The known: International research indicates that hospital admissions for COVID‐19 are costlier than admissions for other viral pneumonias, but detailed economic analysis from the Australian context has been lacking.
The new: During the original and Delta waves of the pandemic, admissions for COVID‐19 incurred 29% higher costs than those for other viral pneumonias. The costs of admissions that included intensive care were six times higher than those that were managed on general wards.
The implications: Acute COVID‐19 and post‐COVID‐19 condition cases have had a significant financial impact on Australian hospitals. Further analysis is required to identify trends over time in the context of increased vaccination rates and subsequent variants of severe acute respiratory syndrome coronavirus 2.
The emergence of coronavirus disease 2019 (COVID‐19) in late 2019 placed unprecedented and intense pressure on health care systems worldwide. While the financial impacts of the pandemic on health care were described as potentially catastrophic in 2020,1 Australia has fared better than many other jurisdictions due to closure of international borders, local public health policies and high vaccination rates.2 However, the pandemic has and continues to have disruptive and far‐reaching consequences for Australian health services.3 The reporting and contextualisation of the economic consequences of the pandemic are crucial considerations for policy makers, administrators and public health leaders interested in the sustainability of the national health care system and preparation for future pandemics.
While the clinical presentation and outcomes of COVID‐19 have been the subject of significant international research, there have been relatively few economic analyses to date. All available evidence indicates that costs associated with hospitalisation of patients who have COVID‐19 are high in comparison to costs for other patient groups, and there have been calls for additional microeconomic studies of hospital costs to inform sustainable economic strategies into the future.4
A range of mean or median COVID‐19 hospitalisation costs per patient have been reported in the international literature. A Brazilian study of 2020 COVID‐19 admissions reported a mean cost of US$12 637, and found ventilators were the most common cost drivers, but overheads were the main cost component.4,5 The mean hospitalisation cost at a public teaching hospital in Iran was US$271, the majority of which was associated with patient accommodation and nursing workforce costs.6 The median hospitalisation cost in China was reported to be US$2869, and lower costs were associated with treatment using traditional Chinese medicine.7 To our knowledge, no comparable published data from an Australian context have been available to date.
Previous research has consistently shown that hospitalisation costs for patients with COVID‐19 are influenced by demographic and clinical factors. Risk factors for poorer clinical outcomes are also associated with significantly greater costs, some of which are related to higher prevalence of intensive care unit (ICU) admissions. These risk factors include age (particularly ≥ 70 years); underlying hypertension or cardiovascular disease; diabetes; renal disease; rheumatological, haematological and neurological conditions; and pregnancy.5,6,8 Obesity and male sex are also associated with higher additional costs (19.8% and 29.7% respectively) along with comorbid conditions (21.1%).5,7
Currently, there is very little evidence about hospitalisation costs at the individual level for people with post‐COVID‐19 condition (also known as long COVID),9 although there is some population‐level evidence. For example, an analysis on long COVID in the United States estimated that it will cost the US economy US$3.7 trillion from lost earnings, higher spending on health care and lost quality‐adjusted life years (QALYs).10
We aimed to compare health care costs for Australian hospital admissions for patients with COVID‐19 and other viral pneumonias. We also aimed to describe hospital admission costs for patients with post‐COVID‐19 condition.
Methods
We conducted a cost comparison analysis from the health care service perspective, applied to data from the Victorian Admitted Episodes Dataset (VAED) with an analysis period of 1 January 2020 to 30 June 2021. Costs were broken down into direct and indirect costs. Direct costs are expenses associated directly with patient treatment, while indirect costs are shared between patients (eg, overhead costs).11 We compared costs and health care resource use for acute and subacute care for people with COVID‐19 (cases) versus patients admitted for other viral pneumonias (controls), including appropriate stratification for key demographic, ICU admission status and socio‐economic factors. In addition, we separately examined a small dataset of admission costs relating to patients with post‐COVID‐19 condition. We report our findings according to the Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) (Supporting Information, appendix 7).12
Setting and location
The Australian state of Victoria recorded about 3 000 000 COVID‐19 cases to 1 October 2023, which is likely to be an underestimation because of incomplete case ascertainment and the cessation of formal case reporting requirements from October 2022.13 A state of emergency was declared in March 2020 to provide the Chief Health Officer with additional powers, which included lockdowns and travel restrictions during the period of this study.
Study population and comparators
The VAED is a comprehensive administrative dataset of the causes, effects and use of Victorian acute health services, containing de‐identified data for admitted patients in Victorian public and private hospitals.14 The database supports health service reporting, planning and policy formulation, epidemiological research, and public hospital funding under the casemix funding system. All Victorian public and private hospitals — including rehabilitation centres, extended care facilities and day procedure centres — report a minimum set of data for each admitted patient episode.
The VAED includes diagnostic‐related group codes for each admission, which groups patients of similar clinical complexity for funding and other purposes.15 The Victorian Cost Data Collection is a separate dataset of direct and indirect costs and the mix of resources employed for patient care; it was linked to the VAED for this analysis.16 The variables in each dataset are listed in Box 1.
Cases and controls were identified using International Classification of Diseases, tenth revision (ICD‐10) codes17 in linked VAED records. COVID‐19 cases with any of the COVID‐19‐specific codes (Supporting Information, appendix 1) during their admitted episodes were considered hospitalisation due to or with COVID‐19.18 A similar approach was undertaken when identifying controls (viral pneumonia cases) and post‐COVID‐19 condition cases. Briefly, health services initially applied codes related to unspecified viral pneumonia (J18.9) or severe acute respiratory syndrome (SARS) (B97.21) to COVID‐19 cases. However, COVID‐19 specific codes were quickly developed by the World Health Organization to improve data accuracy.19 Post‐COVID‐19 condition was identified using codes U07.3 and U07.4, which were activated and effectively used from 1 January 2021.17
Researchers around the world have grappled with the selection of appropriate controls for COVID‐19 studies.20 As infections by one or more COVID‐19 variants continue to rise globally, it is becoming increasingly difficult to identify people who have never had an infection. For our study, we chose non‐COVID‐19 viral pneumonia as the comparator owing to its similar clinical manifestations to COVID‐19 pneumonia.21
Time horizon
The Victorian Agency for Health Information provided additional linked data regarding the COVID‐19 diagnostic status of people admitted to Victorian hospitals between 1 January 2020 and 31 December 2022, with cost data available from 1 January 2020 to 30 June 2021. The short time horizon of single hospital admissions is appropriate for a cost comparison study; however, post‐discharge costs associated with admissions are not included.
