The known: There are few examples of effective models to support doctors to remain resilient when training and working in challenging rural, remote and First Nations community contexts.
The new: This realist evaluation developed a comprehensive theory about how the Remote Vocational Training Scheme (RVTS) comprehensively addresses the professional and non‐professional needs of doctors who are training for general practice or rural generalist fellowship while continuously employed in the same rural and remote practices and Aboriginal medical services.
The implications: The theory suggests that the RVTS stimulates five mechanisms that interact to holistically meet the professional and non‐professional needs of rural and remote doctors. The theory may be applicable to other scenarios where the context is similar.
Global recommendations identify the need for rural‐focused, place‐based education and professional support strategies to retain the rural health workforce, including workers with rural service obligations.1 However, there is limited solution‐focused evidence and minimal guidance available to support the design and implementation of strategies for supervising and supporting rural doctors in a way that promotes retention. In this article, we use the case study of Australia's Remote Vocational Training Scheme (RVTS) — a remotely delivered supervision and support model for doctors who remain in the same rural or remote practice for three to four years while progressing towards their general practice or rural generalist fellowship. The RVTS includes practices in communities classified MMM4–7 (Modified Monash Model classification), which all have a population of less than 15 000, and rural Aboriginal medical services (in communities classified MMM2–7) (Box 1).2,3,4
The RVTS achieves more than 80% satisfaction among participants in mainstream surveys,5 more than 90% satisfaction on key items in its anonymous annual registrar satisfaction survey,6 and 78% fellowship completion7. After the mean period of participation of 3.6 years, 49% of participants remain in the community for up to two additional years, which are exemplary outcomes for this context.7,8 Understanding how and why the RVTS supervision and support model (hereafter referred to as the program) succeeds, and under what conditions, is important for developing effective rural workforce strategies.9
The program operates in a challenging context. On average 82% of doctors enrolled in the RVTS since 2013 are international medical graduates, who are subject to rural work moratoriums.4,10 This is due to Australia's reliance on international medical graduates as rurality increases.11 Many international medical graduates are skilled and experienced but encounter frustrations with registration, discrimination, and limited career support.12,13 As a workforce, their satisfaction levels are lower than those of Australian medical graduates, worsened by remoteness (isolation) and moratoriums.14
Doctors participating in the RVTS work in locations characterised by limited infrastructure, higher and more complex caseloads, and distinct cultural, sociological, historical and geographical differences that influence health care dynamics13,15,16,17 The shortage of doctors in these communities necessitates novel training delivery systems like remote supervision (Box 1).18 This could further challenge the capacity for participants to feel adequately supervised and supported.
We aimed to develop theory about how and why the RVTS supervision and support model addresses the professional and non‐professional needs of participating doctors.
Methods
A realist evaluation was done based on the RAMESES II protocol.19 Realist evaluation aims to develop structurally coherent explanations regarding how complex interventions work in relation to the context in which they operate.19,20 The method seeks to articulate interactions between the conditions in which a program is implemented and the social and psychological responses of program participants, to understand how results are achieved. These are referred to as contexts (C), mechanisms (M) and outcomes (O) respectively, frequently expressed as C + M = O or CMO configurations. Configuring these patterns is the basis for generating theory, as the product of realist evaluations. Developing theory informs scalability because it identifies the pivotal mechanisms that need to fire within a context to produce outcomes, providing transferable results.
Initial program theory
Realist evaluation commences with an initial program theory which is developed and refined.20 Situated learning theory, networked ecological systems theory, cultural theory and geographical narcissism theory provided explanations as to why the program addressed the needs of participants (Box 2).21,22,23,25 These were combined into an overarching program theory (CMO pattern) that was refined during four meetings of a 10‐person project reference group (RVTS executive and research team) held in September and October 2023, in which program documentation and wider literature were reviewed.3,4,18,26,27 This theory posited that when participating doctors from diverse backgrounds (internal context [C]), worked in rural, remote practices and rural Aboriginal medical services (external context [C]), and received specific, regular and timely information, resources, advice and networking (program context [C]), their needs were met (outcomes [O]) because they felt valued, connected, confident and competent (mechanisms [M]). Professional and non‐professional needs are both important for the satisfaction and retention of rural doctors and the outcomes were not pre‐defined so they could emerge as part of the theory‐building.1,14,28
Data collection
To develop the theory, we reviewed grey and published literature.3,4,7,8,27 We then worked with a project reference group, which included the RVTS management team, to identify a contact list of potential interviewees with diverse experiences of the program. The study information was emailed to 470 people, including eight RVTS staff, 24 funders and stakeholders, five registrar and supervisor liaison officers, 338 participating doctors (2014–2023 cohorts [105 who were active, 65 who had withdrawn, 168 who had completed]) and 95 current supervisors. Respondents gave written informed consent for participation in an interview and were offered a $60 gift voucher for completing the interview. Semi‐structured interviews that ran for about 45–60 minutes were held in October and November 2023, with interview questions that were shaped by the project reference group to inform development of the initial theory. The questions had been piloted and refined, and they explored each participant's background, work context and perspectives of the supervision and support model (Supporting Information). Two experienced qualitative researchers (one realist trained) conducted the interviews via telephone or video. All respondents were de‐identified using an identification number, and quotes from the interviews are presented with respondent identification numbers and their roles. Interview responses were then used to expand the understanding of CMO patterns.
