The known: The number of infectious syphilis notifications among young people has been rising since 2012.
The new: Notifications of infectious syphilis in women of reproductive age increased in Australia during 2011–2021, as did those of congenital syphilis; notification rates for each were higher for Aboriginal and Torres Strait Islander than non‐Indigenous people. The mothers of almost half the infants born with congenital syphilis had not received antenatal care.
The implications: More needs to be done to reduce infectious syphilis rates. To avert congenital syphilis, equitable access to antenatal care must be secured for all women.
If untreated, Treponema pallidum infections can cause a variety of clinical manifestations according to the stage of the infection — primary, secondary, latent, tertiary syphilis — ranging from a chancre at the site of infection to neurosyphilis and cardiovascular syphilis 10–30 years after infection.1 Mother‐to‐child transmission of the spirochete causes congenital syphilis, which can have devastating consequences; more than half of untreated infections lead to serious complications, including stillbirth, neonatal death, and major malformations.2 As the risk of a woman transmitting syphilis to her child is greatest during the primary and secondary (infectious) stages of syphilis, pregnancy is a critical time for syphilis testing and treatment.3 Syphilis is routinely diagnosed on the basis of a combination of clinical history and serological testing; benzathine penicillin is recommended for first‐line treatment, the dose determined by the stage of infection.1
Despite effective treatment being readily available, syphilis is among the most frequent sexually transmissible infections; in 2022, the World Health Organization estimated that about eight million new cases of infectious syphilis were diagnosed around the world each year, and an estimated 700 000 cases of congenital syphilis.4 Congenital syphilis, the second leading cause of preventable stillbirth, can be averted by antenatal screening and treatment, and by reducing the prevalence of infectious syphilis in the general population. WHO has called for efforts to eliminate the mother‐to‐child transmission of syphilis, defined as a rate of 50 cases per 100 000 live births or lower.5
In Australia, the infectious syphilis notification rate more than tripled during 2012–2022.6 The rise was initially characterised by outbreaks among men in urban areas who have sex with men and Aboriginal and Torres Strait Islander people in remote areas.7 The outbreak among Aboriginal and Torres Strait Islander people in remote and regional areas of northern and central Australia, first reported in 2011, led to a multi‐jurisdictional syphilis outbreak response in 2015.8 More recently, the increased incidence of syphilis among young men and women in major cities has been reported, together with a parallel increase in cases of congenital syphilis.6
Information on the recent epidemiology of syphilis in Australia has been derived from a national surveillance system that collates all notifications of infectious syphilis and congenital syphilis.9 Since 2018, this system captures additional information from the mothers of babies diagnosed with congenital syphilis, providing an opportunity to identify deficits in testing and treatment pathways. On the basis of this information, we report for the first time notification rates and changes in the rates of both infectious syphilis among women aged 15–44 years and of congenital syphilis, and to explore health care and syphilis testing and treatment for mothers of infants diagnosed with congenital syphilis.
Methods
For our retrospective cohort study we analysed national infectious syphilis and enhanced congenital syphilis surveillance data for 1 January 2011 – 31 December 2021. We included data for women aged 15–44 years, defined by the Australian Institute of Health and Welfare as women of reproductive age,10 and for cases of congenital syphilis diagnosed and notified in Australia. For population denominators, we used Australian Bureau of Statistics population estimates and Aboriginal and Torres Strait Islander births and confinements summary data (by state) and births (by year and month of birth, and state), obtained from the .StatData Explorer site (https://explore.data.abs.gov.au). Remoteness (by postcode of residence) was based on the Australian Statistical Geography Standard.11
Syphilis (congenital and non‐congenital) is notifiable in all Australian states and territories. Reactive syphilis serology test results must be reported by pathology laboratories to public health authorities in each jurisdiction; in some, the medical practitioner or nurse practitioner who diagnoses syphilis must also notify the jurisdictional public health authority. Syphilis cases in Australia are classified as infectious (duration of infection less than two years), unspecified (duration of infection longer than two years, or unknown), or congenital syphilis according to Communicable Disease Network Australia national case definitions.12
Each jurisdictional public health authority provides data on syphilis cases that meet national case definitions to the Australian Department of Health and Aged Care National Notifiable Diseases Surveillance System (NNDSS).9 The NNDSS coordinates the national surveillance of more than 70 communicable diseases and disease groups. Notifications are made to state or territory health authorities according to the provisions of jurisdictional public health legislation; electronic, de‐identified records of notifications are supplied to the NNDSS each day for collation and analysis. Notification data include disease codes for syphilis (infectious, unspecified, congenital), a unique record reference number, state/territory identifier, date of notification to the health authority, birth sex, syphilis onset age, syphilis diagnosis date, Indigenous status, and postcode of residence. Despite complete capture of cases being the aim, data quality and completeness vary because notifications come from different sources (clinicians, laboratories, hospitals), how these sources report cases differs by state and territory, and some people may not provide all requested information to health authorities. The quality of notifications data is continuously assessed and optimised. Enhanced notification data regarding congenital syphilis cases include the infant's clinical condition, and they are linked with the mother's notification reference number, antenatal care details, trimester of congenital syphilis diagnosis, treatment of the mother's syphilis, and the syphilis screening history and country of birth of the mother. Antenatal care history is established on a case‐by‐case basis by the clinician or nurse, and through follow‐up by jurisdictional public health authorities. Women or their infants can be lost to follow‐up, despite considerable effort to avoid losses.
Statistical analysis
We calculated infectious syphilis notification rates by year, separately for Aboriginal and Torres Strait Islander and non‐Indigenous women, by age group (15–24, 25–34, 35–44 years), geographic location (major cities, inner/outer regional, remote/very remote),11 and state/territory of residence. We calculated incidence rate ratios (IRRs) with 95% confidence intervals (CIs), using negative binomial models robust to data overdispersion, to compare changes in notification rate during 2011–2021. Changes in rate were estimated by calendar year; for 2020 we included a binary interaction factor for lockdown status, to account for the substantial change associated with coronavirus disease 2019 (COVID‐19)‐related lockdowns in mid‐2020. Multivariate models in which Indigenous status was the primary predictor were adjusted for age group, geographic region (remoteness), and state/territory of residence; we report IRRs with 95% CIs.
We also calculated congenital syphilis rates (per number of live births) by Indigenous status. We report the number of congenital syphilis cases by year and Indigenous status. Based on information in the enhanced congenital syphilis data fields, we also report the numbers and proportions of cases by clinical outcome for the baby, stage of pregnancy at diagnosis, timing of antenatal care, syphilis screening history, and treatment of the mother's syphilis, each by Indigenous status of the infant.
