Acute rheumatic fever (ARF) and rheumatic heart disease (RHD) are caused by untreated group A streptococcus infections. Their prevalence is much higher among First Nations people than other Australians.1 Treatment guidelines recommend that people with ARF or RHD be hospitalised (RHD) and notified to jurisdictional RHD registers (ARF, RHD); early diagnosis is associated with better clinical outcomes.2,3
In Western Australia, the notification by clinicians of new ARF and RHD diagnoses has been mandatory since 2009 and 2015 respectively.2,4 WA RHD Register staff record demographic and clinical details for each case, and commence recall and reminder services for people with ARF or RHD. For people who are hospitalised, clinical coders enter discharge summary information into the WA Hospital Morbidity Data System (HMDS), using International Classification of Diseases, tenth revision, Australian modification (ICD‐10‐AM) codes (ARF: I00–I02; RHD: I05–I09). The register should also be notified of any person hospitalised with ARF or RHD. In 2020, we estimated that 54% of cases of RHD in First Nations people and 99% of cases in non‐Indigenous people in WA were not recorded in the register, but no person‐identifiable regional analyses or validation studies have been undertaken.5
For our retrospective administrative data analysis, we validated ARF and RHD hospitalisations in the remote Midwest region of WA, calculated RHD register notification rates, and examined demographic and clinical factors associated with notification. [Correction added on 9 October 2024, after first online publication: this sentence has been corrected.] All hospitalisations with ARF or RHD in the Midwest region during 1 May 2012 – 30 April 2022 were identified in the HMDS. Medical records for the admissions were requested (including discharge summaries, pathology results, specialist reports, emergency presentation and inpatient paper medical records), reviewed, and validated by resident medical officers, with cardiologist support as required. Records that could not be obtained or which indicated that the case did not meet the criteria for possible, probable, or confirmed diagnosis of ARF or RHD2 were excluded. First Nations people were identified from information in clinical notes in paper medical records and hospital admission records (in which Indigenous status is self‐reported or recorded by the clinician).
The study was approved by the Western Australian Aboriginal Health Ethics Committee (project reference 717), the WA Health Department (2016/29), and the WA Country Health Service Human Research Ethics Committee (2022.14). First Nations oversight and governance of the parent project for this study (End RHD in Australia: Study of Epidemiology, ERASE6) was provided by First Nations chief investigators. We regularly communicate ERASE findings, prior to their publication, to the National Aboriginal Community Controlled Health Organisation and the Aboriginal Health Council of Western Australia.
Records for 69 people (confirmed ARF, 33; confirmed RHD, 36) were cross‐referenced with the RHD register to determine notification status (Box 1). The small number precluded formal statistical comparisons. Twenty‐five of 33 ARF cases and twelve of 36 RHD cases had been notified to the register. Thirty of the ARF cases and 28 of the RHD cases had been diagnosed during 2015–2022; 31 of 33 people with ARF and 21 of 36 with RHD were First Nations people. The median age for cases of unnotified RHD was higher than for notified cases (68 years; interquartile range [IQR], 42–77 years v 30 years; IQR, 15–49 years), and a larger proportion involved non‐Indigenous people (14 of 24, 58% v one of 12, 8%). The proportions of people with specialist referrals (18 of 25, 72% v 3 of 8, 38%) and people who had commenced secondary prophylaxis (21 of 25, 84% v 5 of 8, 63%) were larger for notified than unnotified cases of ARF. However, only 26 of 33 people with ARF had been referred for echocardiography. The clinical features of unnotified RHD were more frequently consistent with more severe disease (17 of 24, 71% v 6 of 12 notified cases, 50%) (Box 2). The WA RHD register was subsequently notified of all previously unnotified cases of ARF and RHD identified during our study.
Our study was limited to data included in the available medical records. However, WA RHD register notification rates in the Midwest region were similar to those reported elsewhere in Australia.5 ARF and RHD notification rates were higher for First Nations people, and the median age of people with notified RHD was lower. Care aligned with national treatment guidelines, more likely to achieve favourable clinical outcomes, was more frequently noted for notified than unnotified cases of ARF.2,3,7
People with unnotified RHD receive acute care in hospitals in the Midwest region of WA, but the non‐notification rate is concerningly high (67%). People with unnotified RHD do not benefit from the monitoring and case management offered by the WA register. Notification rates in the surrounding WA regions where the burden of ARF and RHD is high (including the Pilbara and Goldfields) should also be examined. Clinician awareness of notification requirements, including for advanced disease, and automated technology that facilitates ARF and RHD notification, are needed.
