The Australian health care system has an urgent sustainability challenge. It generates 236 million kilograms of waste per year,1 making it one of the largest contributors to waste nationwide. In Australia between 2014 and 2015, 235 000 kg of carbon dioxide was produced per day from the incineration of hazardous waste.2 This is of great concern since the World Health Organization (WHO) declared in 2021 that “climate change is the biggest health threat facing humanity”.3
Operating rooms are a hotspot for greenhouse gas (GHG) emissions as they generate at least 20% of the total waste produced in hospitals.4 Worldwide, the number of operations has been increasing every year by 15% since 1992, resulting in an increase in the amount of annual waste produced.5 Besides the number of surgeries increasing, the other reasons for this dramatic increase in waste is the rise of minimally invasive surgeries, such as laparoscopic and robotic surgeries, the need to improve sterile processing,6 and the use of single‐use devices (SUDs).7
All waste increases carbon dioxide emissions.8 However, general non‐hazardous waste, which makes up 85% of hospital waste,9 does not contribute directly to GHG emissions unless incinerated.10 Nevertheless, this general waste still contributes to GHG emissions through the manufacturing process10 and through being disposed of incorrectly as infectious waste that requires incineration.11 This review examines the environmental end points of a linear economy of health care waste. Additionally, there is a global call for health care waste systems to transition from a linear to a circular economy.12 As Australia transitions away from coal and towards a renewable energy electricity grid, opportunities for a circular economy of health care waste will emerge. Therefore, this review also examines environmentally preferable purchasing of reusable and reprocessed devices.
There are a variety of frameworks and strategies proposed to reduce operating room waste. In Australia, the 2018 National Waste Policy (NWP)13 provides a framework to guide investments and sustainable action by businesses, governments, communities, and individuals. The National Waste Policy Action Plan (NWPAP), agreed on in 2019, includes five circular economy principles to implement the 2018 NWP: avoiding waste, improving resource recovery, increasing use of recycled material, better managing material flows, and improving information to support innovation, guide investment and enable informed consumer decision making.14 However, translating these general strategies to scalable implementation in health care has its challenges. An audit conducted by the Australian National Audit Office found that the implementation of the NWPAP has been only partly effective.15
A major challenge to scalable waste reduction strategies was the physical limits of recycling, in that nothing is 100% recyclable.16 Another critical challenge is the “tragedy of the commons”,17 in that hospitals might need to invest large amounts of money to reduce operating room waste, even if that individual hospital is not significantly contributing to the problem. A further challenge is that despite policies to promote waste reduction, these are not considered a priority when compared with key ethical concerns such as reducing patient harm.5,18,19,20 A final challenge is the presence of an external force in the form of policies that have taken the onus off surgeons to drive sustainable change.7,21 There is no comprehensive review of these barriers and potential strategies for overcoming them.
