Raised blood pressure or hypertension is by far the leading risk factor for preventable deaths in Australia, contributing to over 25 000 deaths annually (Supporting Information, figure 1 and figure 2),1,2,3 mainly due to stroke, heart disease, kidney disease, heart failure, atrial fibrillation and dementia.3,4
The reduction of blood pressure to less than 140/90 mmHg is only achieved in 32% of people with hypertension in Australia, and control rates have stagnated for a decade (Supporting Information, figure 3).5,6 As our control rates compare poorly to other high income countries (eg, 68% in Canada),5,6,7 we published a call‐to‐action to urgently bring about changes.5 In response to our call‐to‐action, the National Hypertension Taskforce of Australia (Taskforce) was formed, hosted by the Australian Cardiovascular Alliance and Hypertension Australia (Supporting Information), and launched by the Minister for Health and Aged Care in 2022.8,9 The Taskforce partners are reflected in the authorship of the roadmap, and are listed in the Supporting Information, figure 4.
This article describes the key actions to be taken by the Taskforce, including a roadmap to help implement identified actions.
The methods for identifying the key actions and the structure of the Taskforce are described in the Supporting Information, figure 5 and table 1.
Roadmap to improve blood pressure control in Australia
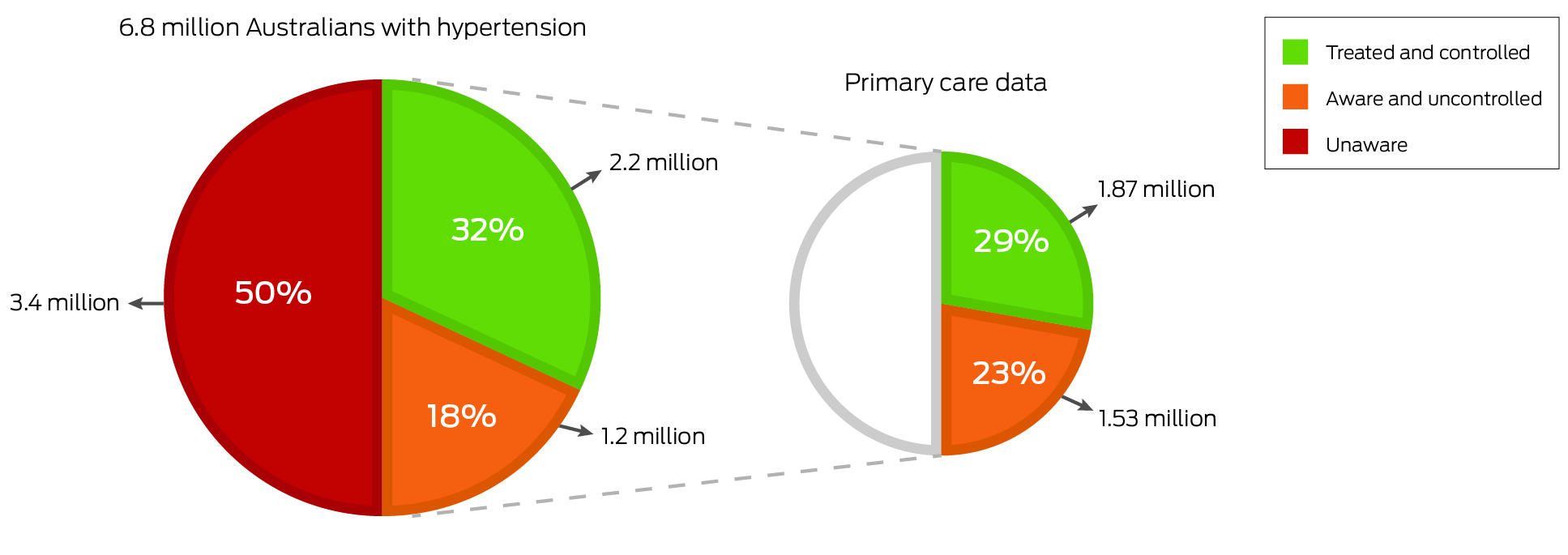
Background. Raised blood pressure is the leading preventable cause of death in Australia. One in three Australian adults (6.8 million people) have hypertension, defined as clinic or office blood pressure greater than or equal to 140/90 mmHg, based on randomised population data.10 Screening campaigns found that about half of these adults (3.4 million) have not had their high blood pressure values detected and are unaware of their hypertension,11 hence are not receiving appropriate treatment. Of those who are diagnosed with hypertension, and treated in the general population, only 32% (2.2 million) are treated effectively, that is, reducing their blood pressure to less than 140/90 mmHg (Box 1).10,11 Australians who visit primary care centres have somewhat different rates, where 55% of patients are treated and have their blood pressure effectively controlled.12
Goal. Increase current population blood pressure control rates (< 140/90 mmHg) from 32% to at least 70% by 2030.5,10
Targets and strategies. The roadmap for 2024–2030 (Box 2) is built on three pillars: (A) prevent; (B) detect; and (C) effectively treat raised blood pressure. An international modelling study recommended 80–80–80 blood pressure targets, which translates to 80% of individuals with hypertension being screened and aware of their diagnosis; 80% of those who are aware being prescribed treatment; and 80% of those on treatment having achieved blood pressure targets.13 However, because 20% remain unaware, and 20% of those aware remain untreated, and 20% of those treated not achieving target, this model would only achieve 51% blood pressure control. To achieve the Taskforce's target of 70%, a 90–90–90 model is required for Australia, as this approach would achieve a 73% blood pressure control rate.
