The known: High blood pressure is the leading cause of premature death in Australia, but the national costs of treating hypertension are unknown.
The new: We estimated that $1.2 billion was spent on the management of hypertension in Australia during 2021–22, including $611 million for pharmacy‐related costs and fees (51%). Patients incurred $503 million in out‐of‐pocket costs ($35 million for general practice consultations, $468 million for blood pressure‐lowering medications).
The implications: A substantial proportion of the cost of hypertension management is directly borne by patients. Recent policy changes may reduce their out‐of‐pocket costs, but further efforts may be needed to ensure these costs are not barriers to improving hypertension control in Australia.
High blood pressure is a leading cause of death and disability in Australia, and its economic impact is considerable.1,2,3 Hypertension awareness, treatment, and control have stagnated in Australia since 1990;4 the rate of controlled hypertension in 2019 (32%)2 is poor compared with rates for comparable countries, such as 51% in the United States and 59% in Canada.4
Following a call to action,5 a national hypertension taskforce was formed in 2022, hosted by the Australian Cardiovascular Alliance and Hypertension Australia, to examine these important problems. The taskforce set a target for Australia of 70% blood pressure control by 2030.6 To help inform taskforce discussions, we sought to quantify the costs of hypertension diagnosis and treatment in Australia during 2012–22, particularly in primary care, including general practices and pharmacies.
Methods
To estimate expenditure on hypertension diagnosis and treatment by source of funding, we used publicly available Pharmaceutical Benefits Scheme (PBS),7 Medicare Benefits Schedule (MBS),8 MedicineInsight general practice reports,9,10 and Community Pharmacy Agreement11 data.
The primary outcome for our study was expenditure on hypertension treatment from the perspective of the Australian health care system (government costs and patient co‐payments). The study population comprised people who received services or medications subsidised by the MBS or PBS during 1 July 2012 – 30 June 2022. The MBS and PBS programs provide universal health care insurance and subsidised medicines as part of the Australian health care system. The MBS and PBS databases include aggregate data regarding health service activities by activity or product and patient type; the demographic and clinical characteristics of people receiving these services or products cannot be determined from these sources. We report costs in 2022 Australian dollars, adjusted for inflation using the mean Australian Bureau of Statistics annual consumer price index (CPI) value for each financial year12 (Supporting Information, table 1).
Pharmaceutical costs
We collated PBS codes for all blood pressure‐lowering medications primarily used to treat hypertension that were available in Australia during 2012–22 (Supporting Information, table 2), and extracted prescription and subsidy data from the Medicare items report database, stratified by financial year. Total PBS expenditure for blood pressure‐lowering medications was defined as the total PBS subsidy amount (government co‐payments) for all contribution types. Historical PBS co‐payments data are published by the PBS.13
To calculate patient out‐of‐pocket expenses for pharmaceuticals, we multiplied the mean annual co‐payment threshold for each category in a given year by the corresponding category prescription volume for the year. The PBS Safety Net program means that prescription distributions by price are not uniform throughout the year; we used the mean cost and volume for ease of analysis. For example, 282 977 prescriptions were dispensed to people in the general dispensing category during 2021–22; as the general co‐payment was $41.30 per dispensing event in 2021 and $42.50 in 2022, we used the mean value ($41.90) to calculate the total general patient co‐payment value for 2021–22. Data for prescriptions dispensed below the co‐payment level were collected from corresponding PBS reports7 and combined with the co‐payment amounts to calculate total patient out‐of‐pocket costs.
In a secondary analysis, overall medication costs for 2021–22 were split into the components outlined in the Community Pharmacy Agreement: manufacturer prices, wholesaler markups, pharmacy administration, handling and infrastructure fees, dispensing fees, and electronic prescription fees.11 As data for electronic prescription fees are not available for individual medications, our calculation is based on the proportions of all PBS‐subsidised prescriptions that were for blood pressure‐lowering medications.14 For PBS‐subsidised prescriptions, we multiplied the published fees by our estimate of the dispensing number for each category. Cost components were also estimated for prescriptions dispensed below the co‐payment level to generate the total figures.
