The age‐adjusted prevalence of diabetes among Aboriginal and Torres Strait Islander people (Indigenous Australians) is almost three times that for non‐Indigenous Australians;1 rates of acute and chronic diabetes complications are also higher.2 Type 2 diabetes leads to other health conditions, poorer quality of life and shorter life expectancy.3 The first national report on Aboriginal health (1979) noted that Indigenous people “were generally in good health and that most of the disorders which commonly affect them today were non‐existent in Australia.”4 A 1970 study had noted that type 2 diabetes was considered rare among Indigenous Australians not living in urban environments.5
Diet and physical activity play primary roles in the prevention and management of type 2 diabetes and are recommended as first line management.6,7,8 Physical activity interventions improve blood glucose and glycated haemoglobin (HbA1c) levels,9,10 triglyceride and high‐density lipoprotein (HDL) cholesterol levels,11 and insulin sensitivity in muscle and liver.12,13 Physical activity is effective for mobilising visceral fat;14 although the reasons remain unclear, aerobic exercise is more effective than resistance training.15
In clinical practice and in research investigations, people may be advised to increase their physical activity, but often without structured physical activity education and only limited direction.16
In light of the high prevalence of diabetes and poor diabetes‐related outcomes for Indigenous Australians, we conducted a systematic review to guide future strategies for the prevention and management of type 2 diabetes. A preliminary search of the PROSPERO, Cochrane Library, Scopus, MEDLINE, SPORTSDiscus, PsycINFO, and Informit databases identified no current or planned systematic reviews of physical activity interventions for preventing and managing type 2 diabetes in Indigenous Australians. We therefore reviewed the evidence regarding the effect of physical activity for preventing and managing type 2 diabetes in Aboriginal and Torres Strait Islander Australians.
Methods
The protocol for our systematic review has been published,17 and the review was prospectively registered with the PROSPERO International Prospective Register of Systematic Reviews (CRD42021247496; 12 May 2021). Our review conforms with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement.18
Search strategy
Our search strategy was developed in consultation with a research librarian. Nine databases were searched during 18 April 2021 – 31 October 2022, from their start dates to 30 October 2022: MEDLINE; Scopus, Embase (both Elsevier); Cumulative Index to Nursing and Allied Health Literature (CINAHL), Sports Discus, PsycInfo (all EBSCO); Informit Complete; ProQuest Dissertations and Theses, and ProQuest Health and Medicine. We searched for published reports in English of physical activity interventions for preventing and managing type 2 diabetes in Aboriginal and Torres Strait Islander adults (18 years of age or older). The key search terms were “type 2 diabetes”, “Indigenous”, “Australia”, and “physical activity” (Supporting Information, table 1).
Studies that included participants other than Indigenous Australians were considered if more than 50% of participants were Indigenous Australians or results for Indigenous Australian participants were separately reported. Individual‐ and group‐based interventions, programs, and activities were included, as were multicomponent interventions if they included exposure to physical activity. Studies without structured physical activity sessions were considered if advice on physical activity was mentioned.
All publications of studies that compared physical activity interventions with usual care or alternative treatments, and studies without comparison groups, were screened for relevance. Experimental studies, including randomised controlled trials and non‐randomised controlled clinical trials, as well as quasi‐experimental, observational, cohort, case–control, and analytical cross‐sectional studies were screened for relevance. Programs, activities, and interventions in any geographic areas or regions of Australia (urban, rural, remote) and setting (clinic, community) were screened for relevance if the participants continued living in their usual environment during the intervention. There were no exclusion criteria based on type, frequency, length, or intensity of physical activity. However, short term events (eg, duration of 1–14 days) were excluded; such interventions may have short term effects, but reports on longer term interventions provide more information about sustained benefits.
The primary outcome of interest for our review was mean change from baseline in glycated haemoglobin (HbA1c) level. Secondary outcomes of interest were changes in physical activity levels, weight, waist circumference, blood pressure, fasting plasma glucose, blood lipid and fasting insulin levels, quality of life, psychological wellbeing, and medication use.
