Falls present a major, growing and neglected public health problem with devastating consequences for older individuals, their families and health care systems.
The recently published World guidelines for falls prevention and management for older adults: a global initiative1 (Guidelines) is a comprehensive document that provides extensive recommendations with additional background materials available on an accompanying website. The Guidelines is a consensus document informed by systematic reviews and a Delphi process. This body of work demonstrates that much is known about what works in falls prevention but there is considerable complexity. The main message is that most falls occur due to a loss of balance while upright or walking, and the most important intervention to prevent this is exercise. Rare causes such as cardioinhibitory syncope are also described. The Guidelines includes important messages about the older person's perspective, and which interventions are effective in hospitals and residential aged care facilities.
The Guidelines1 explicitly states that although we know what interventions are effective, we still need to know how best to implement these interventions in our busy health systems. This perspective article aims to provide a digestible version of the most important points from the Guidelines that may be applied in general health and medical settings. For some of the points, we have added our interpretation of additional scientific information that is relevant to a clinical audience. Some solutions need to be implemented outside of our health systems, such as through community awareness, promotion of lifelong exercise, and provision of safe accessible environments.
Following the Guidelines structure, which highlights the importance of tailored intervention rather than a detailed assessment, this article first discusses effective interventions and thereafter addresses assessment.
Exercise
Exercise is the key intervention to prevent falls and fall injuries. The clear benefits of physical activity and exercise in the prevention and management of most conditions affecting older people (eg, frailty, sarcopenia, dementia, cardiovascular disease, chronic respiratory disease, diabetes, stroke and hip fracture) are highlighted in many previous reviews and guidelines, including the World Health Organization (WHO) guidelines on physical activity and sedentary behaviour.2
Exercise is defined as a “subcategory of physical activity that is planned, structured, repetitive, and purposeful in the sense that the improvement or maintenance of one or more components of physical fitness is the objective”.2 Exercises shown to prevent falls primarily involve control of the body in space, such as while standing, and moving from sitting to standing to walking, that is, functional activities that older people need to be able to complete each day to maximise independence. Such exercises involve using body weight as resistance to improve strength, and gradually narrowing the base of support to improve balance. Priority exercises involve moving from sit to stand and undertaking activities to challenge balance. The evidence shows that improving balance should be prioritised and resistance training may be added.1,3 To ensure effectiveness and safety, exercises are tailored to individual abilities, and are progressive and ongoing. Box 1 shows basic exercises for frail older people.4,5
Medical practitioners should introduce the exercises, demonstrate them, and prescribe them for low risk older people. This use of evidence‐based non‐pharmacological treatment can be termed the “green prescription”6 or “social prescribing” of exercise.7 In the prescription are the exercises to be performed, and the individualised “dose” (sets and frequency specified).8 The older person's preferences and the risk of injury and other adverse effects should be considered and managed. Review and progression of intensity of the exercise is required. Intermediate and high risk older people, or older people with a recent significant injury, should be referred to an appropriate health professional providing exercise therapy, for example a physiotherapist or an exercise physiologist. Low risk older people may be encouraged to join a suitable local community exercise opportunity where available.
For maximum effect, the strength and balance exercise program should have three or more sessions per week.1,3 Programs lasting three to six months may be effective3 but ideally fall prevention programs should be lifelong. Unless exercise is continued, detraining occurs over three to six months.1 This means that encouragement to adhere to exercise is important, and also suggests that a continuing exercise program will be required for many older people with disabilities or frailty to maintain benefit.
Careful attention should be given to factors that will improve adherence to the exercise program, such as a therapeutic alliance between the patient and the health care professional, individual exercise program adaptation, involvement of others (spouse or carer), and use of appropriate environments such as a gym, park, community centre or home. The goal should be to have a program that the older person may follow at home, or to identify a group exercise class that is appropriate, accessible and affordable. Medical practitioners may have an important role supporting older people to identify a suitable way to incorporate ongoing exercise into their days9 or may refer to others for this task.
Information about fall prevention is now more readily available. HealthPathways is an online health information portal designed for Australian general practice and primary health care professionals.10 The HealthPathways website provides information on falls assessment and interventions that are available to general practitioners and patients.
