The known: In some people, infection with SARS‐CoV‐2 has persistent effects on multiple organ systems.
The new: Our model indicated that 172 530–872 799 people would have long COVID symptoms at the end of 2024. The number of working hours lost would be highest for people aged 30–49 years, leading to an estimated mean economic loss of up to $9.6 billion (2020–21 value), or one‐quarter of GDP growth during 2022.
The implications: The health and economic burdens of long COVID are substantial, especially for working adults. Preventing and treating COVID‐19 and treating long COVID will reduce these substantial effects.
Evidence is accumulating that the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) has effects on several organ systems, beyond causing acute coronavirus disease 2019 (COVID‐19).1 “Long COVID” refers to symptoms that develop during or after the acute infection, reflecting respiratory, cardiac, neurocognitive, immunological, and other organ system dysfunctions.2,3,4 Variance in the estimated prevalence of long COVID reflect differences in definitions, measures, population age structures, and population vaccination coverage.5 The duration of persistence varies between the reported symptoms, which include fatigue, short term memory loss, shortness of breath, palpitations, anxiety, and depression.6,7 The incidence and severity of long COVID are influenced by the severity of the acute infection, the SARS‐CoV‐2 variant, vaccination status, other medical conditions, age, sex, re‐infection with SARS‐CoV‐2, and antiviral treatment.8 Hospitalisation and severe illness are associated with greater risk of long COVID, but it can develop after mild or asymptomatic SARS‐CoV‐2 infections.7,9 Re‐infection with SARS‐CoV‐2 may increase the risk of long COVID (about twice as high in one large American study).10
COVID‐19 vaccines protect against long COVID, and the prevalence of long COVID is higher among unvaccinated than vaccinated people. An Italian study found that 41.8% (95% confidence interval [CI], 37.0–46.7%) of unvaccinated health care workers had developed long COVID, 30.0% (95% CI, 6.7–65.2%) of those who had received one vaccine dose, 17.4% (95% CI, 7.8–31.4%) of those who had received two doses, and 16.0% (95% CI, 11.8–21.0%) of those who had received three doses.11 COVID‐19 vaccines may also reduce the severity of long COVID and improve the quality of life of people with the disorder.12 The magnitude of the societal, health system, and economic burdens of long COVID is unknown. Long COVID can lead to unfilled jobs, poor job performance, productivity losses and reduced labour force participation.13,14
The focus of COVID‐19 health policy has been averting hospitalisations and deaths during the acute illness; long COVID has received less attention. For example, recent World Health Organization recommendations that healthy people under 18 years of age do not require COVID‐19 vaccination boosters, that children under 5 years of age are not a priority for primary vaccination, and that primary vaccination should be discretionary, were informed by the estimated number needed to vaccinate to prevent hospitalisations and deaths;15 long COVID was not considered by the WHO assessment. Quantitative projections of the prevalence of long COVID and estimates of its impact could broaden public health strategies.
More recent estimates of the incidence of SARS‐CoV‐2 infections in Australia, based on notifiable infections reporting data, are unreliable because testing has declined markedly since 2021, and because the reporting of positive polymerase chain reaction (PCR) and rapid antigen test (RAT) results is not mandatory.16 Modelling studies can estimate incidence on the basis of hospitalisations and mortality data17 or serological surveys.18 The only alternative is to rely on self‐reports by people with SARS‐CoV‐2 infections, which is likely to substantially underestimate case numbers, as 30–60% of infections are asymptomatic.19,20
The decline in testing rates and the de‐coupling of the numbers of infections from those of hospitalisations and deaths in highly vaccinated populations mean that serosurveys provide an important objective measure of infection in countries such as Australia. The aim of our study was to estimate the burden of long COVID in Australia by age group, and the associated medium term productivity and economic losses.
Methods
Estimated incidence of SARS‐CoV‐2 infections
To estimate the prevalence of SARS‐CoV‐2 infections in Australia, we used data from a serosurvey of Australian blood donors, conducted by the Global Health Program at the Kirby Institute in partnership with public and private pathology providers and Australian Red Cross Lifeblood. Residual blood from specimens collected for other purposes was tested for anti‐SARS‐CoV‐2 nucleocapsid protein to estimate the prevalence of SARS‐CoV‐2 infections by geographic area, age group, and time, to provide information for informing mathematical models of SARS‐CoV‐2 spread and its impact.21 We used data for samples from adults (median age by round, 44–47 years; range, 18–84 years) collected during four time periods: 23 February – 3 March (5185 samples), 9 June – 18 June (5139 samples), 23 August – 2 September (5005 samples), and 29 November – 13 December 2022 (4996 samples). We estimated SARS‐CoV‐2 antibody seroprevalence by age group and by linearly interpolating values between the values for the four time points (further details: Supporting Information, section 1).
The only available serosurvey data for children and adolescents (0–19 years) were for one time point. Children and adolescents having procedures under anaesthesia (but not immunosuppressed or receiving intravenous immunoglobulin) were recruited at eight hospitals in the Paediatric Active Enhanced Disease Surveillance (PAEDS) network (https://paeds.org.au/about‐us/our‐people). Blood samples were collected from 2057 children and adolescents during 8 June – 31 August 2022; 2046 samples were viable for laboratory analysis.22 To estimate seroprevalence for the same four time points as for adults, we assumed that SARS‐CoV‐2 antibody seroprevalence in children and adolescents increased at the same rate as for adults, as the Omicron SARS‐CoV‐2 variants are transmissible respiratory pathogens with high R0 values.23
Mathematical disease model of long COVID prevalence
We used the WHO definition of long COVID:3 the continuation or development of new symptoms three months after the initial SARS‐CoV‐2 infection, with these symptoms lasting for at least two months with no other explanation. We estimated long COVID prevalence over time from the serosurvey data in an adjusted susceptible–exposed–infected–recovered (SEIR) model (Supporting Information, section 2). The model conformed with the principles outlined in a consultation report on incorporating modelling results into WHO guidelines.24 The model runs from January 2022 to December 2023 and uses community‐wide estimates of the prevalence of long COVID, assuming the high COVID‐19 vaccination coverage of the Australian population.