Analysis
BOS, MM and TG read the interview transcripts and assisted with organising key quotes related to the CMO themes, as a deductive analysis framework.29 Multiple iterative versions of intra‐program comparisons were tested, re‐exploring the data for explanatory theories. Results were discussed at four project reference group meetings (held between November 2023 and February 2024) and two 12‐person stakeholder advisory group meetings (held between December 2023 and February 2024). The latter included a wide group of senior rural health executives with knowledge of Australian rural and remote workforce and training issues to broaden reflections. Meeting insights were recorded and applied to the re‐examination of theory until the updated theory was agreed on in February 2024.
Theory refinement
Following realist standards,19 eight experts in senior management roles, who had detailed knowledge of the RVTS training model (four past and two present RVTS staff, and two rural workforce academic experts), were consulted during separate 30‐minute video consultation meetings (February 2024) to refine the theory until it was confirmed in March 2024. Each expert was provided with a copy of the developed theory before their meeting and asked to provide specific feedback during their meeting, which was recorded as notes. The researchers used the notes to refer to the interview transcripts and verify or confirm the final theory.
Ethics approval
This study received ethics approval from the University of Queensland Human Research Ethics Committee (2023/HE001926, 24 October 2023).
Results
The interview respondents included a mix of sexes, ages, roles (supervisor, participant, staff), and it was noted that past participants often became supervisors or staff (Box 3). The program comprehensively addressed the needs of participating doctors because the contexts of person, place and program triggered five interacting mechanisms: comfort, confidence, competence, belonging and bonding (Box 4). The full theory and its alignment with specific theories from the literature is described in Box 5.21,22,23,25 Testing of the theory confirmed the findings, with only minor refinements to concepts regarding the contexts of person, place and program leading to some modifications in terminology.
Mechanisms
Comfort. This occurred because the diverse participants, having encountered significant challenges, and many based in unfavourable locations relative to the values of mainstream medicine and society, experienced a caring relationship with program staff. The continuity of skilled, locally knowledgeable, humble supervisors, of similar background, built safety: “we are all … experienced rural doctors, we have made our mistakes, none of us have egos” (ID27/staff). This made it possible to disclose and seek help for more complex (undifferentiated) and serious problems without judgement, further enhanced by the supervisor's independence from the participating doctor's practice: “external supervisors so that independent feedback” (ID8/participant); “there's not assumed knowledge” (ID5/staff). Staff understood the local context and valued the importance of rural, remote and Aboriginal medical service medical work, so participants felt able to share challenges related to sustaining practice in their location. This tended to mitigate uncertainty regarding reaching out for help, reducing the emotional strain of carrying problems alone, and providing a sense of being empowered: “RVTS makes you feel comfortable” (ID22/participant); “having the freedom to talk openly about what I was struggling with” (ID26/participant/staff).
Confidence. This was engendered through accessible, personalised, proactive and responsive advice and resources that were relevant, specific and timely. Beyond training, supports included direct help to manage broader conflicts within the practice setting: “my supervisor came down to speak to the senior GPs to get this crisis sorted” (ID22/participant). The quality of support across the program felt reliable: “all of them were able to give me advice and direction that made me feel safe, supported” (ID21/participant). The ability to get help when needed was reinforced by the availability of multiple layered supports to navigate a range of issues: “a … conduit of information flows throughout training … each of those layers of support are so interconnected” (ID5/staff); “you feel like you are working in a system” (ID8/participant). Confidence was also embodied in being able to access help or validate decisions in the context of the breadth of presentations and scenarios within rural, remote and First Nations communities, where it was impossible to know everything and where there are few other people to get help from: “I can't do everything, and I need help” (ID24/participant); “I need to bounce things off someone” (ID16/participant).
Competence. This occurred because participating doctors were able to progress on training milestones and continually up‐skill while remaining in the same practice location: “they were … settled in the practice … they could grow, get more skills and apply it in practice” (ID18/participant/supervisor). The education and training supported participants to address a wide variety of gaps in skills and wider professional capabilities required for being an effective doctor in the practice setting: “medicine in Australia … the country … [and] practising in small towns” (ID27/staff). Training was delivered in regular smaller components with respect that doctors had limited time: “breaking down bigger topics into bite‐sizeable digestible content” (ID5/staff); “there's not much time to study or to see what your peers are up to” (ID18/participant/supervisor). In addition, the delivery could be scaled up or down as required, and this stimulated growing competency: “doing a bit‐by‐bit accumulating [knowledge] … and sail[ing] through [exams]” (ID8/participant).