Currency and discount rate
All prices in this analysis are reported in 2021 Australian dollars. Cost data reported in 2020 were adjusted to 2021 values using the Australian Institute of Health and Welfare's final consumption expenditure on hospitals and nursing homes index (1.015 index).22 The exchange rate from Australian dollars to US dollars was based on the 30 June 2021 Reserve Bank of Australia rate of 0.7518.23
Outcome selection and valuation
The variables selected from each dataset were chosen to enable analysis of the admission, clinical, demographic and resource use factors relevant to the cost‐of‐service provision (Box 1).
Analytics, assumptions, rationale and models
Data analysis of every admission episode was undertaken using Stata 16 (StataCorp). Continuous variables are presented as means with standard deviations or as medians with interquartile ranges, as appropriate. Categorical variables are presented as frequencies and percentages. To compare patients between groups, the χ2 test was employed for categorical variables, and the Wilcoxon rank‐sum or t test for continuous variables.24 For cost comparison, we applied a generalised linear regression model with gamma distributions and log link to accommodate the positively skewed cost data.25,26,27 Three models were run:
- model 1 estimated the costs associated with patients diagnosed with any COVID‐19 and those diagnosed with viral pneumonia;
- model 2 estimated the costs associated with patients diagnosed with COVID‐19 pneumonia and those diagnosed with viral pneumonia; and
- model 3 estimated the costs associated with patients diagnosed with post‐COVID‐19 condition.
In each model, admission costs were defined as the outcome variable with dummy variables created for models 1 and 2 to identify patients with any COVID‐19, COVID‐19 pneumonia or viral pneumonia, from which the cost ratio was derived. Multiple admissions were accounted for using cluster robust standard errors, and hospital transfers were considered covariates. This modelling approach established the key drivers influencing patient costs, including variables that were deemed relevant or demonstrated a significant impact on admission costs (P < 0.05) assessed through univariable linear regression. These variables (eg, length of stay, admission source and others) are outlined in detail in the Supporting Information, appendix 2. Due to the exploratory nature of this analysis, the Bonferroni test was performed to control the overall type I error rate. Multivariable results are presented as relative costs with 95% confidence intervals (CIs).
Ethics approval
Ethics approval was obtained for this study from the Deakin University Human Research Ethics Committee (2023‐080, 24 April 2023).
Results
Study parameters
Between 1 January 2020 and 30 June 2021, cost data were available for 2 607 080 admissions. As shown in Box 2, 3197 (0.1%) of the costed admissions were due to COVID‐19 and 15 761 (0.6%) were due to viral pneumonia. Of the 3012 COVID‐19 admissions not deemed to be due to post‐COVID‐19 condition, 1158 (38.4%) were identified as being due to COVID‐19 pneumonia.
Significant demographic differences were identified between COVID‐19 and viral pneumonia admissions (Box 3). Compared with patients who had COVID‐19, a larger proportion of patients with viral pneumonia were aged 60 years or older (12 080 [77%] v 1728 [57%]; P < 0.001), males (8858 [56%] v 1440 [48%]; P < 0.001), born in Australia (9653 [62%] v 1443 [49%]; P < 0.001), English speakers (13 647 [87%] v 2410 [81%]; P < 0.001), and treated in private hospitals (1981 [13%] v 169 [6%]; P < 0.001). Meanwhile, a significantly higher proportion of patients admitted with any COVID‐19 had a caregiver compared with those admitted with viral pneumonia (28 [58%] v 46 [38%]; P = 0.010). No differences between groups were identified for interpreter requirements. Patients experiencing post‐COVID‐19 conditions were identified across all adult age groups, with a mean age of 57 years (standard deviation [SD], 23 years).
In most COVID‐19 cases, the patients had been admitted from their private residence (2252, 75%) via emergency admission (1983, 66%). A small percentage of these patients had been transferred from aged care facilities, accounting for 284 COVID‐19 cases overall (9%) and 799 of other viral pneumonias (5%). Meanwhile, more than half of the 185 identified post‐COVID‐19 condition cases involved patients being sent via emergency admission (108, 58%), and most of the others involved patients arriving via elective admission (58, 31%). Moreover, in 74 post‐COVID‐19 condition admissions (40%), patients received a secondary clinical complexity grading. A detailed overview of hospital admissions data for all case groups is provided in the Supporting Information, appendix 3.
In terms of clinical outcomes, a marked difference was observed between COVID‐19 and viral pneumonia cases (Box 4). Admission to an ICU and use of subacute care were both more common for cases in which patients were diagnosed with COVID‐19 pneumonia (248 [21%] and 63 [5%] respectively) compared with cases in which patients were diagnosed with viral pneumonia (2375 [15%] and 379 [2%] respectively). Moreover, resource use for patients with COVID‐19 pneumonia was significantly higher than for patients with viral pneumonia: intensive care, 9.6 days v 4.6 days; and mechanical ventilation, 11.6 days v 4.6 days. In addition, a lower proportion of patients with COVID‐19 pneumonia survived compared with patients with viral pneumonia (938 [81%] v 14 657 [93%]).
Box 5 and Box 6 summarise the unadjusted (crude) and adjusted (based on the multivariable generalised linear regression model) total, direct and indirect admission episode costs for any COVID‐19 and COVID‐19 pneumonia, consistently showing higher costs compared with other viral pneumonias. After controlling for variables, compared with viral pneumonia admissions, any COVID‐19 admissions cost an additional 29% (95% CI, 26–33%) and COVID‐19 pneumonia admissions cost an additional 41% (95% CI, 35–47%) (P < 0.001 for both). The total adjusted cost of any COVID‐19 admission was A$27 263 (95% CI, A$25 559–A$28 966) or US$20 496 (95% CI, US$19 216–US$ 21 777), while the total adjusted cost of COVID‐19 pneumonia admissions was A$30 261 (95% CI, A$27 752–A$32 769) or US$22 750 (95% CI, US$20 864–US$24 636). The highest unadjusted cost categories for any COVID‐19 admissions, COVID‐19 pneumonia admissions and viral pneumonia admissions were direct ICU, nursing and medical costs (Supporting Information, appendices 4 and 5). When COVID‐19 admissions were stratified according to ICU admission status, the unadjusted mean total cost was six times higher for admissions including intensive care compared with those not requiring intensive care, and this difference was statistically significant (A$120 504 [SD, A$264 533] or US$90 595 [SD, US$198 876] v A$19 634 [SD, A$29 597] or US$14 761 [SD, US$22 251]) (Supporting Information, appendix 6).