Pillar A: prevent the development of hypertension across the nation
The prevention of blood pressure‐related disease will be achieved through system‐based strategies that promote target blood pressure levels of less than 130/80 mmHg across the nation. Setting a target blood pressure of less than 130/80 mmHg recognises that up to half of blood pressure‐related morbidity occurs at a systolic blood pressure less than 140 mmHg.14 Population‐based strategies that shift the whole distribution of risk factors would produce substantial reductions in cardiovascular disease (CVD) burden,14 and will benefit children, older people, people living in rural and remote areas, culturally and linguistically diverse populations and First Nations peoples, as well as those not accessing primary care services. Such strategies would reduce the risk for people at all blood pressure levels.15
The Taskforce will support initiatives to ensure the full implementation of the National Preventive Health Strategy 2021.16 For the prevention of raised blood pressure, a taskforce working group will develop economic tools to make healthy choices the most affordable ones. We will develop context‐specific strategies to target preventive actions with the greatest attributable risk for hypertension development, such as reducing sodium and increasing potassium intake (eg, using potassium‐enriched salt substitutes), a nutritious food supply, a healthy bodyweight, increasing physical activity and avoiding alcohol intake.17
Box 3 lists the top ten key priority areas for action. In this list, Pillar A was identified as key priority action 9 for the Taskforce. The Taskforce has also identified other key priority actions targeting Pillar A, including actions 2, 6 and 10.
Pillar B: detect raised blood pressure through screening programs
Hypertension is a silent killer, as it is usually asymptomatic and requires population screening for detection. In more than 10 000 Australians screened for hypertension as part of the May Measure Month blood pressure awareness campaign taking place from 2017 to 2019, 52% of participants with high blood pressure were unaware of their hypertension status.11 Similarly, the Stroke Foundation's campaign, Australia's Biggest Blood Pressure Check in 2018, recorded 505 581 health checks and found that 82% of participants with high blood pressure were unaware of it.18 To reach the target of 70% blood pressure control, we need to detect and treat significantly more of the 3.4 million Australians with raised blood pressure who are unaware of it. Although opportunistic screening is important, systematic screening in general practice should be incentivised through government support as this would be the most likely route to successfully detect 90% of people with hypertension.19 To address Pillar B, Taskforce actions may include:
- Implementing a screening protocol for all patients visiting general practices to be tested at least once per year. With 87% of people in Australia seeing a general practitioner once in any given year,20 implementation of primary care incentives for routine blood pressure and heart health checks is likely to achieve most success in the detection, diagnosis and treatment of high blood pressure.19
- Using team‐based care to implement systematic blood pressure screening at primary, secondary and tertiary care visits, including physicians, general practice nurses, pharmacists, obstetricians, anaesthetists, audiologists, optometrists, dentists, physiotherapists, or exercise physiologists – with a clear referral pathway.
- Securing strategic funding to expand screening programs, such as the annual May Measure Month (www.maymeasure.org)11 and Australia's Biggest Blood Pressure Check.18
- Implementing more automated health stations to allow the general public to screen and monitor their blood pressure.
- Raising community awareness and knowledge on the importance of raised blood pressure and its consequences through media campaigns.
- Improving health literacy in the community by encouraging the public to #KnowYourNumbers or #RollUpYourSleeves.
The Taskforce identified several key priority actions targeting Pillar B (Box 3), including actions 2–8 and 10.
Pillar C: diagnose and treat hypertension effectively to ensure it is controlled
When raised blood pressure is detected, it is crucial that a diagnosis is made, and blood pressure is treated effectively.
Value‐based care
With about 37 000 general practitioners across Australia,20 and with hypertension being the most common condition managed,21 it is crucial that processes in primary care are optimised to improve health outcomes. In primary care, only 55% of people with hypertension have their blood pressure controlled to the conservative target of 140/90 mmHg.12 The Australian Government's 10‐year primary care reform plan has a strong focus on consumer‐centred primary care,22 and improving team‐based care. The implementation of MyMedicare in 2023 is a step in the right direction as it incentivises continuity of care (beneficial to achieving blood pressure targets).23 Current fee‐for‐service models (paying for each time a service is delivered) work against team‐based care. The fee‐for‐service models lead to financial drivers to maintain the number of services by that professional. A shift towards value‐based care (paying for delivering care that improves patient health outcomes) would ensure optimal use of funding across multiple providers to achieve better health outcomes. These notions were echoed by the 2022 Strengthening Medicare taskforce report.24
Blood pressure targets
International guidelines recommend a blood pressure target for most patients of less than 130/80 mmHg,25,26 emphasising that it is insufficient to lower blood pressure to less than 140/90 mmHg. A target of less than 130/80 mmHg will account for factors frequently associated with poor blood pressure control, including individual patient blood pressure fluctuations and general practitioner visit‐to‐visit fluctuations.27
Older age
Age is the greatest driver of risk.28 Effective treatment of older patients is thus essential. Two major trials in patients (average age of 6829 and 84 years30) demonstrated clear benefit from reducing blood pressure, including reduced mortality, and safety.29,30 Also, orthostatic hypotension should not be a deterrent to more intensive blood pressure lowering therapy — those receiving intensive therapy had reduced risk of cardiovascular and all‐cause deaths regardless of orthostatic hypotension.31 Education is required to overcome the perception of adverse risks of treatment.