We did not include expenditure on guideline‐recommended non‐pharmacological therapies for hypertension, such as salt substitution, weight loss, and alcohol reduction, nor for complementary and alternative therapies. We did not have data for medications dispensed on private prescriptions to vary the cost from the PBS pricing structure (often by discounted pharmacies or as personal arrangements) or for people without Medicare cards. We excluded blood pressure‐lowering medications primarily used for indications other than hypertension according to the Australian Medicine Handbook (https://amhonline.amh.net.au) and clinical expertise. We also excluded the costs of laboratory tests and other monitoring associated with treatment, and the costs of in‐hospital treatment of hypertension. Finally, we estimated the costs of treatment, not those of cardiovascular disease.
Costs of general practice consultations and ambulatory blood pressure monitoring
Numbers of general practice visits and data on MBS subsidies and patient co‐payments were extracted from Medicare item reports (item number 23).8 As 1.5% of general practice encounters in Australia (2016–17) were primarily for hypertension management9 and hypertension was recorded in 6% of consultations during 2020–21,10 we assumed that 3.8% of general practice encounters included hypertension care. In sensitivity analyses, we applied 1.5% as the lower limit and 6% as the upper limit for general practice encounters entirely or partially dedicated to hypertension diagnosis and management. Data on ambulatory blood pressure monitoring during 2021–22 were extracted from Medicare item reports (item number 11607; introduced in November 2021).8
Ethics approval
As a negligible risk project, we did not seek formal ethics review for our analysis of publicly available aggregate data. We report the study according to the Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement.15
Results
Total annual expenditure on the diagnosis and management of hypertension (PBS, MBS, patient out‐of‐pocket costs), in 2022 dollars, was $1321 million in 2012–13 and $1201 million in 2021–22. Between 48 and 56 million PBS‐subsidised prescriptions for blood‐pressure lowering medications were dispensed each year (Box 1). An estimated 2.3 million general practice visits per year were primarily for hypertension management (ie, lower estimate of general practice consultation numbers), and a further 6.9 million visits per year included some aspect of hypertension management (difference between higher and lower estimates) (Supporting Information, table 3). The number of claims for MBS‐subsidised ambulatory blood pressure monitoring was 4998 per month during 1 November 2021 – 30 June 2022.
Expenditure for hypertension care, by source
During 2012–22, the estimated total expenditure for the diagnosis and treatment of hypertension was $12.2 billion (low estimate: $10.3 billion; high estimate: $14.0 billion); $7.3 billion (60%; low estimate: $5.6 billion, 54%; high estimate: 8.9 billion, 64%) was borne by the MBS and PBS, and $4.9 billion (40%; low estimate: $4.7 billion, 46%; high estimate: $5.1 billion, 36%) by patients as out‐of‐pocket costs (Supporting Information, table 4).
During 2021–22, the MBS provided an estimated $310 million for general practice consultation and ambulatory blood pressure monitoring costs, or 26% of all hypertension‐related expenditure for this year, and patients provided $35 million as out‐of‐pocket expenses for this purpose (2.9%) (Supporting Information, table 4).
The mean annual out‐of‐pocket costs for patients for blood pressure‐lowering medications during 2012–22 was $461 million (Supporting Information, table 4). In 2021–22, $275 million of the $468 million out‐of‐pocket costs (59%; 23% of total hypertension‐related expenditure) were incurred by patients who bore the entire medication cost (no government co‐payment) and $193 million (16% of total hypertension‐related expenditure) by people dispensed medications subsidised by the PBS. PBS expenditure for blood pressure‐lowering medicines declined from $609 million in 2012–13 to $387 million (32% of total) in 2021–22 (Supporting Information, table 4).
Expenditure for hypertension care, by component
Total hypertension‐related general practice consultation costs increased from $270 million in 2012–13 to $346 million in 2021–22; the estimated annual number of hypertension‐related general practice consultations increased from 4.9 to 7.2 million (Supporting Information, tables 3 and 4). With the lower estimate of hypertension‐related general practice consultations (1.5%), total costs rose from $107 million to $136 million; using the upper estimate of hypertension‐related consultations (6%), they rose from $427 million to $549 million.
In 2021–22, estimated total direct expenditure for blood pressure‐lowering medications was $244.3 million (ex‐manufacturer price, $221.5 million; wholesale markup, $22.8 million), or 20.3% of total hypertension‐related expenditure) for 55.6 million prescriptions; pharmacy‐related costs totalled $611.1 million (administration and handling fees, $238 million; dispensing fees, $370.6 million; electronic prescription fees, $2.4 million), or 50.8% of total hypertension‐related expenditure (Box 2).