Other effective interventions
There are now many effective fall prevention interventions for specific health conditions. For example, we know that cataract surgery may prevent falls and fractures in affected individuals, and that podiatry intervention may prevent falls in people with foot pain.1,11 There is potential complexity as many factors can potentially contribute to falls, and the goal is to be aware of what these interventions are and consider whether they apply to the particular older person being assessed. The older person will need adequate information to consider the different intervention types. Their adherence with the intervention will be better if they understand and participate in formulation of the intervention plan.
Clinicians need a structure to consider the different health conditions causing falls. One approach is to consider a list of common concerns (Box 2), whereas another approach is to consider body systems and how changes in these lead to falls. This could be central nervous system (impaired cognition, and specific neurological conditions such as dementia, Parkinson disease and past stroke with disability), musculoskeletal (past fracture or significant injury, major foot problems, significant chronic arthritis), cardiovascular disease (hypotension, syncope), and impairment of vision and hearing. It is important to consider the significant external factors including medications (anticholinergics, psychotropics and opioids), the home environment (particularly if there has been recent hospitalisation or there is significant visual impairment), and discuss with and involve facility staff if the older person is living in a residential aged care facility.
Use of medications and deprescribing are controversial and complex. There is more to be learnt about optimal approaches but a reasonable approach is to reduce anticholinergic drugs, psychotropics (including antidepressants), and opioids, and to consider whether medications might be contributing to other problems such as cognitive difficulties and postural hypotension.1,13 The best medication intervention tool is unclear but STOPPfall12 may be recommended.
Interventions in other situations
Dementia
Exercise is effective in people with dementia to prevent falls,1,14 but programs will need to be modified and supervised, and may be built into daily activities. Establishing an active daily routine with opportunities for exercise and social contact is effective as is modifying risks in the home environment. Where funding is available, input from an occupational therapist, physiotherapist or exercise physiologist may establish and support these interventions.
Hospitals
Hospital staff have spent a lot of time and effort applying falls risk screening tools such as STRATIFY15 to patients. However, a cluster randomised non‐inferiority trial has shown that experienced health professionals are able to identify patients who are at a high risk of falls and may apply effective interventions.16 Clinicians did not assign risk scores and instead used clinical reasoning to select fall mitigation strategies using a decision support list. These include educational strategies and appropriate supervision (particularly in high risk activities such as toileting). Physical activity and opportunities for exercise should be encouraged. Bed rest and immobilisation should be avoided as these increase the risk of falling and deconditioning.
Residential aged care facilities
Almost all people living in residential aged care facilities will be vitamin D deficient unless taking a supplement.17 There is moderate evidence that vitamin D may prevent falls in these facilities.18 Exercise programs may be effective but need to be supervised to enable people to stand up to exercise. Recently it has been shown that facility staff working closely with older people and their families may establish an effective falls prevention program in residential aged care.19 Programs also need to be ongoing as benefits are lost quickly once ceased.
Linking with other conditions
The interventions outlined in this article are beneficial in many health conditions in older people.2 Therefore, in addition to reducing fall risk using these interventions, there is likely to be improvement in other conditions. An important aim is to address bone health in people with a high fall risk and who have had a past minimal trauma fracture. In addition to exercise, adequate vitamin D and dietary calcium, pharmacological treatment of established osteoporosis is beneficial with an established treatment gap.20
Assessment
Previously too much attention has been given to assessment rather than intervention. People of all ages are at risk of falls with injury because walking and more complex mobility tasks are intrinsically risky. For older people, falls cause more severe injuries than for younger people. Ageing, disease and deconditioning decrease peoples’ ability to recover from a trip or slip. Hip fracture and traumatic brain injury with hospitalisation (in an 85‐year‐old woman, the annual risks are about 3% and 0.5% respectively)21,22,23 are the greatest risks, but vertebral fractures and other lower extremity fractures also cause substantial morbidity and are associated with mortality.24
Assessment is not difficult and is within the capability of all health professionals. Older people with gait and balance problems are at a substantially increased risk of falling. The best predictor of a future fall is a past fall.1,13 If further data are needed, gait velocity may be measured with walking at slower than 0.8 m/s indicating a higher fall risk.1,25
The assessment algorithm shown in the diagram from the Guidelines [Box 3] stratifies risk as “high”, “intermediate” and “low” and emphasises community exercise and education for the low risk groups (such as people falling less than once a year), and more specialised exercise with input from a health professional for those falling one to two times a year. For the high risk group (ie, those falling more than twice a year), individualised assessments and interventions with scheduled follow‐up are recommended.
