Although the acute disease burden of coronavirus disease 2019 (COVID‐19) in Australia has reduced, the longer term impacts are becoming increasingly apparent.1 The constellation of persistent symptoms is termed “post‐acute COVID‐19 condition”, also known as “long COVID”, and includes dyspnoea, fatigue, cognitive impairments, headaches, and psychiatric symptoms.2,3 The health impact at a population level is significant, with between 10% and 20% of people having persistent symptoms after a COVID‐19 infection.4,5
Impact of long COVID
Patient testimonies describe the devastating impact of symptoms left untreated by health services.6,7 The functional sequalae of long COVID include reduced quality of life8,9 and difficulty engaging in normal life roles, including family, work and caring responsibilities.10 COVID‐19 has also disproportionately affected disadvantaged communities who have less access to health care services and less resources to allow for absences from work.11
As the world has returned to normal, many people living with long COVID continue to report feeling left behind and isolated by persistent symptoms.12 Alongside this, many people report feeling ignored or not believed by health care providers, who often struggle to pinpoint physiological impairment and associated treatments.13 This can lead to a marked discordance between the lived experience of ongoing debilitation and the expectations of the community and health care sector of what recovery from COVID‐19 looks like.
Models of care
Initially, Australia's response to long COVID followed a specialist clinic model of care, including individual referrals to respiratory and cardiac specialists. With the emergence of milder acute illness, the model of care for long COVID in Australia has now moved to primary care, with general practitioners seen as the coordinators of ongoing services and interventions.14
Allied health multidisciplinary care
The heterogeneous nature of long COVID symptoms, coupled with no diagnostic tool or single treatment, means the functional burden of long COVID may best be addressed by symptom management approaches.15,16 In this regard, Australian and international guidelines recommend multidisciplinary and coordinated allied health care as a practice standard for people with long COVID,17,18 and there is emerging evidence of corresponding functional improvement.19,20 In line with these recommendations, the National Health Service in the United Kingdom encourages a three‐tiered approach to care, with multidisciplinary interventions offered to people with the most severe symptoms requiring input from two or more professionals, stepping down to community therapy teams, and then self‐management pathways for individuals with milder symptoms.21 In Australia, access to publicly funded allied health intervention for long COVID remains challenging with no system‐level coordinated care or funding.
The ReCOVery service at Austin Health
In early 2022, Austin Health in Melbourne commenced ReCOVery: an allied health‐led rehabilitation service aimed at providing multidisciplinary management for long COVID symptoms based on international evidence and guidelines translated into the Australian context.17,18 The key principles in the design of the service were (i) a stepped care model, with access to a multidisciplinary team for individuals with the most severe symptoms, and a self‐management pathway for those with less severe symptoms; (ii) symptom management, improved function and participation via coordinated goal‐driven allied health care, mainly offered via telehealth; (iii) care designed to complement rather than replace existing care pathways, such as pulmonary rehabilitation; and (iv) patients as partners in their care through shared rehabilitation goals. The team consisted of exercise physiology, clinical neuropsychology, occupational therapy, clinical psychology, nutrition and dietetics, speech pathology and rehabilitation medicine, who onward referred to other medical specialists as required. The Austin Health Human Research Ethics Committee (HREC 88943/Austin‐2022) provided approval for the service improvement audit presented.
Triage and assessment
ReCOVery opened during the third peak of COVID‐19 in early 2022. Initially, all previous COVID‐19‐positive Austin Health inpatients were contacted via SMS to offer intervention (Box 1). Along with this, referrals internally from specialist clinics and self‐referrals for any Austin Health staff affected by long COVID were accepted. Our system was designed to ensure timely access to care for individuals with the most severe symptoms. This involved:
- completion of an online custom‐designed symptom severity assessment to establish symptom impact using a “mild”, “moderate” and “severe” grading (Supporting Information);
- triaging of participants to access either independent education and resources for milder symptoms or an individual and group therapy program for participants experiencing moderate to severe symptoms; and
- completion of an intake and goal‐setting appointment for rehabilitation plans for participants requiring multidisciplinary team assessment.
The service opened to referrals from general practitioners mid‐2022 and received on average one referral each day.
Participant profile
SMS messages were sent to 4480 former patients of Austin Health who had been treated for COVID‐19. About 40% of these patients (1708) responded, with 254 (15%) indicating they had ongoing symptoms. We additionally received 147 referrals (Box 2). Overall, we triaged and assessed 285 people, with 163 going on to receive individual therapy in the eight months the service operated.