Belonging. This was prompted because participants who felt isolated, and perceived having lower professional status, found their place in a special professional group with a diversity of respected skills and a commitment to remote and Aboriginal medical service medicine: “I met so many incredible doctors … doing extraordinary things in isolated settings” (ID11/participant). Within this group, participating doctors held power, recognised as skilled practitioners who were encouraged to contribute: “[registrars] probably teach me as much as I teach them” (ID10/supervisor). Registrars were recognised: “I felt seen as an individual and valued in my role that I was doing, not just filling a space” (ID26/participant/staff). Further, they felt valued according to wider social norms: “those two workshops, I felt like a bit of a king … flights and taxi vouchers from airports to hotels” (ID8/participant).
Bonding. This was stimulated because socioculturally isolated doctors and their families were able to meet regularly at twice‐yearly multiday workshops. Participants collaborated and engaged with each other, forging strong social connections with others who had similar values and lived experiences: “We made best friends over the years. We are still connected to the people. It's like a family” (ID11/participant). The break from community and social interaction at the workshops helped participants to feel socially recharged. Participants leveraged the workshop contacts when they returned to the community, reinforcing confidence in getting help when needed: “you have a good bunch of people available, even though it is remote, you can just email them and get an answer” (ID8/participant).
Outcomes
The five mechanisms interlinked to meet professional and non‐professional needs, with comfort, belonging and bonding working together to support non‐professional needs and all the mechanisms playing a part in meeting professional needs (Box 5). Feeling professionally supported emerged as increased professional status, relevant skills, and identity as part of a special community of practice contributing to sustaining access to quality health care in underserviced communities. Non‐professional support emerged as improved access to meaningful social networks regardless of location, and feeling socially recharged and recognised as a member of a whole family unit.
Discussion
In this study, we developed theory about how the RVTS model addresses the professional and non‐professional needs of rural and remote doctors who are expected to remain working in mostly challenging and isolated settings for three to four years while they train towards general practice or rural generalist fellowship. The multilevel theory adds a holistic framework to the wider literature, which has been otherwise limited to describing master–apprentice face‐to‐face supervision30 or blended supervision models, rather than the supportive and learning mechanisms at play.18,26
The developed theory suggests that layered program interventions, tailored to the person and place‐based context of different doctors, stimulate five mechanisms: comfort, confidence, competence, belonging and bonding (Box 4). These interrelate and reinforce each other, and they align with the initial theories from the research literature.21,22,23,25 The mechanisms are triggered within a mostly remote delivery model, but the components delivered, rather than the mode of delivery, were found to drive the outcomes. Thus, through explicit description of how and why the model works, this theory might be a framework that can be applied to face‐to‐face or other remote delivery models specifically for doctors in rural, remote and First Nations communities. This could be most relevant where programs are targeting rural workforce retention and are therefore seeking comprehensive, multilayered designs which address multiple person, place and program challenges to resilience.
The theory identified that the mechanisms overlap to wrap around professional and non‐professional needs. Critically, all the program interventions stimulating non‐professional support affected professional support as well (suggesting that the two are not mutually exclusive phenomena). Hence rural programs should address non‐professional supports if they want to fully meet the needs of cohorts similar to those in this study. Non‐professional factors are often considered non‐adaptive, but our research offers a suite of potentially useful interventions, including caring empathetic staff who validate challenges, opportunities to share difficulties with similar professionals and giving doctors a break from their community.
The theory also suggests that addressing professional needs requires a broader approach than just delivering high quality rural‐focused education programs for skills and competence. In the context of this study, having access to continuity of relatable supervisors generated comfort and a feeling of being understood and respected for the complexity of work. Being able to speak openly to supervisors or program staff is particularly relevant for groups originating from cultures where it is less acceptable to disclose feelings and failures.24 Professional needs were also met because participants felt confident based on receiving calm, specific, high quality and reliable advice through a system of support.
Belonging also positively affected professional needs because it related to increased connections with a motivated and specialised rural community of practice in which learners held a legitimate place (recognition of their background skills, as experienced doctors).16,21 This promoted status and recognition against the trend for rural health workers to be “othered” by a geographical narcissism mindset and for more status to be given to those pursuing narrower, more technical specialisations.25,31 Identity as a generalist doctor has been noted as important in research about rural physicians and there is policy development to promote the recognition of rural generalist medicine as a specialisation within the specialty field of general practice.32,33 Belonging to a workplace and group is also increasingly considered an important factor for workforce retention and mitigation of burnout.34,35 In Australia, having an Australian College of Rural and Remote Medicine Fellowship or an advanced rural practice fellowship equivalent to rural generalist training within the Royal Australian College of General Practitioners is associated with improved rural workforce distribution and scope of work.36 Further research could explore how membership of such groups influences belonging and ongoing rural workforce satisfaction and retention.
