The work of prisoner‐of‐war (POW) doctors imprisoned by the Japanese is well known, with men such as Edward “Weary” Dunlop, Bruce Hunt and Rowley Richards celebrated as heroes of the many prison camps scattered across South‐East Asia during the Second World War.1 While accounts of captive medical officers have focused on the general medical and surgical treatment of POWs, the remarkable diaries of Major Kennedy Byron Burnside (Box 1), head of an Australian bacteriology and pathology laboratory in the sprawling Changi prison camp complex, offer a detailed view of the specific pathology services available in the camp. The diaries reveal the integral role that pathology played in the provision of medical care and advancement of medical research in Changi and suggest that the medical and scientific cultures that developed among Allied personnel in Japanese captivity were part of a broader health infrastructure that drew on many forms of prisoner labour and expertise.
JEL Classifications
History and humanities; Diagnostic techniques and procedures
From Melbourne to Singapore: Burnside's war
Kennedy Burnside was born in Victoria in 1913, educated at Melbourne Grammar, and graduated from the University of Melbourne in 1937. He was resident and then registrar at the Alfred Hospital from 1938 to 1939. In July 1940, he joined the Australian Army Medical Corps with the rank of captain and served in various Australian general hospitals. Burnside was sent to Singapore in April 1941 as head of the 2nd Mobile Bacteriological Laboratory, a small unit tasked with studying tropical diseases and providing support services such as blood typing to casualty clearing stations and hospitals treating soldiers wounded in the fight against the Japanese. He was promoted to major a few months later.
When Singapore fell in February 1942, Burnside and his unit were sent to Changi, the main POW camp in South‐East Asia, which, at its peak, held over 50 000 Allied POWs. Although the situation in Changi never descended to the appalling conditions of the work camps along the Burma–Thailand Railway (hereafter, the railway), the camp was overcrowded and inadequately provisioned, and the prisoners were vulnerable to sudden displays of harsh discipline from their captors. Crucially, however, the Allied forces retained significant autonomy over the internal organisation of the camp, including the provision of medical services. This resulted in an improvised but extensive health infrastructure that replicated many aspects of conventional military medicine. Burnside remained in charge of his laboratory for most of his captivity and assumed several other roles including acting commander of the re‐organised 9/10 Field Ambulance. In mid‐1943, he became the Australian Imperial Force's anti‐malaria officer, and from December 1943 to May 1944, assisted in the British–Australian combined hospital's malaria centre. Along with most POWs, Burnside moved from the general Changi camp to the adjacent Changi Gaol in mid‐1944 when the Japanese ordered the POWs to be concentrated in this smaller area. In April 1945, he joined a work party at the River Valley Road Camp (also on Singapore Island) as a medical officer, where he remained until just before the end of the war in August.
Burnside maintained his detailed diaries throughout, burying portions of it (as well as his forbidden cameras) in salvaged naval gun shell cases to protect against Japanese surveillance.2 Although historians recognise that diaries are seldom encompassing or infallible sources, they offer important insights into the past if properly contextualised. Their comprehensive record of Changi's medical infrastructure, combined with their rarity as a surviving account of POW life, make Burnside's diaries a valuable source for understanding daily medical work in Japanese captivity.
Testing, diagnosis and education: the work of the laboratory
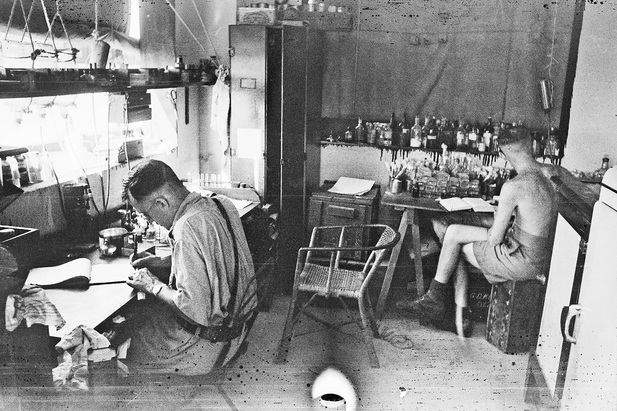
Initially established in a corner of a veranda in the Australian‐occupied Selarang Barracks (its painstaking assembly described in the diary as a “hideous job”), Burnside's laboratory was primarily engaged in what he described as “elementary clinical pathology”: standard testing to detect malaria and dysentery, twin scourges in the early phase of captivity (Box 2, Box 3).2 One critical early task was to distinguish between cases of bacillary and amoebic dysentery, a distinction that guided treatment and prevention. Supported by a rotating team of five assistants and working from 10 am to 9 pm with a break in the afternoon, the laboratory was able to process over fifty blood and stool specimens a day.
