The known: Although anterior cruciate ligament (ACL) injuries are burdensome and expensive for athletes and society, few studies of their economic impact have been published.
The new: A national ACL injury prevention exercise program for amateur soccer players could save $1 501 136 each year in medical and societal costs by averting 125 ACL ruptures, four ACL re‐ruptures, 22 cases of knee osteoarthritis, and three total knee replacements.
The implications: Our findings provide health policymakers and football organisations information that could assist decision making regarding investing in primary ACL injury prevention.
Anterior cruciate ligament (ACL) ruptures are among the most devastating injuries for football players at any playing level, and are associated with high costs for health systems, insurance companies, and sporting organisations. A study in 2023 estimated that the annual cost of ACL reconstructions for amateur soccer players in Australia was $69 623 211.1 In New Zealand, annual cruciate ligament injury‐associated insurance costs increased by 127% during 2007–2020.2
The immediate effects of ACL injuries include reduced quality of life and productivity losses, but their effects extend beyond the immediate rehabilitation period. A systematic review of the longer term effects of ACL injuries found that some people reported prolonged work absences and modified activities of daily living two or more years after their injury.3 ACL injury is also associated with increased risk of developing knee osteoarthritis.4,5,6 Longer term follow‐up studies of people with ACL injuries have reported knee osteoarthritis rates of 44% (11‐year follow‐up5) to 48% (32–37‐year follow‐up4). As knee osteoarthritis is difficult to treat (knee replacements are effective, but only as a last resort) and primary preventive exercise programs can reduce the risk of ACL injuries,7 a population‐level public health response is required.
It is important to consider up‐to‐date cost‐effectiveness estimates and predict the return on investment of efficacious primary preventive exercise programs when seeking funding for a national strategy.8 Only limited population‐level modelling information is currently available for Australia. One economic modelling study found that a national ACL injury prevention program for 12–25‐year‐old participants in all high risk sports would be the most effective strategy.9 However, further modelling is required. First, it is important to project cost savings for specific sports; the infrastructure modifications and partnerships with national and state‐based organisations required by a national strategy10,11 mean that a multi‐sport strategy is less likely to be adopted. Second, it is imperative that modelling studies use pragmatic effectiveness rates to realistically project cost savings and return on investments.12 The complexity of broadly implementing interventions means that their efficacy is lower than that achieved in controlled trials; for example, it was suggested that the real world effectiveness of the Swedish Knee Control Program was likely to be 12% rather than the 64% achieved in a trial.12
The aim of our study was to estimate the long term (over 35 years) cost savings and return on investment and gain in quality‐adjusted life years (QALYs) that could be achieved by a national ACL injury prevention program for football (soccer) players in Australia, by age group and sex.
Methods
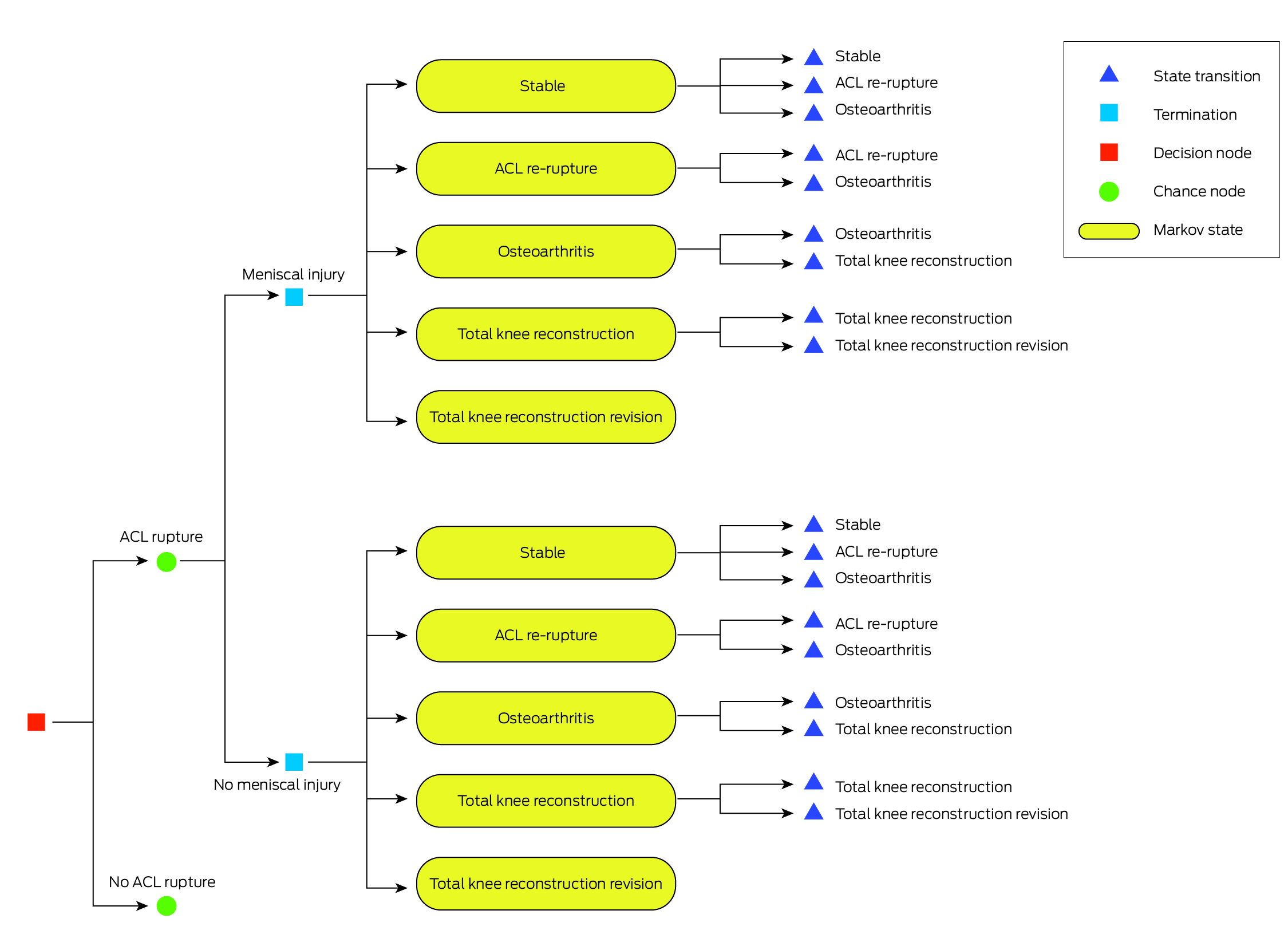
We conducted a Markov decision analysis, in Excel for Mac 2011 (Microsoft), of the costs and benefits of a national ACL injury prevention program for football (soccer) players in Australia. Markov models are often used in public health research to evaluate events with ongoing risks, which have consequences, and which occur more than once, such as ACL ruptures.13 Taking a societal perspective, we used a 35‐year Markov model with yearly cycles discounted by 5%. Footballers either remain in one health state or transition to another health state (eg, ACL rupture to ACL re‐rupture to osteoarthritis to total knee replacement to total knee replacement revision), with different probabilities and costs applied according to whether the ACL rupture was accompanied by meniscal injury (Box 1). Separate models were used for different age groups (10–17, 18–34, 35 years or older) and gender. Our Markov model design was based on that of an earlier British study.9 We report our analysis according to the consolidated health economic evaluation reporting standards (CHEERS) checklist.14