In 2021–22, MBS expenditure for ambulatory blood pressure monitoring was $8.5 million; patient co‐payments were not reported.
Discussion
We estimate that about $1.2 billion was spent on treating hypertension in Australia during 2021–22, and that 42% of this cost was borne by patients as out‐of‐pocket costs. The largest components of expenditure were pharmacy fees (50.9%), general practice consultation costs (28.5%), and pharmaceutical manufacturer costs (18.4%).
About 51% of expenditure on hypertension care during 2021–22 comprised pharmacy service costs for dispensing and administration, and handling fees. As dispensing of 30 days’ medication was standard at this time, fees were incurred each month. The introduction of 60‐day dispensing is expected to reduce medication costs,16 and could also improve medication adherence, although only limited randomised trial evidence for guiding policy in this area is available.17,18 Dispensing of 90 days’ antihypertensive medication is standard in many countries.19 The effect of longer term dispensing and other interventions on medication adherence and the frequency and type of patient interactions should be investigated in randomised trials.
About 29% of hypertension care expenditure was for primary care diagnosis and management. However, to achieve higher hypertension control rates, many more people need to receive recommended and improved treatment. Team‐based care encompassing general practitioners, pharmacists, and nurses is probably the most promising and economic route to this goal. Expanding the skills of pharmacists and nurses and enabling them to contribute more substantially to hypertension diagnosis and management are feasible.20
About 20% of the costs of hypertension care were the direct costs of the medicines. While PBS expenditure steadily declined during 2012–22, patient out‐of‐pocket costs have increased. Consequently, cost‐competitive generic medicines will continue to be needed to economically improve hypertension control.
Finally, but perhaps most importantly, 41% of expenditure comprises out‐of‐pocket costs for patients, which has major implications for equitable access and outcomes. While concessional health care cards mitigate inequity, substantial differences in both absolute cardiovascular risk and cardiovascular disease preventive medicine use associated with socio‐economic disadvantage are major problems in Australia.21 Out‐of‐pocket pharmaceutical expenses can be significant barriers for people in low income households with one or more chronic conditions.22,23 In July 2022, the dispensing number and out‐of‐pocket payments needed to reach the PBS safety net threshold were reduced,13 and the general patient co‐payment was reduced to $30 in 2023, the first reduction since the introduction of the PBS.13
Limitations
Despite the reliability of the publicly available data sources we used, and the breadth and comprehensiveness of the data, our cost estimates rely on assumptions, including the proportion of general practice appointments dedicated to hypertension diagnosis and management. Although we excluded blood pressure‐lowering medications primarily used for other purposes, some dispensed prescriptions for non‐hypertension use will have been included in our analysis. Further, we did not include other out‐of‐pocket costs for managing hypertension, including blood pressure‐monitoring devices and non‐pharmacological therapies; the full cost of hypertension treatment and management will be higher than we estimated. Better blood pressure control could reduce costs to the health system and patients by averting cardiovascular events,3 an effect for which we did not account in our analysis. PBS expenditure is well documented, and we have confidence in our estimates of MBS use. The effect of reaching the Hypertension Taskforce 70% treatment target on costs was beyond the scope of our analysis. Reliable estimates of the number of people being treated for hypertension are needed for robust modelling of the complete costs of current and alternative hypertension care models.