Analyses were undertaken in Stata 15.1. We report this observational study in accordance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.13
Ethics approval
The Aboriginal Health and Medical Research Council of New South Wales (1805/21) and, in accordance with jurisdictional data access protocols, the Northern Territory Department of Health and Menzies School of Health Research Human Research Ethics Committee (HREC 2021‐3991) approved this study. The project was overseen by the Kirby Institute Aboriginal and Torres Strait Islander Reference Group.
Results
Notifications of infectious syphilis in women aged 15–44 years
During 2011–2021, 5011 cases of infectious syphilis in women aged 15–44 years were notified (Aboriginal or Torres Strait Islander women, 2735 cases; non‐Indigenous women, 2276 cases); the annual number rose from 141 cases in 2011 to 902 in 2021. The notification rates were 140 per 100 000 Aboriginal or Torres Strait Islander women and 4 per 100 000 non‐Indigenous women. The highest notification rates were for women aged 25–34 years (163 per 100 000 Aboriginal or Torres Strait Islander women; 6 per 100 000 non‐Indigenous women); for 35–44‐year old women, the rates were 90 per 100 000 Aboriginal or Torres Strait Islander women and 4 per 100 000 non‐Indigenous women. During 2011–2021, notification rates were higher for Aboriginal or Torres Strait Islander women living in remote or very remote areas (385 per 100 000 population) than for those in major cities (35 per 100 000 population); for non‐Indigenous women, the rate was higher in major cities (5 per 100 000 population) than in remote or very remote areas (3 per 100 000 population).
Change in infectious syphilis notification rates, 2011–2021
The notification rate for Aboriginal or Torres Strait Islander women rose from 56 (95% CI, 45–65) per 100 000 in 2011 to 227 (95% CI, 206–248) cases per 100 000 population in 2021; for non‐Indigenous women, it rose from 1 (95% CI, 0.8–1.4) to 9 (95% CI, 8–10) cases per 100 000 population. The notification rate for all women grew by about 20% per year during 2011–2021 (IRR, 1.2; 95% CI, 1.2–1.3). For both Aboriginal or Torres Strait Islander and non‐Indigenous women, the relative rises were similar for all three age groups (Box 1).
For Aboriginal and Torres Strait Islander women, the rise in notification rate was more marked in remote and very remote areas than in major cities and regional areas, and in the Northern Territory and Western Australia than elsewhere. For non‐Indigenous women, the rise was similar in major cities and regional areas, but was less marked in remote and very remote areas; it was greater in Western Australia, Queensland, and Victoria than elsewhere (Box 2, Box 3).
Multivariate analysis
In the multivariate analysis, the infectious syphilis notification rate was higher for Aboriginal and Torres Strait Islander women than for non‐Indigenous women (IRR, 23.1; 95% CI, 19.7–27.1). Among Aboriginal or Torres Strait Islander and non‐Indigenous women combined, the rate was lower for 15–24‐year‐old (IRR, 0.7; 95% CI, 0.6–0.9) and 35–44‐year‐old women (IRR, 0.6; 95% CI, 0.5–0.7) than for 25–34‐year‐old women, and was higher for women living in remote regions than for women living in major cities (IRR, 2.7; 95% CI, 2.2–3.8). It was higher for women living in the Northern Territory (IRR, 6.9; 95% CI, 5.1–9.2), Queensland (IRR, 4.7; 95% CI, 3.7–6.0), Victoria (IRR, 3.1; 95% CI, 2.4–4.0), and Western Australia (IRR, 3.0; 95% CI, 2.4–3.9) than for women in New South Wales (Box 4).
Congenital syphilis notifications
During 2011–2021, 74 cases of congenital syphilis were notified in Australia (Aboriginal or Torres Strait Islander infants, 40; non‐Indigenous infants, 32; unknown Indigenous status, two) (Box 5). In fifty‐eight cases, their mothers were born in Australia; in 41 cases, the mothers lived in major cities. During 2011–2019, the median annual number of notified cases was four (interquartile range, 3–7); 17 cases were reported in 2020, 15 cases in 2021. The overall rate of congenital syphilis ranged between 0.0 (2012) and 5.8 cases per 100 000 live births (2020); the rate among Aboriginal or Torres Strait Islander babies was consistently higher than among non‐Indigenous babies (2021: 38.3 v 2.1 per 100 000 live births) (Box 6).
Twelve of the 40 Aboriginal and Torres Strait Islander babies with congenital syphilis were stillborn, one later died of syphilis‐related causes, ten were born with clinical signs of congenital syphilis, and 14 were born without symptoms of syphilis; 12 were born in major cities, 13 in inner or outer regional areas, and 14 in remote or very remote areas. The mothers of 24 Aboriginal and Torres Strait Islander infants had not received antenatal care. Thirteen mothers had been screened for syphilis during pregnancy, and 26 had not. Four mothers had been diagnosed with syphilis during the third trimester of pregnancy, 12 on the day of delivery, and ten after their child was born. Thirty‐four mothers had been treated for syphilis within 14 days of diagnosis; four had been treated for syphilis more than 30 days before delivery (Box 5).
Four of the 32 non‐Indigenous babies with congenital syphilis were stillborn, 15 were born with clinical signs of congenital syphilis, nine were born without symptoms of syphilis, and four had other outcomes (not defined); 27 were born in major cities, four in inner or outer regional areas, and one in a remote area. The mothers of ten infants had commenced antenatal care during the first trimester, four during the second trimester, and five during the third trimester of their pregnancy; eight mothers did not receive antenatal care. Fifteen women had been screened for syphilis during pregnancy, and 15 had not. Nine mothers had been diagnosed with syphilis during the third trimester, six on the day of delivery, and 13 after their child was born. Twenty‐seven mothers had been treated for syphilis within 14 days of diagnosis; three women were treated for syphilis more than 30 days prior to delivery (Box 5).
Discussion
The annual number of infectious syphilis notifications for Australian women aged 15–44 years increased from 141 in 2011 to 902 in 2021; the annual number of infants born with congenital syphilis increased from six to fifteen. These rises, which affected both non‐Indigenous and Aboriginal or Torres Strait Islander women, together with our finding that many mothers of infants born with congenital syphilis received neither adequate antenatal care nor testing and treatment for syphilis, suggests that more needs to be done to ensure equitable access to appropriate antenatal care, especially for Aboriginal and Torres Strait Islander people.