Study population
We analysed the cost implications of a national ACL injury prevention program for amateur football players in Australia. The population number (340 253 players in the three age groups, including 258 592 male and 81 661 female players) was derived from the Football Australia 2022 participation report15 and a study of ACL characteristics in amateur football players.16 The model included only organised outdoor football; indoor football, community events, and school football were not included. The three major player categories are juniors (7–17 years), seniors (18–34 years), and veterans (35 years or older). For juniors, our 35‐year model started at age 10 years, seniors at age 18 years, and veterans at age 35 years; for example, if a 10‐year‐old player has a ruptured ACL, the model cycles until the player is 45 years old, for an 18‐year old until they are 53 years old, and for a 35‐year‐old until they are 70 years old.
The national ACL injury prevention program
The program we assessed, the Perform+ program,17 combines running, plyometric, and strength exercises in a 20‐minute warm‐up. Although Perform+ is based on the Fédération Internationale de Football (FIFA) 11+ program,18 it includes updated content and adjustments that overcome barriers to its use.17 The program would be included in the football coaching curriculum for all players in Australia (including skills training for current coaches) using implementation guidance.19 The estimated protective effect of the program is based on the finding of a 2018 meta‐analysis (male footballers: 50% lower risk of any ACL injury; female footballers: 50% lower risk for contact and 64% lower risk for non‐contact ACL injury).7 The RE‐AIM framework20 was used to estimate a pragmatic effectiveness rate, calculated by multiplying the efficacy reported by the authors of a meta‐analysis7 by estimates for reach, adoption (by players), implementation (by organisations), and maintenance (male players: 50% × 66% × 64% × 38% × 100% = 8%; female players: 58% × 66% × 64% × 38% × 100% = 9%) (Box 2). The RE‐AIM estimates are based on outcomes for the national Knee Control+ program in Sweden,23 the FIFA 11+ program in Switzerland,10 and an Australian cross‐sectional survey on injury prevention exercise in amateur football players.24
The logistic costs of the program were estimated in consultation with the New Zealand Accident Compensation Corporation (ACC).25 A national football injury prevention program (FIFA 11+) was introduced in New Zealand in 1999, and the ACC has tracked its implementation costs. The total costs were adjusted for cumulative inflation (1999–2021), the relative purchasing power of the New Zealand and Australian dollars in 2021,26 and population size differences, and projected for the full Markov model (further details: Supporting Information, section 1).
Return on investment from the program was calculated by dividing the savings achieved by the program by program implementation costs.
Costs
We have published elsewhere the costs associated with ACL reconstructions for amateur football players in Australia.1 In brief, the cost of ACL reconstructions includes surgical costs, direct and indirect costs (wage and tuition costs), knee magnetic resonance imaging costs, the costs of presenteeism, and unpaid work costs. Knee osteoarthritis costs include costs for medications, physiotherapy, specialist visits, corticosteroid injections, general practitioner visits, knee x‐rays, other direct non‐medical expenses, and indirect costs. Total knee replacement and total knee replacement revision costs include surgical and rehabilitation costs. Annual costs (Box 3) were inflated to 2021 prices using the total health price index28 and converted to Australian dollars, when necessary, using purchasing power parity values26 (further details: Supporting Information, section 2).