Through a review and thematic analysis of the literature, this narrative review assesses the current strategies adopted in the operating room to reduce waste and provides an in‐depth analysis of the barriers to scalable waste reduction strategies. It also explores the knowledge gaps in the current NWP and uses this framework to guide policy and practice implications of the findings.
Search strategy
This narrative review used a systematic search strategy method. That is, a review of evidence based on a clearly formulated question that uses systematic and rigorous methods to select and critically appraise primary research.22 Systematic search strategies have been used in similar studies7,17,18,23,24,25,26,27,28,29,30,31 because they provide an opportunity to identify research gaps in our understanding of sustainability initiatives in hospitals and can be used to improve future research and policies in this area.32
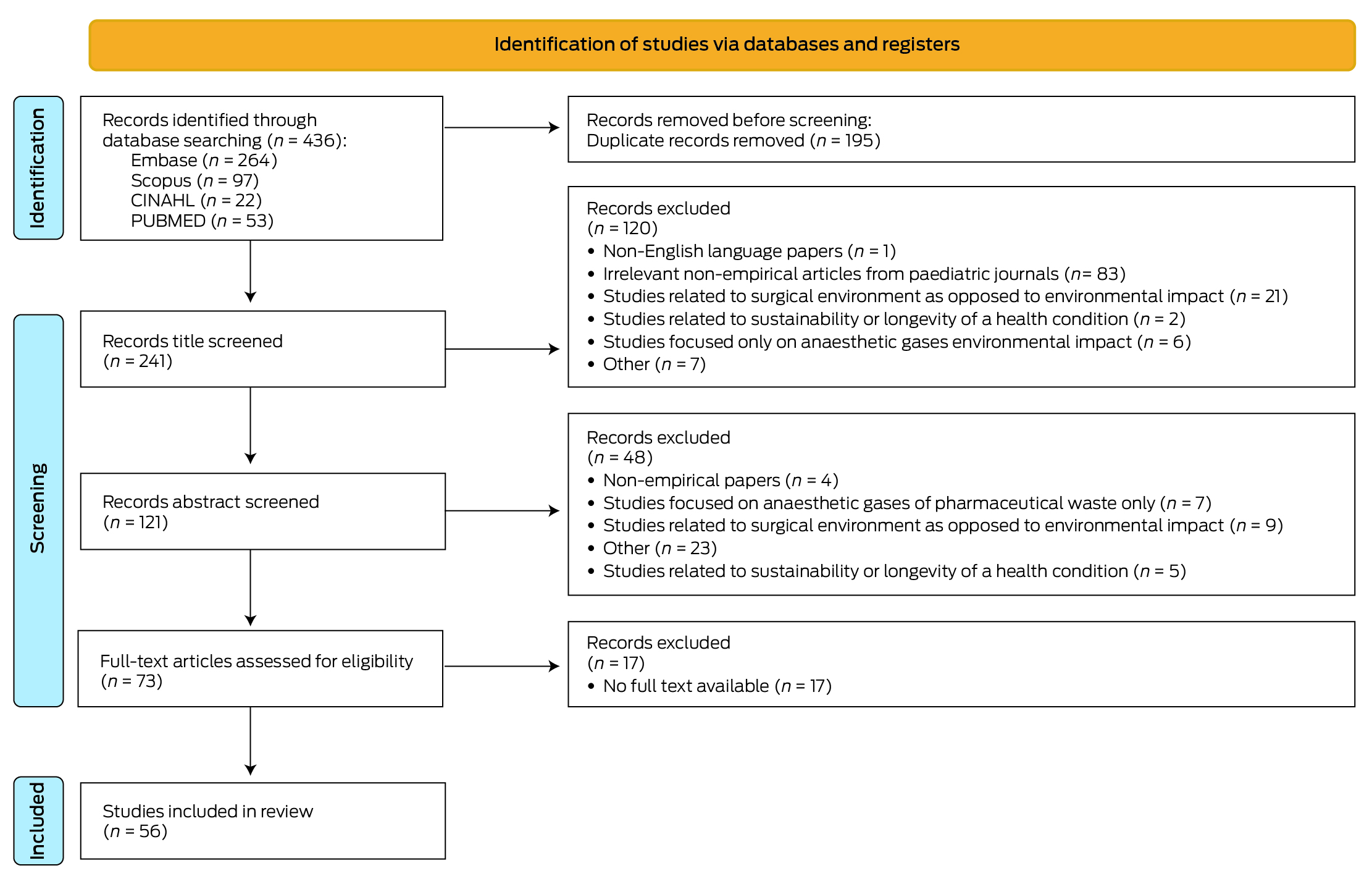
A literature search was conducted in early 2023 by one author (LP) using Embase, Scopus, PUBMED and CINAHL databases to identify articles on operating room waste management. These databases were chosen because they provide access to a breadth of research across the medical and social sciences. The final keywords used for the search were: surgery, waste and plastic. Further details of the search strategy are provided in the Supporting Information. Authors TK and KW reviewed the search results and screening decisions. In the initial search, 436 articles were identified, with that reduced to 56 once the inclusion and exclusion criteria were applied. The Box shows how studies were screened and selected for this narrative review, using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses) method.
A focus on the environmental impact of surgical waste in the operating room was part of the inclusion criteria. Studies on the environmental impact of anaesthetic gases and other pharmaceutical wastes were omitted.
We used a deductive thematic synthesis approach to analyse the included studies.33 This involved identifying a framework of themes in advance to guide literature exploration.34 The framework selected was the 2018 NWP,13 which included circular economy, waste hierarchy and strategies. From here, using the method suggested by Popay and colleagues,35 studies were reviewed and elements of the results and discussion aligning to the NWP were tabulated. These tables were used, in discussion with the research team, to identify patterns and common themes across the included studies. Thematic analysis of the 56 studies led to the identification of strategies used to promote waste management in the operating room and key barriers to implementing these strategies. Further details on methodology are provided in the Supporting Information.