To account for uncertainty, we modelled a wide range of long COVID rates, and report high and low rates of long COVID prevalence at three time points after a single infection (three months, twelve months, more than twelve months), and adjusted our estimates for full and partial recovery from SARS‐CoV‐2 infection, based on reported study data (Supporting Information, table 2). We did not include re‐infection with SAR‐CoV‐2 as a factor in our model. Further, we assumed that 35% of SARS‐CoV‐2 infections are asymptomatic,18 and that the likelihood of long COVID is lower following asymptomatic than symptomatic infections; we used published odds ratio of 0.13 (at three months) and 0.28 (at twelve months), estimated in children and adolescents (at three and eight months).25 The prevalence rates used (Box 1) are consequently weighted mean prevalence rates for people with symptomatic SARS‐CoV‐2 infections, adjusted for the lower incidence of long COVID among people who had asymptomatic infections.
Estimated productivity loss and economic burden associated with long COVID
We estimated the productivity loss associated with long COVID using a labour supply approach. Productivity loss comprises both the reduction in the contribution of labour to gross domestic product (GDP) and the reduction in the contributions of non‐labour production factors that are influenced by labour supply. We provide two estimates of GDP loss caused by reduced labour supply.
First, we estimated reduced labour contribution to GDP by combining the loss of labour supply and the labour share of GDP (Supporting Information, section 3a). This should be considered a lower estimate of GDP loss; it assumes that the contributions to GDP of other factors of production, including infrastructure and machinery, are unaffected by the reduction in labour supply. This assumption is probably unrealistic, as lost labour is likely to lead to infrastructure and capital equipment being used below capacity.
Our second estimate is based on a Leontief input–output analysis, which assumes that the reduction in labour supply is accompanied by a proportional reduction in other factors of production, yielding a higher estimate of GDP loss than our first estimate. Further details and the model parameters by age group, including estimated range of long COVID case numbers, labour force participation rate, and mean number of working weeks per year, are included in the Supporting Information, section 3b. This approach probably overestimates GDP loss, given the degree of commutability between labour and other factors of production.
The GDP of Australia in 2020–21 was $1.97 trillion; the estimated labour contribution to GDP was 50.5%.26 The required inputs per unit of output in each of the 114 economic sectors of Australia in the input–output analysis were calculated from the Australian Bureau of Statistics input–output table for 2020–21.26
The long COVID case rate for each age group was drawn from a triangular distribution bounded by the range and the mode, being the mean of the lower and upper bounds of the low and high estimates (Supporting Information, table 2). For 2022, the share of cases of non‐recovery from long COVID was uniformly distributed in the range 11.0–22.3%, and the share of cases of slow recovery was uniformly distributed in the range 35.9–42.0%.13,27
Statistical analyses were undertaken in MATLAB 2023a.
Ethics approval
We did not seek formal ethics approval for our modelling study because it was based on published data from studies with ethics approval.21,22
Results
Our model projections of the proportion of people in each age group seropositive for SARS‐CoV‐2 antibodies specific for infection (ie, had at least one SARS‐CoV‐2 infection) during 2022–2023 are depicted in Box 2. Seroprevalence grew more rapidly among people under 60 years of age than among those aged 60 years or more. Our high and low projections of the number of people with long COVID from January 2022 to December 2024 are depicted in Box 3. At the peak (September 2022), 1.2–5.4% of all Australians (310 341–1 374 805 people) were projected to have long COVID, declining to 0.7–3.4% (172 530–872 799 people) by December 2024. It was projected that 0.59–2.24% of children aged 0–4 years (7902–30 002 children) would have long COVID in December 2024; 0.5–2.0% of children and adolescents aged 0–19 years (16 936–61 789) and 0.7–3.6% of people aged 20 years or older (155 590–811 010) were projected to have long COVID in December 2024 (Box 3).
The estimated mean labour loss attributable to long COVID in 2022 was projected to be 102.4 million (95% CI, 50.4–162.2 million) hours — 0.48% (95% CI, 0.24–0.76%) of total worked hours in the 2020–21 financial year — or 8.0 (95% CI, 3.9–12.6) hours per employed person. The estimated mean labour loss was greatest for people aged 30–39 years: 27.5 million (95% CI, 16.0–41.0 million) hours (26.9% of total labour loss), or 9.0 hours (95% CI, 5.3–13.5 hours) per employed person. The second greatest loss was for people aged 40–49 years: 24.5 million (95% CI, 12.1–38.7 million) hours (23.9% of total labour loss), or 9.0 hours (95% CI, 4.5–14.3 hours) per employed person. The estimated mean labour loss attributable to long COVID was lowest for people aged 10–19 years, most of whom are not in the workforce (0.7 million [95% CI, 0.3–1.1 million] hours) (Box 4).