Aligned with networked ecological systems theory, the participating doctors felt more resilient when they and their families (microsystems) were connected to resources and social networks (as mesosystems).22 This improved shared understanding of the norms of living and working in remote areas.16 The workshops were a mechanism to value the whole family according to Australian social norms. This is likely to be an enabler for doctors to make the cultural adjustments and overcome sociocultural dislocation, discrimination and a deficit lens of rural places, factors which might otherwise drive volatility.24,25
Given that this theory strongly related to supporting international medical graduates (over 80% of recent participants) who may be on mandatory rural work arrangements,4,7 it could be used to inform models aimed at increasing satisfaction of other doctors on rural service obligations. This is potentially applicable to other programs like the Bonded Medical Program.37 International medical graduates are increasingly used in Australia with plans for expanded access but, as a migrant workforce, they have rights to support and training under a World Health Organization code.11,38,39 It may be useful to apply this theory to a national framework for the inclusion, productivity and safety of rural international medical graduates.
Our study had some limitations. The theory was developed and confirmed with insights from a diverse range of respondents, literature, panels, and experts. However, it requires further adaptation, drawing on the perspectives of a broader range of profession, place and program contexts for more generalisability. Another limitation was that all data collected were positively weighted (despite probing during interviews). Further research could seek to draw out the inhibitors of professional and personal support in this context.
To our knowledge, this study is the first to explore how and why a remotely delivered supervision and support model meets the professional and non‐professional needs of doctors training as general practitioners while continuously based in the same rural, remote and First Nations communities. It identified that five key mechanisms interplay: comfort, confidence, competence, belonging and bonding. Together, these mechanisms produce resilience and build professional identity and status despite the complex and relatively isolated work settings.
Box 1 – The Remote Vocational Training Scheme (RVTS) supervision and support model3
- Australia is a large country in geographical terms, and has had consistent challenges in meeting the needs of distributed communities. In the RVTS, doctors already employed in eligible communities independently apply for and are competitively selected by the RVTS, a national training provider.4
- Doctors enrol and train towards general practice or rural generalist fellowship through the Royal Australian College of General Practitioners and/or the Australian College of Rural and Remote Medicine.
- RVTS supervisors, who have experience in rural and remote practices and Aboriginal medical services and the communities in which participating doctors are training, provide remote supervision. They meet with the participating doctor online for one hour per week for the first six months, then one hour per fortnight for the next six months, and then one hour per month for the remainder of the program.4 They also provide other advice and support as needed via email and phone. Additional standby remote supervisors are also available.
- Each supervisor may support up to two participants depending on learner needs.
- Practice visits and clinical teaching visits are done by supervisors and clinical educators.
- Training reviews are conducted twice yearly by supervisors, training coordinators and medical educator mentors.
