Health care systems are responsible for 4–5% of global greenhouse gas (GHG) emissions.1,2 There is increasing pressure to reduce the environmental effects of health care as more health professionals recognise its contribution to climate change.3,4 However, measuring environmental effects and assessing progress towards decarbonisation are not trivial processes because the mechanisms driving environmental burdens are often hidden. Although much of the early focus in health has been on decarbonisation of building and transport assets, most of health care's GHG emissions occur within the supply chains that provision the health care system before the final delivery of services.5
This article is intended to serve as a beginner's introduction to the environmental footprinting techniques that can be applied to uncover health care's environmental impacts, including impacts occurring along supply chains. This article focuses on GHG emissions, but many other pollutants and environmental stressors can be assessed using these methods.
Impacts near and far
Environmental impacts can be separated into “direct” and “indirect” impacts. Direct impacts occur within an organisation's physical boundary, for example hospital grounds. Indirect impacts occur outside this immediate boundary, for example impacts from purchased products. Direct impacts are relatively easy to estimate using fossil fuel consumption and utility bills. In contrast, estimating indirect emissions is more challenging for health care organisations and requires detailed data on the quantity or cost of procured products and services and the application of environmental footprinting techniques. An organisation's indirect emissions form part of their suppliers’ direct emissions and likely occur in other regions and jurisdictions, rendering them more abstract and intangible.
Introduction to supply chains
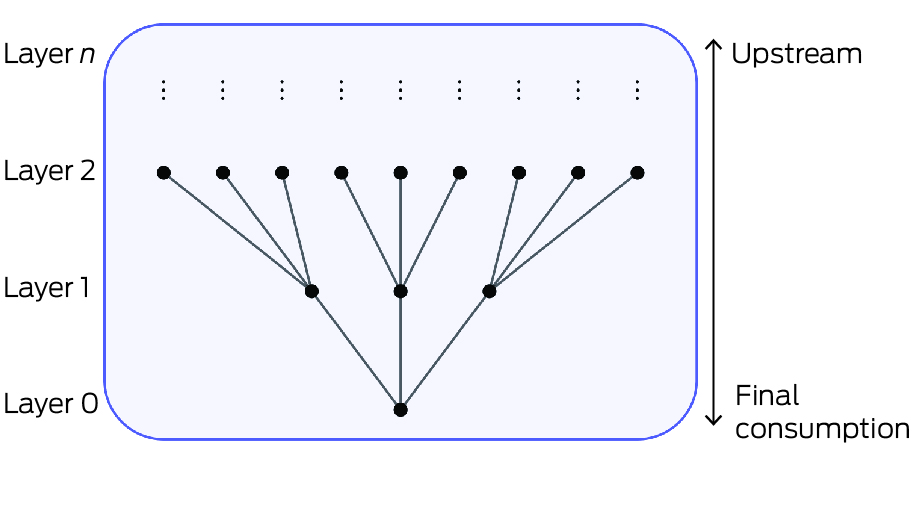
Quantifying indirect environmental impacts requires consideration of the supply chains delivering goods and services to final consumption. Supply chains link production layers together, where at each stage numerous inputs and components are combined to make intermediate products. This can be depicted as a tree branching upwards and outwards from the consumer, with each node representing a production stage (Box 1). Here, “upstream” refers to layers occurring before the product reaches a consumer, and “downstream” refers to layers after final consumption, including disposal of the product.