Data extraction and critical appraisal
All records identified in the database searches were imported into Covidence (https://www.covidence.org) and duplicates removed. The titles and abstracts of each article were independently screened by two authors (RJK, RM). The full text of publications that met our inclusion criteria or required further examination to determine their eligibility was retrieved; the two reviewers independently determined whether the articles met our inclusion criteria. Differences between reviewers regarding eligibility were resolved by discussion and consensus. One reviewer (RJK) extracted data from two‐thirds of the reports, and the second reviewer (RM) extracted data from one‐third. The reviewers worked independently to extract key characteristics of the included articles: author, publication year, location, Aboriginal nations of the participants, study aim, study design, study duration, sample size, mean age, male participant proportion, intervention measures, outcome measures, and findings.
We assessed the quality of each study, including risk of bias, using the Joanna Briggs Institute (JBI) critical appraisal tools19 and the ethical and methodological quality of studies from the Indigenous Australian perspective using the Centre of Research Excellence in Aboriginal Chronic Disease Knowledge Translation and Exchange (CREATE) Critical Appraisal Tool.20 In each case, outcomes were classified as low (0–33%), medium (34–66%), or high quality (67–100%). The reviewers worked independently and differences between reviewers in ratings were resolved by discussion and consensus. The ratings did not influence study inclusion in our review; this deviation from the published protocol was made because of the small number of relevant studies. We assessed the certainly of evidence with the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) assessment tool (https://www.gradeworkinggroup.org).
Results
The database searches identified 703 potentially relevant records; after removing 408 duplicates, the titles and abstracts of 295 publications were screened. A total of 268 records were excluded, most because the participants were not Indigenous Australians, or because no physical activity component was reported (eg, nutrition counselling only). The full text of 27 articles was assessed for eligibility, of which 18 were excluded: seven did not report outcomes related to type 2 diabetes, three did not report relevant interventions, two did not separately report data for Indigenous participants, two did not include Indigenous Australians, two were reviews that provided no original data, one did not include physical activity in the intervention, and one was an abstract (Box 1).
Nine studies met our inclusion criteria (Supporting Information, table 2). One study was published before 2000,21 five during 2000–2010,22,23,24,25,26 and three during 2011–2021.27,28,29 Two were randomised controlled trials,27,28 five were cohort studies,21,22,24,25,29 one a quasi‐experimental study,26 and one was a repeated cross‐sectional study23 (Box 2). One of the cohort studies utilised a mixed methods design but only the quantitative data was relevant to this review.29 The GRADE assessment determined that the studies in this review provide a low certainty of evidence (data not shown). As differences in study design, outcome variables, and the small number of studies precluded meta‐analysis, we provide a narrative summary of their findings.
Study types and intervention components
The repeated cross‐sectional study of a community‐wide intervention for preventing and managing diabetes collected data at baseline and seven years.23 We included this study because it was conducted at the community level, but it provided no information about the impact of physical activity at the individual level.