Box 1 – Identification and validation of cases of people hospitalised with acute rheumatic fever (ARF) or rheumatic heart disease (RHD) in the Midwest region of Western Australia, 1 May 2012 – 30 April 2022
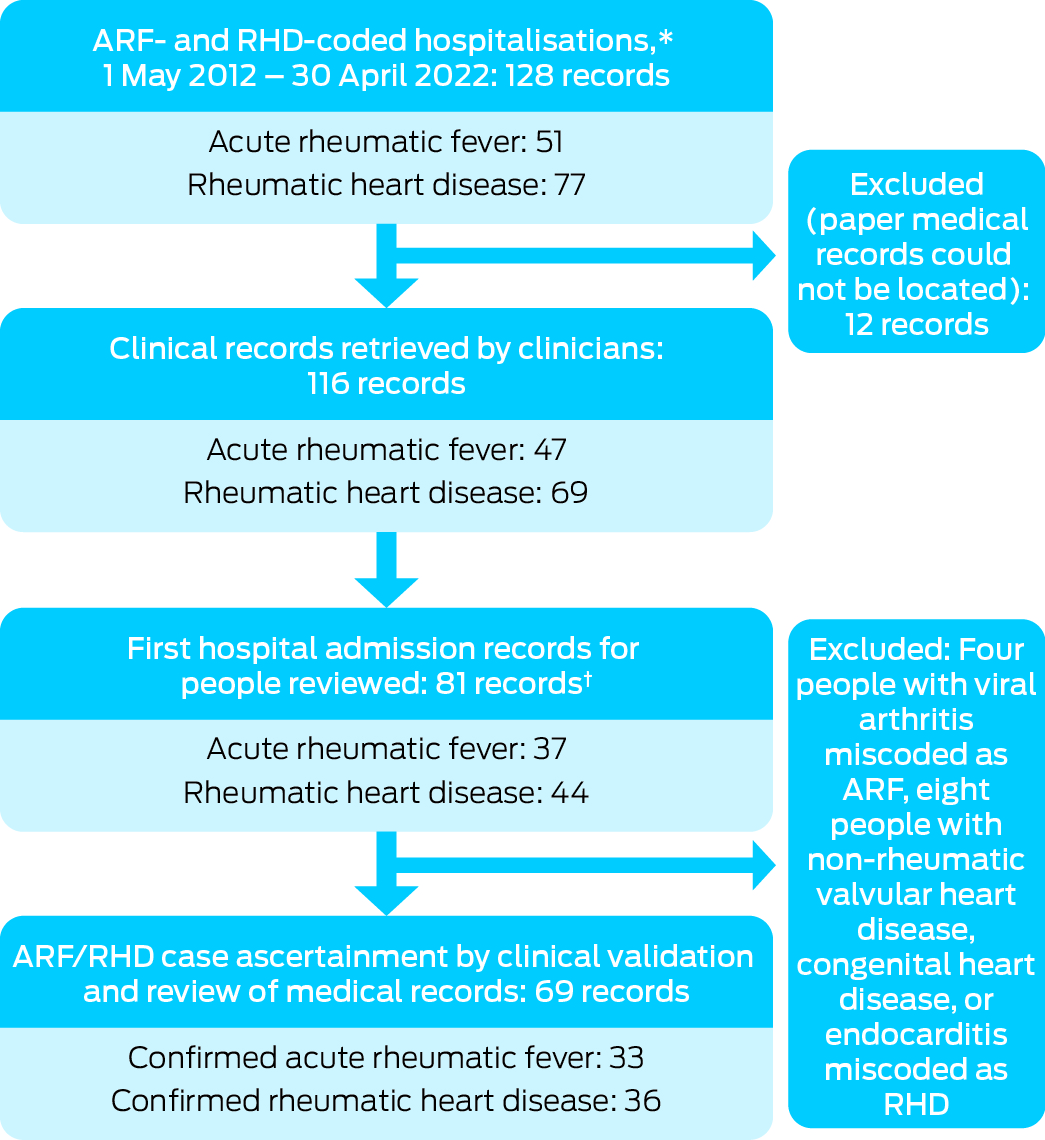
* International Statistical Classification of Diseases, tenth revision, Australian modification diagnosis codes I00–I02 (ARF) and I05–I09 (RHD).† The first hospital admission record for each person was initially reviewed; if RHD register notification was not recorded, subsequent re‐admission records were also reviewed to check the notification status.