Strategies implemented in the operating room to reduce waste
Avoiding products that have a large carbon footprint
Reducing waste production in the operating room begins with thoughtful and environmentally conscious purchasing practices. Hospitals should use environmentally preferable purchasing (EPP) practices, which prioritises products with minimal negative environmental and human health impacts, and long term economic benefits.17,21,23,24,25,36,37 Environmental stewardship organisations, such as Practice Greenhealth, have produced guidelines to support large medical systems to implement EPP practices.17,21,24 Additionally, such teams can coordinate hospital waste audits, which will further inform and guide EPP practices.24,36,37
Reducing waste through correct waste segregation and reducing overage
Targeting waste segregation in the hospital is a crucial step in mitigating the carbon footprint. In 2018, the WHO found that only 15% of health care waste was hazardous.9 However, Lee and colleagues5 found that 73% of operating room waste was disposed of as hazardous waste. Most of this waste was incorrectly disposed of as it did not meet the Environmental Protection Authority (EPA) definition of hazardous waste.38 Hazardous waste requires further disposal steps, including incineration, which generates substantial GHG emissions and costs for the hospital. Three studies identified ways to improve waste segregation, including replacing an infectious waste bin with a general waste bin,5 having a smaller hazardous waste bin,21 and clearly documenting the waste generated at the end of the procedure.39 Improving waste segregation processes can reduce the amount of operating room hazardous waste significantly.
Additionally, a key driver of operating room waste is “overage”.18,20,40 Overage refers to surgical items that are opened but unused and need to be thrown away. Several strategies to reduce overage include surgeon preference cards, surgeon waste score cards,24,25 minimal surgical packs,26,40 the “time‐out” strategy, and donating overage items to developing countries.37 The “time‐out” strategy uses the time before an operation to communicate which high cost equipment needs to be opened.21
Reusing, reprocessing and repurposing devices to reduce waste from single‐use items
Most operating room waste comes from disposable surgical supplies, such as table covers, surgical drapes, face masks and packaging, such as sterilised wraps.41 Switching from a disposable item to a reusable device reduces waste production, GHG emissions and costs.5,42 Moreover, where reusing equipment is not possible, hospital engagement with a third party SUD reprocessing organisation has been suggested.5,17,27,28,36,43,44,45 Wu and colleagues18 discussed repurposing devices as another strategy to keep the material within the circular economy. This was demonstrated in two studies that repurposed polypropylene in blue wrap and polyvinyl chloride (PVC) in plastic into medical devices46 and industrial materials21 respectively.
Improving recycling to reduce landfill and hazardous waste
Operating room strategies to improve recycling included implementing single stream recycling,27 installing specific paper and plastic recycling bins,29 and investing in a blue wrap recycling vendor16 and a polyethylene terephthalate recycling vendor.47 The benefits of recycling plastic have been demonstrated by the Vinyl Council of Australia and Baxter, who both recycle PVC plastics,48 which contribute 23% to the total volume of plastics used in the operating room.4 Through these methods, recycling increased by at least 50%49 and carbon emissions were reduced significantly.16
Barriers to strategies to reduce operating room waste
Surgeons’ perceived risk of harming their patients through waste minimising strategies
A significant factor impeding surgeons from adopting waste reduction strategies is the ethical pillar of “do no harm”.11,19,30,31,50 A major concern surgeons have been documented to have is fear of infection transmission. Chiu and colleagues50 found that this concern was reinforced by the COVID‐19 pandemic. Another documented concern is the downstream impacts of the perceived increased risk of infection, including increased cost to patients due to longer hospital stays.35 Additionally, surgeons might perceive better performance of single‐use products compared with reprocessed SUD.19,31 The final concern we identified was patient autonomy, as the United States Food and Drug Administration (FDA) does not require a patient to be notified about the use of reprocessed SUD.31
Ineffective or insufficient waste education
A significant barrier to waste management appears to be inadequate or insufficient waste education.7,18,51,52,53 Current education fails to incorporate the role of the regulators in approving reprocessed devices,31 the EPA guidelines for waste segregation,15 the environmental benefits of waste management,23,24,54,55 and the economic burden of surgical items.17,21,26,29,56 Moreover, most education is not mandatory and ongoing, which are both required for it to be effective.57,58
Delay in economic and environmental benefits
A key barrier identified was the delayed economic and environmental benefits from reusing and reprocessing devices.11,17,19,24,59 Regarding the costs of implementing reprocessed SUD, Lee and colleagues5 found a prominent concern was manufacturers not accepting liability for equipment containing reprocessed parts. Regarding GHG emissions, Papadopoulou and colleagues25 and McGain and colleagues60 found that reprocessed devices require extra steps in their life cycle that generate a larger carbon footprint than SUD. Similarly, Friedericy and colleagues61 found reusable devices also require extra steps that incur extra costs and carbon emissions. Furthermore, Majernik and colleagues30 highlighted that as the expiration time of reusables is much shorter than disposables, these processes need to be repeated whether the product has been used or not. McGain and colleagues62 found that the immediate costs and GHG emissions to create a circular economy were significantly greater in Australia as 75% of the country's electricity is generated from coal.