Transition probability estimates
The reported ACL reconstruction rate among Australian football players during 2003–0829 was updated with more recent information30 to generate a proxy ACL injury age table (Supporting Information, section 3). The risks of knee osteoarthritis, total knee replacement, and total knee replacement revision were based on the outcomes of a modelling study6 and outcomes reported by people 32–37 years after ACL reconstructions4 (Box 3). In our model, knee osteoarthritis is assumed to commence for all age groups at 30 years of age, reflecting the fact that post‐traumatic knee osteoarthritis generally develops (if at all) 10–15 years after ACL rupture.6
Utility estimates
The number of years of life lived in each health state was multiplied by the utility estimates for each health state (Box 3) to calculate quality‐adjusted life years (QALYs). Once a player has a ruptured ACL, we used the utility value reported in a recent meta‐analysis that pooled seven European Quality of Life 5 Dimensions (EQ‐5D) survey scores.3 The EQ‐5D is a standardised, widely used instrument for assessing health status.31 Knee osteoarthritis utility scores were derived from the Osteoarthritis Initiative database.22
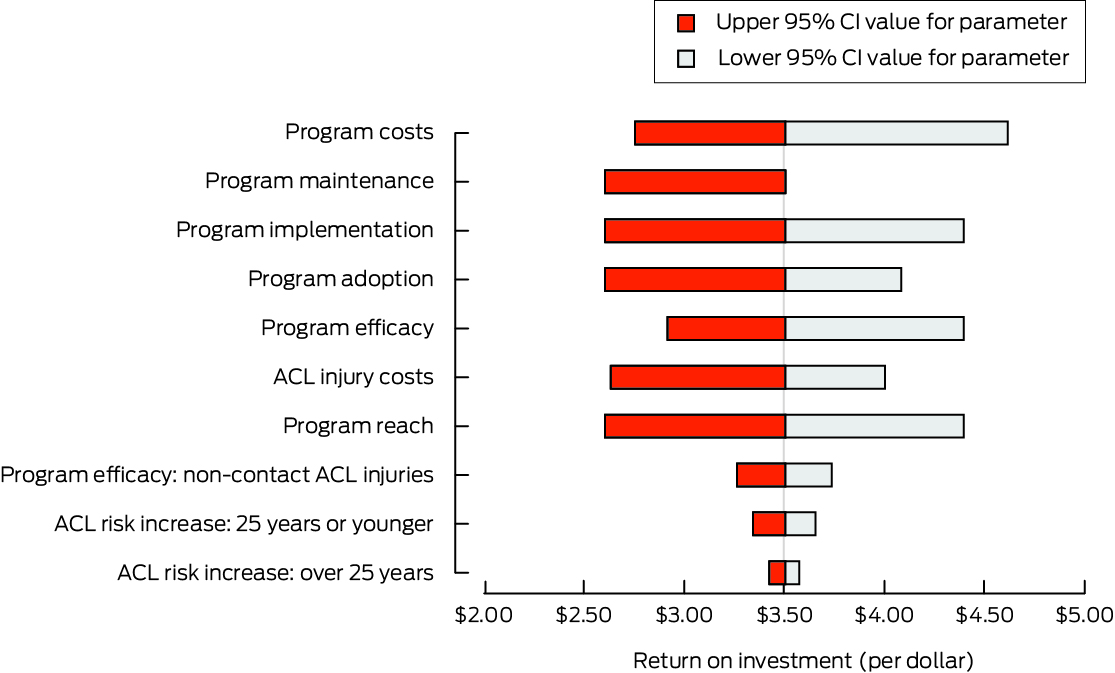
Sensitivity analysis
We tested the robustness of our model projections in one‐way sensitivity analyses in which the model values for 21 parameters related to transition probabilities, costs, and utilities were replaced by their upper or lower 95% confidence interval (CI) values. We also tested the robustness of our model projections in a probabilistic sensitivity analysis using Monte Carlo simulations. For the probabilistic sensitivity analysis, all model inputs were randomly drawn 10 000 times from distributions of the model inputs (gamma distributions for costs and beta distributions for utilities, transition probabilities, and effectiveness).
Ethics approval
We did not seek formal ethics approval for our analysis of publicly available data.
Results
Injury events
Our model estimated a total of 53 816 ACL ruptures over 35 years (15.8% of all players) (Box 4). Among players who had ruptured ACLs, it was estimated that 3.2% would have re‐ruptures, 18% would develop knee osteoarthritis, 2.8% would have total knee replacements, and 0.1% would have total knee replacement revisions. With the injury prevention program, the estimated number of ACL ruptures was reduced by 4385 (to 49 431 ACL ruptures), or by 8.1%. The estimated reduction in number of ruptured ACLs with the injury prevention program was greatest for players aged 10–17 years (1961 fewer in male players [7.8%], 739 fewer in female players [9.3%]). Compared with no program, the number of knee osteoarthritis cases was reduced by 8.1% (780 fewer), the number of total knee replacements by 8.1% (121 fewer), and the number of knee replacement revisions by 6.8% (three fewer) with the injury prevention program (Box 4). It was estimated that about 125 ACL ruptures, four ACL re‐ruptures, 22 cases of knee osteoarthritis, and three total knee replacements would be averted by the program each year.