The mean annual increase in the notification rate of infectious syphilis in women during 2011–2021 was about 20%; similar rates of increase during recent years have been reported in the United States,14 Canada,15 and Japan.16 Access to appropriate health care can influence syphilis rates, as exemplified by the fact that its incidence in Victoria, with one dedicated free sexual health service,17 was three times as high as in New South Wales, with more than twenty services across the state.18 Further, sexual health testing in remote areas of Australia is undertaken in primary care services, where factors such as conflicting care demands and staff capacity can affect testing for sexually transmissible infections.19
Social determinants of health, such as homelessness, unstable housing, poverty, racism and discrimination in health care, substance use, and imprisonment, have been associated with syphilis infection risk.20 A recent study of people attending sexual health clinics in Australia (2011–2019) found that rates of infectious syphilis were particularly high among women who reported recent injecting drug use, lived in areas of lower socio‐economic status, or were Aboriginal or Torres Strait Islander women.21 Alternative approaches for reaching people whose access to health care, including syphilis testing and management, is limited by social factors should be investigated. In the “no wrong door” approach, for example, screening for infectious diseases, such as syphilis, is offered routinely by a range of service providers, including drug and alcohol services. “No wrong door” approaches have been used to increase accessibility to care for substance use, mental health care, and HIV testing.22,23,24 In addition, approaches that improve the testing and management of people with positive test results by using new technology should be explored. For example, as dual treponemal/non‐treponemal point‐of‐care tests become available, alternative testing strategies could facilitate the immediate initiation of treatment, rather than waiting for standard laboratory test results.25,26
Preventing congenital syphilis relies on equitable access to antenatal care, adequate screening during pregnancy, contact tracing of partners, and appropriate treatment. Antenatal care guidelines recommend testing for syphilis during the first antenatal visit, or up to five tests during the course of the pregnancy, birth, and post partum period for women deemed to be at particular risk of infection.27 As part of global elimination efforts, the WHO routinely collects and reports the proportion of women receiving antenatal care who were tested for syphilis during any visit, data that are not consistently collected or reported in Australia as part of the National Perinatal Data Collection.28 National data on syphilis testing of pregnant women should be collated to ensure that testing coverage during antenatal care is consistent with the recommendations.
Overall, 32 of 72 mothers of babies with congenital syphilis (44%) had not received antenatal care during pregnancy, and a further nine received it only during the third trimester, suggesting barriers to such care for both Aboriginal and Torres Strait Islander and non‐Indigenous mothers. The proportion of mothers of Aboriginal and Torres Strait Islander infants with congenital syphilis who did not receive antenatal care (60%), however, was larger than that for non‐Indigenous infants’ mothers (25%). It is crucial that interventions for reducing the rates of infectious and congenital syphilis are co‐designed with the affected communities, and that a holistic approach to health care takes into account the complex and interconnected social factors that restrict access to health care for some women, particularly antenatal care.29,30 For Aboriginal and Torres Strait Islander women, access to evidence‐based, culturally appropriate antenatal services are recommended by national guidelines.31 In recent years, Birthing on Country maternity services have improved access to antenatal care and outcomes for babies, such as reducing the pre‐term birth rate.32 The increase in the number of congenital syphilis cases reported during 2020 and 2021 also suggests interruptions to antenatal care, probably because of COVID‐19‐related restrictions.
Limitations
Syphilis notification numbers may be influenced by changes in testing patterns, public health campaigns, and changes to diagnostic technology. We did not have access to the testing data (eg, positive test result rates) needed to determine whether infectious syphilis notification numbers were influenced by testing patterns. Secondly, we could not explore birth outcomes for all pregnant women with infectious syphilis (that is, we reported outcomes only for mothers of children with congenital syphilis) because the pregnancy status of women with syphilis was not routinely collected in all jurisdictions during the study period. Finally, we could not assess the impact of social determinants of health, as the relevant information was not included in the notifications data.
Conclusion
Infectious and congenital syphilis is an increasingly important public health problem in Australia. Rates of infectious syphilis increased during 2011–2021 among both Aboriginal and Torres Strait Islander and non‐Indigenous women of reproductive age, particularly among Aboriginal or Torres Strait Islander women living in remote areas. More potent responses are needed to control syphilis in Australia, including alternative testing approaches, such as new point‐of‐care testing technologies and “no wrong door” approaches. A collaborative and co‐design process involving the affected communities is needed to ensure equitable access to appropriate diagnosis, treatment, and care options.
Box 1 – Infectious syphilis notification rate for women aged 15–44 years, Australia, 2011–2021, by Indigenous status and age group*
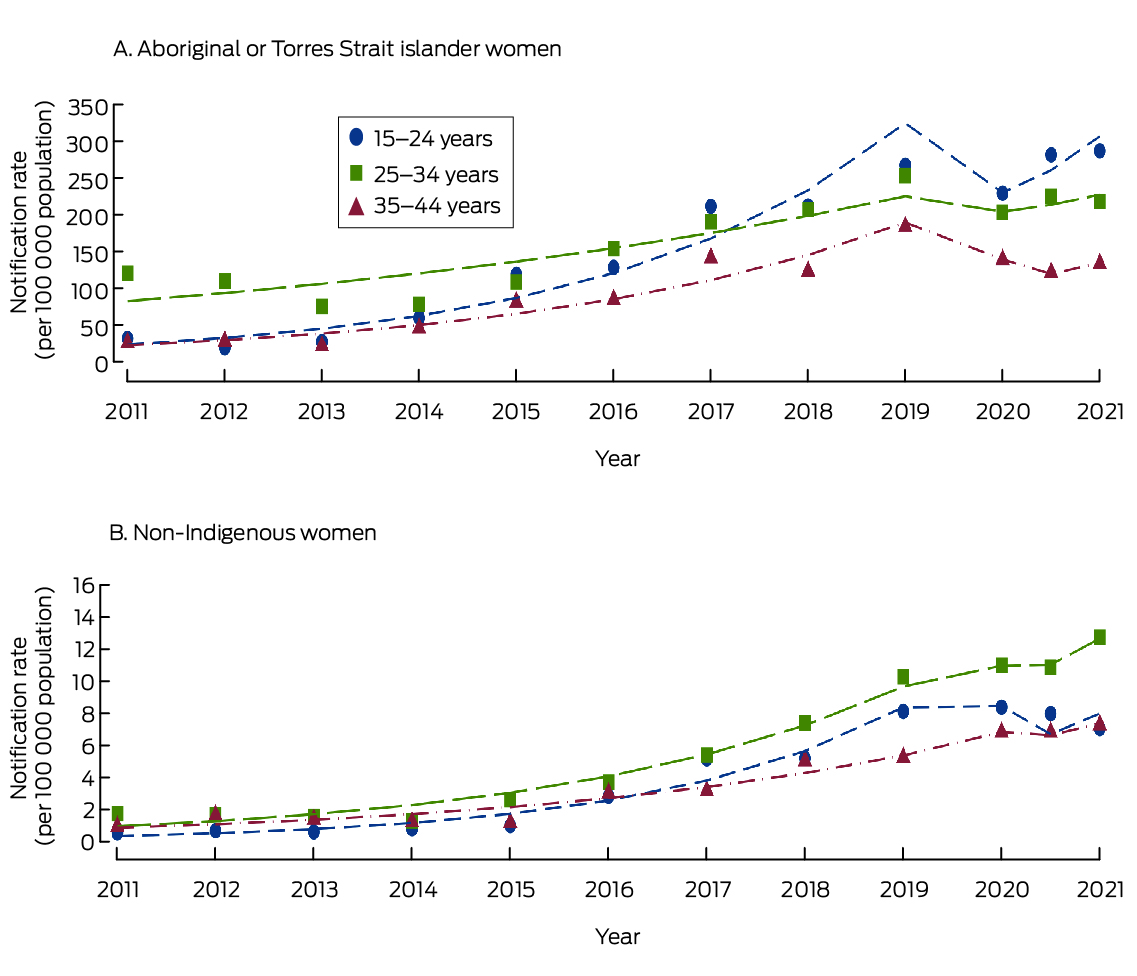
* Midpoint of 2020 also included to reflect effect of pandemic‐related lockdowns. The fitted curves are based on negative binomial regression models for each age group and Indigenous status category, with continuous time variable and binary indicator term for pandemic‐related lockdown status. The data for this graph are included in the Supporting Information, table 1.