Conclusion
Falls and fall‐related injuries may be reduced or prevented using specific exercise interventions involving balance and strength training. Older people at high risk of injury may benefit from a targeted approach that is likely to include exercise and other components, including appropriate management of specific health conditions. The ageing of our population means our health systems need to quickly improve at preventing falls and subsequent injuries.26
Box 1 – Basic exercises for fall prevention,4 showing (A) standing with feet together (with object to hold for safety if required), progressing to standing with one leg in front of the other, then standing on one leg if able; (B) sitting to standing (make easier with a higher chair, make harder with a lower chair or by holding a weight); and (C) stepping in different directions (hold on, if necessary, progress to stepping more quickly and further)
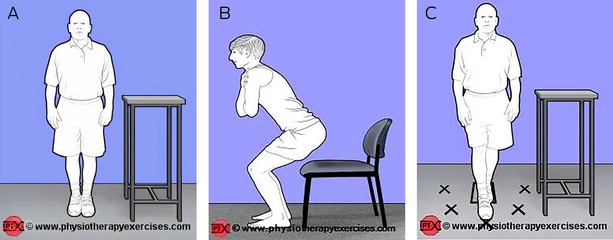
Reproduced with permission from www.physiotherapyexercises.com, which is freely available online exercise prescribing software for physiotherapists. Further advice for older adults from physiotherapists about safely undertaking exercises at home is available here https://www.safeexerciseathome.org.au/for‐older‐people
Box 2 – Examples of interventions for specific concerns
|
Concern |
Intervention |
||||||||||||||
|
|
|||||||||||||||
|
Slow or unstable gait |
|
||||||||||||||
|
Older person excessively concerned about falling and limits activities |
|
||||||||||||||
|
Fall with injury |
|
||||||||||||||
|
Cognitive impairment or dementia |
|
||||||||||||||
|
Parkinson disease or past stroke |
|
||||||||||||||
|
Syncope or presyncope |
|
||||||||||||||
|
Vision (and hearing) impairment |
