers and clinicians.29
Current HITH pathways to manage deteriorating patients rely on existing community‐based systems, such as ambulance and emergency department services, especially after hours (Box). Patients, caregivers and HITH clinicians are usually advised to call 000 despite limited system enablers for information sharing and clinical handover between HITH, paramedicine and receiving emergency department clinicians. Should these emergency system resources be allocated to HITH deteriorating patients? Ironically, deteriorating HITH patients then enter bottlenecks that HITH models of care were designed to ease, waiting for ambulances to arrive, or ramped in emergency departments waiting to access over‐stretched hospital services. Alternative hospital access points (eg, day procedure units, specialist services such as oncology and dialysis, and patient flow wards such as transit lounges) are unable to meet the needs of the deteriorating patient in the community, especially after hours, thus perpetuating reliance on primary care, ambulance services and emergency departments.
Systems to manage HITH deteriorating patients should mitigate these risks through education and partnership with community services, visual clues identifying patients as admitted HITH patients (door signs and patient identification labels), and prominently displayed 24‐hour HITH phone access for patients, caregivers and clinicians. In the United States, regulations mandate safety elements, including service‐specific patient selection criteria, pre‐established advanced care planning, minimum daily in‐person assessments, processes for patients uncontactable within 15 minutes of scheduled care, immediate on‐demand remote audio connection to a registered nurse or physician and in‐home response within 30 minutes if needed.30,31 To meet safety regulations, many American HITH services employ paramedics and buy their own patient transport vehicles.
The future for HITH deteriorating patients
Safely upscaling HITH models of care requires integration of 24/7 HITH‐suitable systems to manage deteriorating patients. Accountability to these systems will mitigate the risk of unintended burden on patients, caregivers, clinicians and existing services, such as ambulance and emergency departments.
Health services implementing HITH models of care must consider the risk management, clinical governance, resourcing, quality, safety, performance monitoring and continuous improvement of these systems. This includes safe, timely provision of 24/7 components of care novel to hospital services such as:
- access to health and care advice and escalation pathways for community‐based patients and their caregivers;
- procurement of digital technology and equipment that optimises remote patient management;
- real‐time information sharing and communication systems with community health and care partners;
- patient transportation options, with or without clinical supervision, and guidance on the mode and timing of safe relocation of HITH patients back to hospital locations of care; and
- patient reception, assessment and treatment areas away from access points for non‐admitted patients, such as emergency departments.
Health departments investing in HITH expansion must incorporate these operational considerations and work with national peak bodies, including the ACSQHC, to drive system level safety and efficiency in:
- HITH‐suitable deterioration systems including policies, procedures, definitions and performance monitoring, including:
- review of the existing deteriorating patient standard to ensure suitability to HITH service models;
- updates that consider expected versus unexpected deterioration;
- triggers for escalation of patients from home to hospital locations of care.
- awareness, knowledge sharing and trust building to reduce unnecessary escalations of care for HITH patients;
- defining, training and credentialling an HITH suitable workforce capable of recognising and responding to deteriorating HITH patients; and
- future research and industry partnerships that advance sustainable patient‐centred, value‐based HITH models of care.
HITH offers opportunities to break down existing silos between hospital and community locations of health and care delivery to advance the safe, timely recognition and response to deteriorating patients.