Lack of systemic policies and regulations governing waste management
A significant barrier to effective waste management is successful implementation of policies and regulations.7,18,28,63,64 Wyssusek and colleagues7 and Weiss and colleagues21 found that surgeons relied on an external source, such as government policies or laws, to enforce strategies for waste reduction. There is a lack of facility regulations and support from hospital administration,19,53,54 which is a crucial barrier to improving waste management.
Translating results into practice and policy
This review aimed to comprehensively analyse waste management strategies in operating rooms and consider gaps in current practices that can be a target for future improvements. The 2018 NWP framework is not specific to health care but guided the analysis to identify opportunities for how it can be applied in the operating room. The four strategies identified were categorised according to the NWP waste hierarchy, and the barriers identified were categorised based on the NWP proposed strategies. Four barriers were identified, including current surgical interpretation of the ethical pillar of “do no harm”; insufficient and ineffective waste education; delayed economic and environmental benefits from reducing waste; and lack of systemic regulations and policies to enforce strategies. Three knowledge gaps were identified, including lack of data, particularly life cycle analyses (LCAs); lack of standardised regulations and policies; and lack of methods to create behavioural change.
The findings of this review provide key insights for the design and implementation of the NWP. The following proposed improvements to the 2018 NWP should increase the framework's usefulness in reducing waste in health care, particularly in operating rooms. This is of significance as several studies revealed national policies and guidelines have a major role in enacting change.7,21,28,63
Incorporating initiatives or incentives in the NWP to promote more standardised LCAs will increase adoption of waste reduction methods as it enhances the transparency and accuracy of measuring progress in the NWP. LCAs can reveal the number of cycles a reusable or reprocessed device takes to achieve the financial break‐even point. This is illustrated by Friedericy and colleagues61 who found that despite initially incurring extra costs, hard sterile containers reached the financial break‐even point after 67 cycles, compared with blue wrap. Therefore, information from LCA research, such as the break‐even point, is a key consideration when purchasing products and driving EPP. Furthermore, how LCAs are conducted is not always standardised, making study comparisons difficult. For example, in the Meissner and colleagues study,65 sterilisation of the multiuse device was not included, yet it contributed significantly to water use and GHG emissions.25,39 Therefore, standardising LCA research has the potential to substantially improve hospital EPP.
Involving regulatory bodies in reporting and releasing data on product performance will likely improve the NWP practicality in operating rooms. Comprehensive policies play a large role in surgeon compliance with waste management strategies.19,21,54 In Australia, the Department of Climate Change, Energy, the Environment and Water is the regulatory body that prepared the NWP. However, a foreseeable issue is that the current regulations are not specific to health care, nor address the concerns of surgeons. Therefore, there is a need for research to assess the perceived risk of infection transmission with reusable instruments and performance benefits of SUD. Additionally, releasing a list of verified reprocessing services for hospitals in Australia, similar to what is done by the FDA in the United States, is an opportunity to standardise regulations and encourage surgeons to adopt waste management policies.
Finally, specifying the need for continuous, mandatory education in hospitals, led by a dedicated “green team” might improve the framework to encourage behavioural change. A green team is ideally a committed team from multiple disciplines to drive bottom‐up sustainability initiatives. Despite the desire to participate in waste management strategies, Meyer and colleagues63 found that of the 95% of 2019 respondents who agreed to change operating room workflow to reduce waste, 67% believed their colleagues were unaware of the environmental crisis. This might be overcome with a collaborative, multidisciplinary green team to prioritise and facilitate change7,17,18,60,66 at the level of the surgeon.