For post‐COVID‐19 condition cases, the total adjusted cost was A$11 090 (95% CI, A$10 252–A$11 928) or US$8337 (95% CI, US$7707–US$8967) (Box 7). The highest mean unadjusted cost categories for post‐COVID‐19 condition cases were direct nursing, medical, theatre and ICU costs.
Discussion
In this study, we aimed to compare hospital admission costs for people with COVID‐19 and people with other viral pneumonias, and describe the admission episode cost for people with post‐COVID‐19 condition. The findings confirm that cases of COVID‐19 incurred higher admissions costs than cases of other viral pneumonias. A key contributor to these higher costs was the more complex care needed for people with COVID‐19, as indicated by longer lengths of stay and by greater ICU and mechanical ventilation hours.28 COVID‐19 is a multisystem syndrome, and these greater costs may reflect a higher need for multidisciplinary intervention.
The significant contribution of intensive care costs to total admission costs has also been noted in previous research. In an analysis of COVID‐19 admissions to private hospitals, it was found that admissions requiring intensive care cost more than double when compared with general ward admissions, and it was noted that a small number of high‐cost cases had a disproportionate impact on overall mean costs.29 Encouragingly, the proportion of Australian COVID‐19 cases requiring ICU admissions continues to decline (from 20% in September 2021 to 2% in July 2022),30 and the mean length of stay for all COVID‐19 cases has also decreased.31 In addition, evidence suggesting that Omicron variant cases have a lower risk of post‐COVID‐19 condition is also beginning to emerge.32
Many of the findings of this study are similar to those of international studies, such as the heavy contribution of direct costs across all case groups.33,34 However, the mean length of stay for COVID‐19 cases was shorter than the 15.4 days reported across international studies,35 in which the intensive care portion of admission was longer than the median of six days reported in another Australian study.36 The very low allied health costs associated with post‐COVID‐19 condition admissions was unexpected, given the key role allied health professionals play in the management of sustained symptoms.3 This could suggest that these resources were underutilised at the time of data collection.
Along with individual patient factors, contextual factors within health care systems (such as access demands and the availability of suitable discharge destinations) have an important influence on hospital admission costs. A greater understanding of context enhances decision making around resource allocation and policy and would be supported by further economic analysis in other Australian jurisdictions.
Our analysis had several limitations, which may affect internal validity and generalisability. It only included cost data on admissions between 1 January 2020 to 30 June 2021; therefore, analysis outside this period is not possible. This limitation could affect hospital stay costs and associated costs, given that the data mostly included people who were not fully vaccinated against COVID‐19.37
Moreover, the impacts of the changes in Victorian hospital activities (eg, a decrease in the number of acute, subacute, non‐acute and emergency department separations from pre‐pandemic levels to pandemic period levels) were not accounted for. However, despite the marked changes in hospital activities, the mean cost per separation did not significantly change from financial year 2016–17 to 2021–22: 2016–17, A$4156; 2017–18, A$4282; 2018–19, A$4505; 2019–20, A$4919; 2020–21, A$5214; 2021–22, A$5573.38,39
Hospitalisations may have been included as COVID‐19 cases where COVID‐19 was incidental and either asymptomatic or not related to the reason for the admission. Relatively few post‐COVID‐19 condition cases were identified, probably due to the relative recency of an ICD‐10 code for this condition (introduced on 1 October 2021) and the challenges associated with identifying this condition on a background of pre‐existing conditions. The data for post‐COVID‐19 condition reflect costs following an initial COVID‐19 diagnosis and therefore describe a distinctively different clinical scenario to data for the other COVID‐19 groups. Other post‐viral conditions with similar presentations may also have been present among the cases but are not identified in current coding systems.
Analysis of costs was hampered by limited data or lack of data for particular categories — including patients from a refugee background, patients with an Indigenous background, vaccination status of patients, models of care, COVID‐19‐burdened hospitals, viral mutations, COVID‐19 severity, treatment advances, and socio‐economic factors — which could affect admission costs. Owing to data constraints, it was challenging to control for these variations in our model. The Charlson comorbidity index was used to adjust for potential confounding factors for patients with comorbid conditions, similar to the approach used in previous studies.40,41 However, comorbid conditions not captured by this index represent another limitation of this research.
Further studies are required to understand long term costs; provide insights on differential costs by certain demographics, variance and categories that could further affect costs; identify trends over time or variation across different periods of the epidemic, and across public health and hospital emergency response levels; and understand the impact of differing health system contexts across jurisdictions.
To our knowledge, our study provides the first analysis of COVID‐19 hospital costs in Australia and underscores the impact of this novel and complex disease on our health care system. Given its recent emergence, both acute COVID‐19 and post‐COVID‐19 condition cases make a significant additional financial impact on Australian hospitals. The proportion of COVID‐19 admissions involving costly intensive care has reduced as treatment has improved,42 and is now comparable to that for viral pneumonia cases.43 However, COVID‐19 has introduced an additional and significant caseload to the health care system, diverting resources from other areas of the system. It is also possible that the diagnostic‐related groups for COVID‐19 infections do not fully reflect the complexity of these admissions, which could contribute to funding shortfalls for health services.