Conclusion
We estimate hypertension diagnosis and management cost $1.2 billion in Australia in 2021–22. Important changes to pharmacy supply and payment policy were introduced in 2023, but further efforts may be needed to reduce treatment costs for patients. These changes are particularly important if the hypertension control rate is to be substantially improved in Australia, given the large number of people for whom treatment should be initiated or improved.2
Box 1 – Expenditure on diagnosis and treatment of hypertension (adjusted to 2022 Australian dollars), and general practice consultations and dispensing of prescriptions of medications for managing hypertension, Australia, 2012–13 to 2021–22
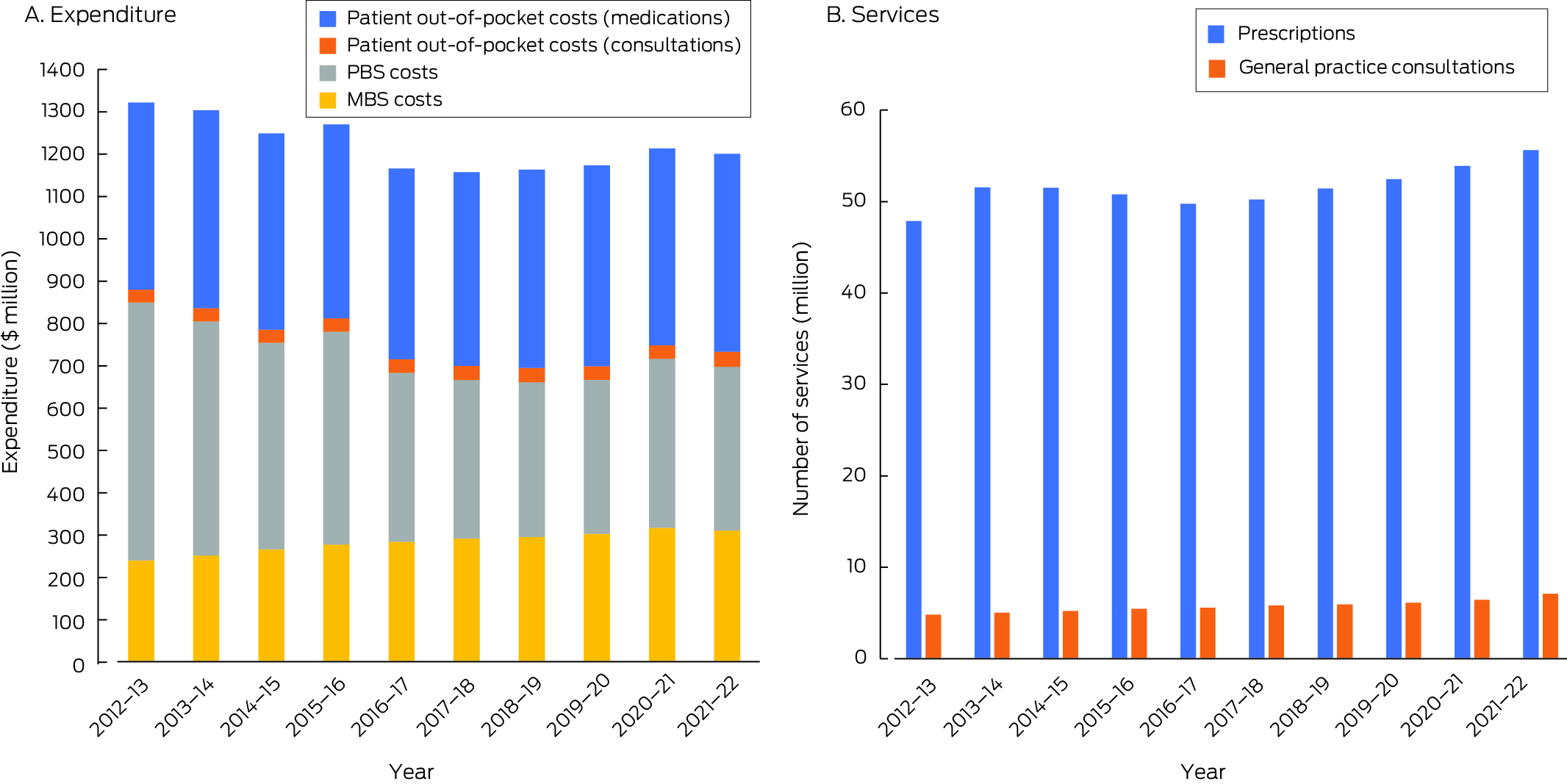
* The data underlying panel A are included in the Supporting Information, table 4A; the data in panel B are included in the Supporting Information, table 3.