How these results reflect the broader literature on sustainable health care
Interest in sustainable health care has grown globally in recent years.67 Despite varying definitions, a common thread is that sustainable health care enables a health care system to respond to immediate priorities while also addressing long term cultural, social, economic, and ecological interests.68 A major barrier identified in broader literature on sustainable health care, and one identified in this narrative review, is interpretation of the Hippocratic principle of “first, do no harm”. This is a pledge taken by doctors to balance the risks and benefits of treatments.69 This concept is usually part of the relationship a clinician has with an individual, rather than a clinician's relationship with communities and the environment. However, Lee70 described that there has been a shift from individual‐based biomedical ethics to public health ethics that broadens clinicians’ concerns to do no harm on an individual, community and environmental level. Therefore, instead of surgeons thinking solely about the immediate consequences for their patients, such as risk of infection, Sherman and Ryan71 urge health care stakeholders to think more broadly about this principle and rethink their roles and responsibilities to incorporate planetary and global human health. This might require sustainability to be incorporated into medical training, guidelines and professional body requirements.72,73
The Sustainable Healthcare Facilities (SHF) framework74 provides an approach to integrate sustainability goals into health care facilities. The four dimensions of the SHF framework (environmental, economic, social and health‐related) align with the results of this narrative review. Firstly, environmental sustainability is measured through pollution and consumption of natural resources75 such as waste management, renewable energy, green materials, and carbon emission reduction. These results reflect waste management in the form of segregation, green materials through reusable materials and custom surgical packs, and carbon emission reductions through reprocessed and repurposed devices. Secondly, economic sustainability refers to the long term economic growth.76 The opportunity identified to increase LCA research could play a key role in estimating life cycle costs, break‐even points and risk management, which can increase sustainable economic growth of the health facility. Thirdly, the social sustainability dimension aims to provide comfortable user‐friendly equipment and environments that are safe and accessible to patients and staff.48 Having a dedicated green team to address staff concerns, and to facilitate the introduction of green materials, is recommended from this narrative review. Finally, the aforementioned three dimensions all impact on human health, including health‐related conditions, costs and patient satisfaction. These results demonstrate that by improving economic, environmental and social dimensions in the health care facility, the resultant reduction in greenhouse gas emissions will positively impact human health. However, this analysis does not address the additional barriers of accessibility to these strategies in low‐ and middle‐income countries (LMICs).
Health care quality and access is improving in LMICs;23 therefore, total emissions from surgery are set to increase. Hence the planetary and global health conundrum of reducing emissions in these countries without affecting access to health care through increased initial costs and resources. Focusing solely on decreasing emissions in health care will have negative implications for these countries and should not be the aim of sustainability frameworks. Instead, tailored, local training programs on sustainable surgical practices should be encouraged, as well as engagement with national and international political leaders to incentivise sustainability education in health care systems.77 In the broader literature on sustainable health care, inherent systemic barriers in LMICs are commonly cited for low sustainable research output including lack of funding, research training and culture of research.78
Strengths and limitations
Only one of the included studies considered the impact that the COVID‐19 pandemic might have on single‐use waste. The pandemic exacerbated the need for infection control and, therefore, the barrier of “do no harm” may have become more significant. More evidence on surgeons’ perspectives during the pandemic is required to understand how their behaviours and perspectives towards infection transmission have changed. The second limitation was having only one author screen and analyse the evidence. Although all the authors reviewed the screening decisions, having multiple authors reviewing each paper would have improved the reliability and reproducibility of results, and minimised bias. The third limitation is that other narrative reviews were included as references, meaning the detail of the findings of those publications, including the limitations of the included studies, may not be reflected in our results. Finally, generalisation to Australia is limited as only five studies were undertaken in Australia.
Conclusion
For policy makers, this narrative review reveals the gaps in the current frameworks, such as Australia's 2018 NWP framework. For researchers, future research should be directed at executing more standardised LCAs that include every aspect of the product life cycle, to understand the economic and environmental implications of waste reduction strategies. For surgeons, this review emphasises the significant role they can play, together with a green team, to fight the biggest health threat facing humanity – climate change.
Provenance: Not commissioned; externally peer reviewed.
- Ludmilla Pillay1
- Kenneth D Winkel2
- Timothy Kariotis1
- 1 University of Melbourne, Melbourne, VIC
- 2 Centre for Health Policy, University of Melbourne, Melbourne, VIC
Open access:
Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
We would like to acknowledge Forbes McGain (Western Health, Melbourne) for his invaluable knowledge and support on this research.
No relevant disclosures.
- 1. Foran P. Education report. ACORN: The Journal of Perioperative Nursing in Australia. 2015; 28: 28‐30.
- 2. Australian Institute of Health and Welfare. Hospital resources 2015–16: Australian hospital statistics. 2017. https://www.aihw.gov.au/reports/hospitals/ahs‐2015‐16‐hospital‐resources/summary (viewed Aug 2022).
- 3. World Health Organization. Climate change. 2023. https://www.who.int/news‐room/fact‐sheets/detail/climate‐change‐and‐health (viewed Aug 2023).
- 4. Lee BK, Ellenbecker MJ, Moure‐Eraso R. Analyses of the recycling potential of medical plastic wastes. Waste Manag 2002; 22: 461‐470.
- 5. Lee RJ, Mears SC. Greening of orthopedic surgery. Orthopedics 2012; 35: e940‐944.