Injury costs
Over 35 years, total discounted ACL injury costs were $825 225 870 (Box 5); 89.7% of these costs were immediate ACL injury treatment costs, and 10.3% were related to future knee osteoarthritis and total knee replacement costs. The mean ACL injury cost (total costs divided by total number of ACL injury events) (Box 4) was $30 665 for both male and female players; by age group, it was $30 451 (10–17 years), $30 786 (18–34 years), and $32 204 (35 years or older). Taking the annual program implementation cost of $925 582 into account, the program was dominant (achieved better outcomes and cost savings compared with no program), with a total cost saving of $52 539 751 over 35 years ($1 501 136 per year), or $3.51 per dollar of total program costs (male footballers, $3.30 per dollar; female footballers, $4.16 per dollar), and a total of 445 QALYs gained. The program was no longer a dominant strategy when the annual program implementation cost was raised to $2 000 000 (Supporting Information, figure 1). The estimated cost savings in medical and societal costs over 35 years were larger if adoption of the program by football players was increased by 15% ($15 787 012 saved [$451 057 per year]; $4.56 per dollar invested) or if program implementation was increased by 15% ($26 735 097 saved [$763 860 per year]; $5.29 per dollar invested).
Sensitivity analyses
In our model, return on investment was most sensitive to changes in program implementation costs, reach, adoption, effectiveness, implementation and maintenance. The return on investment ranged from $2.64 to $4.01 when varying the ACL injury cost value alone (Box 6).
In the probabilistic sensitivity analysis, the median return on investment was $6.23 (interquartile range [IQR], $3.61 to $8.98) per dollar invested. The median total cost difference between the control and intervention groups ($93 634 258; IQR, $54 453 912 to $133 693 771) was greater than in the main analysis; the median discounted program costs were similar to those of the main analysis ($14 931 928; IQR, $13 922 683 to $15 981 146) (Supporting Information, table 6). In the probabilistic sensitivity analysis, 9499 of 10 000 simulations yielded returns on investment exceeding 1:1 (Supporting Information, figure 2). In about 7% of probabilistic sensitivity analysis model runs, loss of QALYs was estimated for the injury prevention program because the randomly selected utility values were larger for injured health states than the uninjured health state.
Discussion
We report the first economic modelling of the cost savings that could be achieved by a national ACL injury prevention program for amateur footballers in Australia. Our findings suggest that such a program could lead to substantial cost savings; as each dollar invested would yield a return of $3.51, the program could be considered a sound financial investment. The robustness of our main findings were confirmed in sensitivity analyses, indicating that the primary prevention of ACL injuries can be economically justified. As the injury prevention program was found to be a dominant strategy (concurrent health benefits and cost savings), incremental cost‐effectiveness ratios were not reported (these are reported when benefits are accompanied by increased costs).32 A New Zealand study found that the return on investment for a national football injury prevention program was NZ$2.41 per dollar, and even higher for rugby union (NZ$7.18) and netball (NZ$12.64).33 National programs should be favoured over local programs; a systematic review of national public health interventions found that they generally achieve a greater return on investment.8 Our model also indicated the importance of optimising program adoption and implementation; increasing either factor by 15% achieved a higher return on investment than with their baseline values (program adoption, $4.56 per dollar; program implementation, $5.29 per dollar). This finding implies, from a cost‐effectiveness perspective, that effective ACL injury prevention programs should be scaled up and widely implemented.19
Another important finding was the sensitivity of cost savings and return on investment to RE‐AIM inputs. Our preliminary study of the costs of ACL reconstructions estimated that $32 792 456 could be saved per year with a program with extremely high coach and player adherence.1 The Markov model indicated that, once the RE‐AIM framework is applied, annual savings of $1 501 136 in medical and societal costs were possible, 95.4% less than our original estimate, but still yielding a 351% return on investment.
Knowing how to measure progress is vital before introducing a national ACL injury prevention program.19 Countries such as Sweden, Switzerland, and Belgium have found that national programs for averting sports injuries can reduce the incidence of ACL injury.34 In Sweden, the incidence of knee injuries in male football players was reduced by 8% (95% CI, 4–11%) and in female players by 21% (95% CI, 17–25%).35 The three countries have two major similarities: they have all used national insurance data or surveys to track injury prevention progress, and all have developed partnerships with their national sporting organisations. Strong partnerships between researchers and national sporting organisations often precede program success.34
Research and policy implications
Our findings provide health policymakers, football organisations, and participants with costs data that can assist decision making regarding the primary prevention of ACL injuries. No organisation is currently responsible for preventing football injuries at the national level in Australia. Health systems (primary and secondary care), insurance companies (insurance claims), and players (direct, indirect, and intangible costs) bear the burden of ACL injuries. As the benefits of population‐level prevention strategies are often long term effects, they are often not priorities for policymakers.36 It may be that football participants, with support from sporting organisations and researchers, can play a role in overcoming this problem. The annual program costs reported in our study could be covered with an additional $2.72 paid by each player at registration and investing this money in injury prevention could make a significant difference.