Box 2 – Expenditure on the diagnosis and treatment of hypertension, and general practice consultations and dispensing of medications for managing hypertension, Australia, 2021–22, by broad expenditure category*
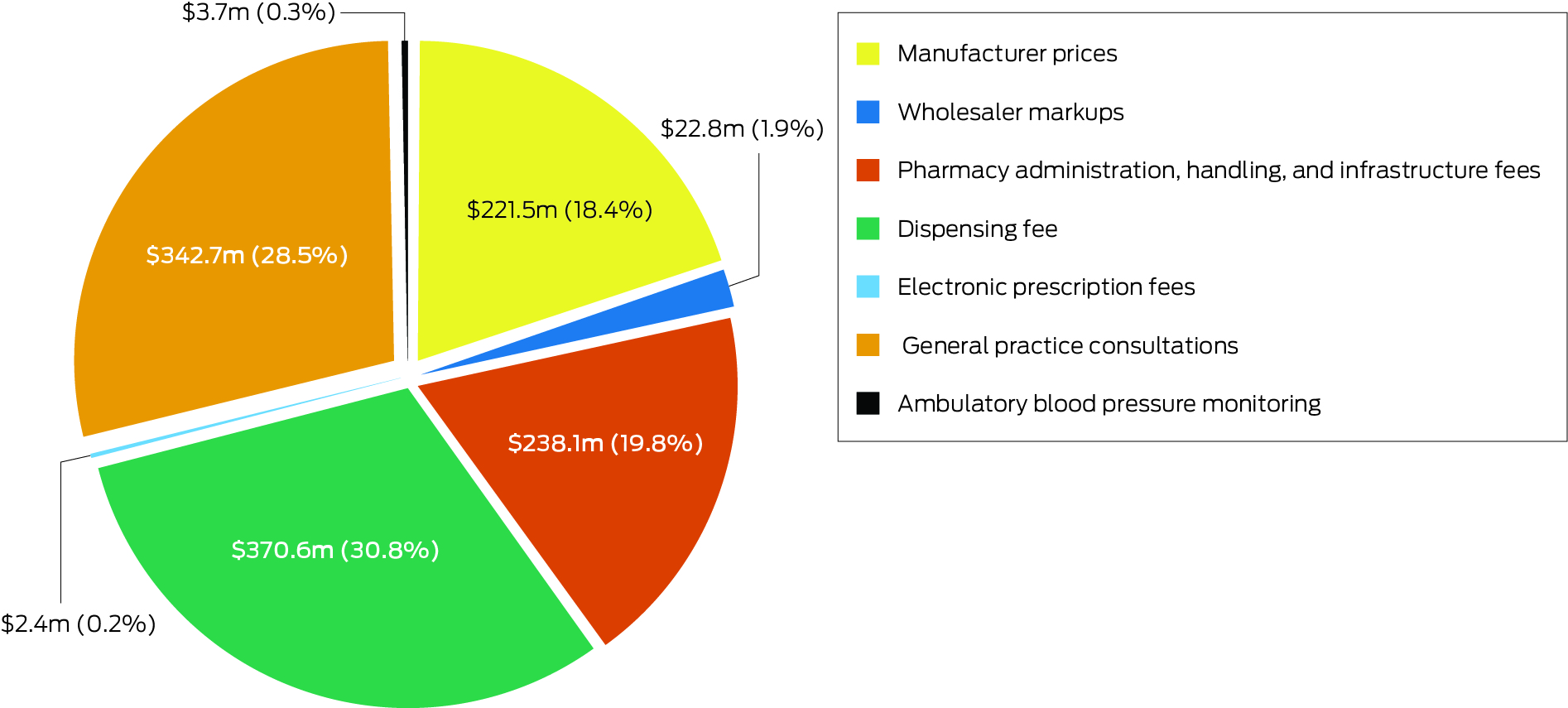
* The pharmaceutical data underlying this graph are included in the Supporting Information, table 6.
Received 5 December 2023, accepted 21 March 2024
- Emily R Atkins1,2
- Long Huy Nguyen3
- Mary Lou Chatterton4
- Markus Schlaich5
- Aletta E Schutte2
- Anthony Rodgers1,2
- 1 The George Institute for Global Health, Sydney, NSW
- 2 The University of New South Wales, Sydney, NSW
- 3 Melbourne Medical School, the University of Melbourne, Melbourne, VIC
- 4 Monash University, Melbourne, VIC
- 5 Dobney Hypertension Centre, the University of Western Australia, Perth, WA
Data Sharing:
This article includes no original data.Received 5 December 2023, accepted 21 March 2024
Aletta Schutte is supported by a National Health and Medical Research Council Leadership Investigator Grant (2017504). Markus Schlaich has received consulting fees, or travel and research support from Medtronic, Abbott, Novartis, Servier, Pfizer, and Boehringer‐Ingelheim.
