Stroke is the world's second‐leading cause of death and the third‐leading cause of death and disability.1 In Australia, stroke is the third most common cause of death and a leading cause of disability.2 As a result, stroke is costly to the health system, society and the individual.3
Three acute stroke interventions have broadly applicable, significant, readily quantifiable health economic benefits: stroke unit care (for both ischaemic stroke and intracerebral haemorrhage)4 and ischaemic stroke reperfusion therapies, thrombolysis5 and endovascular thrombectomy (EVT).6 For every 17 patients treated in a stroke unit, one death or disabled outcome is prevented.4 The number needed to treat to prevent disability for thrombolysis under three hours is ten,5 and the EVT number needed to treat to prevent functional dependency is five.6 Expediting reperfusion therapies substantially magnifies treatment benefits; “saving a minute” gains an extra day of quality‐adjusted life following thrombolytic treatment,7 and an extra week following EVT.7,8
Australia's stroke performance languishes behind international peers
Despite Australia having a national acute stroke clinical care standard,9 a national stroke registry (www.auscr.com.au), several centres of excellence10 and population‐based reperfusion therapy rates comparable to other high income countries,11,12 Australia compares poorly internationally in stroke unit admission percentages and speed of reperfusion treatment.11 In 2022, Australia's median door‐to‐needle (thrombolytic) time was 75 minutes.11 Only 27% of patients were treated within an hour of hospital arrival, compared with 82% in Sweden,12 75% in the United States (US),13 and 61% in the United Kingdom (UK).14 In Sweden during 2022, 93% of patients with stroke were admitted to a stroke unit, compared with 75% in Australia. The US, from 2016 to 2019, reported median door‐arterial puncture times for non‐transferred EVT cases of 78 minutes15 versus 115 minutes in 2022 in Australia.11
Concerningly, door‐to‐needle times and stroke unit admission percentages have not improved over the past six years (Box 1). Regional and remote Australians are most significantly affected by these treatment gaps.11,16 Because a higher proportion of Aboriginal and Torres Strait Islander Australians live in non‐metropolitan areas, improving national stroke performance is a critical Closing the Gap initiative. Given the poorer stroke outcomes associated with suboptimal stroke care, continued national inertia is unjustifiable.
Genesis of the 30/60/90 national stroke targets
In 2023, national stroke leaders proposed that the “Championing Care”‐themed combined Smart Strokes/Australian and New Zealand Stroke Organisation annual conference should urgently tackle these shortcomings.
From February 2023, the largest and most harmful national performance gaps were identified, and improvement targets and timeframes were proposed (Supporting Information). Targets were iteratively developed from the Australian Commission on Safety and Quality in Health Care Acute Stroke Clinical Care Standard indicators9 against an informal matrix (Supporting Information, table 1), where the following criteria could be met:
- broad applicability: targets needed to apply to a significant proportion of patients with stroke;
- measurability: targets needed to be measurable within the current Australian stroke clinical registry;
- quantifiability: the health economic benefit of meeting targets needed to be quantifiable through robust estimates of the associated disability‐adjusted life year benefit; and
- improvability: targets needed to address areas of significant treatment variability, compared against high performing sites nationally and/or high performing nations internationally. Targets needed to be theoretically achievable by 2030.
Five clear standout areas for improvement were identified. Impactful targets reasonably achievable by 2030 were agreed, subsequently termed the “30/60/90 National Stroke Targets” (Box 2), incorporating certified stroke unit admission rates, rapid thrombolytic administration, rapid EVT, and rapid door‐in‐door‐out times for EVT‐eligible patients being transferred via road ambulance (Box 3). These targets were presented to a broad representative group at a pre‐conference workshop and unanimously endorsed by workshop attendees. The targets have since been ratified by every major Australian stroke‐interested organisation (Supporting Information).