The two randomised controlled trials, of 12‐week structured physical activity programs, did not report outcomes for Indigenous participants diagnosed with type 2 diabetes. One trial recruited people with pre‐diabetes,28 the other included participants with type 2 diabetes but did not separately report their outcomes.27 One trial — 51 women in the active group, 49 in the comparison group — evaluated the effectiveness of a 12‐week structured physical activity and nutrition program on biomedical markers of metabolic functioning.27 The second — 16 people in the exercise group, ten in the control group — measured the impact of physical activity change on glucose regulation and inflammatory markers associated with type 2 diabetes in men at risk of type 2 diabetes.28
One cohort study reported changes in type 2 diabetes and heart disease after reverting to a more traditional lifestyle for seven weeks.21 One cohort study assessed the impact of a lifestyle intervention on risk factors associated with type 2 diabetes.25 Two cohort studies examined the prevention and management of diabetes with community‐wide interventions.22,24 One cohort study investigated the effect on diabetes management of the Flinders Model of self‐management care, with trained Aboriginal health workers to assist participants.26 The most recent cohort study evaluated an Aboriginal health care worker‐led, ten‐week diabetes lifestyle program for urban Aboriginal people in an Aboriginal organisation.29
Two studies (both randomised controlled trials) included structured physical activity sessions. One study included two supervised 45–60‐minute physical activity sessions per week, including both aerobic and resistance training, with 30 minutes of each session at medium to high intensity;27 the second study began with two physical activity sessions per week, increasing to three per week from week 6.28 Two studies encouraged participants to increase the number of steps taken each day and provided them with pedometers.25,27 Two cohort studies provided physical activity advice, but did not check the activity of participants; one advised participants to walk each day,29 the other walking, team sports, and hunting.22 Hunting was a component of physical activity in three studies.21,22,23 Two cohort studies mentioned that a physical activity component was involved but provided limited detail.24,26
Diabetes‐related physiological assessments
Six studies reported changes in HbA1c levels. Neither randomised controlled trial reported statistically significant changes in mean HbA1c levels;27,28 one study did not separately report results for participants with and without diabetes.27 Two cohort studies reported statistically significant changes in mean HbA1c level; from 8.15% (65.4 mmol/mol; standard deviation [SD], 1.61%) at baseline to 6.29% (45.2 mmol/mol; SD, 1.04%) at ten weeks,29 and from 8.79% (72.0 mmol/mol; SD not reported) at baseline to 8.09% (64.9 mmol/mol) at twelve months,26 One cohort study reported a slight increase in mean HbA1c level six months after the intervention, but, as diabetes medication use did not change, the increase may have reflected differences in seasonal food intake during the recent holiday season.25 One study reported that HbA1c levels improved but did not report relevant data.24
Improvements in other diabetes‐related measures were reported by some studies: reduced mean fasting plasma glucose (–5.0 mmol/L at seven weeks; SD not reported);21 –0.9 mmol/L at six months (SD not reported);22 –0.3 mmol/L in people without diabetes at seven years (SD not reported);23 reduced mean fasting plasma insulin levels (–11 mU/L at seven weeks; SD not reported);21 reduction in insulin area under the curve (–25% in the intervention group at twelve weeks, no change in the control group28); improved glucose tolerance (community‐wide reduction across the seven years between tests);23 and reduced insulin resistance (greater improvement in Matsuda Insulin Sensitivity Index score for physical activity group than control group between baseline and twelve weeks).28
Study quality, and ethical and methodological quality from an Indigenous perspective
Eight of the nine studies were rated as being low or medium quality (median JBI score, 54%; interquartile range [IQR], 36–64%). The JBI scores for the two randomised controlled trials were 58%28 and 65%,27 those for the five cohort studies ranged from 18%24 to 64%,22 the score for the cross‐sectional study was 75%,23 and that for the quasi‐experimental study 22%26 (Box 2).
Seven of the nine studies were rated as being of low to medium ethical and methodological quality from the Indigenous perspective (median CREATE score, 50%; IQR, 36–64%). The CREATE scores for the two randomised controlled trials were 36%28 and 64%27, those for the five cohort studies ranged from 21%24 to 100%,29 the score for the cross‐sectional study was 50%,23 and that for the quasi‐experimental study 64%.26 The quality of the mixed methods study, assessed with the JBI qualitative assessment tool, was rated as 100% (Box 2).
Discussion
Our review identified few high quality studies of interventions for preventing and managing type 2 diabetes in Indigenous Australians that included physical activity; further, the value of the findings of many studies were affected by shortcomings in design, power, and input from Aboriginal communities and researchers. Our findings suggest areas for improvement in gathering evidence for future strategies for preventing and managing type 2 diabetes in Indigenous Australians.