|
||||||||||||||
|
Multiple medication use |
|
||||||||||||||
|
Pain associated with activity limitation |
|
||||||||||||||
|
|
|||||||||||||||
|
* Consider referral to allied health professional where available, for example, exercise prescription from physiotherapist or exercise physiologist, home and community safety from occupational therapist, cognitive behavioural support from psychologist, foot care and exercises from podiatrist. |
|||||||||||||||
Box 3 – Algorithm for risk stratification, assessments, management and interventions for community‐dwelling older adults1
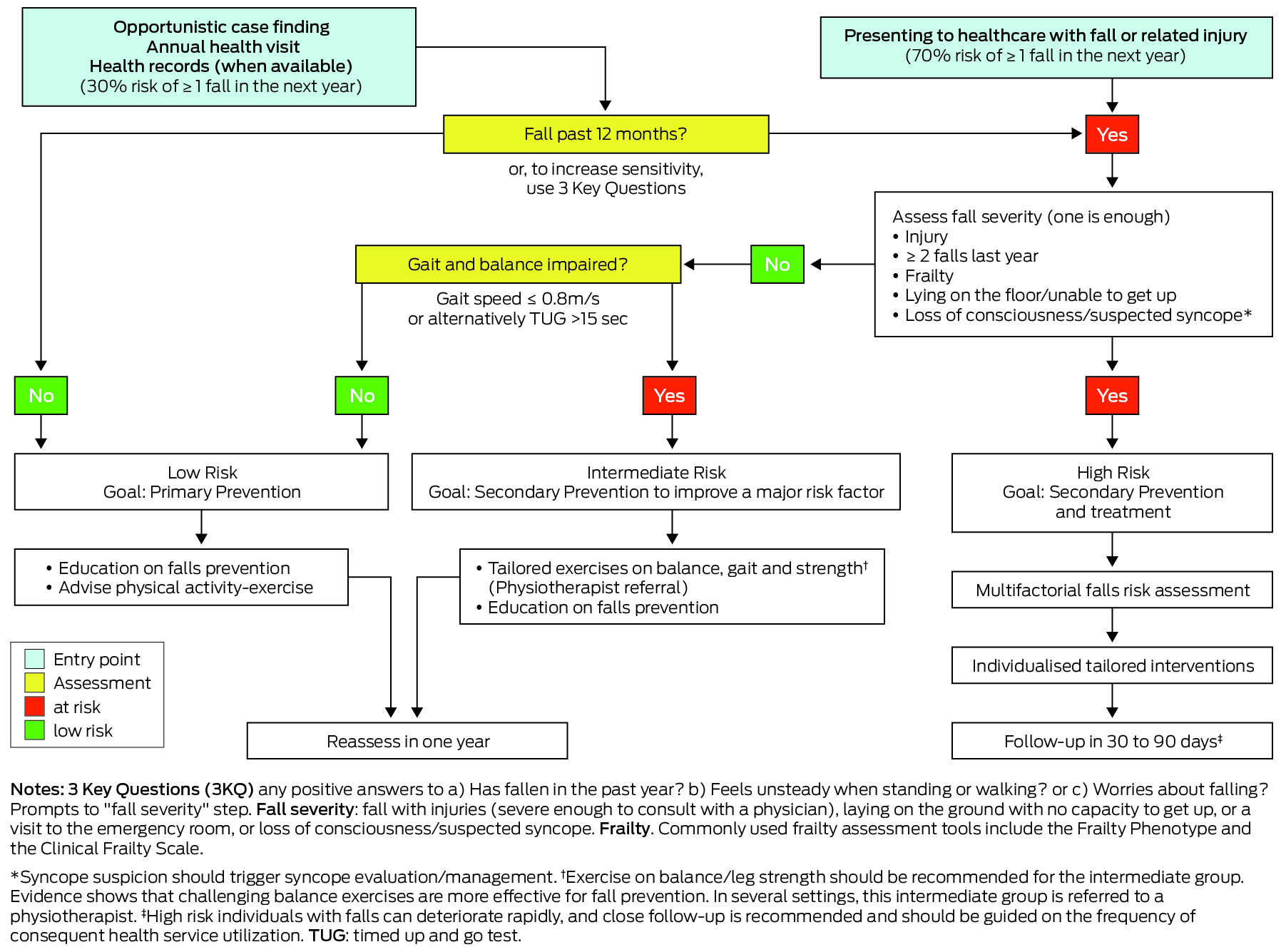
Reproduced under license from Oxford University Press.
Provenance: Commissioned; externally peer reviewed.
- 1. Montero‐Odasso M, van der Velde N, Martin FC, et al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing 2022; 51: 1‐36.
- 2. World Health Organization guidelines on physical activity and sedentary behaviour. Geneva, 2020. chrome‐extension://efaidnbmnnnibpcajpcglclefindmkaj/ https://iris.who.int/bitstream/handle/10665/336656/9789240015128‐eng.pdf?sequence=1 (viewed Feb 2024).
- 3. Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 2019; 1: CD012424.
- 4. PhysioTherapy eXercises (PTX) for people with injuries and disabilities [website]. www.physiotherapyexercises.com/ (viewed Feb 2024).
- 5. Safe Exercise at Home [website]. www.safeexerciseathome.org.au (viewed Feb 2024).
- 6. Health New Zealand. Green prescriptions [website]. www.health.govt.nz/your‐health/healthy‐living/food‐activity‐and‐sleep/green‐prescriptions (viewed Feb 2024).
- 7. World Health Organization. A toolkit on how to implement social prescribing. 2022. www.who.int/publications‐detail‐redirect/9789290619765 (viewed Feb 2024).