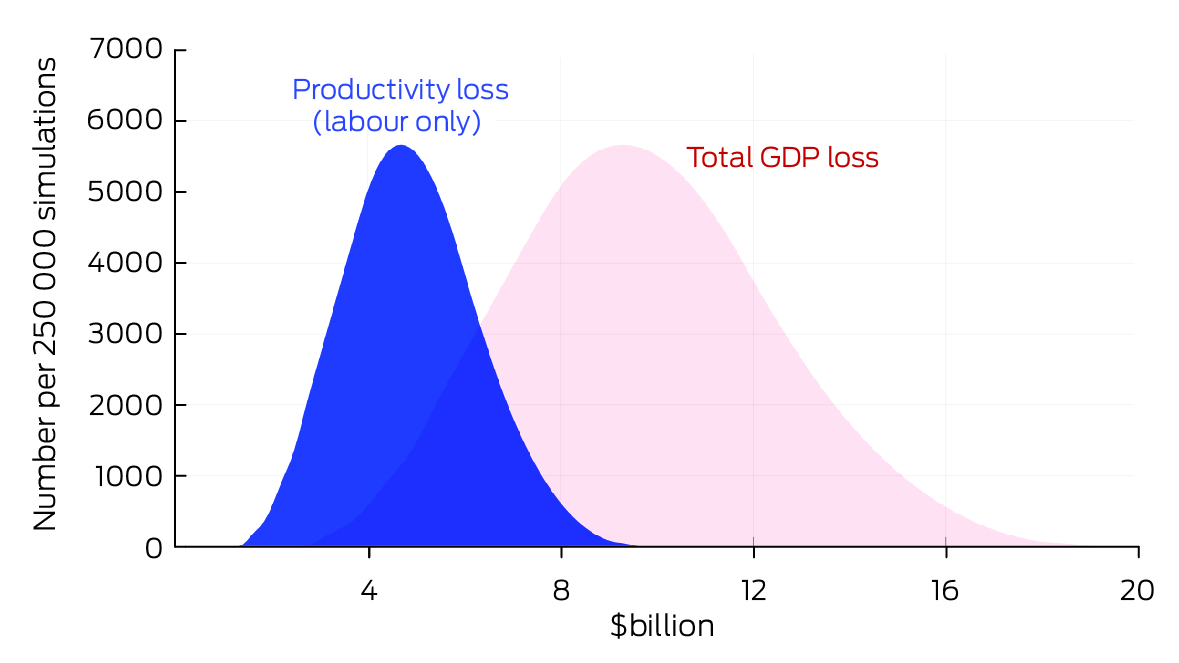
The estimated mean GDP loss attributable to long COVID in 2022 caused by the projected decline in labour supply alone (2020–21 value) was $4.8 billion (95% CI, $2.4–7.7 billion), or 0.2% of GDP. The estimated mean GDP loss caused by the projected decline in labour supply and reduced use of other production factors was $9.6 billion (95% CI, $4.7–15.2 billion), or 0.5% of GDP (Box 5). The seasonally adjusted GDP growth rate was about 0.6% per quarter during 202228 (0.5% during the fourth quarter29).
Discussion
Our modelling indicates that hundreds of thousands of Australians are likely to be living with long COVID after a single infection; 0.7–3.4% of all Australians have long COVID and have not recovered twelve months after SARS‐CoV‐2 infection. By way of comparison, 3% of Australians aged 20 years or older were living with ischaemic heart disease in 2023, the leading cause of the global disease burden.30 The prevalence of ischaemic heart disease is highest among people aged 75 years and older, but our modelled proportion of those with long COVID was largest for people aged 30–49 years, and the estimated mean loss in labour supply for people aged 10–69 years during 2022 was 102.4 million hours. This finding is consistent with the United Kingdom report that the difference in work inactivity rate between people with and without self‐reported long COVID in July 2022 was greatest for people aged 35–49 years.31 The economic impact of long COVID is therefore likely to be greater than that of other leading causes of disease because it affects working age people. The upper mean economic loss in GDP we estimated ($9.6 billion) was equivalent to about one‐quarter of GDP growth in Australia during 2022. SARS‐CoV‐2 re‐infections and further epidemic waves could increase the burden of chronic disease and its economic impact.
Our lower estimates of the prevalence of long COVID are similar to those of an Australian study that predicted 80 000 to 325 000 people would experience long COVID for at least 12 weeks, and that 14 000 to 170 000 people could be affected up to twelve months after acute SARS‐CoV‐2 infection.32
Long COVID can be prevented to some extent by vaccination against COVID‐19,33 and possibly by antiviral treatments during the acute infection.34 According to our model, the burden of long COVID is greatest among adults under 60 years of age; in December 2024, 70–80% of cases were in people under 60 years of age, and 44–34% in people aged 30–49 years. The Australian Technical Advisory Group on Immunisation (ATAGI) did not consider long COVID in its February 2024 vaccination guidelines, and recommended booster doses only for people aged 65 years or older, and for those under 65 years of age who are severely immunocompromised.35 Vaccinating children aged 0–4 years is also important. In Denmark, the incidence of long COVID was reported to be higher among children aged 0–3 years than older children;36 as in Australia, children under 5 years of age are ineligible for routine vaccination in Denmark.
Our two GDP loss estimates do not account for unmeasured economic losses, including healthy employees who cannot work because they are caring for non‐employees (eg, children or older people), ill people requiring isolation, or other employees affected by COVID‐19 or long COVID. Nor do they include losses caused by long COVID beyond six months; productivity losses caused by changes to the work environment, such as working from home; and losses arising from the imperfect mobility of labour between sectors and regions in response to changes caused by COVID‐19, such as unfilled health care or education jobs.
GDP loss might be partially mitigated by increasing the work hours of people who are not sick or have recovered from COVID‐19, and by the influx of new, healthy workers. Longer working time is especially common among health services workers, but may contribute to burnout and reduced productivity. Substitution effects that enhance productivity are possible, such as increasing the ratio of capital to labour and the deployment of labour‐saving technologies to maintain output. Further research is needed to examine these possibilities.