During and following this workshop, we identified barriers to previous quality improvement efforts and facilitators for target progress (Box 4); many of which are counterparts. Key barriers included a previous lack of clearly articulated and prioritised targets and timeframes, lack of a national public‐facing competitive stroke data dashboard (as in the UK),14 our federated health system (with a complex mix of state and federal funding) and incomplete participation of hospitals nationally in transparent quality improvement initiatives. Facilitators include cohesive national stroke organisations, improving national telestroke coverage (both for acute and post‐acute care),17 a national stroke registry with recent development of national data dashboards, the recent national stroke unit certification initiative,18 recent refinement of the National Stroke System Framework19 and innovative pre‐hospital stroke technologies coordinated through the Australian Stroke Alliance.20
We do not need to reinvent the key granular acute “code stroke” time‐saving strategies13,21 — many other countries have managed to improve their stroke care systems — we simply need to modify these proven strategies for the Australian context.
Key supporting initiatives
Most importantly, clinicians, health administrators and politicians need to commit to the key goals of stroke unit care for all, and expedited reperfusion treatment for eligible individuals. Three key initiatives need to then follow.
Stroke hospital mapping
All Australian hospitals should be identified as one of five potential stroke hospital categories, according to the 2023 Stroke Foundation National Acute Stroke Services Framework:19
- comprehensive stroke centre (CSC): a hospital providing 24/7 endovascular thrombectomy and neurosurgical services;
- primary stroke centre (PSC): a hospital providing 24/7 thrombolysis and stroke unit care;
- stroke capable regional general hospital (SCRGH): a hospital geographically distant from metropolitan centres, which provides 24/7 thrombolysis and stroke care approximating stroke unit care, but from which routine transfer to a large PSC or CSC is infeasible, due to distance;
- telestroke thrombolysis centre (TTC): a hospital providing telestroke‐enabled thrombolysis, ideally 24/7, but not providing stroke unit care;
- general hospital: a hospital that does not provide either thrombolysis or stroke unit care, but which should have protocols for patients presenting with stroke, to ensure rapid transfer to hospitals with thrombolysis and stroke unit care.
Ensuring access to stroke and stroke unit care, supported by stroke unit certification
Every person with stroke in Australia should be provided, where possible, with the opportunity to access both stroke unit care and reperfusion therapies, with the support of TTCs, general hospitals, ambulance services, retrieval services and telestroke capability. All current and potential CSCs, PSCs and SCRGHs should be supported by state and territory governments in meeting national stroke unit certification criteria and gaining certification, to ensure that optimal stroke unit care is being provided.
Implementing key reperfusion optimisation strategies at state and local levels
Each state stroke network (or equivalent) should identify state and hospital medical and stroke nursing leads to champion local strategies with proven impact. These strategies have been distilled in the 30/60/90 National Stroke Targets Action Plan, and include direct transfer of stroke patients from hospital arrival to the computed tomography (CT) room on the ambulance stretcher,10 using same‐crew and same‐stretcher transfer to a CSC if an EVT‐eligible large vessel occlusion stroke is identified.22 Thrombolytic agents should be administered as soon as the non‐contrast CT scan confirms eligibility in clear‐cut cases,23 and the EVT team contacted when large vessel occlusion is strongly suspected.23 Neuroimaging on arrival for transferred EVT cases should generally not be repeated, unless there have been protracted delays.24 And, perhaps most importantly, hospitals and stroke networks should acquire stroke metrics using standardised definitions, analyse results, be transparent about shortcomings, and plan improvements.21 It is acknowledged that smaller or more remote hospitals will be less able to reach national targets, and that larger well resourced centres will need to perform substantially better than the targets, to facilitate these national medians.
Monitoring national performance and fine‐tuning action plan strategies
The Australian Stroke Coalition will provide national support and will seek government or philanthropic support to adapt and optimise a “Get with the guidelines”, or similar, program.25 Approaches for funding will be grounded by a health economic analysis of benefits, should targets be met. State and national progress will be assessed at annual or biannual workshops, with lessons and strategies compared and shared. Performance will be incentivised by national achievement and improvement awards, and a national 30/60/90 stroke data dashboard through the national registry, where hospitals and states can compare their performance against their peers and the targets. It is hoped that national agreement on making the data dashboard consumer‐facing will be reached, to allow citizens with lived experience to also advocate for improvements.