Despite the increasing prevalence of type 2 diabetes among Indigenous Australians, only two randomised controlled trials included physical activity as a component for its prevention and management. One of the trials assessed the impact of physical activity on men at risk of type 2 diabetes, and did not include participants with diabetes;28 the second did not include any male participants and did not report results by diabetes status.27
Our review of intervention studies that included physical activity for preventing or managing type 2 diabetes, a key lifestyle change, found no randomised controlled trials that reported outcomes by type 2 diabetes status, and identified that the design of many studies was inadequate. Further, no randomised controlled trials have included both dietary interventions and physical activity, the cornerstone of diabetes type 2 management by general practitioners.8 Inadequate experimental research design in Indigenous health research is not restricted to diabetes research. A review of medical research involving Indigenous Australians completed since the first Closing the Gap report (2008) found that only 57 of 2150 published studies (2.7%) were randomised controlled trials, and that 58% were descriptive studies,30 which may be of questionable validity if Indigenous researchers were not involved. While other research types are important, the outcomes of randomised controlled trials inform guidelines and change clinical practice.31
Only two publications included in our review had Indigenous people as first authors;27,29 none of the other publications identified an Indigenous research team member. More rigorous research is needed, led by Indigenous people, to advance the study of type 2 diabetes in Indigenous people. Well designed randomised controlled studies are needed to evaluate the impact of clinically relevant exercise interventions that prevent type 2 diabetes or improve metabolic control in people with type 2 diabetes, with clearly defined outcomes meaningful for Indigenous Australians. Research led by Indigenous researchers and communities could achieve this aim, as the need to improve health outcomes is best recognised by those who are directly affected.32
Drivers of physical activity at the population level include the availability of safe, accessible, family‐friendly, and inexpensive locations for physical activity. Simple, effective advice and support from health professionals, based on the current level of fitness of the individual, could also improve physical activity levels. Appropriate locations and advice are both often limited in regional and remote communities. Interventions that can lead to a healthy, supporting environment include those in which family members are involved, and advice and support is provided by a trusted health professional who understands the barriers faced by the local community.
Limitations
The findings of our review are limited by the differences in the interventions, their duration, and the assessments described in the nine included publications. The Indigenous peoples of Australia are heterogeneous, with more than 250 language groups (Supporting Information, figure 1), and one cannot assume that the findings of the few studies we included apply to all Indigenous people. Although two authors reviewed the publications at each stage, a risk of bias affecting study inclusion remains. While there is some evidence linking physical activity with improved health for Indigenous Australians with type 2 diabetes, intervention studies that are meaningful, well designed, and provide unambiguous outcomes are still needed.
Conclusion
We have identified that quality research into the impact of physical activity on type 2 diabetes in Aboriginal and Torres Strait Islander people is sparse. To improve research translation, studies that involve Indigenous community members at all levels of the research process are needed, especially during data interpretation and writing. Although advice on diet and physical activity is a cornerstone of the management of type 2 diabetes, rigorous research in this area for Aboriginal and Torres Strait Islander people is limited, and more is required.