Environmental effects can occur at each layer and accumulate along the supply chain as more layers are included.6 Eventually, supply chains reach consumers as final products. Accounting for all upstream environmental impacts associated with a product or service is onerous because of the large number of production layers and the many inputs into each layer. An illustrative example of supply chain is “fossil fuel combustion > petrochemical refining > plastic sample jars > pathology services”, which is just one of the many supply chains contributing to “pathology services”.7
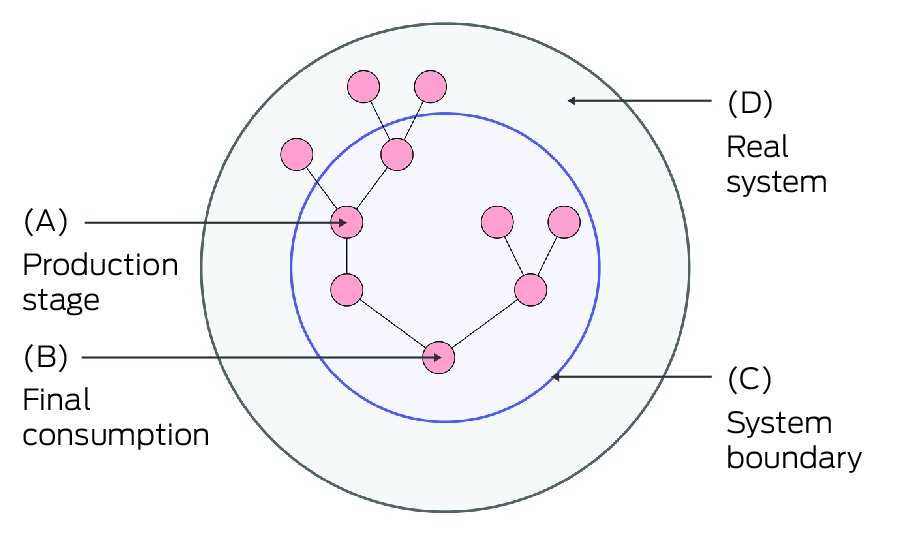
The “system boundary” is a conceptual limit within which environmental effects are captured by an assessment method.8 The boundary is considered “incomplete” when all important activities are not within the boundary, resulting in some fraction of environmental effects being uncounted.9 An awareness of the defined system boundary is important when calculating the full environmental footprint of a product or process and when making comparisons. The extent to which unaccounted impacts are significant depends on the process and activity and may include, for example, impacts arising from capital works, infrastructure and the services sector. Box 2 depicts the system boundary in relation to final consumption and intermediate production stages.
Scope‐based emissions accounting
The distinction between direct and indirect impacts can be further refined into scopes,10 which can be useful for conceptualising where emissions are occurring:
- Scope 1: direct emissions resulting from an organisation's activities within their physical boundary. Includes emissions of anaesthetic gases and emissions from burning natural gas for heat and steam.
- Scope 2: indirect emissions associated with the purchase of energy, for example emissions from electricity generation.
- Scope 3: all upstream emissions associated with the extraction, manufacturing and transport of goods and services. Examples include consumable products such as plastic implements, personal protective equipment and pharmaceuticals. Downstream emissions from waste disposal and treatment are also included.
Although in common use, these scopes are a simplification and do not always neatly align with organisation structure or function. For example, emissions from ambulatory patient transport may be attributed to a health system's scope 1 emissions; however, patient self‐transport emissions remain uncounted. In addition, the scope framework does not consider shared responsibility of emissions between upstream and downstream actors in the supply chain. These difficulties reflect wider societal complexities in attributing responsibility for emissions reductions.11
Environmental footprinting techniques
Two main environmental footprinting methods can be distinguished: life cycle assessment (LCA) and environmentally extended input–output analysis (EE‐IOA).