Individuals accessing the service were more likely to be women (72%) and were of working age (average age 49 years) (Box 3). Participants reported that the impact of long COVID on their lives was profound. Self‐reported measurement of health‐related quality of life and physical and mental health on a 0–100 scale found a significant reduction across all measures since their COVID‐19 diagnosis (P < 0.001 for all).
Symptoms and service utilisation
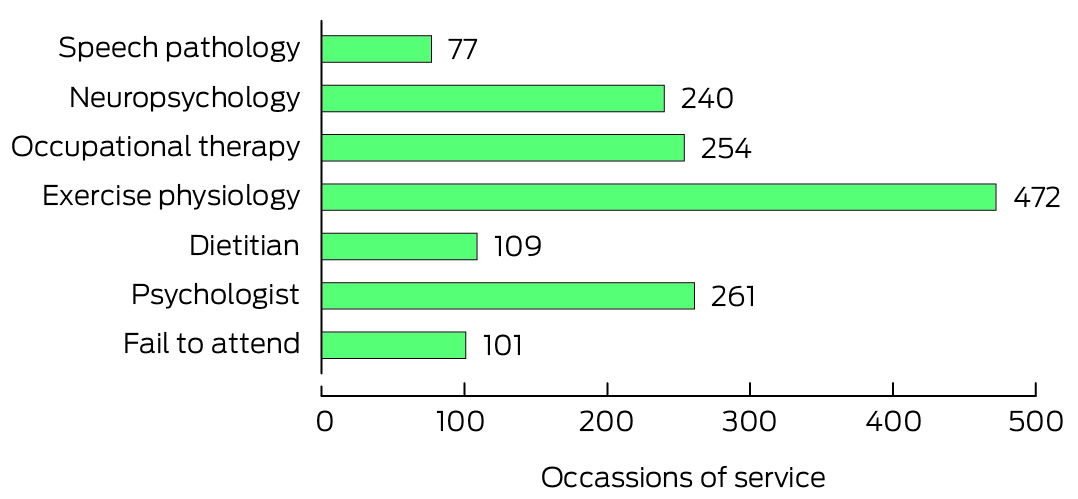
The most common symptoms reported at a moderate to severe level were fatigue, brain fog and psychological impacts (Box 3). Most participants accessing the service were seen by more than one multidisciplinary team member (63%). Exercise physiology was the most in‐demand discipline, followed by clinical psychology and occupational therapy (Box 4). We had a low “fail to attend” rate at 7%. Individual discipline therapy was complemented by online self‐management resources22 and a bespoke virtual group program that was attended by 72 people. Groups consisted of single sessions on living with long COVID, olfactory impairment, brain fog, and managing fatigue.
Interventions
The evidence base for long COVID interventions is emerging, and interventions were based on clinical guidelines, such as the National Institute for Health Care and Excellence guidelines,17 that are mainly at the expert consensus or low level of evidence currently. As per these guidelines, the clinic interventions included (i) a one‐stop, coordinated approach to care; (ii) management of fatigue, brain fog, olfactory impairment, sleep and voice changes; (iii) clinical psychological support and intervention, including for adjustment to persistent symptoms, ongoing COVID‐19 and health anxiety, general psychological difficulties and exacerbation of pre‐morbid mental health concerns; (iv) investigation, diagnosis and management of postural orthostatic tachycardia syndrome in conjunction with hypertension specialist medical services; and (v) occupational therapy supporting functional improvement to allow people to return to important activities and life roles, such as work and caring responsibilities.
Recommendations
There are still relatively few Australian public health services to provide the recommended multidisciplinary care to people living with long COVID. Most people are unable to access rehabilitation services that could provide relief from symptoms, improve quality of life and support return to valued life roles. The ReCOVery model of care was developed using international guidelines and provided impactful care to participants. People accessing our service would otherwise most likely have fallen between the cracks of our health system, unable to access traditional post‐injury or acute rehabilitation services or aged care services. The ReCOVery model provides a viable blueprint for a stepped care approach to support patients, and provides initial evidence for allied health discipline requirements through our utilisation data. Despite this, funding for services has largely ceased across multiple public long COVID clinics in Victoria. This has compounded inequity in who can access care, with private allied health options being simply unaffordable to most people. Care plans for access to allied health services can be completed by a general practitioner but only provide five sessions, with gap fees being common.