An important reason for the low blood pressure control rates is missing a diagnosis of secondary hypertension (eg, primary aldosteronism).15 Specific recommendations for identifying secondary causes should be integrated into routine clinical practice.
Tailoring the HEARTS package for Australia
To optimise hypertension management, the Taskforce adopts the World Health Organization successful32 HEARTS technical package for cardiovascular disease management in primary health care,33 tailored to the Australian setting:
H – Healthy lifestyle counselling
Lifestyle modification is the first‐line treatment for hypertension and has crosscutting benefits such as reducing the risk for cancer and diabetes. Lifestyle coaching modules delivered at the time of diagnosis should ideally be made by the general practice team, including nurses, exercise physiologists, physiotherapists, dieticians, and community pharmacy. Messages should be reinforced with an in‐person follow‐up, eHealth, mHealth or telehealth. Most people diagnosed with hypertension will persist with uncontrolled blood pressure despite lifestyle changes and thus should be given medication while simultaneously making lifestyle changes.
E – Evidence‐based treatment protocols
Low control rates (55%) in Australian primary care12 are largely due to treatment inertia — the hesitancy to start or intensify treatment after elevated blood pressure readings. A 1‐page simplified treatment protocol on targeting a blood pressure less than 130/80 mmHg is regarded as one of the most successful components of HEARTS,32 likely because it helps overcome inertia.34 The protocol will be developed in collaboration with general practitioners, professional colleges and societies to ensure feasibility for adoption. This protocol should include lifestyle coaching plus a linear, stepwise algorithm describing progressively more intensive medication treatment until blood pressure is controlled. The protocol should provide evidence‐based medicines and doses,32 ideally single‐pill combinations (SPC) of two or more drugs as initial therapy. For most patients, successful treatment requires two or more medications.26 SPCs can be cost‐neutral or result in a cost saving35 and benefits include improved medication adherence;36 improved blood pressure control over a shorter period of time,37 with no increase in side effects.37 SPCs also lessen treatment inertia and the impact of infrequent following up of patients after prescribing.
Current practice in Australia is to start treatment with monotherapy, where the dose is often increased at follow‐up visits.35,38 It is safer and more effective to add another blood pressure lowering drug than to double the dose,39 which is another benefit for SPCs as first‐line treatment. However, at present, policy changes are required to allow prescription of SPCs as first‐line treatment in Australia, as SPCs are not subsidised by the Pharmaceutical Benefits Scheme for initial treatment.35
The Taskforce has identified the development of a 1‐page simplified protocol as key priority action 1 targeting Pillar C (Box 3).
A – Access to essential medicines and technology
Medicines. Treating hypertension in primary care cost Australia about $1.2 billion in 2022, with 51% of that pharmacy‐related, 29% general practitioner‐related, and 20% medicine costs.40 With 58% of the cost from federal sources, and 42% from patient out‐of‐pocket payments, these expenses highlight a major equity issue.40 About 37 monotherapy regimens and 57 SPCs (including strength variations) are available in Australia35 and supported by the Pharmaceutical Benefits Scheme. Although prescriptions require a patient co‐payment, in 2023 this cost was set to a maximum of $30 or $7.30 for those with a concession card. Also, several dual and triple SPCs are included in the 2023 update of medicines listed on the Pharmaceutical Benefits Scheme allowing increased dispensing from 30 to 60 days. Longer dispensing durations are likely to improve access, adherence and blood pressure control.7 Availability of different generic SPCs (with different strength variations) would ease effective prescribing.
Blood pressure measurement devices. Clinically validated upper‐arm cuff‐based automated devices should be used for blood pressure measurement in the clinic, and for 24‐hour ambulatory or home blood pressure monitoring. These automated devices eliminate human error associated with manual devices (eg, digit preference, hearing impairment) and require less training.41 Lack of clinical validation is an underappreciated problem. Four out of five automated devices sold online (www.amazon.com) are not validated, meaning they have not been properly tested for accuracy.42 Approval by the Australian Therapeutic Goods Administration, United States Food and Drug Administration or the European Commission's equivalent CE Mark may not reflect adequate accuracy testing. Online resources, such as STRIDE BP (www.stridebp.org), provide lists of devices that are adequately validated. By following the 2023 International consensus on standardized clinic blood pressure measurement,41 accurate diagnosis is much more likely.
High quality clinic measurement can be achieved by automated office blood pressure measurement.38,41 This involves using an automated device that records and averages multiple readings, with or without the presence of a health professional. To confirm diagnosis, 24‐hour ambulatory and home blood pressure monitoring are recommended.25 The gold standard method is 24‐hour ambulatory blood pressure, and there is now a Medicare rebate available (Medicare Benefits Schedule item 11607). For ongoing monitoring, automated office blood pressure or self/home blood pressure monitoring is recommended. More resources supporting doctors and patients in undertaking accurate blood pressure monitoring are needed, and will be developed by the Taskforce.
Many cuffless wearable blood pressure devices are becoming widely available, but they are not recommended until accuracy and utility in clinical practice have been confirmed.43
To address access to quality medicines and devices, the Taskforce has identified key priority actions 1 and 8 targeting Pillars B and C (Box 3).