Box 1 – Identification and selection of publications of studies of physical activity interventions for preventing and managing type 2 diabetes in Aboriginal and Torres Strait Islander Australians
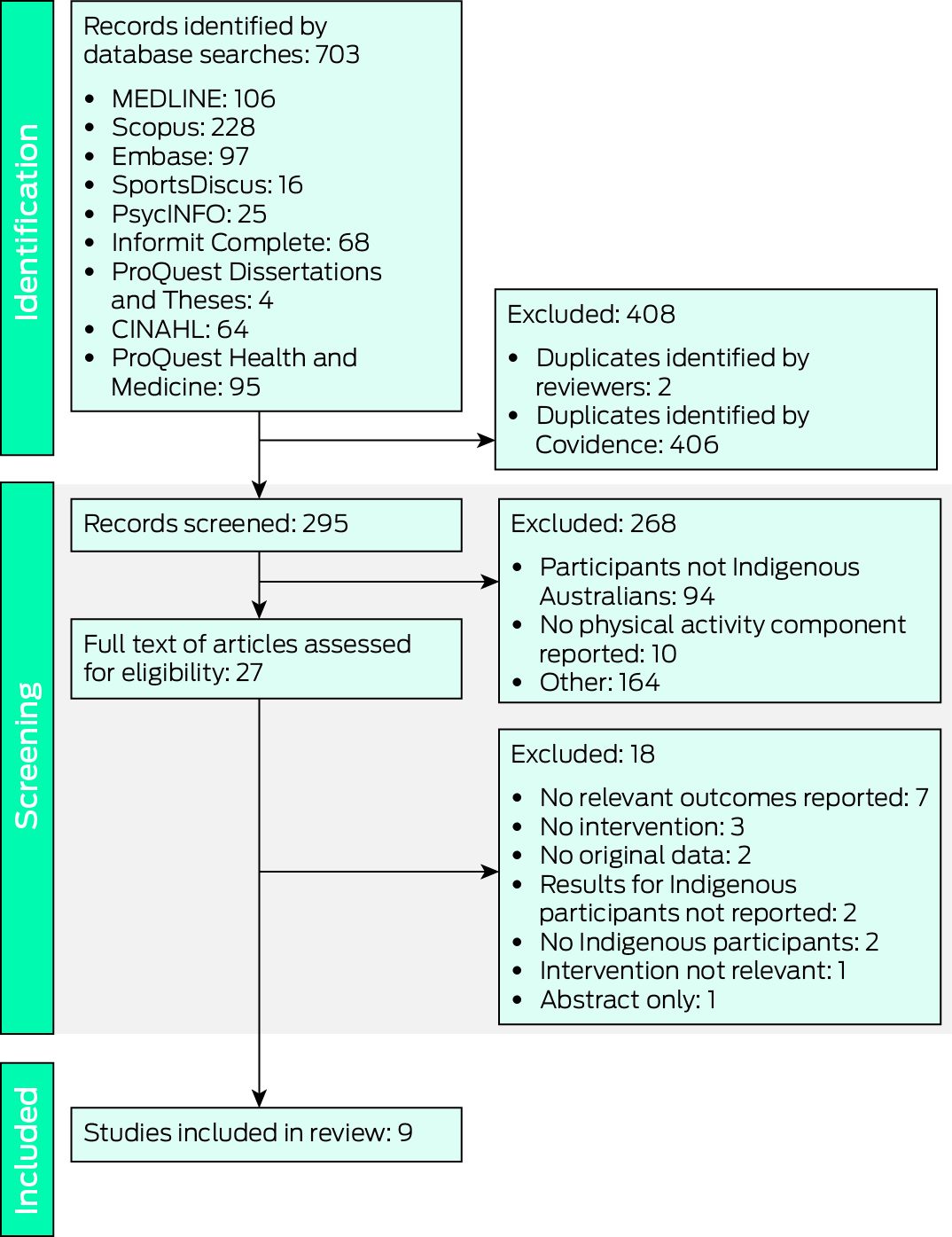
CINAHL = Cumulative Index to Nursing and Allied Health Literature.