- 8. Royal Australian College of General Practitioners. Exercises for falls prevention [website]. www.racgp.org.au/clinical‐resources/clinical‐guidelines/handi/handi‐interventions/exercise/exercises‐for‐falls‐prevention (viewed Feb 2024).
- 9. Wirral age UK. Falls and frailty [website]. https://australia.movingmedicine.ac.uk/consultation‐guides/condition/adult/falls‐and‐frailty‐3/ (viewed Feb 2024).
- 10. Sydney North Health Network. Ageing well [website]. sydneynorthhealthnetwork.org.au/programs/aged‐care/#1692236643838‐c07d30dc‐5ef4 (viewed June 2024).
- 11. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012; 9: CD007146.
- 12. Amsterdam University Medical Centre. Decision advice for withdrawing medication in fallers. kik.amc.nl/falls/decision‐tree/ (viewed Feb 2024).
- 13. Ganz DA, Latham NK. Prevention of falls in community‐dwelling older adults. N Engl J Med 2020; 382: 734‐743.
- 14. Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta‐analysis. Br J Sports Med 2017; 51: 1750‐1758.
- 15. Castellini G, Demarchi A, Lanzoni M, Castaldi S. Fall prevention: is the STRATIFY tool the right instrument in Italian Hospital inpatient? A retrospective observational study. BMC Health Serv Res 2017; 17: 656.
- 16. Morris ME, Haines T, Hill AM, et al. Divesting from a scored hospital Fall Risk Assessment Tool (FRAT): a cluster randomized non‐inferiority trial. J Am Geriatr Soc 2021; 69: 2598‐2604.
- 17. Sambrook PN, Cameron ID, Cumming RG, Lord SR, Schwarz JM, Trube A, March LM. Vitamin D deficiency is common in frail institutionalised older people in northern Sydney. Med J Aust 2002; 176: 560. https://www.mja.com.au/journal/2002/176/11/vitamin‐d‐deficiency‐common‐frail‐institutionalised‐older‐people‐northern
- 18. Cameron ID, Dyer SM, Panagoda CE, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 2018; 9: CD005465.
- 19. Logan PA, Horne JC, Gladman JRF, et al. Multifactorial falls prevention programme compared with usual care in UK care homes for older people: multicentre cluster randomised controlled trial with economic evaluation. BMJ 2021; 375: e066991.
- 20. Halim NK, Harris RG, Cameron ID, et al. Two‐country comparison of the prescription of bone protection medication before and early after hip fracture. Arch Osteoporos 2022; 18: 8.
- 21. Seeman E, Ugoni AM, Pasco JA et al. Age‐ and gender‐specific rate of fractures in Australia: a population‐based study. Osteoporos Int 1999; 10: 240‐247.
- 22. Pozzato I, Tate RL, Rosenkoetter U, Cameron ID. Epidemiology of hospitalised traumatic brain injury in the state of New South Wales, Australia: a population‐based study. Aust N Z J Public Health 2019; 43: 382‐388.
- 23. Sanders KM, Seeman E, Ugoni AM, et al. Age‐ and gender‐specific rate of fractures in Australia: a population‐based study. Osteoporos Int 1999; 10: 240‐247.
- 24. Mitchell PJ, Chan DD, Lee JK, et al. The global burden of fragility fractures ‐ what are the differences, and where are the gaps. Best Pract Res Clin Rheumatol 2022; 36: 101777.
- 25. Cruz‐Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019; 48: 16‐31.
- 26. Delbaere K, Elkington J, Lord SR, et al. The rising cost of falls ‐ Health researchers are calling for action. Australas J Ageing 2022; 41: 487‐489.






Open access:
Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
Ian Cameron and Cathie Sherrington are chief investigators for the National Health and Medical Research Council Centre of Excellence in the Prevention of Fall‐related Injuries grant (APP1198371).
Each author receives funding from Australian government sources (National Health and Medical Research Council and Medical Research Future Fund). Susan Kurrle receives support from public and private philanthropy sources. Ian Cameron receives research grant and salary funding from New South Wales state government sources (NSW State Insurance Regulatory Authority and Insurance and Care NSW (icare)).