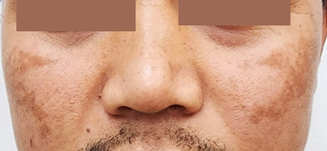
An otherwise healthy man of Southeast‐Asian descent aged in his mid‐30s presented with non‐pruritic hyperpigmented patches involving the face for over 12 months (Figure). Clinically, the findings were consistent with melasma, characterised by brown or dark brown hyperpigmented patches with demarcated or ill‐defined borders, involving the face (zygoma and cheeks) bilaterally. There was no history or clinical features suggestive of diagnoses such as post‐inflammatory hyperpigmentation, drug‐induced pigmentation or photosensitivity, or actinic lichen planus.
Melasma is a common acquired hyperpigmentary condition, described mostly in women of Asian, Middle Eastern or Latin American descent aged 30–50 years.1 Melasma in men is less well recognised,2 with a reported sex ratio of 1:9 (male:female).3 The precise aetiopathogenesis of melasma is incompletely understood. However, there are risk factors related to melasma development, such as sunlight exposure, genetic predisposition, hormonal exposure (contraceptive use and pregnancy), photosensitive medications and cosmetics use, and, rarely, thyroid disorder.2,3,4,5 Melasma can be diagnosed clinically based on distribution and characteristics of pigmentation and skin type or ethnicity; biopsy is rarely required.
Management includes sun protection with the use of a wide‐brim hat and sunscreen (with a sun protection factor of 30 or over), and avoidance of risk factors such as phototoxic drugs, cosmetics, and hormonal contraception (in women). The triple combined topical therapy (hydroquinone 4–5% with tretinoin 0.05–0.1% and low potency corticosteroid), daily for three months, is usually the first line treatment of choice.1,2,3 Adjunct oral tranexamic acid may be considered for extensive lesions, dermal involvement, or for patients refractory to topical therapy, although there are no established studies in men.2 There are also advanced treatment options, such as chemical peeling, microneedling, and light and laser‐based therapies, with unpredictable or mixed results.1,3
- 1. Neagu N, Conforti C, Agozzino M, et al. Melasma treatment: a systematic review. J Dermatolog Treat 2022; 33: 1816‐1837.
- 2. Sarkar R, Ailawadi P, Garg S. Melasma in men: a review of clinical, etiological, and management issues. J Clin Aesthet Dermatol 2018; 11: 53‐59.
- 3. Basit H, Godse KV, Al Aboud AM. Melasma [updated 8 Aug 2023]. In: StatPearls [internet]. Treasure Island (FL): StatPearls Publishing, 2024.
- 4. Majid I, Aleem S. Melasma: update on epidemiology, clinical presentation, assessment, and scoring. J Skin Stem Cell 2021; 8: e120283.
- 5. Doolan BJ, Gupta M. Melasma. Aust J Gen Pract 2021; 50: 880‐885.






Open access:
Open access publishing facilitated by the University of Queensland, as part of the Wiley – the University of Queensland agreement via the Council of Australian University Librarians.
Patient consent:
The patient gave written consent for publication.
No relevant disclosures.