Enablers and barriers
We were able to effectively run the ReCOVery service almost exclusively via telehealth. Centrally located telehealth hubs for long COVID would be a viable model to provide therapy to people who need it most. This telehealth model supports care by specialist disciplines that are difficult for most Australians to access, such as clinical neuropsychology. We acknowledge that people from culturally and linguistically diverse backgrounds and from disadvantaged communities may not have ready access to telehealth infrastructure, with centre‐based options needed for some. A tiered (stepped) approach to care is the most efficient and cost‐effective solution to management of long COVID and has been successfully implemented elsewhere.21 However, our triaging process was time consuming and lengthy for patients. Streamlining through general practice assessment and referrals may mitigate this barrier to access.
Conclusions
General practitioners are now seen as the central specialty in the diagnosis and management of long COVID.16 Although they are well equipped to be the primary medical contact for patients, they still require education on, and referral options for, therapeutic interventions via allied health. Multidisciplinary rehabilitation is the most effective solution to improve quality of life for patients with severe ongoing symptoms and reduce the burden on general practitioners. Unfortunately, in Australia, unless we shore up access via our public health services or Medicare rebates, this opportunity will be limited to people with significant financial means.
Box 1 – ReCOVery long COVID rehabilitation service model of care
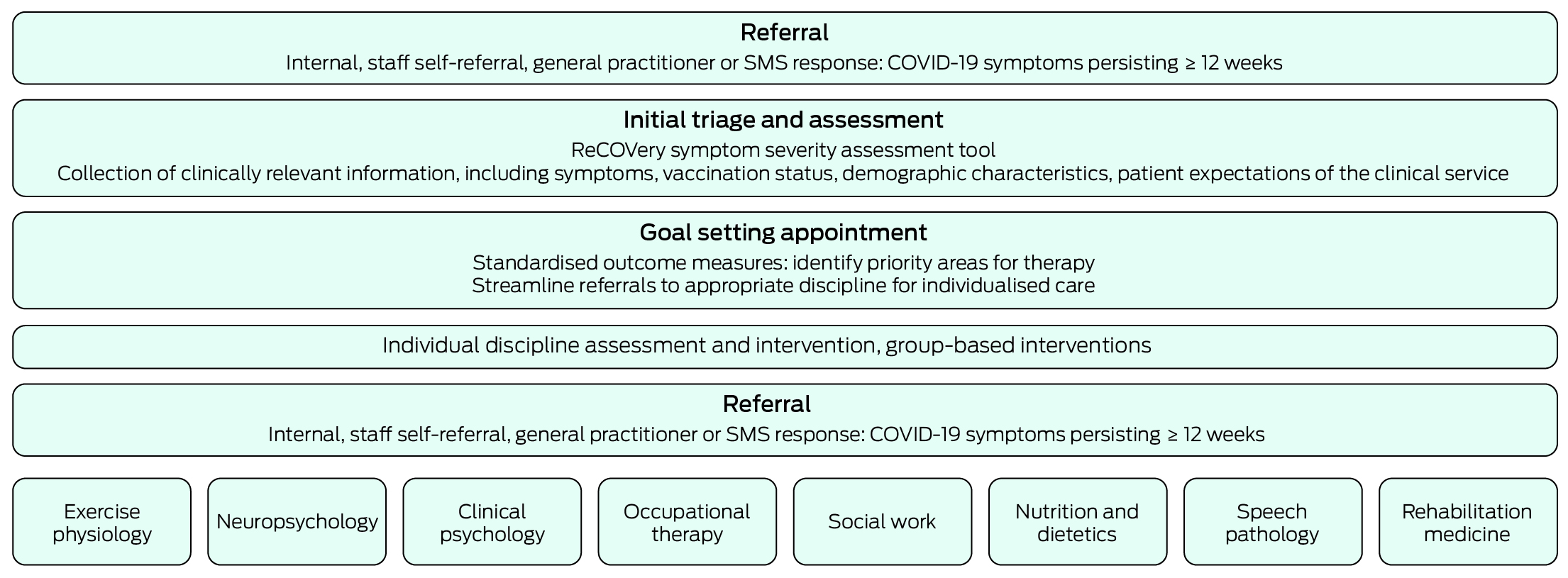
COVID‐19 = coronavirus disease 2019.