Ancillary benefits
Reaching these targets is not an end, but a beginning. It is envisaged that the current targets will be Phase 1 of a sequence of national stroke targets. Achieving these targets will not only lead to improved stroke outcomes, but the streamlining and optimisation of acute stroke treatment pathways will greatly benefit Australian stroke professional training and research, across the continuum of stroke care. The mutual focus on a well articulated meaningful goal will increase team cohesion within hospitals, between professions, between states and between professional organisations.
Additionally, the optimised pre‐hospital pathways for acute stroke treatment will benefit the development of ultra‐early intracerebral haemorrhage pathways,26 and potentially pave the way for ultra‐early minimally invasive intracerebral haemorrhage surgery.27 Consumer‐facing national performance dashboards (if approved) may be adopted by other data‐driven specialties, such as cardiology (for acute coronary syndromes), trauma services and intensive care units. This target‐based, public‐facing, data‐driven approach, if broadly emulated, may serve as a key facilitator of nation‐wide “learning health systems”.28
Conclusion
A concerted effort is required to improve substandard Australian stroke unit admission rates and reperfusion treatment speed. A national commitment to addressing these treatment gaps is required, at all levels of health systems and government, supported by ambulance and retrieval services, emergency and radiology departments, and the medical and nursing staff administering acute stroke treatments. Addressing these shortcomings will provide a platform for further stroke improvements, and, if successful, could serve as a template for quality improvement initiatives in other health areas.
Box 1 – National stroke registry evidence of flatlining stroke unit access rates and intravenous thrombolytic treatment times11
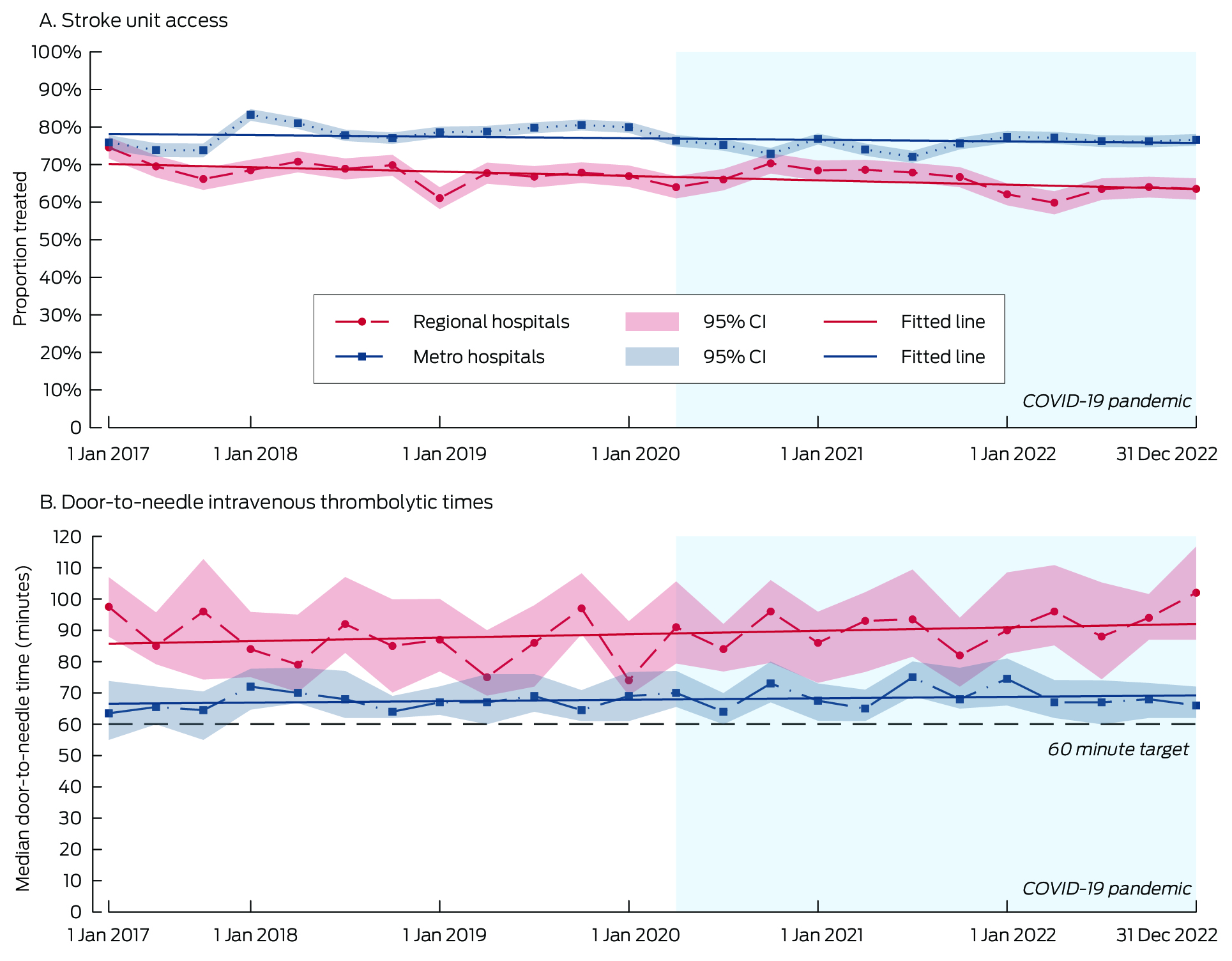