Implications
Strategies for reducing the impact of long COVID should focus on preventing and treating acute COVID‐19. This would include regular access to vaccine boosters and antiviral medications for all working adults, accessible testing, promoting mask wearing during epidemic waves, optimising indoor air quality by improving ventilation, and encouraging the use of high efficiency particulate air (HEPA) filters.37
In the absence of such preventive measures, the capacity of the health system for treating people with long COVID needs to be enhanced, and social structures for supporting people with long COVID and managing their illness need to be improved. There is some evidence that treatment with antiviral medications during acute COVID‐19 can reduce the risk of long COVID.38 In Australia, antiviral treatment of acute COVID‐19 is currently quite restricted, and most working age adults are ineligible. Improved treatment and prevention of acute COVID‐19 would reduce the burden of long COVID, improve quality of life, and increase the speed with which people can return to work. Assisting people with long COVID, particularly those unable to work because of their symptoms, with disability pensions, for example, could reduce their financial burden.
Limitations
As we had only limited specific seroprevalence data for people aged 0–19 years, we assumed that seroprevalence of SARS‐CoV‐2 antibodies would increase at the same rate as for other age groups. Our model projected that 100% of people aged 40–49 or 60–69 years would have been infected with SARS‐COV‐2 between January 2022 and late 2023. We do not know whether this was the case, but the 2022 serosurvey data indicated that almost 80% of people aged 40–49 and 60% aged 60–69 years had been infected by late 2022. Further, our model took into account asymptomatic infections, which may not result in detectable antibodies to SARS‐CoV‐2; consequently, estimates of infection rates based on serosurvey data would be lower than our modelled rates.
We used linear interpolation to derive seroprevalence estimates over two years, but as the data points used were all from the first year of this period, we assumed that trends in 2022 would be maintained during 2023. We did not vary the estimated seroprevalence values in our model, but applied a range of published long COVID rate estimates in the sensitivity analysis to reflect uncertainty. We did not use different long COVID rates according to the number of vaccination doses received because we did not have age group‐specific data in this regard.
For long COVID rates by age group, we selected large scale studies with community‐based selection of participants from largely vaccinated populations.6,36 Differences between public health organisations in the definition of long COVID2,3,4 contribute to differences in its estimated prevalence. As our model did not consider re‐infection with SARS‐CoV‐2, which may increase the risk of long COVID,10,39 it is likely we underestimated the prevalence of long COVID.