Box 1 – Selected variables and outcomes included in the Victorian Admitted Episodes Dataset and Victorian Cost Data Collection
|
Category |
Variables |
||||||||||||||
|
|
|||||||||||||||
|
Admission |
Admission date, admission source, care type, admission unit, discharging unit, intensive care unit hours (including ventilation hours), length of stay, program, separation accommodation, separation date, type of specialist, and separation mode. Clinical complexity was also provided in the Victorian Admitted Episodes Dataset, which categorised episodes into four categories: primary (least complexity), secondary, tertiary (most complexity) and undefined. |
||||||||||||||
|
Clinical |
Australian national subacute and non‐acute patient classification, diagnoses (including number and ICD‐10 codes), functional independence measure score, admission and separation (for subacute admissions), impairment, and onset date. |
||||||||||||||
|
Demographic |
Accommodation type, ambulatory care‐sensitive conditions, birth date, carer availability, country of birth, flagged comorbid conditions (Charlson Comorbidity Index score), sex, health insurance status, Indigenous status, interpreter required, locality, marital status, postcode, preferred language, public or private hospital, and refugee status. |
||||||||||||||
|
Resources |
Co‐payments, diagnostic‐related groups and weighted inlier equivalent separations. |
||||||||||||||
|
Direct costs: allied health, intensive care unit, medical (including non‐surgical costs), medical supplies, surgical (including surgical costs), nursing (including supplies), national blood authority, other, pathology, pharmacy, post‐natal domiciliary care, operating room prostheses, theatre, and total costs. |
|||||||||||||||
|
Indirect costs: all the above plus administration, coronary care unit, associated costs for an admission involving COVID‐19, emergency department, imaging, and hospital in the home. |
|||||||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; ICD‐10 = International Classification of Diseases, tenth revision. |
|||||||||||||||
Box 2 – Analysed admission episodes by group
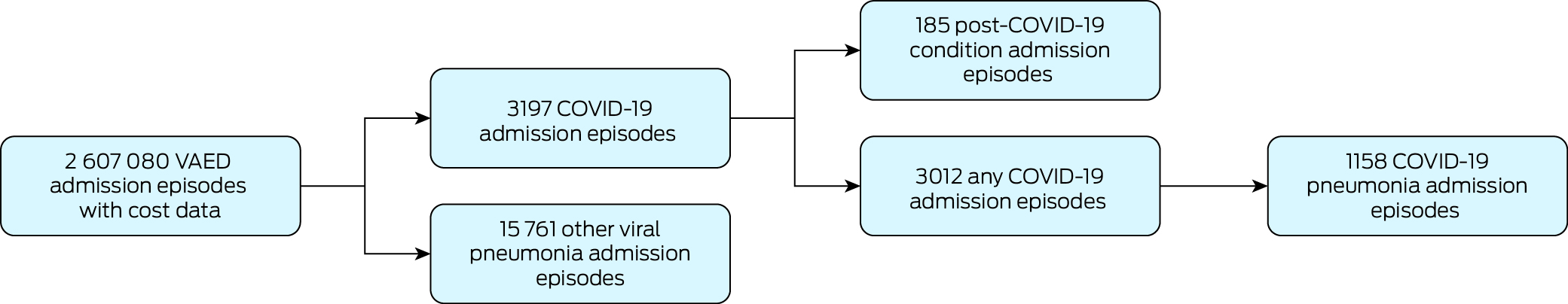
COVID‐19 = coronavirus disease 2019. VAED = Victorian Admitted Episodes Dataset.
Box 3 – Demographic characteristics of patients included in the admissions data that were used for the analysis*
|
Characteristic |
Viral pneumonia (n = 15 761) |
Any COVID‐19 (n = 3012) |
P value for viral pneumonia v any COVID‐19 |
COVID‐19 pneumonia (n = 1158) |
P value for viral pneumonia v COVID‐19 pneumonia |
Post‐COVID‐19 condition (n = 185) |
|||||||||
|
|
|||||||||||||||
|
Age group |
|
|
< 0.001 |
|
< 0.001 |
|
|||||||||
|
0–18 years |
760 (5%) |
105 (3%) |
|
6 (1%) |
|
8 (4%) |
|||||||||
|
19–39 years |
779 (5%) |
488 (16%) |
|
114 (10%) |
|
42 (23%) |
|||||||||
|
40–59 years |
2142 (14%) |
691 (23%) |
|
282 (24%) |
|
42 (23%) |
|||||||||
|
60–79 years |
5894 (37%) |
864 (29%) |
|
414 (36%) |
|
53 (29%) |
|||||||||
|
≥ 80 years |
6186 (39%) |
864 (29%) |
|
342 (30%) |
|
40 (22%) |
|||||||||
|
Sex |
|
|
< 0.001 |
|
0.233 |
|
|||||||||
|
Male |
8858 (56%) |
1440 (48%) |
|
630 (54%) |
|
91 (49%) |
|||||||||
|
Female |
6902 (44%) |
1572 (52%) |
|
528 (46%) |
|
94 (51%) |
|||||||||
|
Marital status† |
|
|
0.428 |
|
< 0.001 |
|
|||||||||
|
Married |
7655 (49%) |
1419 (50%) |
|
645 (59%) |
|
85 (47%) |
|||||||||
|
Unmarried |
7835 (51%) |
1406 (50%) |
|
450 (41%) |
|
97 (53%) |
|||||||||
|
Country of birth |
|
|
< 0.001 |
|
< 0.001 |
|
|||||||||
|
Not Australia |
5981 (38%) |
1490 (51%) |
|
656 (58%) |
|
75 (41%) |
|||||||||
|
Australia |
9653 (62%) |
1443 (49%) |
|
469 (42%) |
|
107 (59%) |
|||||||||
|
Indigenous |
|
|
0.004 |
|
0.004 |
|
|||||||||
|
Indigenous |
215 (1%) |
21 (1%) |
|
≤ 5 (0.4%) |
|
≤ 5 (2%) |
|||||||||
|
Not Indigenous |
15 380 (99%) |
2891 (99%) |
|
1121 (99.6%) |
|
178 (98%) |
|||||||||
|
Preferred language |
|
|
< 0.001 |
|
< 0.001 |
|
|||||||||
|
English |
13 647 (87%) |
2410 (81%) |
|
877 (76%) |
|
157 (85%) |
|||||||||
|
Not English |
2098 (13%) |
579 (19%) |
|
274 (24%) |
|
28 (15%) |
|||||||||
|
Interpreter‡ |
|
|
0.493 |
|
0.617 |
|
|||||||||
|
Not needed |
433 (21%) |
112 (19%) |
|
53 (19%) |
|
≤ 5 (11%) |
|||||||||
|
Needed |
1665 (79%) |
467 (81%) |
|
221 (81%) |
|
25 (89%) |
|||||||||
|
Patient type§ |
|
|
< 0.001 |
|
< 0.001 |
|
|||||||||
|
Public |
13 367 (87%) |
2770 (94%) |
|
1071 (95%) |
|
160 (92%) |
|||||||||
|
Private |
1981 (13%) |
169 (6%) |
|
61 (5%) |
|
14 (8%) |
|||||||||
|
Refugee |
|
|
0.536 |
|
0.701 |
|
|||||||||
|
Patient is a refugee |
≤ 5 (0.01%) |
0 |
|
0 |
|
0 |
|||||||||
|
Patient is not a refugee |
15 759 (100%) |
3012 (100%) |
|
1158 (100%) |
|
185 (100%) |
|||||||||
|
Care availability¶ |
|
|
0.010 |
|
0.078 |
|
|||||||||
|
Carer not needed or not applicable |
39 (32%) |
6 (13%) |
|
3 (14%) |
|
3 (50%) |
|||||||||
|
Has a carer |
46 (38%) |
28 (58%) |
|
8 (38%) |
|
3 (50%) |
|||||||||
|
Has no carer |
29 (24%) |
14 (29%) |
|
10 (48%) |
|
0 |
|||||||||
|