Box – Hospital‐in‐the‐home flowcharts to manage deteriorating patients
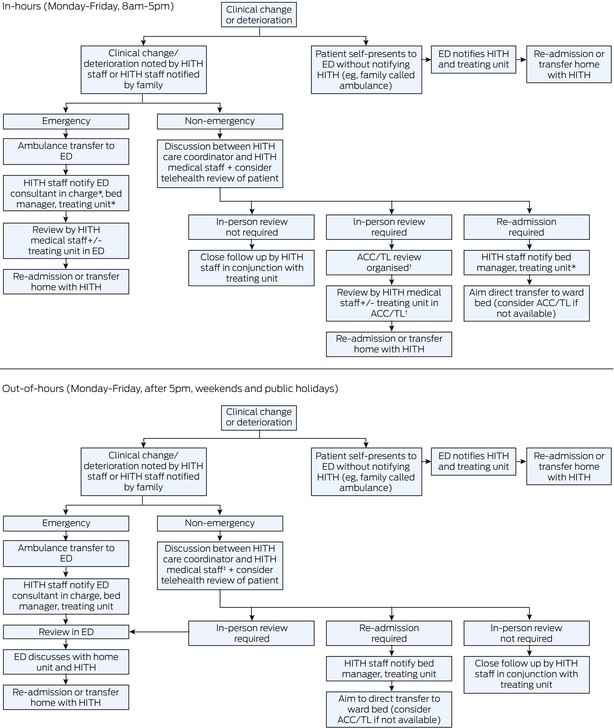
ACC = ambulatory care centre; ED = emergency department; HITH = hospital‐in‐the‐home; TL = transit lounge. * to be performed by HITH medical staff in‐hours. † if out‐of‐hours, follow out‐of‐hours flowchart. ‡ HITH medical staff may include residents on site or consultants on call. Source: used with permission from The Austin Hospital‐in‐the‐Home service, Melbourne, Australia.
Provenance: Not commissioned; externally peer reviewed.
- 1. Kerr R. Time for a revolution in funding public hospital capacity. Sydney: Australasian Medical Publishing Company, 2022. https://insightplus.mja.com.au/2022/46/time‐for‐a‐revolution‐in‐funding‐public‐hospital‐capacity/ (viewed Sept 2024).
- 2. Reddy S, Phelps G, Rasa J. Australia's acute care system: more hospital beds or fewer? Sydney: Australasian Medical Publishing Company, 2022. https://insightplus.mja.com.au/2022/44/australias‐acute‐care‐system‐more‐hospital‐beds‐or‐fewer/ (viewed Sept 2024).
- 3. Hospital in the Home Society Australasia Ltd. Position statement: Definition of Hospital in the Home. HITH Society Australasia Ltd, 2019. https://www.hithsociety.org.au/Definition (viewed Sept 2024).
- 4. Critical Intelligence Unit. Evidence brief: Hospital in the Home. Sydney: NSW Health, 2024.
- 5. Partington A, Schultz T, Gray J, et al. Identifying potential populations for home hospitalisation: a scoping review of the literature to support the review of the South Australian My Home Hospital service. Adelaide: Flinders University; 2022.
- 6. Levine DM, Findeisen S, Desai MP, et al. Hospital at home worldwide: program and clinician characteristics from the World Hospital at Home Congress survey. J Am Geriatr Soc 2024; 12: 3824‐3832.
- 7. Board N, Brennan N, Caplan GA. A randomised controlled trial of the costs of hospital as compared with hospital in the home for acute medical patients. Aust N Z J Public Health 2000; 24: 305‐311.
- 8. Leong MQ, Lim CW, Lai YF. Comparison of Hospital‐at‐Home models: a systematic review of reviews. BMJ Open 2021; 11: e043285.
- 9. Sriskandarajah S, Hobbs J, Roughead E, et al. Safety and effectiveness of ‘hospital in the home’ and ‘outpatient parenteral antimicrobial therapy’ in different age groups: a systematic review of observational studies. Int J Clin Pract 2018: e13216.
- 10. Lim AKH, De Silva ML, Wang RSH, et al. Observational study of the incidence and factors associated with patient readmission from home‐based care under the Hospital in the Home programme. Intern Med J 2021; 51: 1497‐1504.
- 11. Australian Commission on Safety and Quality in Health Care. Recognising and Responding to Acute Deterioration Standard. Sydney: ACSQHC, 2021. https://www.safetyandquality.gov.au/standards/nsqhs‐standards/recognising‐and‐responding‐acute‐deterioration‐standard (viewed Sept 2024).
- 12. College of Intensive Care Medicine of Australia and New Zealand, Australian and New Zealand Intensive Care Society. Joint position statement on rapid response systems in Australia and New Zealand and the roles of intensive care. CICM and ANZICS, 2016. https://www.anzics.org/wp‐content/uploads/2018/09/ANZICS_CICMRapidResponseSystemsPositionStatement_2016.pdf (viewed Sept 2024).
- 13. Jones D. The epidemiology of adult Rapid Response Team patients in Australia. Anaesth Intensive Care 2014; 42: 213‐219.