Box 2 – Infectious syphilis notification rate for women aged 15–44 years, Australia, 2011–2021, by Indigenous status and geographic location*
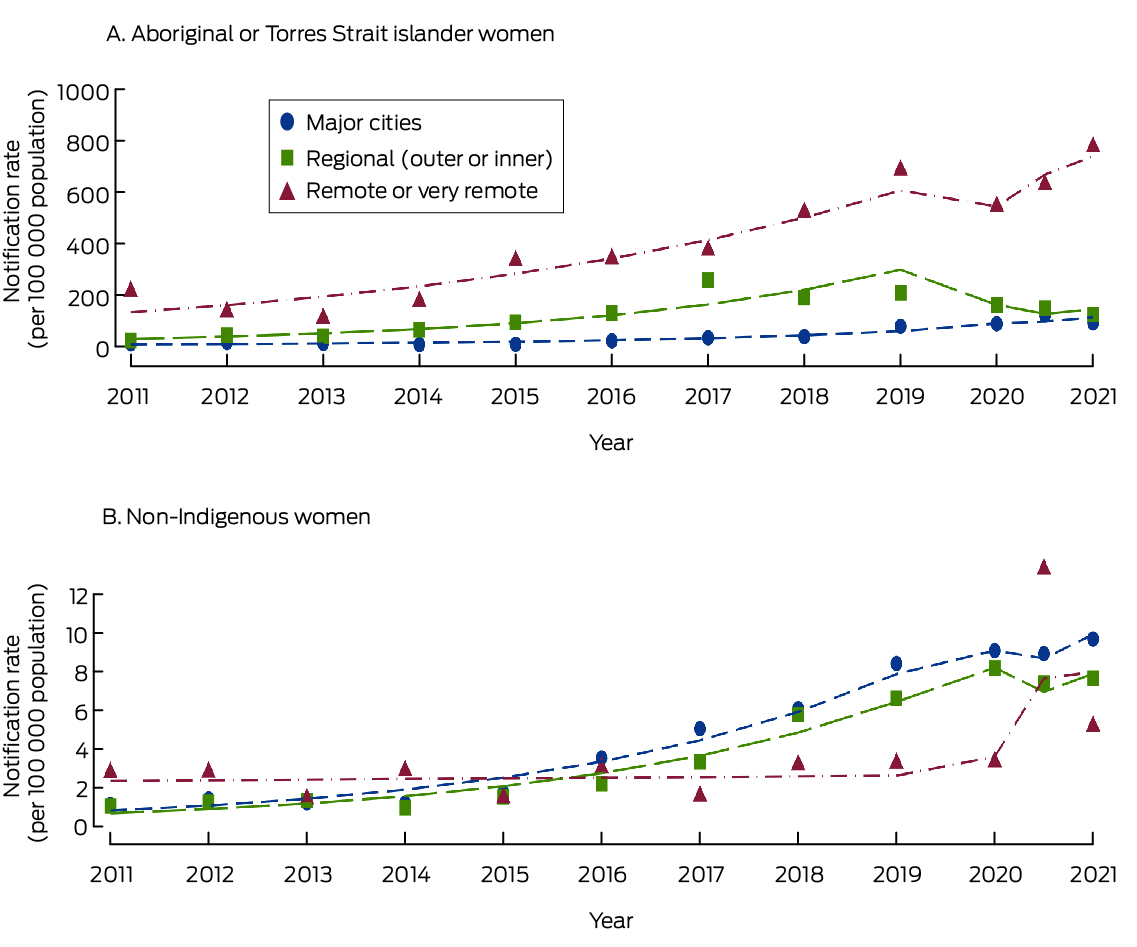
* Midpoint of 2020 also included to reflect effect of pandemic‐related lockdowns. The fitted curves are based on negative binomial regression models for each age group and Indigenous status category, with continuous time variable and binary indicator term for pandemic‐related lockdown status. The data for this graph are included in the Supporting Information, table 2.