Box 2 – Assessment of study quality, and ethical and methodological quality from the Indigenous perspective, of the nine included publications: summary findings*
|
|
Criteria met |
||||||||||||||
|
Publication |
Risk of bias (JBI) |
Ethical/methodological quality (CREATE) |
|||||||||||||
|
|
|||||||||||||||
|
Randomised controlled trials |
|
|
|||||||||||||
|
Canuto et al, 201227 |
8.5/13 (65%; medium) |
9/14 (64%; medium) |
|||||||||||||
|
Mendham et al, 201528 |
7.5/13 (58%; medium) |
5/14 (36%; medium) |
|||||||||||||
|
Cohort studies |
|
|
|||||||||||||
|
O'Dea, 198421 |
6/11 (55%; medium) |
5/14 (36%; medium) |
|||||||||||||
|
Rowley et al, 200022 |
7/11 (64%; medium) |
11/14 (79%; good) |
|||||||||||||
|
Gracey et al, 200624 |
2/11 (18%; poor) |
3/14 (21%; poor) |
|||||||||||||
|
Chan et al, 200725 |
5/11 (45%; medium) |
5/14 (36%; medium) |
|||||||||||||
|
Power et al, 202129 |
5.5/11 (50%; medium) |
14/14 (100%; good) |
|||||||||||||
|
Quasi‐experimental study |
|
|
|||||||||||||
|
Battersby et al, 200826 |
2/9 (22%; poor) |
9/14 (64%; medium) |
|||||||||||||
|
Cross‐sectional study |
|
|
|||||||||||||
|
Rowley et al, 200023 |
6/8 (75%; good) |
7/14 (50%; medium) |
|||||||||||||
|
Qualitative component of cohort study |
|
|
|||||||||||||
|
Power et al, 202129 |
10 (100%; good) |
— |
|||||||||||||
|
|
|||||||||||||||
|
CREATE = Centre of Research Excellence in Aboriginal Chronic Disease Knowledge Translation and Exchange critical appraisal tool;20 JBI = Joanna Briggs Institute critical appraisal tools.19 * The questions and the complete assessments for each set of appraisal tools are included in the Supporting Information, tables 4 to 7. |
|||||||||||||||
Received 17 July 2023, accepted 27 March 2024
- Raymond J Kelly1
- Rona Macniven2
- Leonid Churilov1
- Margaret J Morris2
- David O'Neal3,4
- Elif I Ekinci1,4
- 1 Melbourne Medical School, the University of Melbourne, Melbourne, VIC
- 2 UNSW Sydney, Sydney, NSW
- 3 St Vincent's Hospital, Melbourne, VIC
- 4 Austin Health, Melbourne, VIC
We thank Helen Chan (Information Services Department, University of Technology Sydney) for her assistance with the design of the search strategy.
Elif I Ekinci receives research funding from Eli Lilly, Novo Nordisk, Amgen, Versanis, Endogenex, Novartis, Astra Zeneca; she is on advisory boards and gives presentations for Eli Lilly, Astra Zeneca, and Boehringer. These funds are donated to diabetes research at her institution.
- 1. Australian Bureau of Statistics. National Aboriginal and Torres Strait Islander Health Survey, 2018–19. 11 Dec 2019. https://www.abs.gov.au/statistics/people/aboriginal‐and‐torres‐strait‐islander‐peoples/national‐aboriginal‐and‐torres‐strait‐islander‐health‐survey/latest‐release (viewed Sept 2024).
- 2. Australian Commission on Safety and Quality in Health Care. The fourth Australian atlas of healthcare variation. 28 Apr 2021. https://www.safetyandquality.gov.au/publications‐and‐resources/resource‐library/fourth‐australian‐atlas‐healthcare‐variation‐2021 (viewed Dec 2023).
- 3. Lascar N, Brown J, Pattison H, et al. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol 2018; 6: 69‐80.
- 4. House of Representatives Standing Committee on Aboriginal Affairs. Aboriginal health: report. 1979. https://nla.gov.au/nla.obj‐2720242915 (viewed Nov 2023).
- 5. Wise PH, Edwards FM, Thomas DW, et al. Hyperglycaemia in the urbanized Aboriginal. The Davenport survey. Med J Aust 1970; 2: 1001‐1006.
- 6. Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care 2016; 39: 2065‐2079.
- 7. Dyson P, Twenefour D, Breen C, et al. Diabetes UK evidence‐based nutrition guidelines for the prevention and management of diabetes. Diabet Med 2018; 35: 541‐547.
- 8. Royal Australian College of General Practitioners. Management of type 2 diabetes: a handbook for general practice. July 2020. https://www.racgp.org.au/getattachment/41fee8dc‐7f97‐4f87‐9d90‐b7af337af778/Management‐of‐type‐2‐diabetes‐A‐handbook‐for‐general‐practice.aspx (viewed Nov 2023).