Life cycle assessment
Process‐based LCA is a technique for assessing environmental impacts of specific products or processes. LCA maps each life cycle stage of a product or activity, such as raw materials extraction, manufacturing, product use, and waste treatment and disposal, and accounts for the environmental impacts occurring at each stage.12 There are two main types of LCA: attributional (ALCA) and consequential (CLCA) life cycle assessment.13,14 ALCA accounts for environmental burdens associated with a product's life cycle, including production, use and disposal. CLCA describes how these flows change in response to decisions or changes, for example material design changes. An LCA analyst selects the processes and inputs to include in a particular assessment, which requires judgement and may result in truncated accounting of environmental impacts.6,8 Many health care LCAs have been done, for example, assessing the impacts of surgical and anaesthetic care,15 magnetic resonance imaging machines,16 and health care building construction.17 Repositories such as HealthcareLCA18 and other literature reviews provide useful compilations of LCA studies relevant to health care.19
Environmentally extended input–output analysis
Input–output analysis (IOA) is a well established method for tracing environmental impacts along supply chains.20,21 An environmental footprint calculated using IOA represents a retrospective allocation of impacts among products and services delivered to final consumption. This technique allocates all economy‐wide production impacts to final products, leaving no impacts unallocated. The technique also avoids double counting, as all production environmental effects are attributed only once to final products. EE‐IOA methods have been used to perform global assessments of health care1,2 as well as national level assessments.5,22 The sector detail of IO models is constrained by the underlying national accounting data, which limits IOA from analysing very specific activities or sectors. For example, IO models may distinguish hospitals from other health care services; however, specific activities such as oncology are likely beyond the model resolution. Similarly, issues of price can also distort the footprint calculation, for example in the case of low cost versus high cost pharmaceuticals.
Hybrid approaches
Hybrid approaches can be employed to overcome the limitations inherent in both LCA and IOA methods. LCA and EE‐IOA methods can be seen as complementary:23 LCA performs a bottom‐up attribution of environmental effects to specific processes, and EE‐IOA performs a top‐down allocation of economy‐wide environmental effects to final products. Hybrid approaches augment IOA‐based footprinting methods with process‐specific LCA data, which has the effect of mitigating the sectoral specificity issues of IOA. In addition, the use of IOA guarantees system boundary completeness.24 Hybrid methods were used to do carbon footprinting of England's National Health Service (NHS).25
Assessment quality and method selection
Which assessment technique should be used depends on the health care context and research question. In general, questions involving diagnostic methods and treatments are best answered using LCA techniques, whereas assessing overall progress at the health system level is more suited to EE‐IOA. International Organization for Standardization (ISO) 14040:2006 and 14044:2006 provide guidelines to practitioners doing life cycle assessments. The European Union is introducing new regulations to combat greenwashing26 and has its own guidelines on how LCAs should be done.27 IOA and its extensions are also governed by global standards.28 Adherence to these standards and guidelines can provide an indication of the quality and trustworthiness of sustainability assessments and enables comparison between studies.
Improving the use of environmental footprinting in health care
Environmental impacts will increasingly need to be assessed and considered as part of health sector decision making at every level. However, systems for environmental data collection, storage and analysis are often limited in many health systems and usually not standardised or linked to clinical and population outcomes.29 Information about product environmental performance is rarely provided by manufacturers, and the underlying data are often inaccessible.30
Health care professionals have an important role in normalising consideration of the environmental impact of health care and advocating for availability of evidence and the supporting infrastructure to evaluate and reduce that impact. We are not suggesting that environmental footprinting is the primary role of health care workers, nor are we suggesting that considerations of environmental impact should take precedence over clinical outcomes. Rather, environmental sustainability should be considered as a dimension of quality, safety and good governance alongside patient and population health outcomes.
Key areas for action to improve the use of environmental footprinting techniques in evidence‐based clinical decision making and measures of health system performance include:
- Improving health care environmental footprinting literacy. Undergraduate and postgraduate education should include information on environmental footprinting techniques. Health professionals should consider learning how the different techniques have been applied in their health system, organisation or specialty, and question the environmental impacts of the products and processes used.
- Incorporating environmental footprinting into existing frameworks for quality improvement, procurement and health system performance. This will make environmental costs more visible and facilitate more holistic decision making. Health professionals should call for regulators, procurement agencies and commissioners to include environmental footprinting in their assessment frameworks and contracts.25
- Investing in human and technological infrastructure to allow robust accounting and analysis. Collecting and storing detailed environmental and economic operations data are required for both LCA and EE‐IO studies, and for reporting of health system GHG emissions. A specialist workforce with sufficient capability and capacity to meet demand is needed.