Adapted, with permission, from the Australian stroke clinical registry annual report, 202111 with updated data for 2022 from the Australian stroke clinical registry and Australian stroke data tool (limited to the 45 hospitals that participated between 2017 and 2022 and submitted 30+ episodes each calendar year into the Australian stroke data tool.)
Box 2 – The 30/60/90 National Stroke Targets (Australia 2023)
By 2030:
- National median endovascular clot retrieval door‐to‐puncture time < 30 minutes for transfers
- National median thrombolysis door‐to‐needle time < 60 minutes
- National median door‐in‐door‐out time for endovascular clot retrieval transfers < 60 minutes*
- National median endovascular clot retrieval door‐to‐puncture time < 90 minutes for primary presenters
- Certified stroke unit care provided to > 90% of patients with primary stroke diagnosis
* Where same‐crew ambulance door‐in and door‐out transfer is possible. Regional services retrieving via road should aim for a 75‐minute door‐in‐door‐out time (hospitals requiring aero‐retrieval service are not included in this target).
Box 3 – Idealised hyperacute large vessel occlusion (LVO) stroke pathways at comprehensive and primary stroke centres
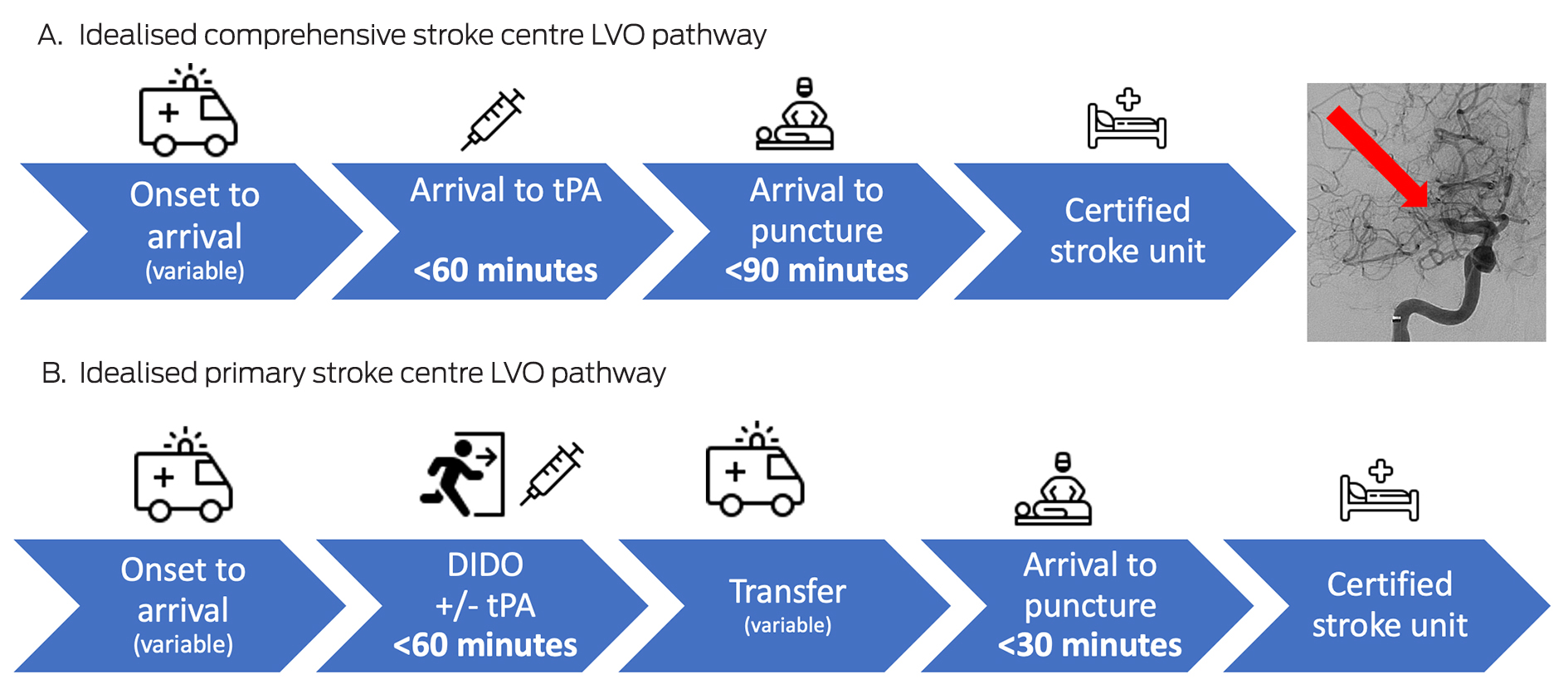
LVO = large vessel occlusion; tPA = tissue Plasminogen Activator; DIDO = door‐in‐door‐out.A. For patients presenting to a comprehensive stroke centre with a large vessel occlusion (such as a right middle cerebral artery occlusion; shown in inset image), identification of the arterial occlusion, notification of the endovascular thrombectomy (EVT) team, and administration of thrombolytic agent should occur in parallel, aiming to promptly move the patient to the EVT theatre, allowing arterial puncture within 90 minutes.B. For patients presenting to a primary stroke centre with a large vessel occlusion, identification of the arterial occlusion, notification of the EVT team, and administration of thrombolytic agent should occur in parallel. Same‐crew ambulance staffing should allow hospital exit parallel to tPA administration. Pre‐notification to the receiving hospital will allow the EVT staff to