Box 2 – Flow diagram of the triage and assessment process for ReCOVery service participants
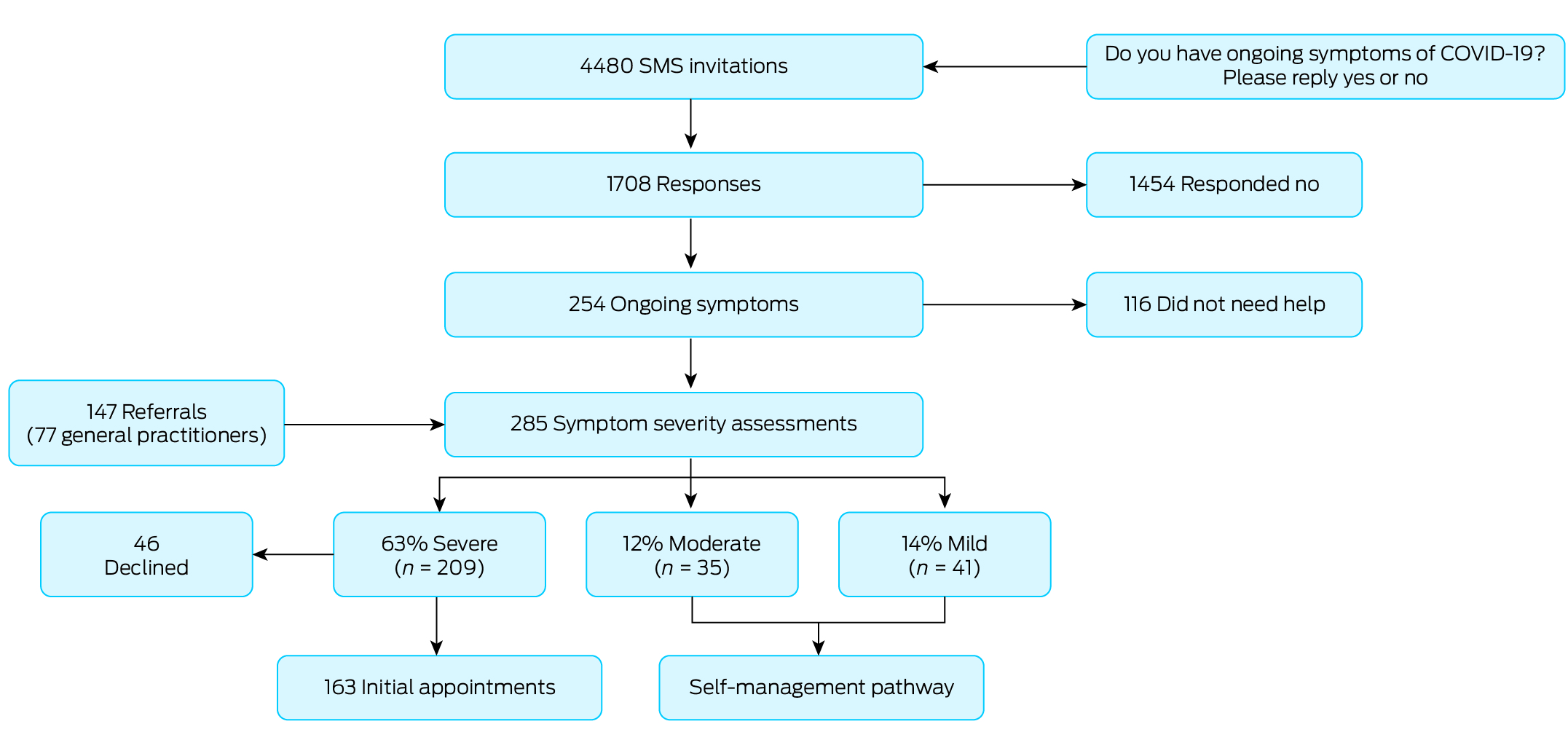
COVID‐19 = coronavirus disease 2019.