R – Risk‐based CVD management
Targeting patients at the highest risk of developing CVD is a proven strategy to improve health outcomes. Higher CVD risk is conferred by factors such as age, sex, smoking status, blood pressure, cholesterol, pre‐existing disease such as diabetes or chronic kidney disease, and postcode. The updated 2023 Australian CVD risk guidelines28 include these components and recommend screening people without known CVD aged 45–79 years (or in people with diabetes aged 35–79 years, and First Nations people aged 30–79 years) using an online calculator (www.cvdcheck.org.au/calculator). Once an estimated intermediate risk of 5–10%, or high risk of more than or equal to 10% of having a cardiovascular event within the next five years is detected, guidelines recommend consideration of pharmacotherapy in the former and combined statin and blood pressure lowering therapy in the latter, regardless of blood pressure and cholesterol level, unless contraindicated. Health professionals are referred to national guidelines to guide treatment.28 The national guidelines on the diagnosis and management of hypertension in adults38 was published in 2016 and requires an update. The Taskforce recommends the use of the 1‐page simplified hypertension protocol to be developed as part of key priority action 1. The Taskforce supports the 2023 CVD risk guidelines recommendation to initiate immediate hypertension treatment based on a blood pressure of more than 160/100 mmHg regardless of the CVD risk result. To improve blood pressure control in Australia, the Taskforce aligns with the statement that “reducing blood pressure reduces CVD risk, in a wide range of age groups, irrespective of baseline blood pressure. However, the higher the initial CVD risk, the greater the benefit”.28 Thus, blood pressure lowering therapy for high risk individuals with an untreated systolic blood pressure of 140–130 mmHg is warranted.
T – Team‐based, patient‐centred care
Team‐based care coordinates care among general practitioners, pharmacists, nurses and others, and requires sharing of clinical and laboratory data, and medications.44 This increased capacity allows for improved patient follow‐up, medication management and adherence support.44 Multidisciplinary teams linking general practitioners, pharmacists and nurses can significantly improve blood pressure control, and have formed the cornerstone of international successes in various settings in the United States and Canada,44 with positive signs also in nurse‐coordinated hypertension care in Australia.45,46 The 2022 Strengthening Medicare taskforce report24 states that general practitioners are “struggling to meet increasingly complex demand”, encouraging team‐based care. The government's intent to strengthen team‐based care as an outcome of the Scope of Practice Review,47 would ensure health professionals are used to their full potential.48 The Taskforce recommends the evaluation of different team‐based care models and implementing those with proven effectiveness — with a particular focus on value‐based care.
To implement team‐based care, the Taskforce has identified key priority action 7 targeting Pillars B and C (Box 3).
Person‐centred strategies are also effective in improving blood pressure control. The National Medicines Policy49 (2022) reiterates the importance of team‐based and person‐centred care, with a clear focus to enhance consumer involvement, empowerment and shared decision making. The Taskforce aims to establish a large‐scale group of people with lived experience to collaborate on actions related to the pillars of prevention, detection and treatment.
To increase patient activation and engagement, the Taskforce has identified key priority action 2 targeting Pillars A, B and C (Box 3).
S – Systems for monitoring
An effective hypertension control program requires the monitoring of blood pressure control at the patient, primary care and health system level.32 In Australia, there are two challenges with this level of monitoring: (i) availability of large‐scale data from the general population (similar to what is available in the United States) — the Taskforce relies on data captured from the Australian Bureau of Statistics National Health Surveys;8 and (ii) systems of data capture and availability of national primary care data are not designed for systematic national monitoring, comparison between practices, or between primary health networks. Complexities include the numerous clinical software packages used by general practitioner clinics (eg, Best Practice, Medical Director), different clinical audit tools (eg, CAT4, POLAR GP), and different health informatic vendors used by primary health networks (PEN CS, POLAR, Primary Sense). For now, the Taskforce cannot track national blood pressure data, or track related medication use through the Pharmaceutical Benefits Scheme, Medicare Benefits Schedule services, disease development, hospitalisation, and health outcomes over time.
Previously MedicineInsight provided access to quality general practitioner data, but its management was transferred to the Australian commission on safety and quality in health care and we look forward to data becoming available again.12 Up‐to‐date high quality data across at least a selection of general practitioner clinics are essential, including a harmonised care pathway. Pathways to incentivise better monitoring may be to include blood pressure control (%) as a quality improvement measure as part of the Practice Incentives Program. There are attempts to achieve harmonisation of data through the primary health network Quality Improvement Program, and the New South Wales Lumos Program, but efforts are not streamlined, national or regularly updated. A national coordinated effort, involving government leadership, is essential.
In Australia, the Department of Health and Aged Care supports health care providers through other platforms, such as the Australian Immunisation Register. Similar to the need to manage raised blood pressure,2 the National Cancer Screening Register includes a single, integrated digital platform, facilitating electronic data capture, and supports the participation in cancer screening.50 Other approaches involving eHealth and mHealth to improve and track blood pressure management show increasing promise and will be evaluated for implementation.
To establish a systems and data‐based approach to blood pressure management, the Taskforce has identified key priority action 4, targeting Pillars B and C (Box 3).