The laboratory also performed diagnostics at the specific request of the Japanese, whose own medical infrastructure was under substantial pressure throughout the war.3 In December 1942, Burnside assisted Japanese medical officers in the testing of 1000 Dutch POWs for dysentery.2 In March 1943, on Japanese orders, the laboratory conducted malaria tests for some 2500 prisoners destined for the railway. The malaria screening saw 600 samples processed per day; a challenging task given dwindling supplies of microscope slides and stains.2
Burnside and his laboratory also contributed to Changi's robust intellectual and scientific culture. Changi presented a unique environment in which medical personnel from different units, specialties and backgrounds were thrust together to work for the benefit of their captive comrades.1 Access to comparatively well developed facilities and the medical personnel's determination to avoid professional stagnation promoted collective endeavours such as the Changi Medical Society, which sought to find innovative solutions to the POWs’ medical problems and to share medical and scientific knowledge among the POW population.2,4 Burnside lectured on physiology, anatomy and malaria diagnosis and, with his senior technicians, trained medical officers and junior laboratory personnel in more advanced pathology techniques, enabling them to prepare and interpret specimens. These skills were vital as Burnside's escalating responsibilities drew him out of the laboratory; they were also important as work parties bound for the railway, Borneo, and other sites throughout Japanese‐occupied Asia required medical officers and technicians with diagnostic expertise.2
Research problems: dysentery and malaria
The routine dysentery and malaria screening work foregrounded two key research projects for Burnside's laboratory. First was the production of a dysentery vaccine, a project in which the psychiatrist John Cade, later famous for the (re)discovery of lithium for the treatment of mania, was an enthusiastic collaborator.5 Burnside spent much of March 1942 reading up on dysentery and addressing the technical aspects of vaccine production. While his technicians prepared various agar plates and growth media, Burnside isolated, cultured, concentrated and heat‐killed the bacteria to produce samples suitable for inoculation. While the work was fraught with technical frustrations and practical difficulties, Burnside wrote that he found it “all very fascinating” and was “really thoroughly enjoying it”.2
On 29 March 1942, Burnside diluted his “first successful experimental batch”, and that evening Cade injected himself and ten volunteers.2 Despite his apprehensions, Burnside also took a dose and found the side effects to be minimal.2 The vaccination program then scaled up rapidly. In the middle of April, Cade inoculated around 200 POWs per day and by May, some 1500 POWs had received two doses. As June opened, Burnside's laboratory was producing hundreds of doses bound for the British lines, where the epidemic had hit hardest.6 The effectiveness of Burnside's vaccine was difficult to quantify, coinciding as it did with an increasing awareness among the POWs about the importance of sanitation and hygiene, but by the middle of the year, the epidemic had slowed. Admissions to the main hospital dropped from a weekly peak of 1196 towards the end of March to 150 per week by the start of June. By the end of 1942, dysentery in Changi was classified as “controlled, but not fully mastered.”6
Burnside's abiding concern, though, was malaria, which reached epidemic proportions in Changi by late 1943.7 A significant medical problem for the Australian forces throughout the war, malaria was especially worrisome in POW camps, where sick and malnourished prisoners were more vulnerable to cerebral malaria and other complications — risks multiplied several times over for those working on the railway.8 In Changi, anti‐malarial work was hampered by a shortage of supplies such as malaroil and mosquito nets, the destruction of existing drainage and other mosquito prevention measures, obstruction by the Japanese (including denial of permission to access known mosquito breeding grounds), and the return of heavily infected POWs from the railway. Limited availability of quinine and atebrin also inhibited adequate treatment. Burnside, who had briefly worked under renowned malaria expert JW Fields in Kuala Lumpur before the Japanese invasion, was given a crash course in large scale clinical management, treating “about 300 cases” in December 1943, amounting to “quite a decent clinical experience of the disease”. One POW colleague, he noted with some satisfaction, told him he would have “a greater experience of malaria than anyone else in the AIF [Australian Imperial Force] Malaya”.2