be on‐site and ready at patient arrival, facilitating an arrival to arterial puncture time of less than 30 minutes.Certified stroke unit care should be provided in all cases, often initially at the comprehensive stroke centre, before down‐transfer if needed to the primary stroke centre before discharge and/or rehabilitation.
Box 4 – Counterpart barriers to and facilitators for improving national stroke performance
|
Barrier |
Facilitator |
||||||||||||||
|
|
|||||||||||||||
|
Federated health care system could impede coordination |
Healthy state‐based competition |
||||||||||||||
|
Incomplete coverage of hospitals in previous national stroke frameworks |
Stroke Framework update covers all hospitals |
||||||||||||||
|
Incomplete national stroke data coverage |
National stroke registry or audit participation in all states and territories |
||||||||||||||
|
Until 2023, no national stroke dashboard |
Since 2023, national stroke dashboard |
||||||||||||||
|
Currently stroke data are not transparent |
Consumer‐facing transparent data dashboards |
||||||||||||||
|
Lack of key performance indicator prioritisation |
Clearly articulated top five goals |
||||||||||||||
|
Annualised improvement approach |
Target setting with a seven‐year plan timeframe |
||||||||||||||
|
Many stroke organisations with potentially competing priorities (previously) |
Cohesive national stroke organisations unanimously adopting and promoting the national targets:
|
||||||||||||||
|
Until 2022, self‐designated stroke units |
National stroke unit certification initiative |
||||||||||||||
|
Until 2018, only one telestroke network (Victoria) |
National telestroke networks potentially reaching every hospital capable of computed tomography |
||||||||||||||
|
The difficulties of distance and population dispersion |
Innovative neuroimaging being brought to the patient in the ambulance or air ambulance |
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
- 1. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990‐2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 2021; 20: 795‐820.