Limitations
Our model assumed that all people with ACL injuries underwent ACL surgery; information on how many do not in Australia is not available. Further, data on costs associated with not having surgery (eg, rehabilitation costs, time cost for moving from conservative rehabilitation to ACL surgery) are not available. In any case, the ACL reconstruction rate in Australia is among the highest in the world (52.0 per 100 000 person‐years).29 With developments in the treatment of ACL injuries, it should be noted that costs are likely to change over time. Finally, the baseline data for program costs and real‐world effectiveness were respectively based on data from New Zealand and Sweden, so our findings should be applied to Australia with caution.
Conclusions
From an economic perspective, our findings support investment in a national, evidence‐based program for the primary prevention of ACL injuries in amateur football players, such as Perform+. Such a program could save our footballers from the short and long term consequences of ACL injuries and reduce their direct medical and societal costs. We found a return on investment of $3.51 per dollar invested in the program. Over 35 years, a pragmatic national ACL injury prevention program could save $52 539 751 in costs, avert 4385 ACL ruptures, and gain 445 QALYs. The program could also reduce the future incidence of knee osteoarthritis in current and former amateur football players. We recommend planning to reduce the risk of ACL injury in Australia, following the examples of New Zealand, Sweden, Switzerland, and Belgium.
Box 1 – Markov model health states for our study of the costs of anterior cruciate ligament (ACL) injuries in amateur football (soccer) players in Australia, and the return of investment of a national program for preventing ACL injuries
Box 2 – The RE‐AIM (reach, effectiveness, adoption, implementation, maintenance) framework, as applied to our Markov model of a national program for preventing anterior cruciate ligament injuries, Australia
|
|
|
Proportional reduction in anterior cruciate ligament injuries* |
|||||||||||||
|
Parameter, source |
Reported value in source |
Male players |
Female players |
||||||||||||
|
|
|||||||||||||||
|
Effectiveness7,† |
Male players: 50% |
50% |
58% |
||||||||||||
|
Reach21 |
66% |
33% |
38% |
||||||||||||
|
64% |
21% |
24% |
|||||||||||||
|
38% |
8% |
9% |
|||||||||||||
|
Maintenance21 |
100% |
8%‡ |
9%‡ |
||||||||||||
|
|
|||||||||||||||
|
* Calculated by serially multiplying the proportional reduction in the preceding row by the reported value for subsequent parameters. † The estimated program efficacy for the trials included in the meta‐analysis. Injury prevention programs are more effective for non‐contact injuries in female than male players.7 However, as an estimated 52% of anterior cruciate ligament injuries in amateur female footballers are non‐contact injuries,16 the value is reduced from 64% to 58%. ‡ These values, used in our model, are estimates of the real world effectiveness of the program. |
|||||||||||||||
Box 3 – Base cost (Australian dollars), and probability and utility assumptions for our Markov model of a national program for preventing anterior cruciate ligament injuries, Australia
|
Parameters |
Value (95% confidence interval)* |
Source |
|||||||||||||
|
|
|||||||||||||||
|
Annual costs |
|
|
|||||||||||||
|
Anterior cruciate ligament reconstruction |
$28 182 ($22 589–31 483) |
See Supporting information, table 1 |
|||||||||||||
|
Knee osteoarthritis |
$4782 ($787–8262) |
See Supporting information, tables 2 and 3 |
|||||||||||||
|
Total knee replacement |
$24 757 ($19 091–32 366) |
See Supporting information, table 1 |
|||||||||||||
|
Total knee replacement revision |
$35 510 ($30 373–42 708) |
See Supporting information, table 1 |
|||||||||||||
|
Transition probabilities |
|
|
|||||||||||||
|
Anterior cruciate ligament rupture |
By age: see Supporting information, table 4 |
See Supporting information, table 4 |
|||||||||||||
|
Anterior cruciate ligament re‐rupture |
By age: see Supporting information, table 5 |
See Supporting information, table 5 |
|||||||||||||
|
Concomitant meniscal injury and anterior cruciate ligament rupture |
48% (25–70%) |
See Supporting information, section 3 |
|||||||||||||
|
Risk of osteoarthritis |
|
|
|||||||||||||
|
Anterior cruciate ligament injury only |
32.1% (31.1–33.1%) |
||||||||||||||
|
Concomitant meniscal injury |
44.1% (33.7–54.5%) |
||||||||||||||
|
Risk of total knee replacement |
|
|
|||||||||||||
|
Anterior cruciate ligament injury only |
8.0% (7.3–8.8%) |
Reference 6 |
|||||||||||||
|
Concomitant meniscal injury |
22.3% (16.8–27.9%) |
Reference 6 |
|||||||||||||
|
Risk of total knee replacement revision |
|
|
|||||||||||||
|