- 6. Cuncannon A, Dosani A, Fast O. Sterile processing in low‐ and middle‐income countries: an integrative review. J Infect Prev 2021; 22: 28‐38.
- 7. Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives ‐ the old, the new, and the way forward: a narrative review. Waste Manag Res 2019; 37: 3‐19.
- 8. Rizan C, Bhutta MF, Reed M, Lillywhite R. The carbon footprint of waste streams in a UK hospital. J Clean Prod 2021; 286: 125446.
- 9. World Health Organization. Health‐care waste. 2018. https://www.who.int/news‐room/fact‐sheets/detail/health‐care‐waste (viewed Sept 2022).
- 10. Waste and climate change. Secretariat of the Pacific Regional Environment Programme. 2009. https://www.sprep.org/climate_change/PYCC/documents/ccwaste.pdf (viewed May 2024).
- 11. McGain F, Jarosz K, Nguyen M, et al. Auditing operating room recycling: a management case report. A A Case Rep 2015; 5: 47‐50.
- 12. Mahjoob A, Alfadhli Y, Omachonu V. Healthcare waste and sustainability: implications for a circular economy. Sustainability. 2023; 15: 7788.
- 13. Department of Climate Change, Energy, the Environment and Water. 2018 National Waste Policy: Less waste, more resources. 2018. https://www.dcceew.gov.au/environment/protection/waste/publications/national‐waste‐policy‐2018 (viewed Sept 2022).
- 14. Department of Climate Change, Energy, the Environment and Water. National Waste Policy Progress Summary Report. 2021. https://www.dcceew.gov.au/sites/default/files/documents/national‐waste‐policy‐progress‐summary‐2021.pdf (viewed May 2024).
- 15. Australian National Audit Office. Australian Government implementation of the National Waste Policy action plan. 2022. https://www.anao.gov.au/work/performance‐audit/australian‐government‐implementation‐the‐national‐waste‐policy‐action‐plan (viewed July 2023).
- 16. Flowers A. Reconceptualising waste: Australia's national waste policies. Journal of Australian Political Economy. 2021; 87: 95‐120.
- 17. Yates E, Bowder A, Roa L, et al. Empowering surgeons, anesthesiologists, and obstetricians to incorporate environmental sustainability in the operating room. Ann Surg 2021; 273: 1108‐1114.
- 18. Wu S, Cerceo E. Sustainability initiatives in the operating room. Jt Comm J Qual Patient Saf 2021; 47: 663‐672.
- 19. Chang DF, Thiel CL, Ophthalmic Instrument Cleaning and Sterilization Task Force. Survey of cataract surgeons’ and nurses’ attitudes toward operating room waste. J Cataract Refract Surg 2020; 46: 933‐940.
- 20. Jabbal I, Colibaseanu D, Blanchfield L, et al. Surgical waste in a colorectal surgery operating room: a five‐year experience. Perioper Care Oper Room Manag. 2021; 25: 100209.
- 21. Weiss A, Hollandsworth HM, Alseidi A, et al. Environmentalism in surgical practice. Curr Probl Surg 2016; 53: 165‐205.
- 22. Wright RW, Brand RA, Dunn W, Spindler KP. How to write a systematic review. Clin Orthop Relat Res 2007; 455: 23‐29.
- 23. Qin RX, Velin L, Yates EF, et al. Building sustainable and resilient surgical systems: a narrative review of opportunities to integrate climate change into national surgical planning in the Western Pacific region. Lancet Reg Health West Pac 2022; 22: 100407.
- 24. Kagoma Y, Stall N, Rubinstein E, Naudie D. People, planet and profits: the case for greening operating rooms. CMAJ 2012; 184: 1905‐1911.
- 25. Papadopoulou A, Kumar NS, Vanhoestenberghe A, Francis NK. Environmental sustainability in robotic and laparoscopic surgery: systematic review. Br J Surg 2022; 109: 921‐932.
- 26. Shoham MA, Baker NM, Peterson ME, Fox P. The environmental impact of surgery: a systematic review. Surgery 2022; 172: 897‐905.
- 27. Bravo D, Thiel C, Bello R, et al. What a waste! The impact of unused surgical supplies in hand surgery and how we can improve. Hand (N Y) 2023; 18: 1215‐1221.
- 28. Pradere B, Mallet R, de La Taille A, et al. Climate‐smart actions in the operating theatre for improving sustainability practices: a systematic review. Eur Urol 2023; 83: 331‐342.
- 29. Perry H, Reeves N, Ansell J, et al. Innovations towards achieving environmentally sustainable operating theatres: a systematic review. Surgeon 2023; 21: 141‐151.