- 9. Bird SR, Hawley JA. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc Med 2017; 2: e000143.
- 10. Boniol M, Dragomir M, Autier P, Boyle P. Physical activity and change in fasting glucose and HbA1c: a quantitative meta‐analysis of randomized trials. Acta Diabetol 2017; 54: 983‐991.
- 11. Shawahna R, Batta A, Asa'ad M, et al. Exercise as a complementary medicine intervention in type 2 diabetes mellitus: a systematic review with narrative and qualitative synthesis of evidence. Diabetes Metab Syndr 2021; 15: 273‐286.
- 12. Taylor R. Pathogenesis of type 2 diabetes: tracing the reverse route from cure to cause. Diabetologia 2008; 51: 1781‐1789.
- 13. Sampath Kumar A, Maiya AG, Shastry BA, et al. Exercise and insulin resistance in type 2 diabetes mellitus: a systematic review and meta‐analysis. Ann Phys Rehabil Med 2019; 62: 98‐103.
- 14. Herzig KH, Ahola R, Leppäluoto J, et al. Light physical activity determined by a motion sensor decreases insulin resistance, improves lipid homeostasis and reduces visceral fat in high‐risk subjects: PreDiabEx study RCT. Int J Obes 2014; 38: 1089‐1096.
- 15. Bellicha A, van Baak MA, Battista F, et al. Effect of exercise training on weight loss, body composition changes, and weight maintenance in adults with overweight or obesity: an overview of 12 systematic reviews and 149 studies. Obes Rev 2021; 22 (Suppl 4): e13256.
- 16. Short CE, Hayman M, Rebar AL, et al. Physical activity recommendations from general practitioners in Australia. Results from a national survey. Aust N Z J Public Health 2016; 40: 83‐90.
- 17. Evans J, Canuto K, Kelly R, et al. Physical activity interventions to prevent and manage type 2 diabetes among Aboriginal and Torres Strait Islander peoples: a systematic review protocol. JBI Evid Synth 2021; 19: 177‐183.
- 18. Moher D, Liberati A, Tetzlaff J, et al; PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Int J Surg 2010; 8: 336‐341.
- 19. Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. Adelaide: Joanna Briggs Institute, 2020. https://jbi‐global‐wiki.refined.site/space/MANUAL/355863557/Previous+versions (viewed Nov 2023).
- 20. Harfield S, Pearson O, Morey K, et al. Assessing the quality of health research from an Indigenous perspective: the Aboriginal and Torres Strait Islander quality appraisal tool. BMC Med Res Methodol 2020; 20: 79.
- 21. O'Dea K. Marked improvement in carbohydrate and lipid metabolism in diabetic Australian Aborigines after temporary reversion to traditional lifestyle. Diabetes 1984; 33: 596‐603.
- 22. Rowley KG, Daniel M, Skinner K, et al. Effectiveness of a community‐directed “healthy lifestyle” program in a remote Australian Aboriginal community. Aust N Z J Public Health 2000; 24: 136‐144.
- 23. Rowley KG, Gault A, McDermott R, et al. Reduced prevalence of impaired glucose tolerance and no change in prevalence of diabetes despite increasing BMI among Aboriginal people from a group of remote homeland communities. Diabetes Care 2000; 23: 898‐904.
- 24. Gracey M, Bridge E, Martin D, et al. An Aboriginal‐driven program to prevent, control and manage nutrition‐related “lifestyle” diseases including diabetes. Asia Pac J Clin Nutr 2006; 15: 178‐188.
- 25. Chan LCK, Ware R, Kesting J, et al. Short term efficacy of a lifestyle intervention programme on cardiovascular health outcome in overweight Indigenous Australians with and without type 2 diabetes mellitus: the healthy lifestyle programme (HELP). Diabetes Res Clin Pract 2007; 75: 65‐71.