The Taskforce is cognisant of the substantial barriers in implementing the roadmap at the community, patient, provider and system level. For each aspect of implementation, we will encourage and expand ongoing research, and liaise widely to design and implement actions that are feasible, acceptable, cost‐effective, scalable and tailored for the Australian setting.
Final perspectives
With timely implementation of the actions in this roadmap, we will be able to achieve a 70% blood pressure control rate in Australian adults by 2030, thereby achieving the best control rate in the world. To achieve this, the Taskforce requires active engagement with all stakeholders — particularly the government.
The health care changes we propose refer to effective use of preventive services. This is well established in preventing cancer in Australia, but much greater gains are possible through cardiovascular preventive services. Compared with colonoscopy, mammography and flu vaccinations, modelling in the United States51 indicates that the treatment of hypertension would prevent the greatest number of deaths (Box 4). These services will prevent large numbers of deaths due to high blood pressure being very common (one in three adults), and affordable treatment being highly effective in reducing deaths.51 If the prevalence of hypertension was reduced by 25% and if everyone with hypertension in Australia was effectively treated and controlled, this would result in savings of $91.6 billion in gross domestic product (taking into account productivity losses due to hypertension and its sequalae over the working lifetime).52
This roadmap paves the way for success. We have all the tools to achieve our goal. With strong drive, commitment and collaboration, Australia is poised to become the global exemplar of blood pressure control.
Box 1 – Awareness, treatment and control rates of the general population (Australian Institute of Health and Welfare10 and May Measure Month11 data); and control rates in primary care (55% according to MedicineInsights data12)
Box 3 – The top 10 key priority areas for action*
|
|
Actions |
Pillar† |
|||||||||||||
|
|
|||||||||||||||
|
1 |
Developing up‐to‐date, simple blood pressure management tools for health care providers |
C |
|||||||||||||
|
2 |
Increasing patient activation and engagement |
A, B, C |
|||||||||||||
|
3 |
Raising and maintaining awareness at all levels |
B |
|||||||||||||
|
4 |
Establishing a systems‐ and data‐based approach to blood pressure management |
B, C |
|||||||||||||
|
5 |
Detection (screening) of people with elevated blood pressure to identify those at risk |
B |
|||||||||||||
|
6 |
Health economic analyses to inform discussions with the federal government as well as state and territory government officials |
A, B, C |
|||||||||||||
|
7 |
Explore and drive implementation of multidisciplinary team‐based care approaches to manage hypertension |
B, C |
|||||||||||||
|
8 |
Ensuring standardised accurate blood pressure measurement |
B, C |
|||||||||||||
|
9 |
Implement population‐based actions to reduce blood pressure across Australia |
A |
|||||||||||||
|
10 |
Regularly re‐evaluate and update the current roadmap via engagement with all relevant stakeholders, and consolidate and guide actions of the Hypertension Taskforce |
A, B, C |
|||||||||||||
|
|
|||||||||||||||
|
* Across all activities, ensure co‐design with stakeholders, equity across people living in rural and remote areas, and equity in engaging with First Nations people and culturally and linguistically diverse populations. † Pillars: A, prevent; B, detect; C, treat. |
|||||||||||||||