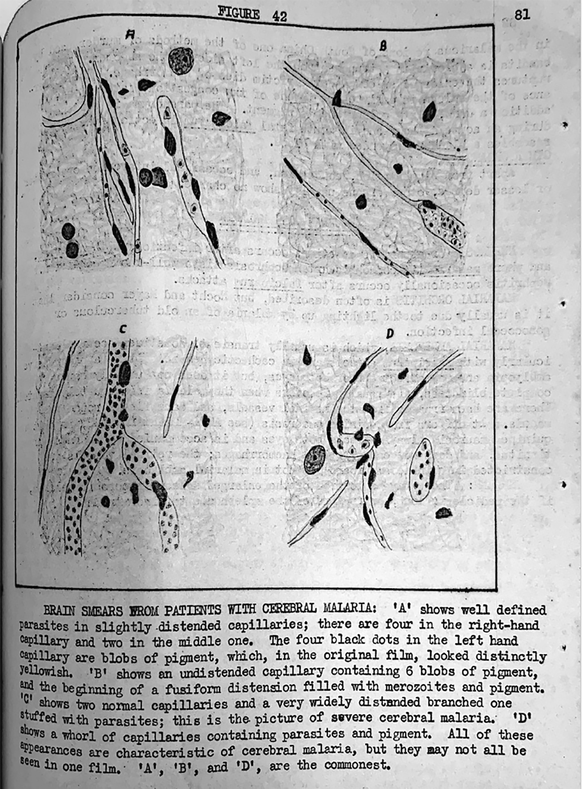
The diagnostic testing carried out by Burnside's laboratory played a crucial role in the response to malaria in Changi, both by confirming cases even in the absence of overt symptoms and by identifying the dangerous Plasmodium falciparum strain, which required more stringent attention. Occasionally, infections appeared to proceed by stealth, likely complicated by the compounding effects of nutritional deficiencies and related conditions such as beriberi. In these circumstances, autopsies emerged as a significant tool in understanding malaria's systemic effects. In Changi, autopsies appear to have been the rule rather than the exception, and in his diary Burnside detailed several autopsies performed on infected prisoners whose symptoms gave little warning of their impending fatal collapse.2 Burnside helped arrange demonstrations of brain smears that provided definitive evidence of infection, which was especially important in disputed cases. In September 1944, for example, a heated disagreement between Burnside, Lieutenant Colonel John Strahan of the Royal Army Medical Corps (former Malaria Research Officer at Kuala Lumpur's Institute for Medical Research) and 2/10th Australian General Hospital pathologist Roy Maynard over a prisoner's cause of death was only settled after the latter was shown smears exhibiting the telltale parasite and pigments of cerebral malaria.2
It is clear from his diaries that the diagnosis, treatment and prevention of malaria presented Burnside — who was also studying anatomy, mathematics and languages in his spare time — with a compelling intellectual challenge. Beginning in 1942, he wrote articles about malarial diagnosis, which he shared among his fellow medical officers and with malaria specialists like Strahan for critique. By 1944, these articles had evolved into a comprehensive textbook, Principles of malaria, complete with Burnside's hand‐drawn illustrations of parasites detected in blood and other samples (Box 4). This text, which now resides in the Australian War Memorial, is notable for the sections on blood film preparation and interpretation urging careful attention to the procedures that ensured accurate diagnosis.
A camp‐wide effort: POW medical and scientific cultures
Burnside's diaries also confirm the extent to which other POWs — from all ranks and backgrounds — contributed to the medical infrastructure of the camp. Some helped secure hospital and laboratory supplies, either from the Japanese, through black market trading, or through improvisation. Others volunteered for scientific experiments, including Burnside's dysentery vaccine, and for nutritional studies led by the camp Nutritional Advisory Group (some details were later published in the MJA).4,9 While historians of medicine acknowledge that wartime complicates the conventional hierarchies of civilian medicine, in Changi and other POW camps, the demarcations of expertise and authority were further tested by privation and widespread illness.10 In such circumstances, clinicians might easily become patients, and patients might also become part of an improvised medical workforce acquiring new technical skills under unusual pressure. Such work might even be a form of respite. Soon after the fall of Singapore, Burnside's friend Captain Tom Mitchell arrived in Changi in a state of “severe mental shock” after being badly concussed during the fighting on the peninsula. Placed under the care of John Cade, he was allowed to recuperate by learning the routines of Burnside's laboratory, eventually transferring there when he was well enough.