Anterior cruciate ligament injury only |
1.1% (1.0–1.2%) |
Reference 6 |
|||||||||||||
|
Concomitant meniscal injury |
3.9% (2.7–5.1%) |
Reference 6 |
|||||||||||||
|
Utilities |
|
|
|||||||||||||
|
No knee injury |
0.910 (0.728–1.00) |
Reference 21 |
|||||||||||||
|
Anterior cruciate ligament rupture |
0.740 (0.540–0.940) |
Reference 3 |
|||||||||||||
|
Knee osteoarthritis |
0.780 (0.660–0.860) |
Reference 22 |
|||||||||||||
|
After total knee replacement |
0.835 (0.668–1.00) |
Reference 27 |
|||||||||||||
|
|
|||||||||||||||
|
* Used for ranges for sensitivity analyses. |
|||||||||||||||
Box 4 – Simulated number of events over 35 years, with and without the injury prevention prgram, by gender and age group
|
Group |
Control |
Intervention |
Difference in number of events |
||||||||||||
|
|
|||||||||||||||
|
Total population |
340 253 |
340 253 |
— |
||||||||||||
|
Anterior cruciate ligament ruptures |
53 816 (15.8%) |
49 431 (14.5%) |
4385 (8.1%) |
||||||||||||
|
Male players |
|
|
|
||||||||||||
|
10–17 years |
25 117 (5.4%) |
23 155 (4.9%) |
1961 (7.8%) |
||||||||||||
|
18–34 years |
13 322 (1.6%) |
12 281 (1.5%) |
1040 (7.8%) |
||||||||||||
|
35 years or older |
2461 (0.1%) |
2268 (0.1%) |
193 (7.8%) |
||||||||||||
|
Female players |
|
|
|
||||||||||||
|
10–17 years |
7932 (5.4%) |
7192 (4.9%) |
739 (9.3%) |
||||||||||||
|
18–34 years |
4207 (1.6%) |
3826 (1.4%) |
381 (9.1%) |
||||||||||||
|
35 years or older |
777 (0.1%) |
707 (0.1%) |
70 (9.1%) |
||||||||||||
|
Anterior cruciate ligament re‐rupture* |
1740 (3.2%) |
1597 (3.2%) |
143 (8.2%) |
||||||||||||
|
Male players |
1323 (3.2%) |
1219 (3.2%) |
104 (7.9%) |
||||||||||||
|
Female players |
418 (3.2%) |
377 (3.2%) |
41 (9.8%) |
||||||||||||
|
Knee osteoarthritis† |
9618 (2.8%) |
8838 (2.6%) |
780 (8.1%) |
||||||||||||
|
Male players |
7310 (2.8%) |
6739 (2.6%) |
571 (7.8%) |
||||||||||||
|
Female players |
2309 (2.8%) |
2099 (2.6%) |
210 (9.1%) |
||||||||||||
|
Total knee replacement‡ |
1491 (0.4%) |
1370 (0.4%) |
121 (8.1%) |
||||||||||||
|
Male players |
1133 (0.4%) |
1045 (0.4%) |
89 (7.9%) |
||||||||||||
|
Female players |
358 (0.4%) |
326 (0.4%) |
32 (8.9%) |
||||||||||||
|
Total knee replacement revision§ |
47 (< 0.1%) |
43 (< 0.1%) |
4 (6.4%) |
||||||||||||
|
Male players |
36 (< 0.1%) |
33 (< 0.1%) |
3 (8.3%) |
||||||||||||
|
Female players |
11 (< 0.1%) |
10 (< 0.1%) |
1 (9.1%) |
||||||||||||
|
|
|||||||||||||||
|
* Denominator: number of anterior cruciate ligament ruptures. † Denominator: number of anterior cruciate ligament ruptures or anterior cruciate ligament re‐ruptures, ‡ Denominator: number of cases of knee osteoarthritis. § Denominator: number of total knee replacements. |
|||||||||||||||
Box 5 – Simulated total anterior cruciate ligament injury costs over 35 years, with and without the injury prevention program, by gender and age group
|
|
|
Total costs |
Mean costs (per player) |
||||||||||||
|
Gender/age group (years) |
Population |
Control |
Intervention |
Costs saved |
Control |
Intervention |
Costs saved |
||||||||
|
|
|||||||||||||||
|
All players |
340 253 |
$825 225 870 |
$772 686 119 |
$52 539 751 |
$2425 |
$2271 |
$154 |
||||||||
|
Male players |
|
|
|
|
|
|
|
||||||||
|
10–17 |
142 743 |
$352 817 303 |
$331 551 370 |
$21 265 932 |
$2472 |
$2323 |
$149 |
||||||||
|
18–34 |
81 198 |
$223 945 940 |
$210 038 714 |
$13 907 226 |
$2758 |
$2587 |
$171 |
||||||||
|
35 or older |
34 651 |
$50 408 419 |
$47 993 236 |
$2 415 183 |
$1455 |
$1385 |
$70 |
||||||||
|
Female players |
|
|
|
|
|
|
|
||||||||
|
10–17 |
45 077 |
$111 415 990 |
$102 702 216 |
$8 713 774 |
$2472 |
$2278 |
$193 |
||||||||
|
18–34 |
25 641 |
$70 719 770 |
$65 444 066 |
$5 275 704 |
$2758 |
$2552 |
$206 |
||||||||
|
35 or older |
10 943 |
$15 918 448 |
$14 956 516 |
$961 932 |
$1455 |
$1367 |
$88 |
||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 4 October 2023, accepted 15 January 2024
- Andrew Ross1,2
- Joosup Kim3
- Marnee McKay4
- Evangelos Pappas5
- Natalie Hardaker6,7
- Matt Whalan8,9
- Kerry Peek4
- 1 The University of Sydney, Sydney, NSW
- 2 Victoria University, Melbourne, VIC
- 3 Southern Clinical School, Monash University, Melbourne, VIC
- 4 Sydney School of Health Sciences, University of Sydney, Sydney, NSW
- 5 Illawarra Health and Medical Research Institute, University of Wollongong, Wollongong, NSW
- 6 Sports Performance Research Institute New Zealand (SPRINZ), Auckland University of Technology, Auckland, New Zealand
- 7 Accident Compensation Corporation, Wellington, New Zealand
- 8 Centre of Medical and Exercise Physiology, University of Wollongong, Wollongong, NSW
- 9 Football Australia, Sydney, NSW
Open access:
Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
Data sharing:
Not applicable; the study was based on publicly available data.