- 26. Battersby M, Ah Kit J, Prideaux C, et al. Implementing the Flinders Model of self‐management support with Aboriginal people who have diabetes: findings from a pilot study. Aust J Prim Health 2008; 14: 66‐74.
- 27. Canuto K, Cargo M, Li M, et al. Pragmatic randomised trial of a 12‐week exercise and nutrition program for Aboriginal and Torres Strait Islander women: clinical results immediate post and 3 months follow‐up. BMC Public Health 2012; 12: 933.
- 28. Mendham AE, Duffield R, Marino F, Coutts AJ. A 12‐week sports‐based exercise programme for inactive Indigenous Australian men improved clinical risk factors associated with type 2 diabetes mellitus. J Sci Med Sport 2015; 18: 438‐443.
- 29. Power T, East L, Gao Y, et al. A mixed‐methods evaluation of an urban Aboriginal diabetes lifestyle program. Aust N Z J Public Health 2021; 45: 143‐149.
- 30. Kennedy M, Bennett J, Maidment S, et al. Interrogating the intentions for Aboriginal and Torres Strait Islander health: a narrative review of research outputs since the introduction of Closing the Gap. Med J Aust 2022; 217: 50‐57. https://www.mja.com.au/journal/2022/217/1/interrogating‐intentions‐aboriginal‐and‐torres‐strait‐islander‐health‐narrative
- 31. National Health and Medical Research Council. 2016 NHMRC standards for guidelines. 2016. https://www.nhmrc.gov.au/guidelinesforguidelines/standards (viewed Dec 2023).
- 32. Lewis C, Mehmet M, Quinton S, Reynolds N. Methodologies for researching marginalised and/or potentially vulnerable groups. International Journal of Market Research 2023; 65: 147‐154.






Abstract
Objectives: To review evidence regarding the impact of physical activity interventions for preventing and managing type 2 diabetes in Aboriginal and Torres Strait Islander Australians.
Study design: We searched for published reports of physical activity interventions for preventing and managing type 2 diabetes in Indigenous adults (18 years or older). There were no exclusion criteria regarding study type or duration, frequency, length, or intensity of physical activity, except that short term interventions were excluded. We assessed the quality of each study using the Joanna Briggs Institute (JBI) critical appraisal tools and the ethical and methodological quality of studies from an Indigenous Australian perspective with the Centre of Research Excellence in Aboriginal Chronic Disease Knowledge Translation and Exchange (CREATE) Critical Appraisal Tool.
Data sources: MEDLINE; Scopus, Embase (Elsevier); Cumulative Index to Nursing and Allied Health Literature (CINAHL), Sports Discus, PsycINFO (EBSCO); Informit Complete; ProQuest Dissertations and Theses, and ProQuest Health and Medicine; each from their inception to 30 October 2022.
Results: The database searches identified 703 potentially relevant records; after removing duplicates and initial screening, the full text of 27 articles was assessed for eligibility. Nine studies met our inclusion criteria: two randomised controlled trials, five cohort studies, one quasi‐experimental study, and one repeated cross‐sectional study. Eight studies were rated as being of low or medium quality (median JBI score, 54%; interquartile range [IQR], 36–64%); seven studies were rated as being of low to medium ethical and methodological quality from the Indigenous perspective (median CREATE score, 50%; IQR, 36–64%). Six studies reported changes in glycated haemoglobin (HbA1c) levels, of which two (both cohort studies) reported significantly lower mean HbA1c levels after the intervention, but only one publication provided detailed results. No randomised controlled trials that investigated the effect of a combination of physical activity and dietary change for Indigenous Australians diagnosed with type 2 diabetes were identified. Differences in study design, outcome variables, and the small number of studies precluded meta‐analysis.
Conclusions: Quality research into the impact of physical activity interventions on type 2 diabetes in Indigenous people is sparse. To improve research translation, studies that involve Indigenous community members at all levels of the research process are needed.
Registration: PROSPERO CRD42021247496 (prospective).