- 30. Majernik M, Daneshjo N, Malega P, Stofkova Z. Environmental waste management of disposable surgical coverage. Pol J Environ Stud 2021; 30: 5163‐5174.
- 31. Ubaldi K. Reprocessing single‐use devices in the ambulatory surgery environment. AORN J 2019; 109: 452‐462.
- 32. Peričić TP, Tanveer S. Why systematic reviews matter. Elsevier. 2019. https://beta.elsevier.com/connect/why‐systematic‐reviews‐matter?trial=true (viewed Apr 2023).
- 33. Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res 2007; 42: 1758‐1772.
- 34. Daniels K. Understanding context in reviews and syntheses of health policy and systems research. In: Langlois EV, Daniels K, Akl EA editors. Evidence synthesis for health policy and systems: a methods guide. Geneva: World Health Organization, 2018. https://www.ncbi.nlm.nih.gov/books/NBK569586/ (viewed Apr 2023).
- 35. Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. Lancaster University, 2006. https://www.lancaster.ac.uk/media/lancaster‐university/content‐assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1‐April2006.pdf (viewed Apr 2023).
- 36. Thiel CL, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol 2015; 49: 1779‐1786.
- 37. Stall NM, Kagoma YK, Bondy JN, Naudie D. Surgical waste audit of 5 total knee arthroplasties. Can J Surg 2013; 56: 97‐102.
- 38. IWRG612.1: Clinical and related waste – operational guidance. Environment Protection Authority Victoria; 2009. https://www.epa.vic.gov.au/about‐epa/publications/iwrg612‐1 (viewed Sept 2022).
- 39. de Sa D, Stephens K, Kuang M, et al. The direct environmental impact of hip arthroscopy for femoroacetabular impingement: a surgical waste audit of five cases. J Hip Preserv Surg 2016; 3: 132‐137.
- 40. Farrokhi FR, Gunther M, Williams B, Blackmore CC. Application of lean methodology for improved quality and efficiency in operating room instrument availability. J Healthc Qual 2015; 37: 277‐286.
- 41. Harding C, Van Loon J, Moons I, et al. Design opportunities to reduce waste in operating rooms. Sustainability. 2021; 13(4): 2207.
- 42. Vozzola E, Overcash M, Griffing E. An environmental analysis of reusable and disposable surgical gowns. AORN J 2020; 111: 315‐325.
- 43. Weller M. A general review of the environmental impact of health care, hospitals, operating rooms, and anesthetic care. Int Anesthesiol Clin 2020; 58: 64‐69.
- 44. Thiel CL, Woods NC, Bilec MM. Strategies to reduce greenhouse gas emissions from laparoscopic surgery. Am J Public Health 2018; 108: S158‐164.
- 45. Candan Dönmez Y, Aslan A, Yavuz van Giersbergen M. Environment‐friendly practices in operating rooms in Turkey. J Nurs Res 2019; 27: e18.
- 46. van Straten B, Heiden DR, Robertson D, et al. Surgical waste reprocessing: injection molding using recycled blue wrapping paper from the operating room. J Clean Prod 2021; 322: 129121.
- 47. Wyssusek K, Keys M, Laycock B, et al. The volume of recyclable polyethylene terephthalate plastic in operating rooms ‐ a one‐month prospective audit. Am J Surg 2020; 220: 853‐855.
- 48. Vinyl Council of Australia. Vinyl Council of Australia's PVC Recycling in Hospitals program expands in regional areas. 2022. https://vinyl.org.au/item/200‐vinyl‐council‐of‐australia‐s‐pvc‐recycling‐in‐hospitals‐program‐expands‐in‐regional‐areas (viewed Aug 2023).
- 49. Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg (Oakv) 2015; 23: 235‐238.
- 50. Chiu CK, Chan CYW, Cheung JPY, et al. Personal protective equipment usage, recycling and disposal among spine surgeons: an Asia Pacific Spine Society survey. J Orthop Surg (Hong Kong) 2021; 29: 2309499020988176.
- 51. Azouz S, Boyll P, Swanson M, et al. Managing barriers to recycling in the operating room. Am J Surg 2019; 217: 634‐638.
- 52. Agrawal D, Shoup V, Montgomery A, et al. Disposal of endoscopic accessories after use: do we know and do we care? Gastroenterol Nurs 2017; 40: 13‐18.
- 53. Petre MA, Bahrey L, Levine M, et al. A national survey on attitudes and barriers on recycling and environmental sustainability efforts among Canadian anesthesiologists: an opportunity for knowledge translation. Can J Anaesth 2019; 66: 272‐286.