- Participants attend weekly webinars (90 structured 60–90‐minute teaching sessions; 80% participation required) in small groups and access online learning materials. They also complete two emergency medicine courses.
- Various online chat groups are used by participants for peer support.
- Participants and families attend two fully funded multiday residential workshops each year (100% attendance required).
- Participants complete a cultural education program and receive support from cultural educators and/or mentors throughout their training.
- RVTS staff and training coordinators act as a point of contact for other matters (eg, arranging emergency support, overseeing processes for emergency case review and discussing procedures).
- Program delivery is governed by RVTS standards and policies.
Box 2 – Theories applied to initial overarching CMO (context–mechanism–outcome) program theory
|
|
|||||||||||||||
|
Situated learning theory: If learning occurs within a place‐based and social context of isolated practice facilitated by remote supervision and support, and the participating doctor becomes part of a community of professionals who share the experience of real‐world rural and remote practice, aided by proximal and relevant resources, then professional needs are met.21 |
|||||||||||||||
|
Networked ecological systems theory: If interconnected mesosystems of participating doctors, their families, practices, supervisors, training coordinators, cultural mentors and a peer group interact to support emerging issues, then professional and non‐professional needs are met.22 Social, personal, professional and educational interactions between various levels of the networked system can influence the experience of the participating doctor and their family. |
|||||||||||||||
|
Cultural theory: If the program reduces the gradient of power between cultures of people and places and reduces uncertainty avoidance while promoting collective practices, then professional and non‐professional needs are met.23 This theory has been applied to international medical graduates transitioning to western practice24 and could equally support adjustment to working and training in rural, remote and First Nations communities, acknowledging that every place has its own culture(s). |
|||||||||||||||
|
Geographical narcissism theory: If the program increases the professional and non‐professional recognition of doctors working in challenging rural, remote and First Nations communities, then the differential status allocated to rural compared with metropolitan work is mitigated and professional and non‐professional needs are met.13,25 |
|||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – Characteristics of the 27 interview respondents
|
|
Number (%) |
||||||||||||||
|
|
|||||||||||||||
|
Sex |
|
||||||||||||||
|
Women |
18 (67%) |
||||||||||||||
|
Men |
9 (33%) |
||||||||||||||
|
Age group (years) |
|
||||||||||||||
|
30–49 years |
15 (56%) |
||||||||||||||
|
≥ 50 years |
12 (44%) |
||||||||||||||
|
Role* |
|
||||||||||||||
|
Supervisor |
11 (37%) |
||||||||||||||
|
Participating doctor |
14 (47%)† |
||||||||||||||
|
Remote Vocational Training Scheme board member or staff |
5 (17%) |
||||||||||||||
|
Location |
|
||||||||||||||
|
Australian Capital Territory or New South Wales |
9 (33%) |
||||||||||||||
|
Queensland |
8 (30%) |
||||||||||||||
|
Other |
10 (37%) |
||||||||||||||
|
|
|||||||||||||||
|
* Multiple roles possible; percentages indicate percentage of all 30 roles. † Five current participating doctors (two Australian medical graduates, three international medical graduates) and nine past participants (all international medical graduates). |
|||||||||||||||
Box 4 – Mechanisms firing to achieve holistic professional and non‐professional support of doctors training as general practitioners in the same rural or remote practice*
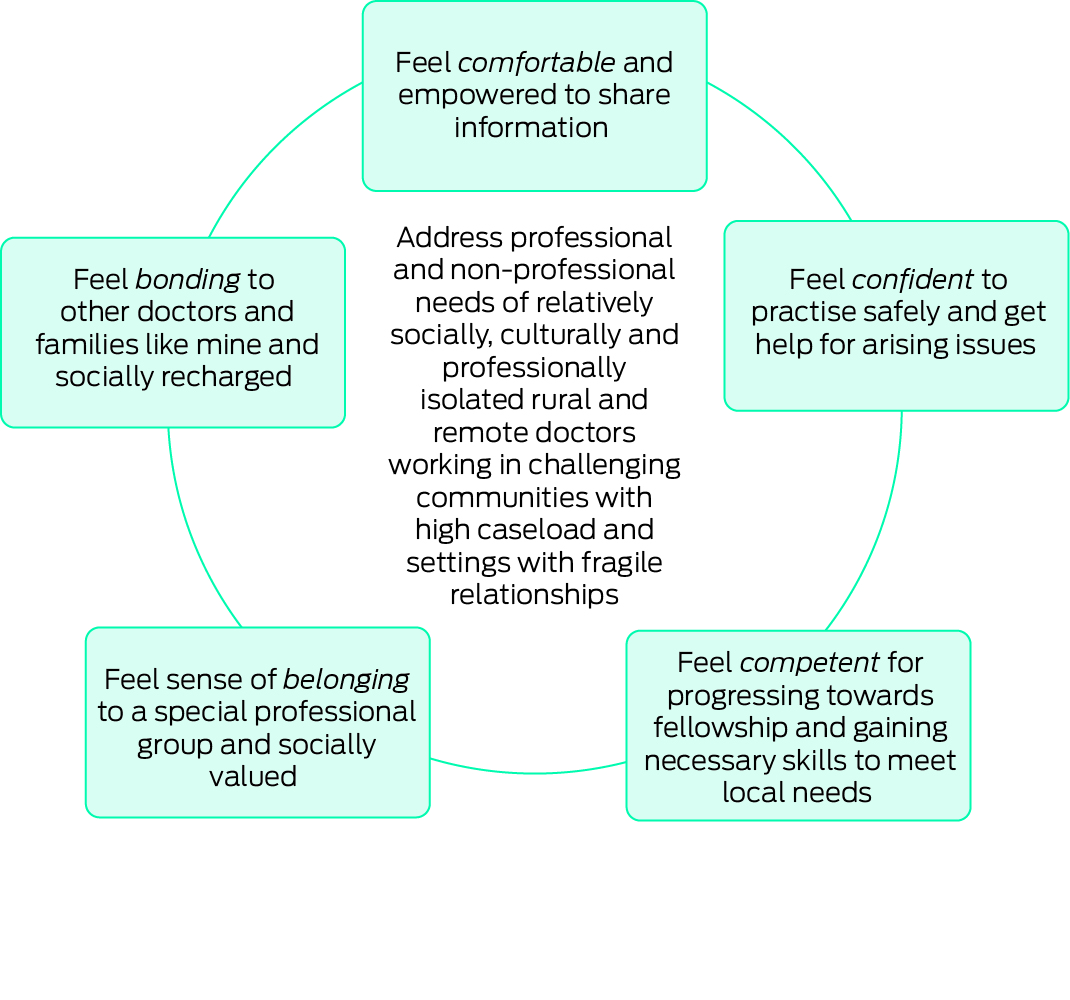
* More detail about how the mechanisms fire (full theory) is depicted in Box 5.