Box 3 – Infectious syphilis notification rate for women aged 15–44 years, Australia, 2011–2021, by Indigenous status and state/territory*
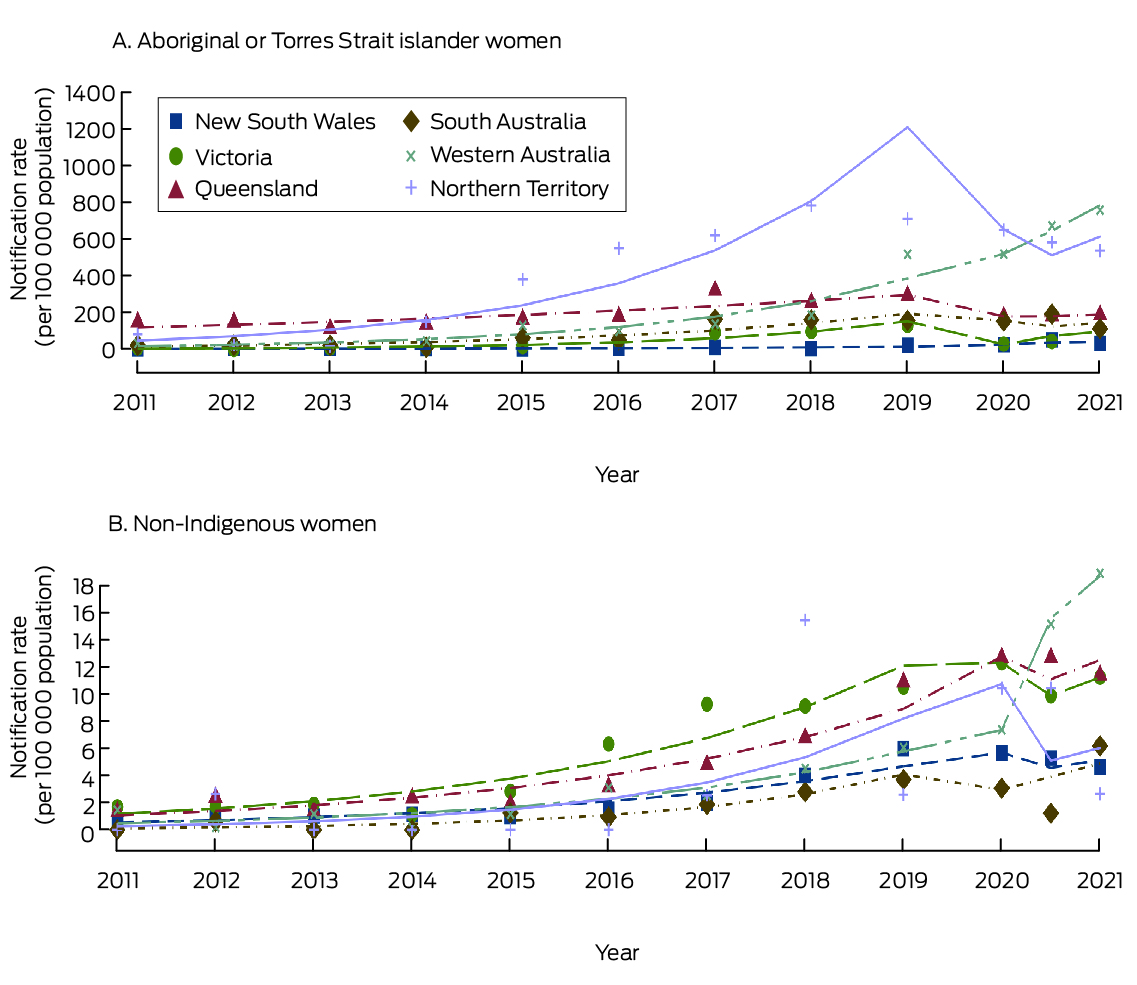
* Midpoint of 2020 also included to reflect effect of pandemic‐related lockdowns. Data for Tasmania and the Australian Capital territory are not depicted because of the low number of cases (2011–2021: Tasmania, eight cases; ACT, 17 cases). The fitted curves are based on negative binomial regression models for each age group and Indigenous status category, with continuous time variable and binary indicator term for pandemic‐related lockdown status. The data for this graph are included in the Supporting Information, table 3.
Box 4 – Notifications of infectious syphilis, Australia, 2011–2021: multivariate analysis
|
|
|
Incidence rate ratio (95% confidence interval) |
|||||||||||||
|
Characteristics |
Cases |
Univariate analysis |
Multivariate analysis* |
||||||||||||
|
|
|||||||||||||||
|
Total number of notifications |
5011 |
|
|
||||||||||||
|
Change in annual number (per year) |
— |
1.2 (1.2–1.3) |
1.3 (1.3–1.3) |
||||||||||||
|
Indigenous status |
|
|
|
||||||||||||
|
Aboriginal or Torres Strait Islander |
2735 |
43.5 (35.8–52.8) |
23.1 (19.7–27.1) |
||||||||||||
|
Non‐Indigenous |
2276 |
1 |
1 |
||||||||||||
|
Age group (years) |
|
|
|
||||||||||||
|
15–24 |
1857 |
0.8 (0.6–1.1) |
0.7 (0.6–0.9) |
||||||||||||
|
25–34 |
2087 |
1 |
1 |
||||||||||||
|
35–44 |
1067 |
0.5 (0.3–0.7) |
0.6 (0.5–0.7) |
||||||||||||
|
Geographic location11 |
|
|
|
||||||||||||
|
Major city |
2124 |
1 |
1 |
||||||||||||
|
Inner and outer regional |
1367 |
3.5 (2.5–4.8) |
1.2 (1.0–1.5) |
||||||||||||
|
Remote and very remote |
1520 |
6.2 (4.5–8.7) |
2.7 (2.2–3.8) |
||||||||||||
|
State/territory |
|
|
|
||||||||||||
|
New South Wales |
524 |
1 |
1 |
||||||||||||
|
Victoria |
973 |
3.2 (1.9–5.4) |
3.1 (2.4–4.0) |
||||||||||||
|
Queensland |
1637 |
16.0 (10.1–25.4) |
4.7 (3.7–6.0) |
||||||||||||
|
South Australia |
159 |
6.3 (3.8–10.5) |
1.7 (1.3–2.3) |
||||||||||||
|
Western Australia |
877 |
16.4 (10.4–26.0) |
3.0 (2.4–3.9) |
||||||||||||
|
Tasmania |
8 |
0.1 (0.0–0.3) |
0.2 (0.1–0.4) |
||||||||||||
|
Northern Territory |
816 |
34.4 (20.9–56.6) |
6.9 (5.1–9.2) |
||||||||||||
|
Australian Capital Territory |
17 |
0.4 (0.1–0.9) |
0.9 (0.5–1.6) |
||||||||||||
|
|
|||||||||||||||
|
* Adjusted for age group, geographic region (remoteness), and state/territory. |
|||||||||||||||
Box 5 – Notifications of congenital syphilis, Australia, 2011–2021, by Indigenous status
|
|
Indigenous status of infant |
|
|||||||||||||
|
Characteristic |
Aboriginal or Torres Strait Islander |
Non‐Indigenous |
Unknown |
All people |
|||||||||||
|
|
|||||||||||||||
|
Number of congenital syphilis cases reported |
40 |