- 54. McGain F, White S, Mossenson S, et al. A survey of anesthesiologists’ views of operating room recycling. Anesth Analg 2012; 114: 1049‐1054.
- 55. Tudor TL, Barr SW, Gilg AW. Linking intended behaviour and actions: a case study of healthcare waste management in the Cornwall NHS. Resour Conserv Recycl 2007; 51: 1‐23.
- 56. Bravo D, Gaston RG, Melamed E. Environmentally responsible hand surgery: past, present, and future. J Hand Surg Am 2020; 45: 444‐448.
- 57. Rammelkamp Z, Dirnberger J, Johnson G, Waisbren S. An audit of all waste leaving the operating room: can the surgical suite be more environmentally sustainable? World Med Health Policy 2021; 13: 126‐136.
- 58. Denny NA, Guyer JM, Schroeder DR, Marienau MS. Operating room waste reduction. AANA J 2019; 87: 477‐482.
- 59. Brennan, B. Greening the OR: an Australian perspective. Todays OR Nurse 1994; 16: 25‐32.
- 60. McGain F, Cox N, Cecchin S. Sustainable cardiac services – from the catheterization laboratory to the operating room and beyond. Prog Pediatr Cardiol 2012; 33: 81‐84.
- 61. Friedericy HJ, van Egmond CW, Vogtländer JG, et al. Reducing the environmental impact of sterilization packaging for surgical instruments in the operating room: a comparative life cycle assessment of disposable versus reusable systems. Sustainability 2022; 14: 430.
- 62. McGain F, Story D, Lim T, McAlister S. Financial and environmental costs of reusable and single‐use anaesthetic equipment. Br J Anaesth 2017; 118: 862‐869.
- 63. Meyer MJ, Chafitz T, Wang K, et al. Surgeons’ perspectives on operating room waste: multicenter survey. Surgery 2022; 171: 1142‐1147.
- 64. Sherman JD, Thiel C, MacNeill A, et al. The Green Print: advancement of environmental sustainability in healthcare. Resour Conserv Recycl 2020; 161: 104882.
- 65. Meissner M, Lichtnegger S, Gibson S, Saunders R. Evaluating the waste prevention potential of a multi‐ versus single‐use surgical stapler. Risk Manag Healthc Policy 2021; 14: 3911‐3921.
- 66. Rose ED, Modlin DM, Ciampa ML, et al. Evaluation of operative waste in a military medical center: analysis of operating room cost and waste during surgical cases. Am Surg 2019; 85: 717‐720.
- 67. Pereno A, Eriksson D. A multi‐stakeholder perspective on sustainable healthcare: from 2030 onwards. Futures 2020; 122: 102605.
- 68. Fischer M. Fit for the future? A new approach in the debate about what makes healthcare systems really sustainable. Sustainability 2015; 7: 294‐312.
- 69. Shmerling RH. First, do no harm. Harvard Health, 2015. https://www.health.harvard.edu/blog/first‐do‐no‐harm‐201510138421 (viewed Aug 2023).
- 70. Lee LM. A bridge back to the future: public health ethics, bioethics, and environmental ethics. Am J Bioeth 2017; 17: 5‐12.
- 71. Sherman JD, Ryan S. Ecological responsibility in anesthesia practice. Int Anesthesiol Clin 2010; 48: 139‐151.
- 72. Stanford V, Barna S, Gupta D, Mortimer F. Teaching skills for sustainable health care. Lancet Planet Health 2023; 7: e64‐67.
- 73. Borges de Oliveira K, de Oliveira OJ. Making hospitals sustainable: towards greener, fairer and more prosperous services. Sustainability 2022; 14: 9730.
- 74. Li Y, Pan X, Han Y, Taylor JE. Sustainable healthcare facilities: a scoping review. J Constr Eng Manag 202; 147: 03121007.
- 75. Buffoli M, Capolongo S, Bottero M, et al. Sustainable healthcare: how to assess and improve healthcare structures’ sustainability. Ann Ig 2013; 25: 411‐418.
- 76. Buffoli M, Gola M, Rostagno M, et al. Making hospitals healthier: how to improve sustainability in healthcare facilities. Ann Ig 2014; 26: 418‐425.
- 77. Gosselin RA, Gyamfi YA, Contini S. Challenges of meeting surgical needs in the developing world. World J Surg 2011; 35: 258‐261.
- 78. Elliott IS, Sonshine DB, Akhavan S, et al. What factors influence the production of orthopaedic research in East Africa? A qualitative analysis of interviews. Clin Orthop Relat Res 2015; 473: 2120‐2130.






Summary