Box 4 – Modelling in the USA: cause‐specific model estimating the number of additional deaths prevented in those aged less than 80 years, per year, by increasing the use of selected clinical preventive services51
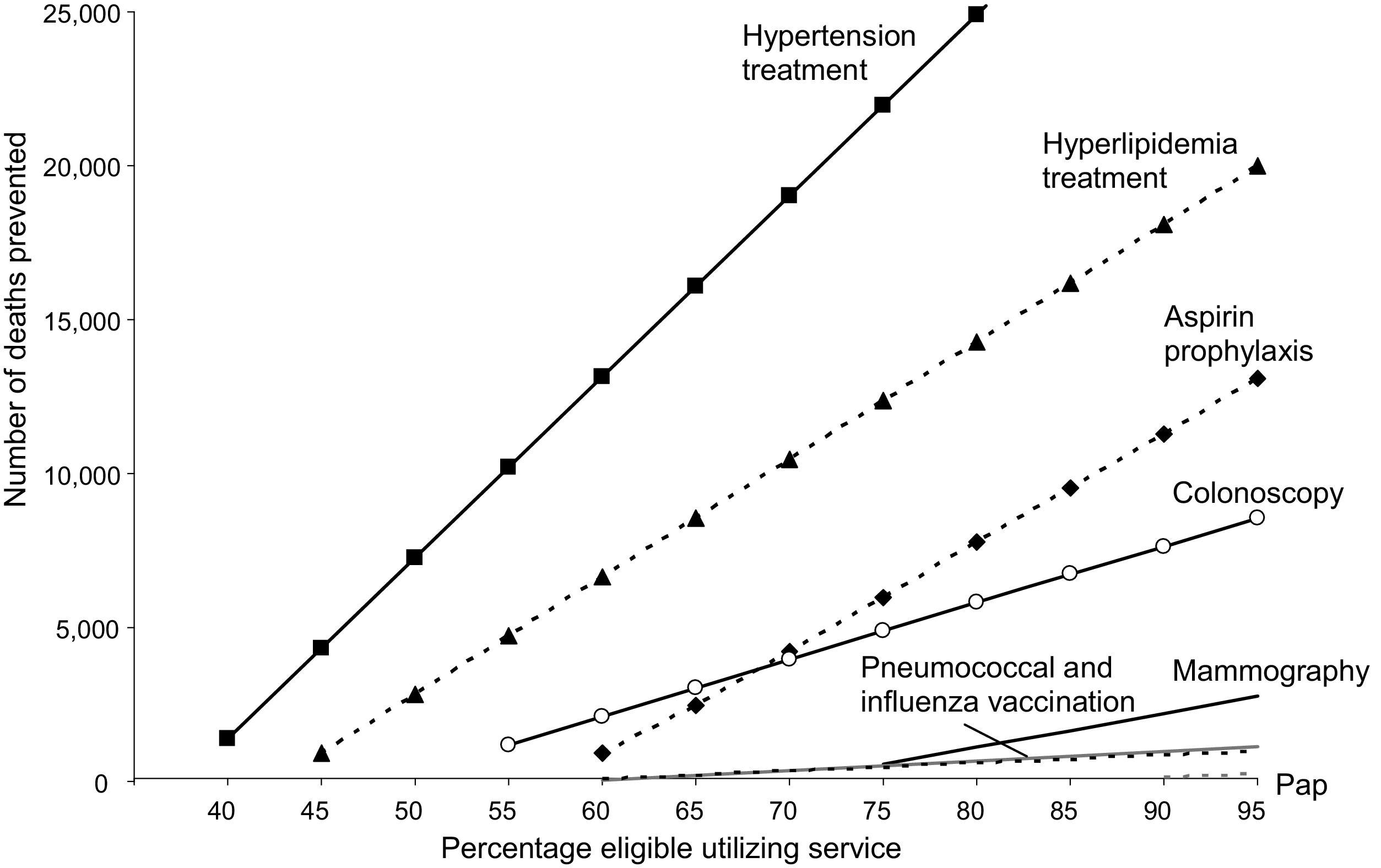
The all‐cause model predicted much greater numbers of deaths prevented, where every 10% increase in hypertension treatment would lead to an additional 14 000 deaths prevented per year. Figure reproduced with permission.
Provenance: Not commissioned; externally peer reviewed.
- 1. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990‐2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396: 1223‐1249.
- 2. Institute of Health Metrics and Evaluation. Global burden of disease. Deaths by risk factor in Australia. IHME, 2019. https://ourworldindata.org/grapher/number‐of‐deaths‐by‐risk‐factor?country=~AUS (viewed Apr 2024).
- 3. Xu X, Islam SMS, Schlaich M, Jennings G, Schutte AE. The contribution of raised blood pressure to all‐cause and cardiovascular deaths and disability – adjusted life‐years (DALYs) in Australia: analysis of global burden of disease study from 1990 to 2019. PLoS One 2024; 19: e0297229.
- 4. Institute of Health Metrics and Evaluation. Disability adjusted life years attributable to raised systolic blood pressure, Australia. 2019. https://vizhub.healthdata.org/gbd‐results/ (viewed June 2024).
- 5. Schutte AE, Webster R, Jennings G, Schlaich MP. Uncontrolled blood pressure in Australia: a call to action. Med J Aust 2022; 216: 61‐63. https://www.mja.com.au/journal/2022/216/2/uncontrolled‐blood‐pressure‐australia‐call‐action
- 6. NCD Risk Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population‐representative studies with 104 million participants. Lancet 2021; 398: 957‐980.
- 7. World Health Organization. Global report on hypertension: the race against a silent killer. 2023. ISBN 978‐92‐4‐008106‐2. https://www.who.int/publications/i/item/9789240081062 (viewed Apr 2024).
- 8. Australian Cardiovascular Alliance. The National Hypertension Taskforce is launched by the Honourable Mark Butler MP, Minister for Health and Aged Care [media release]. 8 Dec 2023. ozheart.org/taskforce‐launched‐by‐minister/.
- 9. National Hypertension Taskforce of Australia [website]. https://www.hypertensiontaskforce.au (viewed July 2024).
- 10. Australian Institute of Health and Welfare. High blood pressure [website]. Canberra: AIHW, 2019. https://www.aihw.gov.au/reports/risk‐factors/high‐blood‐pressure/contents/summary (viewed June 2024).
- 11. Carnagarin R, Nolde JM, Yang J, et al. Stagnating rates of blood pressure control in Australia: insights from opportunistic screening of 10046 participants of the May Measurement Month campaigns. J Hypertens 2023; 41: 632‐637.
- 12. Roseleur J, Gonzalez‐Chica DA, Bernardo CO, et al. Blood pressure control in Australian general practice: analysis using general practice records of 1.2 million patients from the MedicineInsight database. J Hypertens 2021; 39: 1134‐1142.
- 13. Pickersgill SJ, Msemburi WT, Cobb L, et al. Modeling global 80‐80‐80 blood pressure targets and cardiovascular outcomes. Nat Med 2022; 28: 1693‐1699.
- 14. Rodgers A, Ezzati M, Vander HS, et al. Distribution of major health risks: findings from the Global Burden of Disease study. PLoS Med 2004; 1: e27.
- 15. Olsen MH, Angell SY, Asma S, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet 2016; 388: 2665‐2712.
- 16. Australian Government Department of Health. National preventive health strategy 2021–2030. Canberra: Commonwealth of Australia, 2021. https://www.health.gov.au/sites/default/files/documents/2021/12/national‐preventive‐health‐strategy‐2021‐2030_1.pdf (viewed Apr 2024).