- Increasing transparency and standardisation of methods of data collection, analysis and reporting. Transparent and standardised data collection and methods allow benchmarking and comparisons to be drawn to drive and monitor progress.25 Concerns of commercial non‐disclosure may be addressed by using trusted third parties and data sharing agreements.
- Learning from others. In health care, the NHS in England has taken a leading role in using environmental footprinting to drive decarbonisation of its own services and its suppliers and several other countries are now following suit. For buildings, the National Australian Built Environment Rating System (NABERS) in Australia has been effective at using continuous monitoring and evaluation to drive improvements in energy efficiency.32
Provenance: Not commissioned; externally peer reviewed.
- 1. Pichler P, Jaccard I, Weisz U, Weisz H. International comparison of health care carbon footprints. Environ Res Lett 2019; 14: 064004.
- 2. Lenzen M, Malik A, Li M, et al. The environmental footprint of health care: a global assessment. Lancet Planet Health 2020; 4: e271‐e279.
- 3. Doctors for the Environment Australia. National Health and Climate Strategy: response to the Australian Government consultation paper. Melbourne: DEA, 2023. https://assets.nationbuilder.com/docsenvaus/pages/376/attachments/original/1712644179/DEA‐response‐National‐Health‐Climate‐Strategy‐FINAL‐amended‐Approved‐31‐Jul‐2023.pdf?1712644179 (viewed May 2024).
- 4. World Health Organization. Alliance for Transformative Action on Climate and Health (ATACH). WHO, 2022. https://www.who.int/initiatives/alliance‐for‐transformative‐action‐on‐climate‐and‐health (viewed May 2024).
- 5. Malik A, Lenzen M, McAlister S, McGain F. The carbon footprint of Australian health care. Lancet Planet Health 2018; 2: e27‐e35.
- 6. Suh S, Lenzen M, Treloar GJ, et al. System boundary selection in life–cycle inventories using hybrid approaches. Environ Sci Technol 2004; 38: 657‐664.
- 7. McAlister S, Grant T, McGain F. An LCA of hospital pathology testing. Int J Life Cycle Assess 2021; 26: 1753‐1763.
- 8. Tillman AM, Ekvall T, Baumann H, Rydberg T. Choice of system boundaries in life cycle assessment. J Clean Prod 1994; 2: 21‐29.
- 9. Lenzen M. Differential convergence of life–cycle inventories toward upstream production layers. J Ind Ecol 2002; 6: 137‐160.
- 10. Clean Energy Regulator. Emissions and energy types [website] Canberra: Commonwealth of Australia, 2023. https://www.cleanenergyregulator.gov.au/NGER/About‐the‐National‐Greenhouse‐and‐Energy‐Reporting‐scheme/Greenhouse‐gases‐and‐energy (viewed Sept 2024).
- 11. Weidema BP, Pizzol M, Schmidt J, Thoma G. Attributional or consequential life cycle assessment: a matter of social responsibility. J Clean Prod 2018; 174: 305‐331.
- 12. Joshi S. Product environmental life–cycle assessment using input‐output techniques. J Ind Ecol 2008; https://doi.org/10.1162/108819899569449.
- 13. Finnveden G, Hauschild MZ, Ekvall T, et al. Recent developments in life cycle assessment. J Environ Manage 2009; 91: 1‐21.
- 14. Schaubroeck T, Schaubroeck S, Heijungs R, et al. Attributional and consequential life cycle assessment: definitions, conceptual characteristics and modelling restrictions. Sustainability 2021; 13: 7386.
- 15. Drew J, Christie SD, Tyedmers P, et al. Operating in a climate crisis: a state‐of‐the‐science review of life cycle assessment within surgical and anesthetic care. Environ Health Perspect 2021; 129: 76001.