Box 5 – Full theory about how and why the professional and non‐professional needs of doctors training as general practitioners in the same rural or remote practice are met*
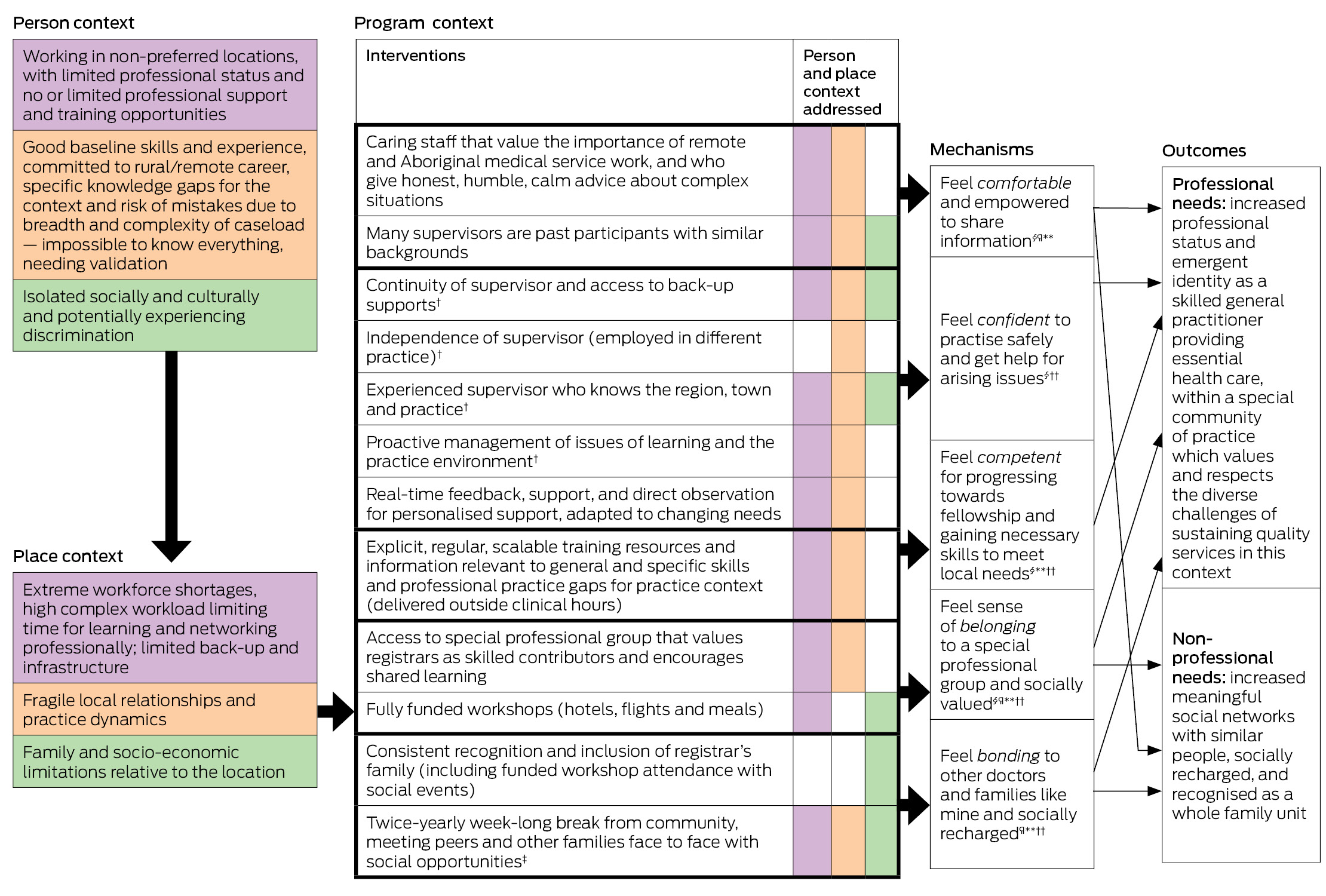
* Shaded colours show direct alignment between person and place contexts and program context. † Also impacts feeling comfortable. ‡ Also impacts feeling confident because participants access peer support from each other online once they have connected at workshops. § Situated learning theory. ¶ Cultural theory. ** Geographical narcissism theory. †† Networked ecological systems theory.
Provenance: Not commissioned; externally peer reviewed.
Received 14 May 2024, accepted 9 August 2024
- Belinda G O'Sullivan1,2
- Patrick Giddings3,4
- Ronda Gurney3
- Matthew R McGrail5
- Tiana Gurney1
- 1 Rural Clinical School, University of Queensland, Toowoomba, QLD
- 2 School of Rural Health, Monash University, Bendigo, VIC
- 3 Remote Vocational Training Scheme, Albury, NSW
- 4 Rural Clinical School, University of New South Wales, Albury, NSW
- 5 Rural Clinical School, University of Queensland, Rockhampton, QLD
Open access:
Open access publishing facilitated by The University of Queensland, as part of the Wiley ‐ The University of Queensland agreement via the Council of Australian University Librarians.
Data sharing:
The de‐identified data we analysed are not publicly available, but we will seek to provide data through requests to the corresponding author which will be considered on a case‐by‐case basis.
The Remote Vocational Training Scheme is supported by funding from the Australian Government. Executive and senior leaders at the Rural Doctors Association of Australia, Australian College of Rural and Remote Medicine, Royal Australian College of General Practitioners, General Practice Supervision Australia, General Practice Registrars Australia, New South Wales Rural Doctors Network, and individuals including Jenny May (University of Newcastle) and Susan Wearne (Australian National University) contributed insights through a stakeholder advisory group and the expert review of the theory. Others including Greg Gladman (Australian College of Rural and Remote Medicine), Karin Jodlowski‐Tan (Royal Australian College of General Practitioners) and RVTS staff including Murray Towne, Clara Smith, Tony Trevaskis, Marlene Drysdale and Veeraja Uppal, along with an RVTS associate researcher, Taras Mikulin, contributed to data collection, interpretation of the findings and/or expert review of the theory.