32 |
2 |
74 |
|||||||||||
|
Geographic location11 |
|
|
|
|
|||||||||||
|
Major cities |
12 (30%) |
27 (84%) |
2 |
41 (55%) |
|||||||||||
|
Inner and outer regional |
13 (33%) |
4 (13%) |
0 |
17 (23%) |
|||||||||||
|
Remote and very remote |
14 (35%) |
1 (3%) |
0 |
15 (20%) |
|||||||||||
|
Missing data |
1 (3%) |
0 |
0 |
1 (1%) |
|||||||||||
|
Clinical outcome for baby |
|
|
|
|
|||||||||||
|
Live birth, asymptomatic |
14 (35%) |
9 (28%) |
1 |
24 (32%) |
|||||||||||
|
Live birth, clinical signs |
10 (25%) |
15 (47%) |
0 |
25 (34%) |
|||||||||||
|
Live birth, died of syphilis‐related cause |
1 (3%) |
0 |
0 |
1 (1%) |
|||||||||||
|
Syphilis‐related stillbirth |
12 (30%) |
4 (13%) |
1 |
17 (23%) |
|||||||||||
|
Other (including late presentation) |
3 (8%) |
4 (13%) |
0 |
7 (9%) |
|||||||||||
|
Stage of pregnancy (syphilis diagnosis) |
|
|
|
|
|||||||||||
|
1st trimester |
0 |
2 (6%) |
0 |
2 (3%) |
|||||||||||
|
2nd trimester |
6 (15%) |
1 (3%) |
0 |
7 (9%) |
|||||||||||
|
3rd trimester |
11 (28%) |
9 (28%) |
0 |
20 (27%) |
|||||||||||
|
Day of delivery |
12 (30%) |
6 (19%) |
0 |
18 (24%) |
|||||||||||
|
After birth |
10 (25%) |
13 (41%) |
2 |
25 (34%) |
|||||||||||
|
Missing data |
1 (3%) |
1 (3%) |
0 |
2 (3%) |
|||||||||||
|
Antenatal care first received |
|
|
|
|
|||||||||||
|
1st trimester |
5 (13%) |
10 (31%) |
2 |
17 (23%) |
|||||||||||
|
2nd trimester |
3 (8%) |
4 (13%) |
0 |
7 (9%) |
|||||||||||
|
3rd trimester |
4 (10%) |
5 (16%) |
0 |
9 (12%) |
|||||||||||
|
Did not receive antenatal care |
24 (60%) |
8 (25%) |
0 |
32 (43%) |
|||||||||||
|
Missing data |
4 (10%) |
5 (16%) |
0 |
9 (12%) |
|||||||||||
|
Syphilis screening (current pregnancy) |
|
|
|
|
|||||||||||
|
Yes |
13 (33%) |
15 (47%) |
1 |
29 (39%) |
|||||||||||
|
No |
26 (65%) |
15 (47%) |
1 |
42 (57%) |
|||||||||||
|
Missing data |
1 (3%) |
2 (6%) |
0 |
3 (4%) |
|||||||||||
|
Mother treated for syphilis within 14 days of diagnosis |
|
|
|
|
|||||||||||
|
Yes |
34 (85%) |
27 (84%) |
2 |
63 (85%) |
|||||||||||
|
No |
5 (13%) |
2 (6%) |
0 |
7 (9%) |
|||||||||||
|
Missing data |
1 (3%) |
3 (9%) |
0 |
4 (5%) |
|||||||||||
|
Mother received adequate treatment for syphilis more than 30 days prior to delivery |
|
|
|
|
|||||||||||
|
Yes |
4 (10%) |
3 (9%) |
0 |
7 (9%) |
|||||||||||
|
No |
34 (85%) |
26 (81%) |
2 |
62 (84%) |
|||||||||||
|
Missing data |
2 (5%) |
3 (9%) |
0 |
5 (7%) |
|||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 6 – Numbers and rate of notifications of congenital syphilis, Australia, 2011–2021, by Indigenous status*
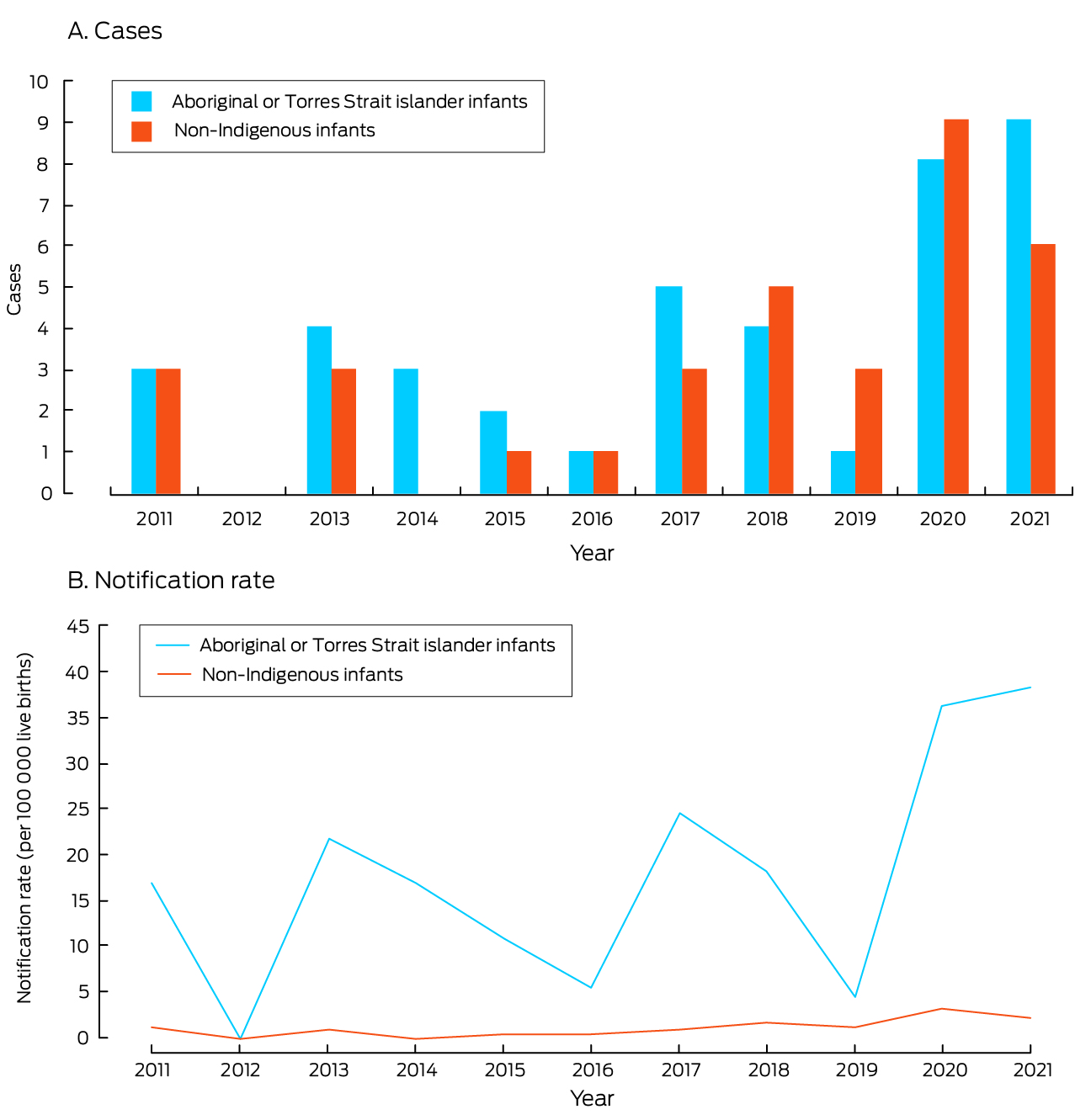
* Indigenous status was not recorded for two cases (2019, 2020); they are classified as “non‐Indigenous” in this figure. The data underlying this graph are included in the Supporting Information, table 4.