- 16. McAlister S, McGain F, Petersen M, et al. The carbon footprint of hospital diagnostic imaging in Australia. Lancet Reg Health West Pac 2022; 24: 100459.
- 17. Botejara‐Antúnez M, Garrido‐Píriz P, Sánchez‐Barroso G, et al. Life cycle assessment (LCA) in the construction of healthcare buildings. Analysis of environmental impact. IOP Conf Ser: Earth Environ Sci 2021; 664: 012053.
- 18. Drew J, Christie SD, Rainham D, Rizan C. HealthcareLCA: an open‐access living database of health‐care environmental impact assessments. Lancet Planet Health 2022; 6: e1000‐e1012.
- 19. McGain F, Story D, Kayak E, et al. Workplace sustainability: the “cradle to grave” view of what we do. Anesth Analg 2012; 114: 1134‐1139.
- 20. Leontief W. Studies in the structure of the American economy: theoretical and empirical explorations in input–output analysis. New York: Oxford University Press, 1953. OCLC: 1012843.
- 21. Ayres RU, Kneese AV. Production, consumption, and externalities. Am Econ Rev 1969; 59: 282‐297.
- 22. Nansai K, Fry J, Malik A, et al. Carbon footprint of Japanese health care services from 2011 to 2015. Resour Conserv Recycl 2020; 152: 104525.
- 23. Agez M, Wood R, Margni M, et al. Hybridization of complete PLCA and MRIO databases for a comprehensive product system coverage. J Ind Ecol 2020; 24: 774‐790.
- 24. Majeau‐Bettez G, Strømman AH, Hertwich EG. Evaluation of process‐ and input–output‐based life cycle inventory data with regard to truncation and aggregation issues. Environ Sci Technol 2011; 45: 10170‐10177.
- 25. Tennison I, Roschnik S, Ashby B, et al. Health care's response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health 2021; 5: e84‐e92.
- 26. News European Parliament. EU to ban greenwashing and improve consumer information on product durability [press release]. 19 Sept 2023. https://www.europarl.europa.eu/news/en/press‐room/20230918IPR05412/eu‐to‐ban‐greenwashing‐and‐improve‐consumer‐information‐on‐product‐durability (viewed May 2024).
- 27. Damiani M, Ferrara N, Ardente F. Understanding product environmental footprint and organisation environmental footprint methods. European Commission, Joint Research Centre, Publications Office of the European Union; 2022. https://data.europa.eu/doi/10.2760/11564 (viewed May 2024).
- 28. Frischknecht R, Jolliet O; editors. Global guidance for life cycle impact assessment indicators, vol. 1. Paris: United Nations Environment Programme (UNEP), Society of Environmental Toxicology and Chemistry (SETAC), Life Cycle Initiative; 2016. https://www.lifecycleinitiative.org/training‐resources/global‐guidance‐lcia‐indicators‐v‐1 (viewed May 2024).
- 29. Smith CL, Zurynski Y, Braithwaite J. We can't mitigate what we don't monitor: using informatics to measure and improve healthcare systems’ climate impact and environmental footprint. J Am Med Inform Assoc 2022; 29: 2168‐2173.
- 30. McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability in anaesthesia and critical care. Br J Anaesth 2020; 125: 680‐692.
- 31. Mortimer F, Isherwood J, Wilkinson A, Vaux E. Sustainability in quality improvement: redefining value. Future Healthc J 2018; 5: 88‐93.
- 32. Precious B. Energy efficiency in commercial buildings. National Australian Built Environment Rating System, Department of Industry, Science, Energy and Resources; 2022. https://www.nabers.gov.au/publications/energy‐efficiency‐commercial‐buildings (viewed May 2024).





We thank Anthony Capon, Richard Wood and Michael Frommer for their comments on an earlier version of this manuscript.
No relevant disclosures.