The researchers were engaged by the RVTS through funds from the Australian Government Department of Health and Aged Care. The funder was involved in the project reference group but we worked independently.
- 1. World Health Organization. Increasing access to health workers in remote and rural areas through improved retention. Geneva: WHO, 2010. https://iris.who.int/bitstream/handle/10665/44369/9789241564014_eng.pdf?sequence=1 (viewed Aug 2024).
- 2. Department of Health and Aged Care. Modified Monash Model. 2023. https://www.health.gov.au/topics/rural‐health‐workforce/classifications/mmm (viewed Aug 2024).
- 3. Remote Vocational Training Scheme Ltd. Training program. 2024. https://www.rvts.org.au/rvts‐training‐program (viewed Aug 2024).
- 4. Giddings P, O'Sullivan B, McGrail M, et al. Australia's Remote Vocational Training Scheme: training and supporting general practitioners in rural, remote and First Nations communities. Med J Aust 2024; 221 (Suppl): S3‐S8.
- 5. Medical Board of Australia; Australian Health Practitioner Regulation Agency. Medical Training Survey [website]. Melbourne: MBA and AHPRA, 2024. https://www.medicaltrainingsurvey.gov.au (viewed Aug 2024).
- 6. Remote Vocational Training Scheme Ltd. Outcomes and research. https://www.rvts.org.au/outcomes‐research (viewed Aug 2024).
- 7. McGrail M, O'Sullivan B, Giddings P. Continuity of service and longer term retention of doctors training as rural general practitioners in the Remote Vocational Training Scheme. Med J Aust 2024; 221 (Suppl): S9‐S15.
- 8. Wearne S, Giddings P, McLaren J, et al. Where are they now? The career paths of the Remote Vocational Training Scheme registrars. Aust Fam Physician 2010; 39: 53‐56.
- 9. Australian Government Department of Health and Aged Care. National Medical Workforce Strategy 2021–2031. 2024. https://www.health.gov.au/our‐work/national‐medical‐workforce‐strategy‐2021‐2031 (viewed Aug 2024).
- 10. Australian Government Department of Health and Aged Care. 10‐year moratorium and scaling. 2021. https://www.health.gov.au/topics/doctors‐and‐specialists/what‐we‐do/19ab/moratorium (viewed Aug 2024).
- 11. O'Sullivan B, Russell DJ, McGrail MR, et al. Reviewing reliance on overseas‐trained doctors in rural Australia and planning for self‐sufficiency: applying 10 years’ MABEL evidence. Hum Resour Health 2019; 17: 8.
- 12. Marcus K, Purwaningrum F, Short S. Towards more effective health workforce governance: the case of overseas‐trained doctors. Aust J Rural Health 2021; 29: 52‐60.
- 13. Gilles MT, Wakerman J, Durey A. “If it wasn't for OTDs, there would be no AMS”: overseas‐trained doctors working in rural and remote Aboriginal health settings. Aust Health Rev 2008; 32: 655‐663.
- 14. McGrail M, Humphreys J, Joyce C, et al. International medical graduates mandated to practise in rural Australia are highly unsatisfied: results from a national survey of doctors. Health Policy 2012; 108: 133‐139.
- 15. McGrail MR, Humphreys JS, Joyce CM, et al. How do rural GPs’ workloads and work activities differ with community size compared with metropolitan practice? Aust J Prim Health 2012; 18: 228‐233.
- 16. Konkin J, Grave L, Cockburn E, et al. Exploration of rural physicians’ lived experience of practising outside their usual scope of practice to provide access to essential medical care (clinical courage): an international phenomenological study. BMJ Open 2020; 10: e037705.
- 17. Wakerman J, Bourke L, Humphreys J, Taylor J. Is remote health different to rural health? Rural Remote Health 2017; 17: 3832.
- 18. Wearne S, Dornan T, Teunissen PW, et al. Twelve tips on how to set up postgraduate training via remote clinical supervision. Med Teach 2013; 35: 891‐894.
- 19. Wong G, Westhorp G, Manzano A, et al. RAMESES II reporting standards for realist evaluations. BMC Med 2016; 14: 96.
- 20. Pawson R, Tilley N. Realistic evaluation. 1st ed. London: SAGE Publications, 1997.
- 21. Lave J, Wenger E. Situated learning: legitimate peripheral participation. Cambridge: Cambridge University Press, 1991.
- 22. Neal JW, Neal ZP. Nested or networked? Future directions for ecological systems theory. Soc Dev 2013; 22: 722‐737.
- 23. Hofstede G. Culture's consequences: comparing values, behaviors, institutions and organizations across nations. 2nd ed. Thousand Oaks: Sage Publications, 2001.
- 24. Morrow G, Rothwell C, Burford B, et al. Cultural dimensions in the transition of overseas medical graduates to the UK workplace. Med Teach 2013; 35: e1537‐e1545.