Conclusion
The outcomes of our modelling study indicate that further research into the population impact of expanded access to COVID‐19 vaccine boosters and antiviral medications is needed. Our model suggests health and economic burdens of long COVID comparable with those of the leading causes of the burden of disease in Australia, but, unlike cardiovascular disease and cancer, the burden of long COVID is highest among working age adults, a key difference that results in major economic losses. The focus of public policy on COVID‐19 must shift from solely preventing hospitalisations and deaths during the acute disease to encompassing the prevention of long COVID.
Box 1 – Estimated proportions of people with long COVID symptoms (prevalence rates), by duration of symptoms and age group: high and low estimates*
|
|
Duration of symptoms |
||||||||||||||
|
Age group (years) |
Up to 3 months |
Up to 12 months |
Longer than 12 months |
||||||||||||
|
|
|||||||||||||||
|
High estimates† |
|
|
|
||||||||||||
|
0–4 |
8.90% |
4.59% |
2.24% |
||||||||||||
|
5–9 |
3.06% |
1.58% |
0.75% |
||||||||||||
|
10–19 |
3.27% |
1.69% |
0.75% |
||||||||||||
|
20–59 |
14.5% |
7.47% |
4.49% |
||||||||||||
|
60 or older |
18.7% |
9.66% |
4.49% |
||||||||||||
|
Low estimates |
|
|
|
||||||||||||
|
0–4 |
2.29% |
1.18% |
0.59% |
||||||||||||
|
5–9 |
0.79% |
0.40% |
0.20% |
||||||||||||
|
10–19 |
0.84% |
0.43% |
0.22% |
||||||||||||
|
20–29 |
2.64% |
1.36% |
0.68% |
||||||||||||
|
30–39 |
5.15% |
2.65% |
1.33% |
||||||||||||
|
40–49 |
3.75% |
1.87% |
0.97% |
||||||||||||
|
50–59 |
3.34% |
1.72% |
0.86% |
||||||||||||
|
60–69 |
3.06% |
1.58% |
0.78% |
||||||||||||
|
70 or older |
1.81% |
0.94% |
0.46% |
||||||||||||
|
|
|||||||||||||||
|
* Derived from published Australian estimates (Supporting Information, table 2) and calculated for the general population, taking asymptomatic severe acute respiratory syndrome coronavirus 2 infections into account. † For the high estimates, the rates were the same for 20–59‐year‐old people; consequently we do not report the rates by 10‐year brackets within this range. |
|||||||||||||||
Box 2 – Estimated (2022) and projected (2023) seroprevalence of SARS‐CoV‐2 antibodies, Australia, by age group*
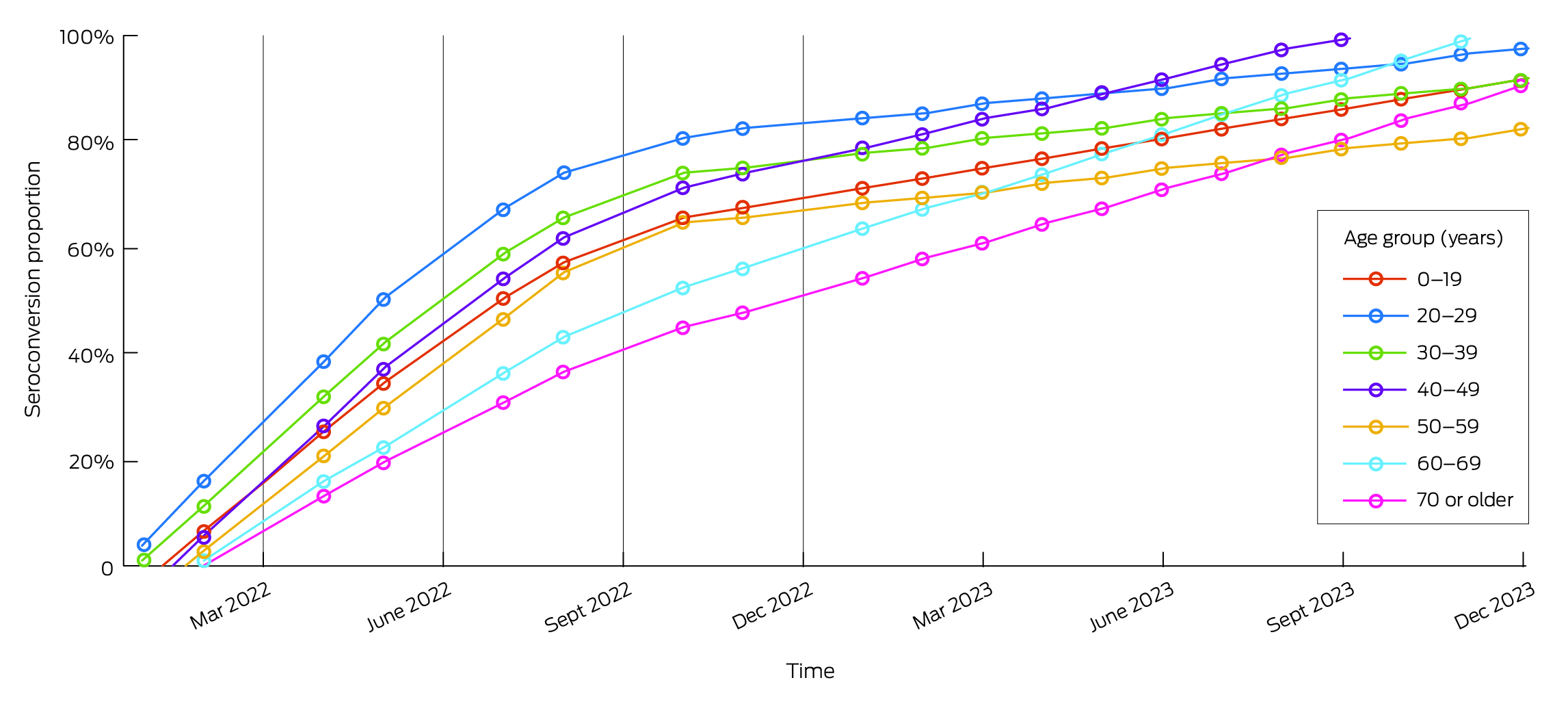
SARS‐CoV‐2 = severe acute respiratory syndrome coronavirus 2.* The vertical grey lines indicate the data collection points, the dots the estimates obtained by linear interpolation.
Box 3 – Projected numbers of people with long COVID symptoms, 2022–2024, by age group: high and low model projections*
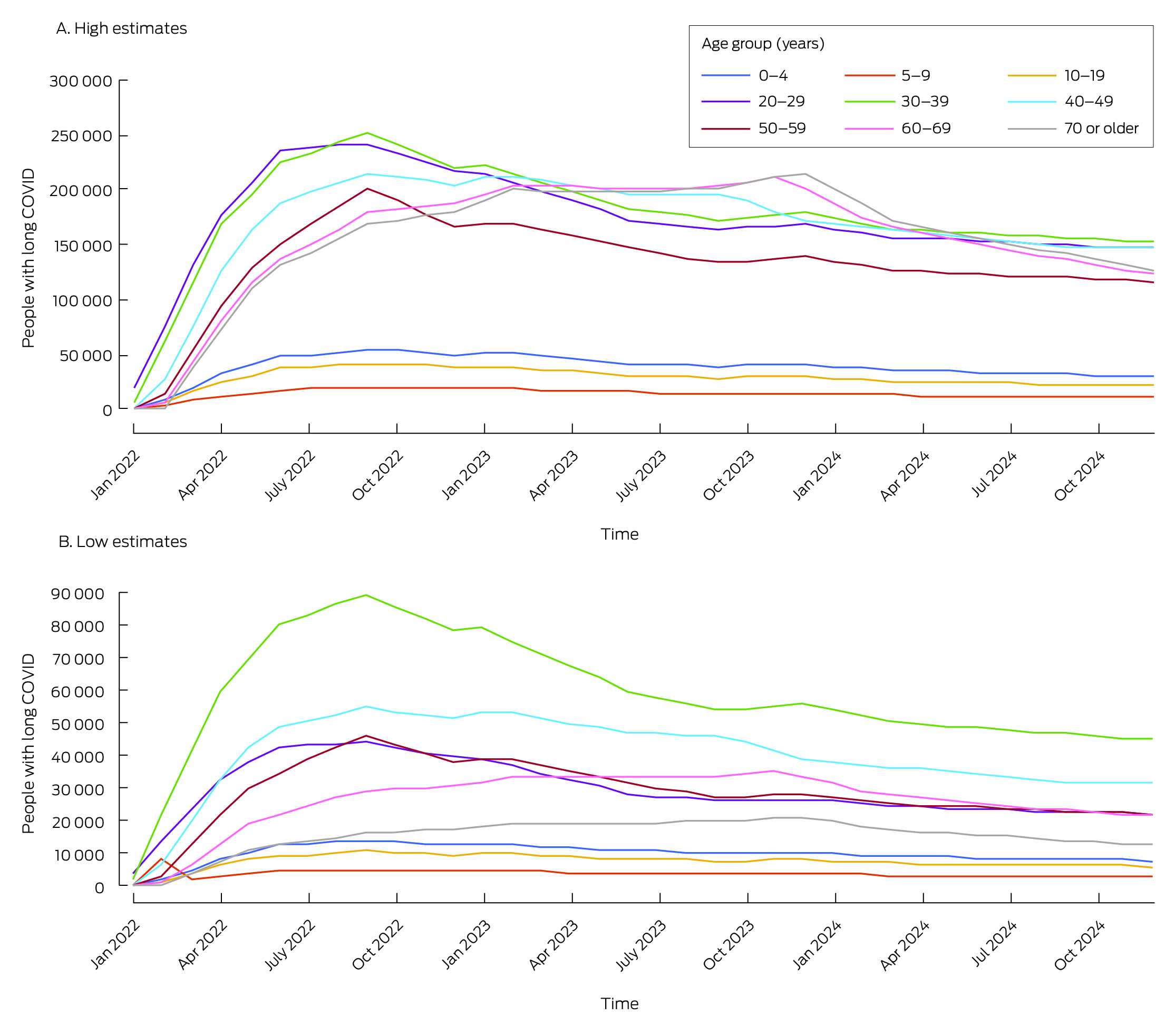
SARS‐CoV‐2 = severe acute respiratory syndrome coronavirus 2.* Model includes people with SARS‐CoV‐2 infections during January 2022 – December 2023. The data for these graphs is included in the Supporting Information, table 4.