Received 11 September 2023, accepted 15 April 2024
- Belinda Hengel1
- Hamish McManus1
- Robert Monaghan1
- Donna B Mak2,3
- Amy Bright4
- Ximena Tolosa5
- Kellie Mitchell3
- Lorraine Anderson1,6
- Jackie R Thomas1
- Nathan Ryder7
- Louise Causer1
- Rebecca J Guy1
- Skye McGregor1
- 1 The Kirby Institute, Sydney, NSW
- 2 University of Notre Dame Australia, Fremantle, WA
- 3 Communicable Disease Control Directorate, Western Australia Department of Health, Perth, WA
- 4 Office of Health Protection, Australian Department of Health, Canberra, ACT
- 5 Public Health Intelligence Branch, Queensland Department of Health, Brisbane, QLD
- 6 Kimberley Aboriginal Medical Services Council Inc, Broome, WA
- 7 Sexual Health Pacific Clinic, Hunter New England, Newcastle, NSW
Open access:
Open access publishing facilitated by University of New South Wales, as part of the Wiley – University of New South Wales agreement via the Council of Australian University Librarians.
Data sharing:
Applications for access to the data we analysed for this study should be directed to the Australian Department of Health and Aged Care.
We acknowledge the contribution and valuable insights of the Kirby Institute Aboriginal and Torres Strait Islander Reference Group, and State and Territory Health Department surveillance officers.
No relevant disclosures.
- 1. Hook EW. Syphilis. Lancet 2017; 389: 1550‐1557.
- 2. Gomez GB, Kamb ML, Newman LM, et al. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta‐analysis. Bull World Health Organ 2013; 91: 217‐226.
- 3. Hawkes SJ, Gomez GB, Broutet N. Early antenatal care: does it make a difference to outcomes of pregnancy associated with syphilis? A systematic review and meta‐analysis. PLoS One 2013; 8: e56713.
- 4. World Health Organization. Syphilis. 21 May 2024. https://www.who.int/news‐room/fact‐sheets/detail/syphilis (viewed July 2024).
- 5. World Health Organization. Global guidance on criteria and processes for validation: elimination of mother‐to‐child transmission of HIV, syphilis and hepatitis B virus. Geneva: World Health Organization, 2021. https://www.who.int/publications/i/item/9789240039360 (viewed Jan 2023).
- 6. King J, McManus H, Kwon A, et al. HIV, viral hepatitis and sexually transmissible infections in Australia: annual surveillance report 2022. Sydney: Kirby Institute; UNSW Sydney, 2022. https://www.kirby.unsw.edu.au/sites/default/files/documents/Annual‐Surveillance‐Report‐2022_STI.pdf (viewed Jan 2023).
- 7. Read P, Fairley CK, Chow EP. Increasing trends of syphilis among men who have sex with men in high income countries. Sex Health 2015; 12: 155‐163.
- 8. Australian Department of Health and Aged Care. National response to syphilis. Updated 12 July 2022. https://www.health.gov.au/our‐work/national‐response‐to‐syphilis (viewed Jan 2023).
- 9. Australian Department of Health and Aged Care. National Notifiable Diseases Surveillance System (NNDSS). Updated 19 July 2023. https://www.health.gov.au/our‐work/nndss (viewed July 2023).
- 10. Australian Institute of Health and Welfare. Australia's mothers and babies. Updated 13 Dec 2023. Australia's mothers and babies. https://www.aihw.gov.au/reports/mothers‐babies/australias‐mothers‐babies/contents/summary (viewed July 2024).
- 11. Australian Bureau of Statistics. Remoteness areas. Australian Statistical Geography Standard (ASGS) edition 3, July 2021 – June 2026. 21 Mar 2023. https://www.abs.gov.au/statistics/standards/australian‐statistical‐geography‐standard‐asgs‐edition‐3/jul2021‐jun2026/remoteness‐structure/remoteness‐areas (viewed May 2023).
- 12. Australian Department of Health and Aged Care. CDNA surveillance case definitions. 29 May 2022. https://www.health.gov.au/resources/collections/cdna‐surveillance‐case‐definitions (viewed Jan 2023).
- 13. von Elm E, Altman DG, Egger M, et al; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453‐1457.
- 14. National Centre for HIV, Viral Hepatitis, STD, and TB Prevention (Centers for Disease Control and Prevention). Syphilis surveillance supplemental slides, 2016–2020. Updated 30 Jan 2024. https://www.cdc.gov/std/statistics/syphilis‐supplement/default.htm (viewed Jan 2024).
- 15. Aho J, Lybeck C, Tetteh A, et al. Rising syphilis rates in Canada, 2011–2020. Can Commun Dis Rep 2022; 48: 52‐60.
- 16. Takahashi T, Arima Y, Yamagishi T, et al. Rapid increase in reports of syphilis associated with men who have sex with women and women who have sex with men, Japan, 2012 to 2016. Sex Transm Dis 2018; 45: 139‐143.