Box 3 – Demographic characteristics and symptom information of patients who completed triage screening in ReCOVery (all participants endorsed having ongoing symptoms before triage)
|
|
N (%) |
Mean (SD) |
Range |
||||||||||||
|
|
|||||||||||||||
|
Age (years) |
|
|
|
||||||||||||
|
Females |
204 (71.6%) |
46.8 (14.6) |
18 to 86 |
||||||||||||
|
Males |
80 (28.1%) |
54.6 (16) |
18 to 91 |
||||||||||||
|
Prefer not to say |
1 (< 1.0%) |
40.8 |
|
||||||||||||
|
Total |
285 |
48.9 (15.3) |
18 to 91 |
||||||||||||
|
Initial infection year |
|
|
|
||||||||||||
|
2020 |
11 (3.9%) |
|
|
||||||||||||
|
2021 |
68 (23.9%) |
|
|
||||||||||||
|
2022 |
206 (72.2%) |
|
|
||||||||||||
|
Current vaccination status |
|
|
|
||||||||||||
|
Vaccinated |
266 (90.5%) |
|
|
||||||||||||
|
Vaccination timeline |
|
|
|
||||||||||||
|
Before COVID‐19 infection |
244 (91.7%) |
|
|
||||||||||||
|
After COVID‐19 infection |
22 (8.3%) |
|
|
||||||||||||
|
Employed before illness |
207 (72.6%) |
|
|
||||||||||||
|
Health care worker |
83 (29.1%)* |
|
|
||||||||||||
|
Acute illness severity |
|
|
|
||||||||||||
|
No symptoms |
4 (1.5%) |
|
|
||||||||||||
|
Had symptoms but remained at home |
203 (73%) |
|
|
||||||||||||
|
Admitted to hospital |
46 (16.5%) |
|
|
||||||||||||
|
Admitted to hospital and received high flow oxygen or ICU admission |
25 (9.0%) |
|
|
||||||||||||
|
Impact† |
|
|
|
||||||||||||
|
Change in mental health (0–100) |
|
‐19.8 (24.5) |
‐96 to 44 |
||||||||||||
|
Change in physical health (0–100) |
|
‐26.2 (22.4) |
‐90 to 31 |
||||||||||||
|
Change in quality of life (0–100) |
|
‐28.3 (25.3) |
‐100 to 30 |
||||||||||||
|
Top ten symptoms |
|
|
|
||||||||||||
|
Fatigue |
270 (95.0%) |
|
|
||||||||||||
|
Brain fog |
229 (80.0%) |
|
|
||||||||||||
|
Anxiety/worry |
209 (75.2%) |
|
|
||||||||||||
|
Mood changes |
212 (76.8%) |
|
|
||||||||||||
|
Voice changes |
110 (41.5%) |
|
|
||||||||||||
|
Persistent muscle pain |
187 (68.8%) |
|
|
||||||||||||
|
Shortness of breath |
202 (73.7%) |
|
|
||||||||||||
|
Sleep disturbance |
195 (73.3%) |
|
|
||||||||||||
|
Cough |
162 (59.8%) |
|
|
||||||||||||
|
Headache |
201 (74.2%) |
|
|
||||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; ICU = intensive care unit; SD = standard deviation. * We note that the proportion of our cohort who were health care professionals reflects our deliberate policy of allowing direct access to care for these individuals. † Difference between self‐reported mental health, physical health and quality of life self‐reported pre‐ and post‐COVID‐19 diagnosis. |
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
- 1. Gram MA, Emborg HD, Schelde AB, et al. Vaccine effectiveness against SARS‐CoV‐2 infection or COVID‐19 hospitalization with the Alpha, Delta, or Omicron SARS‐CoV‐2 variant: a nationwide Danish cohort study. PLoS Med 2022; 19: e1003992.
- 2. Montani D, Savale L, Noel N, et al. Post‐acute COVID‐19 syndrome. Eur Respir Rev 2021; 31: 210185.
- 3. Lopez‐Leon S, Wegman‐Ostrosky T, Perelman C, et al. More than 50 long‐term effects of COVID‐19: a systematic review and meta‐analysis. Sci Rep 2021; 11: 16144.
- 4. Woldegiorgis M, Cadby G, Ngeh S, et al. Long COVID in a highly vaccinated but largely unexposed Australian population following the 2022 SARS‐CoV‐2 Omicron wave: a cross‐sectional survey. Med J Aust 2024; 220: 323‐330. https://www.mja.com.au/journal/2024/220/6/long‐covid‐highly‐vaccinated‐largely‐unexposed‐australian‐population‐following
- 5. Thompson EJ, Williams DM, Walker AJ, et al. Long COVID burden and risk factors in 10 UK longitudinal studies and electronic health records. Nat Commun 2022; 13: 3528.
- 6. Callan C, Ladds E, Husain L, et al. “I can't cope with multiple inputs”: a qualitative study of the lived experience of “brain fog” after COVID‐19. BMJ Open 2022; 12: e056366.