Lives in a mutually dependent situation |
7 (6%) |
0 |
|
0 |
|
0 |
|||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019. * Pearson χ2 test was performed and P < 0.05 was considered statistically significant; data shown exclude answers that were categorised as not stated or unallocated; data for cells showing ≤ 5 patients have been suppressed for confidentiality reasons. † Marital status indicated as married includes de facto and married; marital status indicated as unmarried includes divorced, never married, partnered, separated, single and widowed. ‡ Interpreter data only includes episodes with English as not the preferred language. § Data for patient types (separation patient type) categorised as compensable, Department of Veterans’ Affairs or “ineligible” are not presented in this table but are included in the analysis, and the admissions that fell into these categories made up less than 5% of the overall study population. ¶ Carer data presented in this table exclude episodes with missing data. |
|||||||||||||||
Box 4 – Clinical outcomes of the admissions inluded on our analysis*
|
Outcomes |
Viral pneumonia (n = 15 761) |
Any COVID‐19 (n = 3012) |
P value for viral pneumonia v any COVID‐19 |
COVID‐19 pneumonia (n = 1158) |
P value for viral pneumonia v COVID‐19 pneumonia |
Post‐COVID‐19 condition (n = 185) |
|||||||||
|
|
|||||||||||||||
|
Receiving subacute services,† n (%) |
379 (2%) |
275 (9%) |
< 0.001 |
63 (5%) |
< 0.001 |
15 (8%) |
|||||||||
|
Admitted to ICU, n (%) |
2375 (15%) |
347 (12%) |
< 0.001 |
248 (21%) |
< 0.001 |
16 (9%) |
|||||||||
|
Survived, n (%) |
14 657 (93%) |
2634 (87%) |
< 0.001 |
938 (81%) |
< 0.001 |
177 (96%) |
|||||||||
|
Mechanical ventilation, n (%) |
734 (5%) |
174 (6%) |
0.009 |
139 (12%) |
< 0.001 |
≤ 5 (< 3%) |
|||||||||
|
Non‐invasive ventilation, n (%) |
545 (3%) |
55 (2%) |
< 0.001 |
46 (4%) |
0.196 |
≤ 5 (< 3%) |
|||||||||
|
Length of stay in days, mean (SD) |
8 (12) |
11 (14) |
< 0.001 |
12 (14) |
< 0.001 |
6 (8) |
|||||||||
|
ICU hours,‡ mean (SD) |
110 (163) |
212 (336) |
< 0.001 |
231 (364) |
< 0.001 |
44 (32) |
|||||||||
|
Mechanical ventilation hours,§ mean (SD) |
111 (179) |
263 (381) |
< 0.001 |
280 (409) |
< 0.001 |
69 (83) |
|||||||||
|
Non‐invasive ventilation hours,¶ mean (SD) |
23 (40) |
14 (21) |
0.103 |
15 (22) |
0.163 |
14 (17) |
|||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; ICU = intensive care unit; SD = standard deviation. * Data for cells showing ≤ 5 patients have been suppressed for confidentiality reasons. † Data derived from availability of the functional independence measure score. ‡ Among episodes with ICU admissions; data derived from availability of direct ICU costs. § Among episodes with mechanical ventilation; data derived from availability of direct ICU costs. ¶ Among episodes with non‐invasive ventilation; data derived from availability of direct ICU costs. |
|||||||||||||||
Box 5 – Any COVID‐19 versus viral pneumonia admission costs
|
|
Any COVID‐19 admission costs |
Viral pneumonia admission costs |
Cost ratio (95% CI)* |
P |
|||||||||||
|
|
|||||||||||||||
|
Total cost |
|
|
|
|
|||||||||||
|
Crude median (IQR) |
A$11 935 (A$3742–A$31 223) |
A$8762 (A$4318–A$19 824) |
– |
|
|||||||||||
|
Crude mean (95% CI) |
A$31 254 (A$27 708–A$34 801) |
A$18 522 (A$17 958–A$19 085) |
– |
|
|||||||||||
|
Adjusted mean (95% CI)† |
A$27 263 (A$25 559–A$28 966) |
A$21 071 (A$19 812–A$22 331) |
1.29 (1.26–1.33) |
< 0.001 |
|||||||||||
|
Direct costs |
|
|
|
|
|||||||||||
|
Crude median (IQR) |
A$9798 (A$3001–A$25 997) |
A$6959 (A$3434–A$15 885) |
– |
|
|||||||||||
|
Crude mean (95% CI) |
A$26 803 (A$23 542–A$30 064) |
A$15 015 (A$14 547–A$15 483) |
– |
|
|||||||||||
|
Adjusted mean (95% CI)† |
A$23 533 (A$21 880–A$25 187) |
A$17 293 (A$16 125–A$18 460) |
1.36 (1.32–1.4) |
< 0.001 |
|||||||||||
|
Indirect costs |
|
|
|
|
|||||||||||
|
Crude median (IQR) |
A$1776 (A$584–A$4571) |
A$1751 (A$798–A$3908)‡ |
– |
|
|||||||||||
|
Crude mean (95% CI) |
A$4451 (A$4122–A$4780) |
A$3507 (A$3404–A$3610) |
– |
|
|||||||||||
|
Adjusted mean (95% CI)† |
A$3816 (A$3669–A$3963) |
A$3791 (A$3666–A$3916) |
1.01 (0.98–1.04) |
0.667‡ |
|||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; IQR = interquartile range; VicDRG = Victorian diagnosis‐related group. * Viral pneumonia is the reference. † Adjusted costs were derived from a multivariable generalised linear model that accounted for key confounding variables including admission source, care type, country of birth, ambulatory care‐sensitive condition, Charlson comorbidity index score, number of diagnoses, sex, hospital insurance level, intensive care hours, length of stay, mechanical ventilation hours, non‐invasive ventilation hours, separation accommodation type, VicDRG level, VicDRG type, VicDRG specialty, subacute care, age group, lockdown, use of intensive care unit, and survival. ‡ Most adjusted mean costs exhibited statistical significance in the generalised linear model except for the indirect cost measurements. To compare the mean crude costs between groups, a t test was employed, revealing statistically significant differences in all crude cost measurements. To compare the median crude costs between groups, a Wilcoxon rank‐sum test was employed, revealing statistically significant differences in most crude cost measurements except for the comparison of any COVID‐19 versus viral pneumonia indirect median cost. |