We thank Football NSW, Northern NSW Football, and an insurance company (anonymity requested) for providing some of the costs data.
No relevant disclosures.
- 1. Ross AG, Agresta B, McKay M, et al. Financial burden of anterior cruciate ligament reconstructions in football (soccer) players: an Australian cost of injury study. Injur Prev 2023; 29: 474‐481.
- 2. Pryymachenko Y, Wilson R, Abbott JH. Epidemiology of cruciate ligament injuries in New Zealand: exploring differences by ethnicity and socioeconomic status. Injur Prev 2023; 29: 213‐218.
- 3. Filbay SR, Skou ST, Bullock GS, et al. Long‐term quality of life, work limitation, physical activity, economic cost and disease burden following ACL and meniscal injury: a systematic review and meta‐analysis for the OPTIKNEE consensus. Br J Sports Med 2022; 56: 1465‐1474.
- 4. Filbay S, Andersson C, Gauffin H, et al. Prognostic factors for patient‐reported outcomes at 32 to 37 years after surgical or nonsurgical management of anterior cruciate ligament injury. Orthop J Sports Med 2021; 9: 23259671211021592.
- 5. Lohmander LS, Roemer FW, Frobell RB, Roos EM. Treatment for acute anterior cruciate ligament tear in young active adults. NEJM Evid 2023; 2: EVIDoa2200287.
- 6. Suter LG, Smith SR, Katz JN, et al. Projecting lifetime risk of symptomatic knee osteoarthritis and total knee replacement in individuals sustaining a complete anterior cruciate ligament tear in early adulthood. Arthritis Care Res (Hoboken) 2017; 69: 201‐208.
- 7. Webster KE, Hewett TE. Meta‐analysis of meta‐analyses of anterior cruciate ligament injury reduction training programs. J Orthop Res 2018; 36: 2696‐2708.
- 8. Masters R, Anwar E, Collins B, et al. Return on investment of public health interventions: a systematic review. J Epidemiol Community Health 2017; 71: 827‐834.
- 9. Lewis DA, Kirkbride B, Vertullo CJ, et al. Comparison of four alternative national universal anterior cruciate ligament injury prevention programme implementation strategies to reduce secondary future medical costs. Br J Sports Med 2018; 52: 277‐282.
- 10. Gebert A, Gerber M, Pühse U, et al. Injury prevention in amateur soccer: a nation‐wide study on implementation and associations with injury incidence. Int J Environ Res Public Health 2019; 16: 1593.
- 11. Quarrie K, Gianotti S, Murphy I, et al. RugbySmart: challenges and lessons from the implementation of a nationwide sports injury prevention partnership programme. Sports Med 2020; 50: 227‐230.
- 12. O'Brien J, Hagglund, M, Bizzini, M. Implementing injury prevention. The rocky road from RCT to real‐world injury reduction. Aspetar 2018; 7(June): 70‐76.
- 13. Carta A, Conversano C. On the use of Markov models in pharmacoeconomics: pros and cons and implications for policy makers. Front Public Health 2020; 8: 569500.
- 14. Husereau D, Drummond M, Petrou S, et al; CHEERS Task Force. Consolidated health economic evaluation reporting standards (CHEERS) statement. Int J Technol Assess Health Care 2013; 29: 117‐122.
- 15. Football Federation Australia. 2022 National participation report. https://www.footballaustralia.com.au/sites/ffa/files/2023‐04/19686_FA_Participation%20Reports_2022_High%20Res_Full.pdf (viewed Oct 2022).
- 16. Ross AG, McKay M, Pappas E, Peek K. Insurance cost and injury characteristics of anterior cruciate ligament injuries in sub‐elite football: a population analysis involving 3 years of Australian insurance data. J Sci Med Sport 2023; 26: 365‐371.
- 17. Football Australia. Football Australia Perform+. Undated. www.footballaustralia.com.au/performance/football‐australia‐perform (viewed Nov 2022).
- 18. Bizzini M, Dvorak J. FIFA 11+: an effective programme to prevent football injuries in various player groups worldwide: a narrative review. Br J Sports Med 2015; 49: 577‐579.