Box 4 – Projected mean loss in labour supply attributable to long COVID in 2022, by age group
|
|
Work hours lost |
||||||||||||||
|
Age group (years) |
Total, in millions of hours (95% CI) |
Per employed person, in hours (95% CI) |
Proportion of total |
||||||||||||
|
|
|||||||||||||||
|
Total (10–69) |
102.4 (50.4–162.2) |
8.0 (3.9–12.6) |
|
||||||||||||
|
10–19 |
0.7 (0.3–1.1) |
1.0 (0.5–1.6) |
0.7% |
||||||||||||
|
20–29 |
20.9 (9.0–34.5) |
7.9 (3.4–13.1) |
20.4% |
||||||||||||
|
30–39 |
27.5 (16.0–41.0) |
9.0 (5.3–13.5) |
26.9% |
||||||||||||
|
40–49 |
24.5 (12.1–38.7) |
9.0 (4.5–14.3) |
23.9% |
||||||||||||
|
50–59 |
17.7 (8.4–28.4) |
7.4 (3.5–11.9) |
17.3% |
||||||||||||
|
60–69 |
11.1 (4.6–18.6) |
7.8 (3.2–13.1) |
10.9% |
||||||||||||
|
|
|||||||||||||||
|
CI = confidence interval. |
|||||||||||||||
Received 19 July 2023, accepted 17 April 2024
- Valentina Costantino1
- Quentin Grafton2
- Tom Kompas3
- Long Chu2
- Damian Honeyman1
- Adriana Notaras1
- C Raina MacIntyre1
- 1 The Kirby Institute, Sydney, NSW
- 2 Crawford School of Public Policy, Australian National University, Canberra, ACT
- 3 Centre of Excellence for Biosecurity Risk Analysis, University of Melbourne, Melbourne, VIC
Open access:
Open access publishing facilitated by University of New South Wales, as part of the Wiley ‐ University of New South Wales agreement via the Council of Australian University Librarians.
Publication note:
An earlier version of the manuscript for this article was submitted to the House of Representatives Standing Committee on Health, Aged Care and Sport inquired into and reported on Long COVID and Repeated COVID Infections, 2022 (https://www.aph.gov.au/DocumentStore.ashx?id=54413018‐123c‐417d‐84c7‐a258d113d561&subId=726017).
Data sharing:
As no original data were generated for this report, data sharing is not possible.
C Raina MacIntyre is funded by an investigator L3 grant from the National Health and Medical Research Council (2016907). The funder had no role in the study and the researchers involved are independent of the funder. Valentina Costantino is funded by the Balvi Filantropic Fund.
C Raina MacIntyre is a member of the WHO COVID‐19 Vaccine Composition Technical Advisory Group. She has received support from Sanofi for influenza research.
- 1. Thaweethai T, Jolley SE, Karlson EW, et al; RECOVER Consortium. Development of a definition of postacute sequelae of SARS‐CoV‐2 infection. JAMA 2023; 329: 1934‐1946.
- 2. Centers for Disease Control and Prevention. Long COVID basics. Updated 11 June 2024. https://www.cdc.gov/covid/long‐term‐effects/?CDC_AAref_Val=https://www.cdc.gov/coronavirus/2019‐ncov/long‐term‐effects (viewed June 2024).
- 3. World Health Organization. Post COVID‐19 condition (long COVID). 7 Dec 2022. https://www.who.int/europe/news‐room/fact‐sheets/item/post‐COVID‐19‐condition (viewed Nov 2023).