|||||||||||||||
Box 6 – COVID‐19 pneumonia versus viral pneumonia admission costs
|
|
COVID‐19 pneumonia admission costs |
Viral pneumonia admission costs |
Cost ratio (95% CI)* |
P |
|||||||||||
|
|
|||||||||||||||
|
Total cost |
|
|
|
|
|||||||||||
|
Crude median (IQR) |
A$18 278 (A$7140–A$44 800) |
A$8762 (A$4318–A$19 824) |
– |
|
|||||||||||
|
Crude mean (95% CI) |
A$47 900 (A$39 226–A$56 574) |
A$18 522 (A$17 958–A$19 085) |
– |
|
|||||||||||
|
Adjusted mean (95% CI)† |
A$30 261 (A$27 752–A$32 769) |
A$21 529 (A$19 855–A$23 202) |
1.41 (1.35–1.47) |
< 0.001 |
|||||||||||
|
Direct cost |
|
|
|
|
|||||||||||
|
Crude median (IQR) |
A$15 158 (A$5757–A$38 821) |
A$6959 (A$3434–A$15 885) |
– |
|
|||||||||||
|
Crude mean (95% CI) |
A$41 925 (A$33 884–A$49 966) |
A$15 015 (A$14 547–A$15 483) |
– |
|
|||||||||||
|
Adjusted mean (95% CI)† |
A$26 375 (A$23 906–A$28 844) |
A$17 733 (A$16 164–A$19 301) |
1.49 (1.42–1.56) |
< 0.001 |
|||||||||||
|
Indirect cost |
|
|
|
|
|||||||||||
|
Crude median (IQR) |
A$2778 (A$1208–A$6379) |
A$1751 (A$798–A$3908) |
– |
|
|||||||||||
|
Crude mean (95% CI) |
A$5975 (A$5292–A$6659) |
A$3507 (A$3404–A$3610) |
– |
|
|||||||||||
|
Adjusted mean (95% CI)† |
A$4045 (A$3841–A$4248) |
A$3809 (A$3658–A$3959) |
1.06 (1.02–1.11) |
0.004 |
|||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; IQR = interquartile range; VicDRG = Victorian diagnosis‐related group. * Viral pneumonia is the reference. † The adjusted costs were derived from a multivariable generalised linear model that accounted for key confounding variables including admission source, care type, country of birth, ambulatory care‐sensitive condition, Charlson comorbidity index score, number of diagnoses, sex, hospital insurance level, intensive care hours, length of stay, mechanical ventilation hours, non‐invasive ventilation hours, separation accommodation type, VicDRG level, VicDRG type, VicDRG specialty, subacute care, age group, lockdown, use of intensive care unit, and survival. All adjusted mean costs exhibited statistical significance in the generalised linear model. To compare the mean crude costs between groups, a t test was employed, revealing statistically significant differences in all crude cost measurements. To compare the median crude costs between groups, a Wilcoxon rank‐sum test was employed, revealing statistically significant differences in all crude cost measurements. |
|||||||||||||||
Box 7 – Post‐COVID‐19 condition admission costs
|
|
Post‐COVID‐19 condition admission costs |
||||||||||||||
|
|
|||||||||||||||
|
Total cost |
|
||||||||||||||
|
Crude median (IQR) |
A$5156 (A$1854–A$13 401) |
||||||||||||||
|
Crude mean (95% CI) |
A$11 202 (A$8639–A$13 765) |
||||||||||||||
|
Adjusted mean (95% CI)* |
A$11 090 (A$10 252–A$11 928) |
||||||||||||||
|
Direct costs |
|
||||||||||||||
|
Crude median (IQR) |
A$3925 (A$1506–A$10 190) |
||||||||||||||
|
Crude mean (95% CI) |
A$8940 (A$6917–A$10 962) |
||||||||||||||
|
Adjusted mean, 95% CI)* |
A$8848 (A$8166–A$9530) |
||||||||||||||
|
Indirect costs |
|
||||||||||||||
|
Crude median (IQR) |
A$1067 (A$347–A$2588) |
||||||||||||||
|
Crude mean (95% CI) |
A$2262 (A$1706–A$2818) |
||||||||||||||
|
Adjusted mean (95% CI)* |
A$2252 (A$2058–A$2446) |
||||||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; IQR = interquartile range. * The adjusted costs were derived from a multivariable generalised linear model that accounted for key confounding variables including Charlson comorbidity index score, number of diagnoses, sex, hospital insurance level, intensive care hours, length of stay, separation accommodation type, Victorian diagnosis‐related group level, age group, use of intensive care unit, survival, and patient type. All adjusted mean costs exhibited statistical significance in the generalised linear model. |
|||||||||||||||
Received 22 January 2024, accepted 27 August 2024
- Danielle Hitch1,2
- Mary Rose Angeles1
- Eric Lau1
- Kelli Nicola‐Richmond1
- Catherine Bennett1
- Catherine M Said2,3
- Sara Holton1,2
- Kimberley Haines2
- Bodil Rasmussen1
- Genevieve Pepin1
- Kieva Richards1
- Martin Hensher4
- 1 Deakin University, Geelong, VIC
- 2 Western Health, Melbourne, VIC
- 3 University of Melbourne, Melbourne, VIC
- 4 University of Tasmania, Hobart, TAS
Open access:
Open access publishing facilitated by Deakin University, as part of the Wiley ‐ Deakin University agreement via the Council of Australian University Librarians.
Data Sharing:
Data used in this study are protected under the privacy policy of the Victorian Government Department of Health. We have signed a deed of confidentiality that prevents us from sharing the data.