- 17. Victorian Department of Health. (December 2023). Programs and services for sexual health, viral hepatitis and HIV. 7 Dec 2023. https://www.health.vic.gov.au/preventive‐health/programs‐and‐services‐for‐sexual‐health‐and‐viral‐hepatitis (viewed July 2024).
- 18. NSW Health. NSW sexual health clinics. Updated 5 June 2024. https://www.health.nsw.gov.au/sexualhealth/Pages/sexual‐health‐clinics.aspx (viewed June 2024).
- 19. Hengel B, Guy R, Garton L, et al. Barriers and facilitators of sexually transmissible infection testing in remote Australian Aboriginal communities: results from the Sexually Transmitted Infections in Remote Communities, Improved and Enhanced Primary Health Care (STRIVE) Study. Sex Health 2015; 12: 4‐12.
- 20. Johnson KA, Snyder RE, Tang EC, et al. Geospatial social determinants of health correlate with disparities in syphilis and congenital syphilis cases in California. Pathogens 2022; 11: 547.
- 21. Carter A, McManus H, Ward JS, et al. Infectious syphilis in women and heterosexual men in major Australian cities: sentinel surveillance data, 2011–2019. Med J Aust 2023; 218: 223‐228. https://www.mja.com.au/journal/2023/218/5/infectious‐syphilis‐women‐and‐heterosexual‐men‐major‐australian‐cities‐sentinel
- 22. Collins B, Bronson H, Elamin F, et al. The “no wrong door” approach to HIV testing: results from a statewide retail pharmacy‐based HIV testing program in Virginia, 2014–2016. Public Health Rep 2018; 133(2 Suppl): 34S‐42S.
- 23. Abdel‐Baki A, Aubin D, Morisseau‐Guillot R, et al. Improving mental health services for homeless youth in downtown Montreal, Canada: partnership between a local network and ACCESS Esprits ouverts (Open Minds), a National Services Transformation Research initiative. Early Interv Psychiatry 2019; 13(Suppl 1): 20‐28.
- 24. South Western Sydney PHN. No Wrong Door initiative. 2024. https://swsphn.com.au/what‐we‐do/mental‐health/no‐wrong‐door‐initiative (viewed Jan 2024).
- 25. Angel‐Müller E, Grillo‐Ardila CF, Amaya‐Guio J, et al. Diagnostic accuracy of rapid point‐of‐care tests for detecting active syphilis: a systematic review and meta‐analysis. Sex Transm Dis 2021; 48: e202‐e208.
- 26. Zhang Y, Goh SM, Mello MB, et al. Improved rapid diagnostic tests to detect syphilis and yaws: a systematic review and meta‐analysis. Sex Transm Infect 2022; 98: 608‐616.
- 27. Australian Department of Health and Aged Care. Pregnancy care guidelines. 2020. Updated 26 Apr 2024. https://www.health.gov.au/resources/pregnancy‐care‐guidelines/part‐f‐routine‐maternal‐health‐tests/syphilis#362‐syphilis‐testing (viewed June 2024).
- 28. Australian Institute of Health and Welfare. National Perinatal Data Collection. Updated 14 Mar 2024. https://www.aihw.gov.au/about‐our‐data/our‐data‐collections/national‐perinatal‐data‐collection (viewed June 2023).
- 29. Park E, Yip J, Harville E, et al. Gaps in the congenital syphilis prevention cascade: qualitative findings from Kern County, California. BMC Infect Dis 2022; 22: 129.
- 30. Willemsma K, Barton L, Stimpson R, et al. Characterizing female infectious syphilis cases in British Columbia to identify opportunities for optimization of care. Can Commun Dis Rep 2022; 48: 68‐75.
- 31. Council of Australian Governments Health Council. Woman‐centred care: strategic directions for Australian maternity services. 2019. Updated 23 Aug 2022. https://www.health.gov.au/resources/publications/woman‐centred‐care‐strategic‐directions‐for‐australian‐maternity‐services?language=en (viewed June 2023).
- 32. Kildea S, Gao Y, Hickey S, et al. Effect of a Birthing on Country service redesign on maternal and neonatal health outcomes for First Nations Australians: a prospective, non‐randomised, interventional trial. Lancet Glob Health 2021; 9: e651‐e659.






Abstract
Objectives: To estimate notification rates for infectious syphilis in women of reproductive age and congenital syphilis in Australia.
Study design: Retrospective cohort study; analysis of national infectious syphilis and enhanced congenital syphilis surveillance data.
Setting, participants: Women aged 15–44 years diagnosed with infectious syphilis, and babies with congenital syphilis, Australia, 2011–2021.
Main outcome measures: Numbers and rates of infectious syphilis notifications, by Indigenous status and age group; numbers and rates of congenital syphilis, by Indigenous status of the infant; antenatal care history for mothers of infants born with congenital syphilis.
Results: During 2011–2021, 5011 cases of infectious syphilis in women aged 15–44 years were notified. The notification rate for Aboriginal and Torres Strait Islander women rose from 56 (95% confidence interval [CI], 45–65) cases per 100 000 in 2011 to 227 (95% CI, 206–248) cases per 100 000 population in 2021; for non‐Indigenous women, it rose from 1.1 (95% CI, 0.8–1.4) to 9.2 (95% CI, 8.4–10.1) cases per 100 000 population. The notification rate was higher for Aboriginal and Torres Strait Islander women than for non‐Indigenous women (incidence rate ratio [IRR], 23.1; 95% CI, 19.7–27.1), lower for 15–24‐ (IRR, 0.7; 95% CI, 0.6–0.9) and 35–44‐year‐old women (IRR, 0.6; 95% CI, 0.5–0.7) than for 25–34‐year‐old women, and higher in remote regions than in major cities (IRR, 2.7; 95% CI, 2.2–3.8). During 2011–2021, 74 cases of congenital syphilis were notified, the annual number increasing from six in 2011 to a peak of 17 in 2020; the rate was consistently higher among Aboriginal and Torres Strait Islander infants than among non‐Indigenous infants (2021: 38.3v 2.1 per 100 000 live births). The mothers of 32 infants with congenital syphilis (43%) had not received antenatal care.
Conclusions: The number of infectious syphilis notifications for women of reproductive age increased in Australia during 2011–2021, as did the number of cases of congenital syphilis. To avert congenital syphilis, antenatal screening of pregnant women, followed by prompt treatment for infectious syphilis when diagnosed, needs to be improved.