George Health Enterprises Pty Ltd, the social enterprise arm of the George Institute for Global Health, has received investment funding to develop fixed dose combination products containing aspirin, statin, and blood pressure‐lowering drugs. The George Institute holds and have filed applications for method of treatment and composition patents in relation to low and ultra‐low dose fixed dose combination products for the treatment of hypertension and diabetes on which Anthony Rodgers is listed as an inventor (granted: US 10 369 156; US 10 799 487; US 10 322 117; US 11 033 544; US 11 478 462; pending: US 17/932 982; US 18/446 268; US 17/598 122; US 17/317 614). Anthony Rodgers is seconded part‐time to George Medicines Pty Ltd, a subsidiary of George Health Enterprises. All staff employed by the George Institute have an institutional interest to declare with respect to George Health Enterprises; none have financial interests in these investments.
- 1. Hird TR, Zomer E, Owen AJ, et al. Productivity burden of hypertension in Australia: a life table modeling study. Hypertension 2019; 73: 777‐784.
- 2. Australian Institute of Health and Welfare. High blood pressure [web report]. 19 July 2019. https://www.aihw.gov.au/reports/risk‐factors/high‐blood‐pressure/contents/high‐blood‐pressure (viewed Feb 2024).
- 3. Roseleur J, Gonzalez‐Chica DA, Harvey G, et al. The cost of uncontrolled blood pressure in Australian general practice: a modelling study using electronic health records (MedicineInsight). Pharmacoeconomics 2023; 41: 573‐587.
- 4. NCD Risk Factor Collaboration. Long‐term and recent trends in hypertension awareness, treatment, and control in 12 high‐income countries: an analysis of 123 nationally representative surveys. Lancet 2019; 394: 639‐651.
- 5. Schutte AE, Jennings G, Schlaich MP. Uncontrolled blood pressure in Australia: a call to action. Med J Aust 2022; 216: 61‐63. https://www.mja.com.au/journal/2022/216/2/uncontrolled‐blood‐pressure‐australia‐call‐action
- 6. Schutte AE, Bennett B, Chow CK, et al. National Hypertension Taskforce of Australia: a roadmap to achieve 70% blood pressure control in Australia by 2030. Med J Aust 2024; 221: 126‐134. https://www.mja.com.au/journal/2024/221/3/national‐hypertension‐taskforce‐australia‐roadmap‐achieve‐70‐blood‐pressure
- 7. Services Australia. Pharmaceutical Benefits Schedule item reports. http://medicarestatistics.humanservices.gov.au/statistics/pbs_item.jsp (viewed Mar 2024).
- 8. Services Australia. Medicare item reports. http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp (viewed Mar 2024).
- 9. NPS MedicineWise. MedicineInsight: General practice insights report July 2016 – June 2017. A working paper. 2018. https://www.nps.org.au/assets/63df68106933b7b1‐100a108a779c‐GPIR‐2016_17_FinalVersion13‐Dec.pdf (viewed Mar 2024).
- 10. NPS MedicineWise. MedicineInsight: General practice insights report July 2020 – June 2021. 2022. https://www.nps.org.au/assets/NPS/pdf/Report‐2020‐21‐GPIR‐final.pdf (viewed Mar 2024).
- 11. Australian Department of Health and Aged Care. Seventh Community Pharmacy Agreement (7CPA). Updated 23 Feb 2022. Archived: https://webarchive.nla.gov.au/awa/20220603090820/https://www.pbs.gov.au/info/general/seventh‐community‐pharmacy‐agreement (viewed Feb 2024).
- 12. Australian Bureau of Statistics. Consumer price index, Australia, December quarter 2022. 25 Mar 2023. https://www.abs.gov.au/statistics/economy/price‐indexes‐and‐inflation/consumer‐price‐index‐australia/dec‐quarter‐2022 (viewed Feb 2024).