This study was supported by a Category 1 Seed Funding Grant from Deakin University's School of Health and Social Development and Institute for Health Transformation. Data for this study were accessed with the kind permission of the Victorian Agency for Health Information (VAHI).
This study was supported by a Category 1 Seed Funding Grant from Deakin University's School of Health and Social Development and Institute for Health Transformation. We were independent from the funder's decisions and allocation of grants.
- 1. Kaye AD, Okeagu CN, Pham AD, et al. Economic impact of COVID‐19 pandemic on healthcare facilities and systems: international perspectives. Best Pract Res Clin Anaesthesiol 2021; 35: 293‐306.
- 2. Basseal J, Bennett C, Collignon P, et al. Key lessons from the COVID‐19 public health response in Australia. Lancet Reg Health West Pac 2022; 30: 100616.
- 3. House of Representatives Standing Committee on Health, Aged Care and Sport. Sick and tired: casting a long shadow. Inquiry into long COVID and repeated COVID infections. Canberra: Commonwealth of Australia, 2023. https://www.aph.gov.au/Parliamentary_Business/Committees/House/Health_Aged_Care_and_Sport/LongandrepeatedCOVID/Report (viewed Jan 2024).
- 4. Beck da Silva Etges AP, Bertoglio Cardoso R, Marcolino MS, et al. The economic impact of COVID‐19 treatment at a hospital‐level: investment and financial registers of Brazilian hospitals. J Health Econ Outcomes Res 2021; 8: 36‐41.
- 5. Miethke‐Morais A, Cassenote A, Piva H, et al. COVID‐19‐related hospital cost‐outcome analysis: the impact of clinical and demographic factors. Braz J Infect Dis 2021; 25: 101609.
- 6. Aghajani M, Sistanizad M, Toloui A, et al. COVID‐19 related hospitalization costs; assessment of influencing factors. Front Emerg Med 2021; 6: e3.
- 7. Dong M, Yang Z, Chen Y, et al. Hospitalization costs of COVID‐19 cases and their associated factors in Guangdong, China: a cross‐sectional study. Front Med (Lausanne) 2021; 8: 655231.
- 8. Esteban EMA, Ares AC, Rodríguez MJD. Increased healthcare costs in COVID‐19 patients with unhealthy habits: the case of smoking. Tob Induc Dis 2023; 21: 82.
- 9. Katz GM, Bach K, Bobos P, et al. Understanding how post‐COVID‐19 condition affects adults and health care systems. JAMA Health Forum 2023; 4: e231933.
- 10. Cutler DM. The economic cost of long COVID: an update. Cambridge: Harvard University, 2022. https://scholar.harvard.edu/files/cutler/files/long_covid_update_7‐22.pdf (viewed Sept 2023).
- 11. Victorian Government Department of Health. Victorian Cost Data Collection (VCDC). https://www.health.vic.gov.au/publications/vcdc‐deriving‐cost‐buckets (viewed Sept 2023).
- 12. Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. BMC Med 2022; 20: 23.
- 13. Lucas C, Ilanbey S. Mandatory testing to end along with forced COVID‐19 isolation. The Age (Melbourne), 9 Oct 2022. https://www.theage.com.au/politics/victoria/mandatory‐testing‐to‐end‐along‐with‐forced‐covid‐19‐isolation‐20221008‐p5bo8d.html (viewed Oct 2022).
- 14. Victorian Government Department of Health. Victorian Admitted Episodes Dataset (VAED) manual 2022–2023. https://www.health.vic.gov.au/publications/victorian‐admitted‐episodes‐dataset‐manual‐2022‐2023 (viewed Sept 2023).
- 15. Suleiman M, Demirhan H, Boyd L, et al. Incorporation of expert knowledge in the statistical detection of diagnosis related group misclassification. Int J Med Inform 2020; 136: 104086.
- 16. Centre for Victorian Data Linkage. Datasets available in the Centre for Victorian Data Linkage's Integrated Data Resource. https://vahi.vic.gov.au/sites/default/files/2023‐07/datasets‐available‐in‐the‐centre‐for‐victorian‐data‐linkages‐integrated‐data‐resource.docx (viewed Sept 2023).
- 17. World Health Organization. ICD‐10: international statistical classification of diseases and related health problems: tenth revision, 2nd ed. WHO, 2004. https://iris.who.int/handle/10665/42980 (viewed Sept 2024).
- 18. Rowe SL, Leder K, Dyson K, et al. Associations between COVID‐19 and hospitalisation with respiratory and non‐respiratory conditions: a record linkage study. Med J Aust 2023; 218: 33‐39. https://www.mja.com.au/journal/2023/218/1/associations‐between‐covid‐19‐and‐hospitalisation‐respiratory‐and‐non
- 19. Independent Health and Aged Care Pricing Authority. How to classify COVID‐19: guidance for data analysts using ICD‐10‐AM eleventh edition. Sydney: IHACPA, 2022. https://www.ihacpa.gov.au/sites/default/files/2022‐12/How%20to%20classify%20COVID‐19%20%E2%80%93%20Guidance%20for%20data%20analysts%20using%20ICD‐10‐AM%20Eleventh%20Edition.PDF (viewed Sept 2023).
- 20. Høeg T, Ladhani S, Prasad C. How methodological pitfalls have created widespread misunderstanding about long COVID. BMJ Evid Based Med 2024; 29: 142‐146.
- 21. Eslambolchi A, Maliglig A, Gupta A, Gholamrezanezhad A. COVID‐19 or non‐COVID viral pneumonia: how to differentiate based on the radiologic findings? World J Radiol 2020; 12: 289‐301.
- 22. Australian Institute of Health and Welfare. Health expenditure Australia 2020–21 [web report]. Canberra: AIHW, 2022. https://www.aihw.gov.au/reports/health‐welfare‐expenditure/health‐expenditure‐australia‐2020‐21/data (viewed Jan 2024).
- 23. Reserve Bank of Australia. Exchange rates. https://www.rba.gov.au/statistics/frequency/exchange‐rates.html (viewed Dec 2023).
- 24. Field A. An adventure in statistics: the reality enigma. Sage Publications, 2016.
- 25. Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic evaluation in clinical trials. 2nd ed. Oxford: Oxford University Press, 2014.
- 26. Zhou J, Williams C, Keng MJ, et al. Estimating costs associated with disease model states using generalized linear models: a tutorial. Pharmacoeconomics 2024; 42: 261‐273.