- 14. Subramaniam A, Botha J, Tiruvoipati R. The limitations in implementing and operating a rapid response system. Intern Med J 2016; 46: 1139‐1145.
- 15. The Australian Council on Healthcare Standards 2024. https://www.achs.org.au. (viewed Oct 2024).
- 16. Colt Cowdell J, Lopez E, Haney A, et al. Risk factors associated with escalation of care in a quaternary academic hospital at home program. J Hosp Med 2024; 19: 1‐8.
- 17. Sriskandarajah S, Ritchie B, Eaton V, et al. Safety and clinical outcomes of Hospital in the Home. J Patient Saf 2020; 16: 123‐129.
- 18. Daniels A, Walsh D, Ledford C, Wilkins T. Hospital at home readmissions. Ann Fam Med 2023; 21: 3756.
- 19. Hecimovic A, Matijasevic V, Frost SA. Characteristics and outcomes of patients receiving Hospital at Home Services in the South West of Sydney. BMC Health Serv Res 2020; 20: 1090.
- 20. Pati S, Thompson GE, Mull CJ, et al. Improving patient selection and prioritization for hospital at home through predictive modeling. AMIA Annu Symp Proc 2023; 2022: 856‐865.
- 21. Aagaard N, Larsen AT, Aasvang EK, Meyhoff CS. The impact of continuous wireless monitoring on adverse device effects in medical and surgical wards: a review of current evidence. J Clin Monit Comput 2023; 37: 7‐17.
- 22. Paganelli AI, Mondéjar AG, da Silva AC, et al. Real‐time data analysis in health monitoring systems: a comprehensive systematic literature review. J Biomed Inform 2022; 127: 104009.
- 23. Gray E, Currey J, Considine J. Hospital in the Home nurses’ recognition and response to clinical deterioration. J Clin Nurs 2018; 27: 2152‐2160.
- 24. McCullough K, Baker M, Bloxsome D, et al. Clinical deterioration as a nurse sensitive indicator in the out‐of‐hospital context: a scoping review. J Clin Nurs 2024; 33: 874‐889.
- 25. Oakley E, Moulden A, Mills E, et al. Improving the safety of care for Victorian children. Melbourne: Safer Care Victoria; 2023.
- 26. Hodge SY, Ali MR, Hui A, et al. Recognising and responding to acute deterioration in care home residents: a scoping review. BMC Geriatr 2023; 23: 399.
- 27. van Oppen JD, Coats T, Conroy S, et al. Person‐centred decisions in emergency care for older people living with frailty: principles and practice. Emerg Med J 2024: 41: 694‐699.
- 28. Moss CT, Schnipper JL, Levine DM. Caregiver burden in a home hospital versus traditional hospital: a secondary analysis of a randomized controlled trial. J Am Geriatr Soc 2024; 72: 286‐289.
- 29. Australian College for Emergency Medicine, Australian and New Zealand College of Anaesthetists, College of Intensive Care Medicine of Australia and New Zealand. PG52 Guideline for transport of critically ill patients 2024. ACEM, ANZCA, CICM, 2024. https://www.anzca.edu.au/getattachment/bd5938d2‐d3ab‐4546‐a6b0‐014b11b99b2f/PG52(G)‐Guideline‐for‐transport‐of‐critically‐ill‐patients‐(PS52) (viewed Oct 2024).
- 30. Adams D, Wolfe AJ, Warren J, et al. Initial findings from an acute hospital care at home waiver initiative. JAMA Health Forum 2023; 4: e233667.
- 31. Pandit JA, Pawelek JB, Leff B, Topol EJ. The hospital at home in the USA: current status and future prospects. NPJ Digit Med 2024; 7: 48.






Open access:
Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
We acknowledge the work of The Austin Hospital‐in‐the‐Home (HITH) team and creators of the flowcharts in the Box, supplied and included with permission. Our thanks to: Angela Sullivan, Nurse Unit Manager, HITH and Virtual Care; Mark Horrigan, Medical Director HITH and Virtual Care; Danielle Panaccio, HITH Consultant; and Daniel Thuys, HITH Case Manager.
No relevant disclosures.