- 17. Charchar FJ, Prestes PR, Mills C, et al. Lifestyle management of hypertension: International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. J Hypertens 2024; 42: 23‐49.
- 18. Stroke Foundation. Australia under pressure. Australia's biggest blood pressure check report. 2018. https://strokefoundation.org.au/media/cerfkt0t/abbpc2018_australia_under_pressure_report.pdf (viewed Oct 2023).
- 19. Si S, Moss JR, Sullivan TR, et al. Effectiveness of general practice‐based health checks: a systematic review and meta‐analysis. Br J Gen Pract 2014; 64: e47‐53.
- 20. Gordon J, Britt H, Miller GC, et al. General practice statistics in Australia: pushing a round peg into a square hole. Int J Environ Res Public Health 2022; 19: 1912.
- 21. NPS MedicineWise. General practice insights report July 2018 ‐ June 2019. Sydney: NPS MedicineWise, 2020.
- 22. Australian Government Department of Health and Aged Care. Australia's primary health care 10 year plan 2022–2032. 2022. https://www.health.gov.au/resources/publications/australias‐primary‐health‐care‐10‐year‐plan‐2022‐2032 (viewed June 2024).
- 23. Khanam MA, Kitsos A, Stankovich J, et al. Association of continuity of care with blood pressure control in patients with chronic kidney disease and hypertension. Aust J Gen Pract 2019; 48: 300‐306.
- 24. Australian Government Department of Health and Aged Care. Strengthening Medicare Taskforce Report 2022 https://www.health.gov.au/sites/default/files/2023‐02/strengthening‐medicare‐taskforce‐report_0.pdf (viewed June 2024).
- 25. Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020; 75: 1334‐1357.
- 26. Mancia G, Kreutz R, Brunström M, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens 2023; 41: 1874‐2071.
- 27. Schutte AE, Kollias A, Stergiou GS. Blood pressure and its variability: classic and novel measurement techniques. Nat Rev Cardiol 2022; 19: 643‐654.
- 28. National Heart Foundation of Australia. Australian Guideline for assessing and managing cardiovascular disease risk [website]. 2023. https://www.cvdcheck.org.au/overview (viewed Apr 2024).
- 29. Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med 2015; 373: 2103‐2116.
- 30. Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008; 358: 1887‐1898.
- 31. Juraschek SP, Hu JR, Cluett JL, et al. Orthostatic hypotension, hypertension treatment, and cardiovascular disease: an individual participant meta‐analysis. JAMA 2023; 330: 1459‐1471.
- 32. Moran AE, Gupta R, Global Hearts Initiative Collaborators. Implementation of Global Hearts Hypertension Control Programs in 32 low‐ and middle‐income countries: JACC International. J Am Coll Cardiol 2023; 82: 1868‐1884.
- 33. World Health Organization. HEARTS Technical Package (WHO Ref. No. WHO/NMH/NVI/19.8). 2021. https://www.who.int/publications/i/item/WHO‐NMH‐NVI‐19‐8 (viewed Apr 2024).
- 34. Jaffe MG, Lee GA, Young JD, et al. Improved blood pressure control associated with a large‐scale hypertension program. JAMA 2013; 310: 699‐705.
- 35. Nguyen LH, Bruyn E, Webster R, et al. Are we there yet? Exploring the use of single‐pill combination therapy in the management of raised blood pressure in Australia. Heart Lung Circ 2022; 31: 954‐963.
- 36. Parati G, Kjeldsen S, Coca A, et al. Adherence to single‐pill versus free‐equivalent combination therapy in hypertension: a systematic review and meta‐analysis. Hypertension 2021; 77: 692‐705.
- 37. Salam A, Kanukula R, Atkins E, et al. Efficacy and safety of dual combination therapy of blood pressure‐lowering drugs as initial treatment for hypertension: a systematic review and meta‐analysis of randomized controlled trials. J Hypertens 2019; 37: 1768‐1774.
- 38. National Heart Foundation of Australia. Guideline for the diagnosis and management of hypertension in adults. 2016. Melbourne: National Heart Foundation of Australia. https://www.heartfoundation.org.au/getmedia/c83511ab‐835a‐4fcf‐96f5‐88d770582ddc/PRO‐167_Hypertension‐guideline‐2016_WEB.pdf (viewed Apr 2024).
- 39. Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ 2003; 326: 1427.
- 40. Atkins E, Nguyen LH, Chatterton ML, et al. The costs of treating hypertension in Australia. Med J Aust 2024; in press.
- 41. Cheung AK, Whelton PK, Muntner P, et al. International consensus on standardized clinic blood pressure measurement ‐ a call to action. Am J Med 2023; 136: 438‐445.
- 42. Picone DS, Chapman N, Schultz MG, et al. Availability, cost, and consumer ratings of popular nonvalidated vs validated blood pressure‐measuring devices sold online in 10 countries. JAMA 2023; 329: 1514‐1516.
- 43. Stergiou GS, Mukkamala R, Avolio A, et al. Cuffless blood pressure measuring devices: review and statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens 2022; 40: 1449‐1460.
- 44. Carter BL, Bosworth HB, Green BB. The hypertension team: the role of the pharmacist, nurse, and teamwork in hypertension therapy. J Clin Hypertens (Greenwich) 2012; 14: 51‐65.