- 27. Malehi AS, Pourmotahari F, Angali KA. Statistical models for the analysis of skewed healthcare cost data: a simulation study. Health Econ Rev 2015; 5: 11.
- 28. Johnson C, Subramanianm A, Orosz J, et al. Intensive care admissions following rapid response team reviews in patients with COVID‐19 in Australia. Crit Care Resusc 2022; 24: 106‐115.
- 29. Wagner E, Claxton G, Amin K, Cox C. Cost of COVID‐19 hospital admissions among people with private health coverage. 14 Nov 2022. https://www.kff.org/coronavirus‐covid‐19/issue‐brief/cost‐of‐covid‐19‐hospital‐admissions‐among‐people‐with‐private‐health‐coverage (viewed Dec 2023).
- 30. Read M. COVID‐19 hospital admissions hit record high, but cases peak in sight. Financial Review, 25 July 2022. https://www.afr.com/politics/covid‐19‐hospital‐admissions‐hit‐record‐high‐but‐case‐peak‐in‐sight‐20220725‐p5b4be (viewed July 2022).
- 31. Tobin RJ, Wood JG, Jayasundara D, et al. Real‐time analysis of hospital length of stay in a mixed SARS‐CoV‐2 Omicron and Delta epidemic in New South Wales, Australia. BMC Infect Dis 2023; 23: 28.
- 32. Antonelli M, Pujol J, Spector T, et al. Risk of long COVID associated with Delta versus Omicron variants of SARS‐CoV‐2. Lancet 2022; 399: 2263‐2264.
- 33. Seringa J, Pedreiras S, Freitas MJ, et al. Direct costs of COVID‐19 inpatient admissions in a Portuguese tertiary care university centre. Port J Public Health 2022; 40: 26‐34.
- 34. Newall A, Schuffham P, Hodgkinson B. Economic report into the cost of influenza to the Australian health system: report to the Influenza Specialist Group. 2007. https://isg.org.au/assets/assets/isg‐cost‐influenza‐report‐30‐2007.pdf (viewed Jan 2024).
- 35. Alimohamadi Y, Yekta EM, Sepandi M, et al. Hospital length of stay for COVID‐19 patients: a systematic review and meta‐analysis. Multidiscip Respir Med 2022; 17: 856.
- 36. Burrell A, Pellegrini B, Salimi F, et al. Outcomes for patients with COVID‐19 admitted to Australian intensive care units during the first four months of the pandemic. Med J Aust 2021; 214: 23‐30. https://www.mja.com.au/journal/2021/214/1/outcomes‐patients‐covid‐19‐admitted‐australian‐intensive‐care‐units‐during‐first
- 37. Australian National Audit Office. Australia's COVID‐19 vaccine rollout 2022. https://www.anao.gov.au/sites/default/files/2022‐10/Auditor‐General_Report_2022‐23_3_0.pdf (viewed Jan 2024).
- 38. Independent Health and Aged Care Pricing Authority. National Hospital Cost Data Collection (NHCDC) public sector report 2018–19. Sydney: IHACPA, 2021. https://www.ihacpa.gov.au/resources/national‐hospital‐cost‐data‐collection‐nhcdc‐public‐sector‐report‐2018‐19#:~:text=NHCDC%20Public%20Sector%20Cost%20Report&text=For%20the%20NHCDC%20Public%20Sector,per%20cent%20from%202017%2D18 (viewed July 2024).
- 39. Independent Health and Aged Care Pricing Authority. National Hospital Cost Data Collection (NHCDC) public sector 2021–22. Sydney: IHACPA, 2022. https://www.ihacpa.gov.au/resources/national‐hospital‐cost‐data‐collection‐nhcdc‐public‐sector‐2021‐22#:~:text=This%20includes%2048.0%20million%20patient,tables%20relating%20to%20the%20collection (viewed July 2024).
- 40. García‐Nogueras I, Aranda‐Reneo I, Peña‐Longobardo LM, et al. Use of health resources and healthcare costs associated with frailty: the FRADEA study. J Nutr Health Aging 2017; 21: 207‐214.
- 41. Diernberger K, Luta X, Bowden J, et al. Healthcare use and costs in the last year of life: a national population data linkage study. BMJ Support Palliat Care 2024; 14: e885‐e892.
- 42. Burrell AJC, Neto AS, Broadley T, et al. Comparison of baseline characteristics, treatment and clinical outcomes of critically ill COVID‐19 patients admitted in the first and second waves in Australia. Crit Care Resusc 2021; 23: 308‐319.
- 43. Storms AD, Chen J, Jackson LA, et al. Rates and risk factors associated with hospitalization for pneumonia with ICU admission among adults. BMC Pulm Med 2017; 17: 208.






Abstract
Objectives: To compare hospital admission costs for coronavirus disease 2019 (COVID‐19) cases to hospital admission costs for other viral pneumonia cases in Australia, and to describe hospital admission costs for post‐COVID‐19 condition.
Design, setting, participants: A cost comparison analysis of hospital admissions due to COVID‐19 or other viral pneumonias between 1 January 2020 and 30 June 2021 at Victorian public health acute and subacute services.
Main outcome measures: Demographic characteristics, clinical outcomes (including diagnoses, impairment, subacute admission, intensive care unit admissions, ventilation, and length of stay) and cost data (including diagnostic‐related groups, and total, direct and indirect costs).
Results: During the study period, 3197 patients were admitted to hospital due to COVID‐19 and 15 761 were admitted for other viral pneumonias. Admissions for COVID‐19 cost 29% more than admissions for other viral pneumonias. Admissions for COVID‐19 requiring intensive care unit admission incurred significantly higher mean costs (A$120 504 or US$90 595) compared with those not requiring intensive care unit admission (A$19 634 or US$14 761). The adjusted cost of admissions related to post‐COVID‐19 condition was A$11 090 or US$8 337, and these admissions were significantly more likely to be elective. Direct costs accounted for most of the costs for all groups, and admissions for post‐COVID‐19 condition used less allied health services than other groups.
Conclusions: Given its recent emergence, cases of acute COVID‐19 and post‐COVID‐19 condition have had a significant additional financial impact on Australian hospitals. Further studies are required to understand long term costs and identify trends over time in the context of increased vaccination rates and subsequent variants of severe acute respiratory syndrome coronavirus 2.