Professional identities: wartime and beyond
Finally, the diaries provide a window into wartime's effects on professional identities. Writing in August 1944, Burnside mused over whether his wartime labours would have any relevance to his post‐war career — a common concern for POW doctors. He concluded that they were worth doing for their own sake; that he would “never have a better opportunity for work. “Starved of other joys”, he concluded, “the pleasure of learning comes into its own”.2
This “pleasure of learning” appears to have underpinned much of Burnside's professional life after the war. He took his membership of the Royal College of Surgeons and fellowship of the Royal College of Surgeons in England in 1947, before returning to the Alfred Hospital in 1948 and becoming a Fellow of the Royal Australasian College of Surgeons. While he did not continue with his bacteriology and pathology work, Burnside did pursue another medical specialisation: urology. He became a (self‐taught) expert in the use of endoscopic surgical techniques and, in 1956, formed the Alfred's first separate urological unit. He continued to work as a consultant urologist during the 1960s and 1970s, serving as president of the Urological Society of Australia from 1973 to 1974. When Burnside died in 1983, the reminiscences published in the MJA remarked on the self‐discipline and energy that made these achievements possible — qualities also evident throughout his time in Changi.11
Box 1 – Major Kennedy Byron Burnside in Changi, 1942
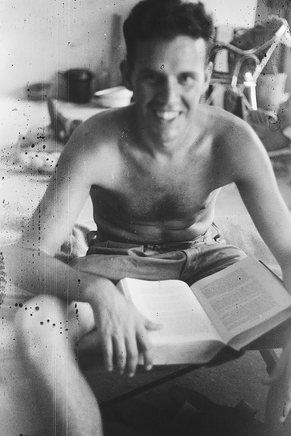
Source: Australian War Memorial collection, AWM P03821.058.
Box 2 – Burnside's veranda laboratory, 1942. The relatively sophisticated set up and capabilities of the laboratory owed much to Burnside and his assistants’ dedication to maintaining their equipment and their adaptation of methods to produce and store various reagents
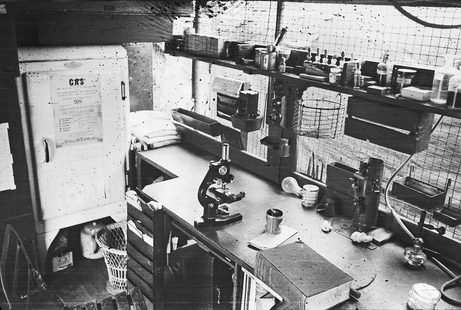
Source: Australian War Memorial collection, AWM P03821.006.
Provenance: Not commissioned; externally peer reviewed.
- 1. Hearder R. Keep the men alive: Australian POW doctors in Japanese captivity. Sydney: Allen & Unwin, 2009.
- 2. Australian War Memorial. Burnside, Kennedy B (Major, AAMC and POW Malaya), 3DRL/7665, Collection. Australian War Memorial, Canberra.
- 3. Pennington LK. Casualties of history: wounded Japanese servicemen and the Second World War. Ithaca: Cornell University Press, 2015.
- 4. Westmore A, Weisz GM. Medical research undertaken in captivity: a form of resistance to imprisonment and attempted extermination. War Soc 2009; 28: 89‐112.
- 5. Cade JFJ. Lithium salts in the treatment of psychotic excitement. Med J Aust 1949; 2: 349‐351.
- 6. Royal Army Medical Corps Muniments Collection. Annual Medical Report POW Camp Changi, February 1942‐1943 Part I. (Reference RAMC/1016/2). Wellcome Collection.
- 7. Royal Army Medical Corps Muniments Collection. Annual Medical Report POW Camp Changi, February 1943‐1944 Part II. (Reference RAMC/1016/3). Wellcome Collection.
- 8. Shanks GD. Malaria‐associated mortality in Australian and British prisoners of war on the Thai‐Burma Railway 1943‐1944. Am J Trop Med Hyg 2019; 100: 846‐850.
- 9. Harvey C. Medical aspect of the Singapore captivity. Med J Aust 1946; 1: 769‐772.
- 10. Cooter R, Harrison M, Sturdy S, editors. Medicine and modern warfare. Amsterdam–Atlanta, GA: Rodopi, 1999.
- 11. Kennedy D. Kennedy Byron Burnside. Med J Aust 1984; 3: 169.





Kate Ariotti's salary is supported by a research fellowship (Australian Research Council DE200100099).
No relevant disclosures.