- 4. National Institute for Health and Care Excellence. COVID‐19 rapid guideline: managing the long‐term effects of COVID‐19 [NG188]. Updated 25 Jan 2024. https://www.who.int/docs/default‐source/immunization/sage/covid/sage‐prioritization‐roadmap‐covid19‐vaccines.pdf?Status=Temp&sfvrsn=bf227443_2 (viewed June 2024).
- 5. Munblit D, Nicholson TR, Needham DM, et al. Studying the post‐COVID‐19 condition: research challenges, strategies, and importance of Core Outcome Set development. BMC Med 2022; 20: 50.
- 6. Bull‐Otterson L, Baca S, Saydah S, et al. Post‐COVID conditions among adult COVID‐19 survivors aged 18–64 and ≥ 65 years: United States, March 2020–November 2021. MMWR Morb Mortal Wkly Rep 2022; 71: 713‐717.
- 7. Lopez‐Leon S, Wegman‐Ostrosky T, Ayuzo del Valle NC, et al. Long‐COVID in children and adolescents: a systematic review and meta‐analyses. Sci Rep 2022; 12: 9950.
- 8. Adler L, Gazit S, Pinto Y, et al. Long‐COVID in patients with a history of mild or asymptomatic SARS‐CoV‐2 infection: a nationwide cohort study. Scand J Prim Health Care 2022; 40: 342‐349.
- 9. Ma Y, Deng J, Liu Q, et al. Long‐term consequences of asymptomatic SARS‐CoV‐2 infection: a systematic review and meta‐analysis. Int J Environ Res Public Health 2023; 20: 1613.
- 10. Bowe B, Xie Y, Al‐Aly Z. Acute and postacute sequelae associated with SARS‐CoV‐2 reinfection. Nat Med 2022; 28: 2398‐2405.
- 11. Azzolini E, Levi R, Sarti R, et al. Association between BNT162b2 vaccination and long COVID after infections not requiring hospitalization in health care workers. JAMA 2022; 328: 676‐678.
- 12. Tran V, Perrodeau E, Saldanha J, et al. Efficacy of first dose of covid‐19 vaccine versus no vaccination on symptoms of patients with long covid: target trial emulation based on ComPaRe e‐cohort. BMJ Med 2023; 2: e000229.
- 13. Davis HE, Assaf GS, McCorkell L, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine 2021; 38: 101019.
- 14. Trades Union Congress (United Kingdom). Workers’ experience of Long Covid. Joint report by the TUC and Long Covid Support. 27 Mar 2023. https://www.tuc.org.uk/research‐analysis/reports/workers‐experience‐long‐covid (viewed July 2024).
- 15. World Health Organization. WHO SAGE Roadmap for prioritizing uses of COVID‐19 vaccines. 10 Dec 2023. https://www.who.int/docs/default‐source/immunization/sage/covid/sage‐prioritization‐roadmap‐covid19‐vaccines.pdf?Status=Temp&sfvrsn=bf227443_2 (viewed May 2023).
- 16. Syed A, O'Connor P. Australian state governments and mandatory reporting of positive COVID tests as a new surge begins. World Socialist Web Site, 1 Nov 2022. https://www.wsws.org/en/articles/2022/11/02/xssk‐n02.html (viewed July 2024).
- 17. Giattino C. How epidemiological models of COVID‐19 help us estimate the true number of infections. Our World in Data, 24 Aug 2020. https://ourworldindata.org/covid‐models (viewed Nov 2022).
- 18. Hozé N, Paireau J, Lapidus N, et al. Monitoring the proportion of the population infected by SARS‐CoV‐2 using age‐stratified hospitalisation and serological data: a modelling study. Lancet Public Health 2021; 6: e408‐e415.
- 19. Oran DP, Topol EJ. Prevalence of asymptomatic SARS‐CoV‐2 infection: a narrative review. Ann Intern Med 2020; 173: 362‐367.
- 20. Oran DP, Topol EJ. The proportion of SARS‐CoV‐2 infections that are asymptomatic: a systematic review. Ann Intern Med 2021; 174: 655‐662.
- 21. Kirby Institute. Serosurveillance for SARS‐CoV‐2 infection to inform public health responses. Undated. https://kirby.unsw.edu.au/project/serosurveillance‐sars‐cov‐2‐infection‐inform‐public‐health‐responses (viewed Nov 2022).
- 22. Paediatric Active Enhanced Disease Surveillance. Paediatric SARS‐CoV‐2 serosurvey 2022, Australia. Summary report. 3 Nov 2022. https://paeds.org.au/sites/default/files/2022‐11/PAEDS%20NCIRS_COVID‐19%20Paediatric%20Serosurvey%202022%20Report_3‐11‐2022_Final_1.pdf (viewed Nov 2022).
- 23. Liu Y, Rocklöv J. The effective reproductive number of the Omicron variant of SARS‐CoV‐2 is several times relative to Delta. J Travel Med 2022; 29: taac037.
- 24. World Health Organization. Consultation on the development of guidance on how to incorporate the results of modelling into WHO guidelines Geneva, Switzerland, 27–29 April 2016. https://iris.who.int/bitstream/handle/10665/258987/WHO‐HIS‐IER‐REK‐2017.2‐eng.pdf (viewed Mar 2024).
- 25. Ertesvåg NU, Iversen A, Blomberg B, et al; Bergen COVID‐19 research group. Post COVID‐19 condition after delta infection and omicron reinfection in children and adolescents. eBioMedicine 2023; 92: 104599.
- 26. Australian Bureau of Statistics. Australian national accounts: input–output tables, 2020–21; here: Table 5. 30 Mar 2023. https://www.abs.gov.au/statistics/economy/national‐accounts/australian‐national‐accounts‐input‐output‐tables/2020‐21/5209055001DO001_202021.xlsx (viewed June 2023).