- 2. Australian Institute of Health and Welfare. Deaths in Australia [website]. Australian Government AIHW, 2023. https://www.aihw.gov.au/reports/life‐expectancy‐deaths/deaths‐in‐australia/contents/leading‐causes‐of‐death (viewed Mar 2024).
- 3. Deloitte Access Economics. The economic impact of stroke in Australia, 2020. https://www.deloitte.com/content/dam/assets‐zone1/au/en/docs/services/economics/dae‐economic‐impact‐stroke‐report‐061120.pdf (viewed Mar 2024).
- 4. Langhorne P, Ramachandra S, Stroke Unit Trialists Collaboration. Organised inpatient (stroke unit) care for stroke: network meta‐analysis. Cochrane Database Syst Rev 2020; 4: CD000197.
- 5. Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta‐analysis of individual patient data from randomised trials. Lancet 2014; 384: 1929‐1935.
- 6. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large‐vessel ischaemic stroke: a meta‐analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723‐1731.
- 7. Meretoja A, Keshtkaran M, Saver JL, et al. Stroke thrombolysis: save a minute, save a day. Stroke 2014; 45: 1053‐1058.
- 8. Meretoja A, Keshtkaran M, Tatlisumak T, et al. Endovascular therapy for ischemic stroke: Save a minute‐save a week. Neurology 2017; 88: 2123‐2127.
- 9. Australian Commission on Safety and Quality in Health Care. Acute stroke clinical care standard. Australian Commission on Safety and Quality in Health Care, 2019. https://www.safetyandquality.gov.au/sites/default/files/2022‐05/Acute‐Stroke‐Clinical‐Care‐Standard‐2019.pdf (viewed Mar 2024).
- 10. Park PSW, Frost T, Tan S, et al. The quest to reduce stroke treatment delays at a Melbourne metropolitan primary stroke centre over the past two decades. Intern Med J 2022; 52: 1978‐1985.
- 11. Cadilhac DA DL, Morrison J, et al. The Australian Stroke Clinical Registry annual report 2022. The Florey Institute of Neuroscience and Mental Health, December 2023. https://auscr.com.au/wp‐content/uploads/2024/03/australian‐stroke‐clinical‐registry‐annual‐report‐2022.pdf (viewed Mar 2024).
- 12. The Swedish Stroke Register. Riksstroke: quality of the Swedish stroke care 2022. Riksstroke – The Swedish Stroke Register, 2023. https://www.riksstroke.org/wp‐content/uploads/2023/12/Arsrapport‐2022‐engelsk‐sammanfattning_final.pdf (viewed Mar 2024).
- 13. Xian Y, Xu H, Smith EE, et al. Achieving more rapid door‐to‐needle times and improved outcomes in acute ischemic stroke in a nationwide quality improvement intervention. Stroke 2022; 53: 1328‐1338.
- 14. Sentinel Stroke National Audit Programme. SSNAP Summary for July ‐ September 2023 admissions and discharges. King's College London, 2023. https://www.strokeaudit.org/Documents/National/Clinical/JulSep2023/JulSep2023‐SummaryReport.aspx (viewed Mar 2024).
- 15. Nogueira RG, Haussen DC, Smith EE, et al. Higher procedural volumes are associated with faster treatment times, better functional outcomes, and lower mortality in patients undergoing endovascular treatment for acute ischemic stroke. Ann Neurol 2023; https://doi.org/10.1002/ana.26803 [online ahead of print].