- 19. Milat AJ, Newson R, King L, et al. A guide to scaling up population health interventions. Public Health Res Pract 2016; 26: e2611604.
- 20. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE‐AIM framework. Am J Public Health 1999; 89: 1322‐1327.
- 21. Viney R, Norman R, King MT, et al. Time trade‐off derived EQ‐5D weights for Australia. Value Health 2011; 14: 928‐936.
- 22. Ferket BS, Feldman Z, Zhou J, et al. Impact of total knee replacement practice: cost effectiveness analysis of data from the Osteoarthritis Initiative. BMJ 2017; 356: j1131.
- 23. Lindblom H, Sonesson S, Forslind J, et al. Implementation of the injury prevention exercise programme Knee Control+: a cross‐sectional study after dissemination efforts within a football district. Inj Prev 2023; 29: 399‐406.
- 24. Ross AG, McKay MJ, Pappas E, et al. The FIFA 11+: Why is adherence so challenging? Insights from a cross‐sectional study of stakeholders in Australian amateur football (soccer). International Journal of Sports Science and Coaching 2023; 19: 17479541231174506.
- 25. Gianotti S, Hume PA, Tunstall H. Efficacy of injury prevention related coach education within netball and soccer. J Sci Med Sport 2010; 13: 32‐35.
- 26. Organisation for Economic Cooperation and Development. Purchasing power parities [OECD Data]. https://data.oecd.org/conversion/purchasing‐power‐parities‐ppp.htm#indicator‐chart (viewed Aug 2023).
- 27. Losina E, Weinstein AM, Reichmann WM, et al. Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res (Hoboken) 2013; 65: 703‐711.
- 28. Australian Institute of Health and Welfare. Health expenditure Australia 2020–21. 23 Nov 2022. https://www.aihw.gov.au/reports/health‐welfare‐expenditure/health‐expenditure‐australia‐2020‐21/contents/summary (viewed Oct 2022).
- 29. Janssen KW, Orchard JW, Driscoll TR, van Mechelen W. High incidence and costs for anterior cruciate ligament reconstructions performed in Australia from 2003–2004 to 2007–2008: time for an anterior cruciate ligament register by Scandinavian model? Scand J Med Sci Sports 2012; 22: 495‐501.
- 30. Zbrojkiewicz D, Vertullo C, Grayson JE. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2015. Med J Aust 2018; 208: 354‐358. https://www.mja.com.au/journal/2018/208/8/increasing‐rates‐anterior‐cruciate‐ligament‐reconstruction‐young‐australians
- 31. EuroQol Group. EuroQol: a new facility for the measurement of health‐related quality of life. Health Policy 1990; 16: 199‐208.
- 32. Klok RM, Postma MJ. Four quadrants of the cost‐effectiveness plane: some considerations on the south‐west quadrant. Expert Rev Pharmacoecon Outcomes Res 2004; 4: 599‐601.
- 33. Gianotti S, Hume PA. A cost–outcome approach to pre and post‐implementation of national sports injury prevention programmes. J Sci Med Sport 2007; 10: 436‐446.
- 34. Ross AG, Donaldson A, Poulos RG. Nationwide sports injury prevention strategies: a scoping review. Scand J Med Sci Sports 2021; 31: 246‐264.
- 35. Åman M, Larsén K, Forssblad M, et al. A nationwide follow‐up survey on the effectiveness of an implemented neuromuscular training program to reduce acute knee injuries in soccer players. Orthop J Sports Med 2018; 6: 2325967118813841.
- 36. Williamson A, Tait H, El Jardali F, et al. How are evidence generation partnerships between researchers and policy‐makers enacted in practice? A qualitative interview study. Health Res Policy Syst 2019; 17: 41.






Abstract
Objectives: To estimate the long term cost savings, return on investment, and gain in quality‐adjusted life years (QALYs) that could be achieved by a national anterior cruciate ligament (ACL) injury prevention program for amateur football (soccer) players in Australia.
Study design: Markov model decision analysis.
Setting, participants: Two hypothetical scenarios including all amateur football players in Australia (340 253 players): no intervention, and a national ACL injury prevention program. Transitions between health states, including ACL rupture, meniscal injury, knee osteoarthritis, and total knee replacement were made in one‐year cycles over 35 years from a societal perspective.
Main outcome measures: Cost savings, return on investment, and QALY gain achieved in the prevention program scenario relative to control scenario, by age group (10–17, 18–34, 35 years or older) and gender. Secondary outcomes: incidence of ACL rupture, knee osteoarthritis, total knee replacement, and total knee replacement revision.
Results: The total mean cost of an ACL injury was estimated to be $30 665. The national injury prevention program was projected to save $52 539 751 in medical and societal costs caused by ACL ruptures in amateur footballers over 35 years; the estimated return on each dollar invested in the program was $3.51. Over this period, the number of players with ruptured ACLs could be reduced by 4385 (9%), the number of knee osteoarthritis cases by 780 (8.1%), and the number of total knee replacements by 121 (8.1%); 445 QALYs were gained.
Conclusion: Our findings support investing in a national, evidence‐based program for the primary prevention of ACL injuries in amateur football players.