Box 2 – Demographic and clinical characteristics of people hospitalised with acute rheumatic fever or rheumatic heart disease in the Midwest region of Western Australia, 1 May 2012 – 30 April 2022, by Western Australian RHD register notification status
|
Characteristic |
Notified cases |
Unnotified cases |
|||||||||||||
|
|
|||||||||||||||
|
Confirmed cases of acute rheumatic fever |
25 |
8 |
|||||||||||||
|
Age (years), median (IQR) |
15 (10–15) |
12 (8.5–14.5) |
|||||||||||||
|
Age (years), range |
5–48 |
6–36 |
|||||||||||||
|
Sex (women) |
12 (48%) |
5 (63%) |
|||||||||||||
|
First Nations people |
25 (100%) |
6 (75%) |
|||||||||||||
|
Diagnosis 2015–2022* |
24 (96%) |
6 (75%) |
|||||||||||||
|
Major diagnostic criteria |
|
|
|||||||||||||
|
Joint involvement |
22 (88%) |
8 (100%) |
|||||||||||||
|
Carditis |
2 (8%) |
3 (38%) |
|||||||||||||
|
Fever |
14 (56%) |
4 (50%) |
|||||||||||||
|
Elevated C‐reactive protein level |
7 (28%) |
0 |
|||||||||||||
|
Acute rheumatic fever treatment |
|
|
|||||||||||||
|
Specialist referral |
18 (72%) |
3 (38%) |
|||||||||||||
|
Echocardiogram referred/performed |
19 (76%) |
7 (88%) |
|||||||||||||
|
Secondary prophylaxis commenced |
21 (84%) |
5 (63%) |
|||||||||||||
|
Confirmed cases of rheumatic heart disease |
12 |
24 |
|||||||||||||
|
Age (years), median (IQR) |
30 (15–49) |
68 (42–77) |
|||||||||||||
|
Age (years), range |
8–73 |
12–84 |
|||||||||||||
|
Sex (women) |
10 (83%) |
16 (67%) |
|||||||||||||
|
First Nations people |
11 (92%) |
10 (42%) |
|||||||||||||
|
Diagnosis 2015–2022 |
8 (67%) |
20 (83%) |
|||||||||||||
|
Rheumatic heart disease presentation |
|
|
|||||||||||||
|
Admitted with valvular pathology |
7 (58%) |
15 (63%) |
|||||||||||||
|
Severe rheumatic heart disease |
6 (50%) |
17 (71%) |
|||||||||||||
|
History of acute rheumatic fever |
2 (17%) |
8 (33%) |
|||||||||||||
|
History of cardiac surgery |
6 (50%) |
12 (50%) |
|||||||||||||
|
|
|||||||||||||||
|
* That is, after notifications of acute rheumatic fever and rheumatic heart disease were both mandatory in Western Australia. |
|||||||||||||||
Received 4 October 2023, accepted 7 June 2024
- 1. Katzenellenbogen JM, Bond‐Smith D, Seth RJ, et al. Contemporary incidence and prevalence of rheumatic fever and rheumatic heart disease in Australia using linked data: the case for policy change. J Am Heart Assoc 2020; 9: e016851.
- 2. RHDAustralia (ARF/RHD writing group). The 2020 Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease, 3.2 edition. Mar 2022. https://www.rhdaustralia.org.au/system/files/fileuploads/arf_rhd_guidelines_3.2_edition_march_2022.pdf (viewed May 2024).
- 3. Stacey I, Hung J, Cannon J, et al. Long‐term outcomes following rheumatic heart disease diagnosis in Australia. Eur Heart J Open 2021; 1: oeab035.
- 4. Heart Foundation; Menzies School of Health Research. Western Australian RHD Register and control program. Updated 6 Aug 2024. https://www.rhdaustralia.org.au/western‐australia (viewed Aug 2024).
- 5. Agenson T, Katzenellenbogen JM, Seth R, et al. Case ascertainment on Australian registers for acute rheumatic fever and rheumatic heart disease. Int J Environ Res Public Health 2020; 17: 5505.
- 6. Katzenellenbogen JM, Bond‐Smith D, Seth RJ, et al; ERASE Collaboration Study Group. The End Rheumatic Heart Disease in Australia Study of Epidemiology (ERASE) Project: data sources, case ascertainment and cohort profile. Clin Epidemiol 2019; 11: 997‐1010.
- 7. Stacey I, Ralph A, de Dassel J, et al. The evidence that rheumatic heart disease control programs in Australia are making an impact. Aust N Z J Public Health 2023; 47: 100071.






Open access:
Open access publishing facilitated by The University of Western Australia, as part of the Wiley – the University of Western Australia agreement via the Council of Australian University Librarians.
Ingrid Stacey is supported by a National Health and Medical Research Council Postgraduate Scholarship (2005398) and an ad hoc postgraduate scholarship from the University of Western Australia. Judith Katzenellenbogen holds a Heart Foundation Future Leader Fellowship (102043). The study was a research translation activity by the University of Western Australia and the Western Australian Country Health Service in response to the research findings of ERASE.
No relevant disclosures.