- 16. Cadilhac DA DL, Morrison J, et al. The Australian Stroke Clinical Registry annual report 2021. The Florey Institute of Neuroscience and Mental Health, December 2022. https://auscr.com.au/wp‐content/uploads/2022/12/auscr‐2021‐annual‐report.pdf (viewed Mar 2024).
- 17. Garcia‐Esperon C, Bladin CF, Kleinig TJ, et al. The acute telestroke model of care in Australia: a potential roadmap for other emergency medical services? Med J Aust 2022; 216: 498‐500. https://www.mja.com.au/journal/2022/216/10/acute‐telestroke‐model‐care‐australia‐potential‐roadmap‐other‐emergency‐medical
- 18. Australian Stroke Coalition. ASC Stroke Unit Certification Project [website]. Australian Stroke Coalition, 2024. https://australianstrokecoalition.org.au/portfolio/certification/ (viewed Mar 2024).
- 19. Stroke Foundation. National acute stroke services framework 2023. Stroke Foundation, 2023. https://informme.org.au/media/xkkfjqm1/national‐acute‐stroke‐services‐framework‐2023.pdf (viewed Mar 2024).
- 20. Australian Stroke Alliance. The plan [website]. Australian Stroke Alliance, 2024. https://austrokealliance.org.au/our‐story/the‐plan/ (viewed Mar 2024).
- 21. Xian Y, Xu H, Lytle B, et al. Use of strategies to improve door‐to‐needle times with tissue‐type plasminogen activator in acute ischemic stroke in clinical practice: findings from target: stroke. Circ Cardiovasc Qual Outcomes 2017; 10: e003227.
- 22. Choi PMC, Tsoi AH, Pope AL, et al. Door‐in‐door‐out time of 60 minutes for stroke with emergent large vessel occlusion at a primary stroke center. Stroke 2019; 50: 2829‐2834.
- 23. Campbell BCV. Optimal Imaging at the primary stroke center. Stroke 2020; 51: 1932‐1940.
- 24. Sarraj A, Goyal N, Chen M, et al. Direct to angiography vs repeated imaging approaches in transferred patients undergoing endovascular thrombectomy. JAMA Neurol 2021; 78: 916‐926.
- 25. Reeves MJ, Fonarow GC, Smith EE, et al. Twenty years of get with the guidelines‐stroke: celebrating past successes, lessons learned, and future challenges. Stroke 2024; 55: 1689‐1698.
- 26. Li Q, Yakhkind A, Alexandrov AW, et al. Code ICH: a call to action. Stroke 2024; 55: 494‐505.
- 27. Kleinig TJ, Abou‐Hamden A, Laidlaw J, et al. Early minimally invasive intracerebral hemorrhage evacuation: a phase 2a feasibility, safety, and promise of surgical efficacy study. J Neurointerv Surg 2024; 16: 555‐558.
- 28. Committee on the Learning Health Care System in America. Best care at lower cost: the path to continuously learning health care in America. Institute of Medicine of the National Academies, The National Academies Press, 2013. https://nap.nationalacademies.org/catalog/13444/best‐care‐at‐lower‐cost‐the‐path‐to‐continuously‐learning (viewed Mar 2024).






Open access:
Open access publishing facilitated by The University of Adelaide, as part of the Wiley ‐ The University of Adelaide agreement via the Council of Australian University Librarians.
Geoff Donnan and Stephen Davis for their helpful manuscript comments. Lachlan Dalli for assistance with the updated AuSCR data trends, and the hospital coordinators who have contributed data via the AuSCR.
No relevant disclosures for named authors. The Angels Initiative (a non‐promotional healthcare project of Boehringer Ingelheim International to improve stroke care around the world) provided support for the 2023 National Stroke Targets 30/60/90 workshop and logistical support surrounding this. The Angels Initiative is a member of the Australian Stroke Coalition taskforce. The Angels Initiative did not propose any target or amendment to any target, and had no input into this manuscript.