- 7. Greenhalgh T, Ladds E, Knight M, Ravindran D. “Long COVID”: evidence, recommendations and priority research questions. London: UK Parliament, 2020. https://committees.parliament.uk/writtenevidence/12345/pdf/ (viewed Sept 2023).
- 8. Sanchez‐Ramirez DC, Normand K, Zhaoyun Y, Torres‐Castro R. Long‐term impact of COVID‐19: a systematic review of the literature and meta‐analysis. Biomedicines 2021; 9: 900.
- 9. Logue JK, Franko NM, McCulloch DJ, et al. Sequelae in adults at 6 months after COVID‐19 infection. JAMA Netw Open 2021; 4: e210830.
- 10. Davis HE, Assaf GS, McCorkell L, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021; 38: 101019.
- 11. de Leeuw E, Yashadhana A, Hitch D. Long COVID: sustained and multiplied disadvantage. Med J Aust 2022; 216: 222‐224. https://www.mja.com.au/journal/2022/216/5/long‐covid‐sustained‐and‐multiplied‐disadvantage
- 12. Ladds E, Rushforth A, Wieringa S, et al. Persistent symptoms after COVID‐19: qualitative study of 114 “long COVID” patients and draft quality principles for services. BMC Health Serv Res 2020; 20: 1144.
- 13. Burton A, Aughterson D, Fancourt D, Philip KEJ. Factors shaping the mental health and well‐being of people experiencing persistent COVID‐19 symptoms or “long COVID”: qualitative study. BJPsych Open 2022; 8: e72.
- 14. Parliament of Australia. Sick and tired: casting a long shadow. Inquiry into long COVID and repeated COVID infections. Canberra: Commonwealth of Australia, 2023. https://parlinfo.aph.gov.au/parlInfo/download/committees/reportrep/RB000006/toc_pdf/SickandtiredCastingalongshadow.pdf (viewed Sept 2023).
- 15. Barr ML, Welberry H, Comino EJ, et al. Understanding the use and impact of allied health services for people with chronic health conditions in Central and Eastern Sydney, Australia: a five‐year longitudinal analysis. Prim Health Care Res Dev 2019; 20: e141.
- 16. Fowler Davis S, Farndon L, Harrop D, et al. A rapid review and expert identification of the Allied Health Professions’ interventions as a contribution to public health outcomes. Public Health Pract (Oxf) 2020; 2: 100067.
- 17. National Institute for Health Care and Excellence. COVID‐19 rapid guideline: managing the long‐term effects of COVID‐19 [NICE guideline NG188]. London: NICE, 2020. https://www.nice.org.uk/guidance/ng188#:~:text=This%20guideline%20covers%20identifying%2C%20assessing,start%20of%20acute%20COVID%2D19 (viewed Sept 2023).
- 18. National Clinical Evidence Taskforce COVID‐19. Australian guidelines for the clinical care of people with COVID‐19: care after COVID‐19. NCET, 2023. https://app.magicapp.org/#/guideline/L4Q5An/section/jDJJJQ (viewed Sept 2023).
- 19. Harenwall S, Heywood‐Everett S, Henderson R, et al. Post‐COVID‐19 syndrome: improvements in health‐related quality of life following psychology‐led interdisciplinary virtual rehabilitation. J Prim Care Community Health 2021; 12: 21501319211067674.
- 20. Nopp S, Moik F, Klok FA, et al. Outpatient pulmonary rehabilitation in patients with long COVID improves exercise capacity, functional status, dyspnea, fatigue, and quality of life. Respiration 2022; 101: 593‐601.
- 21. Parkin A, Davison J, Tarrant R, et al. A multidisciplinary NHS COVID‐19 service to manage post‐COVID‐19 syndrome in the community. J Prim Care Community Health 2021; 12: 21501327211010994.
- 22. ReCOVery Team. Learn about long COVID. Melbourne: Austin Health, 2022. https://www.austin.org.au/learn‐about‐long‐covid/ (viewed Sept 2023).






Open access:
Open access publishing facilitated by The University of Melbourne, as part of the Wiley – The University of Melbourne agreement via the Council of Australian University Librarians.
We acknowledge the Allied Health ReCOVery team. The service would not have been possible without the support of Austin Health allied health leaders, in particular Brit Gordon and Sue Berney. We also thank all the people who attended our service and who openly shared their stories and goals with us on their road to recovery.
No relevant disclosures.