- 27. Peter RS, Nieters A, Kräusslich HG, et al; EPILOC Phase 1 Study Group. Post‐acute sequelae of covid‐19 six to 12 months after infection: population based study. BMJ 2022; 379 e071050.
- 28. Australian Bureau of Statistics. Australian national accounts: national income, expenditure and product. Table 1. 2024. https://www.abs.gov.au/statistics/economy/national‐accounts/australian‐national‐accounts‐national‐income‐expenditure‐and‐product/mar‐2024/5206001_Key_Aggregates.xlsx (viewed July 2024).
- 29. Janda M. Australia's economy grew 0.5pc in December 2022 quarter, ABS data reveal, well below most economists' forecasts. ABC News (Australia), 1 Mar 2023. https://www.abc.net.au/news/2023‐03‐01/australian‐gdp‐december‐2022‐abs‐economic‐growth‐slowing/102038014 (viewed June 2023).
- 30. Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts. Updated 30 June 2023. Archived: https://web.archive.org/web/20230928063950/https://www.aihw.gov.au/reports/heart‐stroke‐vascular‐diseases/hsvd‐facts/contents/disease‐types (viewed June 2023).
- 31. Office for National Statistics. Self‐reported long COVID and labour market outcomes, UK: 2022. 5 Dec 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/selfreportedlongcovidandlabourmarketoutcomesuk2022/selfreportedlongcovidandlabourmarketoutcomesuk2022 (viewed Nov 2023).
- 32. Hensher M, Angeles MR. Potential scale of long COVID cases from the Omicron wave in Australia: summer 2021–2022 [briefing paper]. Geelong: Institute for Health Transformation, Deakin University, 2022. https://iht.deakin.edu.au/wp‐content/uploads/sites/153/2022/02/Long‐COVID‐Omicron‐briefing‐paper‐IHT‐02‐2022.pdf (viewed Nov 2023).
- 33. Byambasuren O, Stehlik P, Clark J, et al. Effect of covid‐19 vaccination on long covid: systematic review. BMJ Med 2023; 2: e000385.
- 34. Xie Y, Choi T, Al‐Aly Z. Association of treatment with nirmatrelvir and the risk of post‐COVID‐19 condition. JAMA Intern Med 2023; 183: 554‐564.
- 35. Australian Technical Advisory Group on Immunisation. Statement on the administration of COVID‐19 vaccines in 2024. 29 Feb 2024. https://www.health.gov.au/sites/default/files/2024‐03/atagi‐statement‐on‐the‐administration‐of‐covid‐19‐vaccines‐in‐2024.pdf (viewed July 2024).
- 36. Kikkenborg Berg S, Palm P, Nygaard U, et al. Long COVID symptoms in SARS‐CoV‐2‐positive children aged 0–14 years and matched controls in Denmark (LongCOVIDKidsDK): a national, cross‐sectional study. Lancet Child Adolesc Health 2022; 6: 614‐623.
- 37. Guo Y, Dou Z, Zhang N, et al. Student close contact behavior and COVID‐19 transmission in China's classrooms. PNAS Nexus 2023; 2: pgad200.
- 38. Suran M. Studies investigate whether antivirals like paxlovid may prevent long COVID. JAMA 2024; 331: 98‐100.
- 39. Yang C, Zhao H, Espín E, Tebbutt SJ. Association of SARS‐CoV‐2 infection and persistence with long COVID. Lancet Respir Med 2023; 11: 504‐506.






Abstract
Objective: To estimate the number of people in Australia with long COVID by age group, and the associated medium term productivity and economic losses.
Study design: Modelling study: a susceptible–exposed–infected–recovered (SEIR) model to estimate the number of people with long COVID over time following single infections, and a labour supply model to estimate productivity losses as a proportion of gross domestic product (GDP).
Setting: Australia, 2022–2024.
Main outcome measures: Estimated number of people infected with severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) during 2022–2023 (based on serosurvey data) who have long COVID, 2022–2024, by age group; estimated GDP loss during 2022 caused by reduced labour supply attributable to long COVID.
Results: Our model projected that the number of people with long COVID following a single infection in 2022 would peak in September 2022, when 310 341–1 374 805 people (1.2–5.4% of Australians) would have symptoms of long COVID, declining to 172 530–872 799 people (0.7–3.4%) in December 2024, including 7902–30 002 children aged 0–4 years (0.6–2.2%). The estimated mean labour loss attributable to long COVID in 2022 was projected to be 102.4 million (95% confidence interval [CI], 50.4–162.2 million) worked hours, equivalent to 0.48% (95% CI, 0.24–0.76%) of total worked hours in Australia during the 2020–21 financial year. The estimated mean GDP loss caused by the projected decline in labour supply and reduced use of other production factors was $9.6 billion (95% CI, $4.7–15.2 billion), or 0.5% of GDP. The estimated labour loss was greatest for people aged 30–39 years (27.5 million [95% CI, 16.0–41.0 million] hours; 26.9% of total labour loss) and people aged 40–49 years (24.5 million [95% CI, 12.1–38.7 million] hours; 23.9% of total labour loss).
Conclusion: Widespread SARS‐CoV‐2 infections in Australia mean that even a small proportion of infected people developing long COVID‐related illness and disability could have important population health and economic effects. A paradigm shift is needed, from a sole focus on the immediate effects of coronavirus disease 2019 (COVID‐19) to preventing and treating COVID‐19 and treating long COVID, with implications for vaccine and antiviral policy and other mitigation of COVID‐19.