- 45. Stephen C, Halcomb E, Fernandez R, et al. Nurse‐led interventions to manage hypertension in general practice: a systematic review and meta‐analysis. J Adv Nurs 2022; 78: 1281‐1293.
- 46. Carrington MJ, Jennings GL, Harris M, et al. Impact of nurse‐mediated management on achieving blood pressure goal levels in primary care: insights from the Valsartan Intensified Primary carE Reduction of Blood Pressure Study. Eur J Cardiovasc Nurs 2016; 15: 409‐416.
- 47. Australian Government Department of Health and Aged Care. Unleashing the potential of our health workforce ‐ scope of practice review [website]. 2024. https://www.health.gov.au/our‐work/scope‐of‐practice‐review (viewed June 2024).
- 48. Australian Primary Heatlh Care Nurses Association. Nurse skills, experience being wasted despite nursing shortage ‐ national survey [media release]. 13 June 2023. https://www.apna.asn.au/about/media/archive‐media‐releases/nurse‐skills‐‐experience‐being‐wasted‐despite‐nursing‐shortage‐‐‐national‐survey (viewed June 2024).
- 49. Australian Government Department of Health and Aged Care. National medicines policy 2022. 2nd edition. https://www.health.gov.au/sites/default/files/2022‐12/national‐medicines‐policy.pdf (viewed Apr 2024).
- 50. Gertig D, Lee J. Supporting health care providers in cancer screening: the role of the National Cancer Screening Register. Med J Aust 2023; 219: 94‐98. https://www.mja.com.au/journal/2023/219/3/supporting‐health‐care‐providers‐cancer‐screening‐role‐national‐cancer‐screening
- 51. Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the US by improvements in use of clinical preventive services. Am J Prev Med 2010; 38: 600‐609.
- 52. Hird TR, Zomer E, Owen AJ, et al. Productivity burden of hypertension in Australia. Hypertension 2019; 73: 777‐784.







Open access:
Open access publishing facilitated by University of New South Wales, as part of the Wiley ‐ University of New South Wales agreement via the Council of Australian University Librarians.
Aletta Schutte is supported by a National Health and Medical Research Council (NHMRC) investigator grant (APP2017504). Jun Yang is supported by an NHMRC investigator grant (APP1994576). Clara Chow is supported by an NHMRC investigator grant (APP1195326). The National Hypertension Taskforce would like to thank all members of the International Advisory Panel (Sheldon Tobe, Norm Campbell, Mike Rakotz, Janet Wright, Paul Muntner, Andrew Moran and Pedro Ordunez) for their time and helpful guidance. We acknowledge the input and collaboration of many Australians volunteering to join working groups, workshops and other meetings to inform our decisions. We express sincere gratitude towards the Australian Cardiovascular Alliance for excellent and continued strategic and administrative support.
Aletta Schutte is past president of the International Society of Hypertension, secretary of the Australian Cardiovascular Alliance, board member of Hypertension Australia. Garry Jennings is the chief medical advisor of the Heart Foundation of Australia and board member of Hypertension Australia. Markus Schlaich is the chair of Hypertension Australia, and treasurer of the World Hypertension League. Sharon James is a board director of the Australian Primary Health Care Nurses Association. Mark Nelson is deputy‐chair of the Research Advisory Committee, Stroke Foundation, co‐chair of the Expert Advisory Committee CVD Guidelines, member of the Board of Hypertension Australia. Lisa Murphy is chief executive officer of the Stroke Foundation, member of the Advisory Group for the CVD Risk Guidelines. James Sharman is a board member of Hypertension Australia. Taskeen Khan works at the World Health Organization, but the views do not represent the views of the organisation. Jun Yang is a member of the Endocrine Society Primary Aldosteronism Guideline Development Panel and lead of the Primary Aldosteronism Foundation Patient Engagement Committee. Breonny Robson is general manager, Clinical & Research at Kidney Health Australia, and member of the Advisory Group for the CVD Risk Guidelines. Aletta Schutte, Markus Schlaich, James Sharman, Garry Jennings, Mark Nelson, Lisa Murphy, Andrew Goodman are members of the National Hypertension Taskforce Steering Committee. Aletta Schutte has received speaker fees from Omron, Medtronic, Aktiia, Servier, Sanofi, Novartis and is advisory board member for Skylabs and Abbott. Mark Nelson has received speaker fees from Medtronic. Stephen Nicholls has received research support from AstraZeneca, Amgen, Anthera, CSL Behring, Cerenis, Eli Lilly, Esperion, Resverlogix, New Amsterdam Pharma, Novartis, InfraReDx and Sanofi‐Regeneron and is a consultant for Amgen, Akcea, AstraZeneca, Boehringer Ingelheim, CSL Behring, Eli Lilly, Esperion, Kowa, Merck, Takeda, Pfizer, Sanofi‐Regeneron, Vaxxinity, CSL Sequiris and Novo Nordisk. Geoffrey Cloud received speaker fees from Astra Zeneca and serves on their Advisory Board. Markus Schlaich has received research support from Medtronic, ReCor (Otsuka), Boehringer‐Ingelheim, Abbott, Idorsia, Janssen, and serves on scientific advisory boards for Medtronic, Abbott, Novartis and Astra Zeneca.