- 13. Australian Department of Health and Aged Care. Pharmaceutical benefits. Fees, patient contributions and safety net thresholds. Updated 23 Feb 2024. https:/www.pbs.gov.au/info/healthpro/explanatory‐notes/front/fee (viewed Feb 2024).
- 14. Australian Department of Health and Aged Care. PBS expenditure and prescriptions. Updated 22 Dec 2022. https://www.pbs.gov.au/info/statistics/expenditure‐prescriptions/pbs‐expenditure‐and‐prescriptions (viewed Feb 2024).
- 15. Husereau D, Drummond M, Augustovski F, et al; CHEERS 2022 ISPOR Good Research Practices Task Force. Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Int J Technol Assess Health Care 2022; 38: e13.
- 16. Australian Department of Health and Aged Care. Benefits and cost savings. Updated 23 Apr 2024. https://www.health.gov.au/cheaper‐medicines/benefits‐and‐cost‐savings (viewed Apr 2024).
- 17. Taitel M, Fensterheim L, Kirkham H, et al. Medication days’ supply, adherence, wastage, and cost among chronic patients in Medicaid. Medicare Medicaid Res Rev 2012; 2: mmrr.002.03.a04.
- 18. King S, Miani C, Exley J, et al. Impact of issuing longer‐versus shorter‐duration prescriptions: a systematic review. Br J Gen Pract 2018; 68: e286‐e292.
- 19. World Health Organization. Global report on hypertension: the race against a silent killer. 19 Sept 2023. https://www.who.int/publications/i/item/9789240081062 (viewed Feb 2024).
- 20. Nissen L, Kyle G, Cardiff L, et al. Pharmacist prescribing in Australia: an exploration of current pharmacist capabilities, required education and training to prescribe medicines and a process for moving forward. A report commissioned by the Pharmacy Board of Australia. Oct 2017. https://www.pharmacyboard.gov.au/documents/default.aspx?record=WD18%2f26419&dbid=AP&chksum=DvM%2fXysazPMCPbCSI6LNLw%3d%3d (viewed Feb 2024).
- 21. Paige E, Welsh J, Agostino J, et al. Socioeconomic variation in absolute cardiovascular disease risk and treatment in the Australian population. Prev Med 2018; 114: 217‐222.
- 22. Kemp A, Preen DB, Glover J, et al. Impact of cost of medicines for chronic conditions on low income households in Australia. J Health Serv Res Policy 2013; 18: 21‐27.
- 23. Hynd A, Roughead EE, Preen DB, et al. The impact of co‐payment increases on dispensings of government‐subsidised medicines in Australia. Pharmacoepidemiol Drug Saf 2008; 17: 1091‐1099.





Abstract
Objective: To quantify the costs of hypertension diagnosis and treatment in Australia, particularly in primary care, including general practices and pharmacies.
Study design: Economic analysis; analysis of Pharmaceutical Benefits Scheme (PBS) and Medicare Benefits Schedule (MBS) data.
Setting: Australia, 2012–22.
Main outcome measure: Estimated expenditure on hypertension care (adjusted to 2022 Australian dollars), overall and by expenditure type (general practice consultations, medications), cost bearer (PBS, MBS, patient out‐of‐pocket costs), and broad expenditure category (medication costs, pharmacy costs, general practice consultations, ambulatory blood pressure monitoring).
Results: During 2012–22, estimated total expenditure for the diagnosis and treatment of hypertension in Australia was $12.2 billion: $7.3 billion (60%) was borne by the MBS and PBS, $4.9 billion (40%) by patients as out‐of‐pocket costs. During 2021–22, an estimated $1.2 billion was spent on the management of hypertension; the three main cost components were pharmacy‐related costs (administration and handling fees, dispensing fees, electronic prescription fees: $611.1 million, 50.8%), general practice consultations ($342.7 million, 28.5%), and blood pressure‐lowering medications (manufacturer and wholesale costs: $244.3 million, 20.3%).
Conclusions: During 2012–22, about 40% of the cost of managing hypertension in Australia was borne directly by patients (about $494 million per year). Important changes to pharmacy supply and payment policies were introduced in 2023, but further efforts may be needed to reduce treatment costs for patients. These changes are particularly important if the hypertension control rate is to be substantially improved in Australia, given the large numbers of undertreated and untreated people with hypertension.