- 25. Fors M. Geographical narcissism in psychotherapy: countermapping urban assumptions about power, space, and time. Psychoanal Psychol 2018; 35: 446‐453.
- 26. Martin P, O'Sullivan B, Taylor C, et al. Blended supervision models for post‐graduate rural generalist medical training in Australia: an interview study. BMC Med Educ 2022; 22: 478.
- 27. Wearne S. General practice supervision at a distance—is it remotely possible? Aust Fam Physician 2005; 34: 31‐33.
- 28. McGrail MR, Russell DJ, O'Sullivan BG. Family effects on the rurality of GP's work location: a longitudinal panel study. Hum Resour Health 2017; 15: 75.
- 29. Braun V, Clark V, Hayfield N, et al. Thematic analysis. In: Liamputtong P, editor. Handbook of research methods in health social sciences. Singapore: Springer Nature, 2019.
- 30. O'Sullivan B Hickson H, Kippen R, et al. Exploring attributes of high‐quality clinical supervision in general practice through interviews with peer‐recognised GP supervisors. BMC Med Educ 2021; 21: 441.
- 31. McGrail M, O'Sullivan B, Russell D. Rural work and specialty choices of international students graduating from Australian medical schools: implications for policy. Int J Environ Res Public Health 2019; 16: 5056.
- 32. Ostini R, McGrail M, Kondalsamy‐Chennakesavan S, et al. Building a sustainable rural physician workforce. Med J Aust 2021; 215(1 Suppl): S1‐S33. https://www.mja.com.au/journal/2021/215/1/building‐sustainable‐rural‐physician‐workforce
- 33. Worley P, O'Sullivan B, Ellis R. From locum‐led outposts to locally led continuous regional learning networks: the National Rural Generalist Pathway. Med J Aust 2019; 211: 57‐60. https://www.mja.com.au/journal/2019/211/2/locum‐led‐outposts‐locally‐led‐continuous‐rural‐training‐networks‐national‐rural
- 34. Silver JK, Ellinas E, Augustus‐Wallace A. Sense of belonging is a critical component of workforce retention [editorial]. BMJ 2024; 384: q392.
- 35. Yewande A, Altieri MS, Kauffman JD, et al. A sense of belonging and community can mitigate physician burnout. Chicago: American College of Surgeons, 2019. https://www.facs.org/for‐medical‐professionals/news‐publications/news‐and‐articles/bulletin/2019/08/a‐sense‐of‐belonging‐and‐community‐can‐mitigate‐physician‐burnout (viewed Aug 2024).
- 36. McGrail M, O'Sullivan B. Faculties to support general practitioners working rurally at broader scope: a national cross‐sectional study of their value. Int J Environ Res Public Health 2020; 17: 4652.
- 37. Australian Government Department of Health and Aged Care. Bonded Medical Program. 2024. https://www.health.gov.au/our‐work/bonded‐medical‐program (viewed Aug 2024).
- 38. Kruk R. Independent review of Australia's regulatory settings relating to overseas health practitioners. Final report. Canberra: Australian Government Department of Finance, 2023. https://www.regulatoryreform.gov.au/priorities/health‐practitioner‐regulatory‐settings‐review (viewed Aug 2024).
- 39. World Health Assembly, 63. WHO global code of practice on the international recruitment of health personnel (World Health Assembly sixty‐third session, agenda item 11.5, document number WHA63.16). Geneva: World Health Organization, 2010. https://iris.who.int/bitstream/handle/10665/3090/A63_R16‐en.pdf?sequence=1&isAllowed=y (viewed Aug 2024).






Abstract
Objective: To develop theory about how and why the supervision and support model used by the Remote Vocational Training Scheme (RVTS) addresses the professional and non‐professional needs of doctors (including many international medical graduates) who are training towards general practice or rural generalist fellowship while based in the same rural or remote practice.
Design, setting, participants: We conducted a realist evaluation based on the RAMESES II protocol. The initial theory was based on situated learning theory, networked ecological systems theory, cultural theory and geographical narcissism theory. The theory was developed by collecting empirical data through interviews with 27 RVTS stakeholders, including supervisors, participants and RVTS staff. The theory was refined using a project reference and a stakeholder advisory group and confirmed using individual meetings with experts.
Main outcomes measures: Theory about how the contexts of person, place and program interacted to address professional and non‐professional needs.
Results: The RVTS program offers remote access to knowledgeable and caring supervisors, real‐time tailored advice, quality resources and regular professional networking opportunities, including breaks from the community. It worked well because it triggered five mechanisms: comfort, confidence, competence, belonging and bonding. These mechanisms collectively fostered resilience, skills, professional identity and improved status; they effectively counteracted the potential effects of complex and relatively isolated work settings.
Conclusion: This theory depicts how a remotely delivered supervision and support model addresses the place and practice challenges faced by different doctors, meeting their professional and non‐professional needs. The participants felt valued as part of a special professional group delivering essential primary health care services in challenging locations. The theory could be adapted and applied to support other rural and remote doctors.