The elimination of health disparities, as disproportionately experienced by Aboriginal and Torres Strait Islander peoples, is a central tenet of the Australian health policy landscape.1 Social and cultural determinants of health1,2,3 are patient‐important factors for many families and communities accessing health support for dialysis‐requiring kidney failure in the Northern Territory (NT). The NT has a dispersed population of 228 822 people, of whom nearly 27% identify as Aboriginal and/or Torres Strait Islander, with a majority who live in very remote NT communities.4,5 An estimated 85% of dialysis‐dependent Territorians identify as Aboriginal and/or Torres Strait Islander,6 and relocating to access dialysis treatment is a disparate health outcome not usually experienced by non‐Indigenous Territorians. As well as physical dislocation, this has included social, cultural and emotional hardship.7 In combination, slowing progression of kidney disease, sustaining residual kidney function that permits health and results in a safe delay of dialysis initiation, and promoting access to self‐care dialysis and transplantation are profoundly important health outcomes.4 Reporting the attainment of patient‐preferred outcomes not only validates care processes but also asserts health sovereignty for Aboriginal and Torres Strait Islander people. When these care principles are adopted as standard practice, there is an optimistic expectation of reducing health disparities.
Method
This lessons from practice article combines scientific reporting with Storying, focusing on a model of care whose principles (Box 1) prioritised Indigenous health ethics and strived to attain patient‐driven outcomes within the context of late‐stage chronic kidney disease (CKD). The case reporting spanned six years and, once described, was presented to the patient, who advocated for inclusion of her expert explanation. We prepared five guiding questions that assisted the reporting using Storying methodology.
The Storying questions were:
- What were the main ways you cared for yourself in your health journey [since you first knew you had low kidney function]?
- [Since that time], how did you bring your Indigenous knowledge of health into your own self‐care practices?
- How important to you was the extended time you experienced before you needed to start dialysis?
- In your own health journey, what challenges do you want to share with readers (eg, clinician or family). Why were those challenges selected?
- Please include one or two other stories you want to share about your kidney care health journey.
Using a face‐to‐face interview, the oral Storying was facilitated between the patient and the Aboriginal and Torres Strait Islander Renal Specialist Health Practitioner involved in her care. So the patient's Story can be relatable and useful to others (in this published form), we used the term Ipeka, which in Mabuyag dialect of KalalagawYa language of western Torres Strait means “woman”. The use of Storying intentionally positioned the patient as expert and leader in her care journey and mitigates bias in meaning since Ipeka is the teller and knower of this Story. Storying is a profound, enduring and reliable method of knowledge collation and archiving inherent in Aboriginal and Torres Strait Islander cultures, honouring their expertise in recounting personal and collective experiences for the preservation and dissemination of knowledge.8,9 Within a health reporting context, Storying as method amplifies marginalised voices and serves as an educational tool for receptive audiences, including health care providers and other Aboriginal and Torres Strait Islander people (patient, family, clinicians) navigating comparable health care journeys8,9 (Supporting Information, appendix 1). We have confirmed the five questions as suitable for collaborative reflection for herself, her family and clinical team. Contextualising excerpts are included in the health journey, as quotes, acknowledging Ipeka's maintained authority and control of her information, and respect for her Indigenous knowledge and data rights.
The patient consented to the written description of her health journey in this form, in addition to approval by the Human Research Ethics Committee of the Northern Territory Department of Health and Menzies School of Health Research (reference number 2022–4232).
Positionality statement
The authors include the patient herself (Miss Luta), an elder of the Kaurareg nation, and the clinicians who provided her renal specialty health care support. Naidu, a medical registrar, of Indian heritage, received mentorship from First Nation clinicians Paolucci and Hughes. Paolucci, an Aboriginal and Torres Strait Islander woman, provided support as the Aboriginal and Torres Strait Islander Health Practitioner. Hughes, a Koike of Medicine of Wagadagam tribe, a Torres Strait Islander woman, and a senior specialist nephrologist, supervised the clinical care for the patient within the multidisciplinary clinical team.
The health journey
We describe a six‐year health journey, commencing in 2017, of Ipeka, a 58‐year‐old Torres Strait Islander woman living and working in remote NT. She was first diagnosed in 2017 with advanced CKD and continued with community‐based health care and employed for five years before starting chronic maintenance haemodialysis, and then achieving self‐ and family‐supported home‐haemodialysis.
Clinical care continuity and respecting self‐determination in patient decision making
In 2017, Ipeka experienced visual changes and headaches, and an urgent health assessment revealed hypertensive emergency with encephalopathy. She was transferred to the tertiary hospital and commenced multi‐agent antihypertensive therapy with stabilisation of blood pressure and resolution of encephalopathy. An initial elevated serum creatinine recorded on presentation (609 μmol/L; reference interval, 45–90 μmol/L) persisted after discharge, and radiological and other biochemical features confirmed stage 5 CKD. Causes of rapidly progressive glomerulonephritis were excluded, and Ipeka disclosed a hypertension diagnosis a decade earlier with no primary health care involvement or antihypertensive therapy for two years, and two first‐degree relatives who had hypertensive nephropathy. She established a health care relationship with the tertiary hospital team, and a primary health care team in the same city, before returning to her remote community to resume work. Information and education about antihypertensive therapy, living with advanced CKD including dialysis, dialysis access preparation, and preferred modality were shared by the nephrology team, and Ipeka engaged her family and community in planning her late‐stage CKD care.
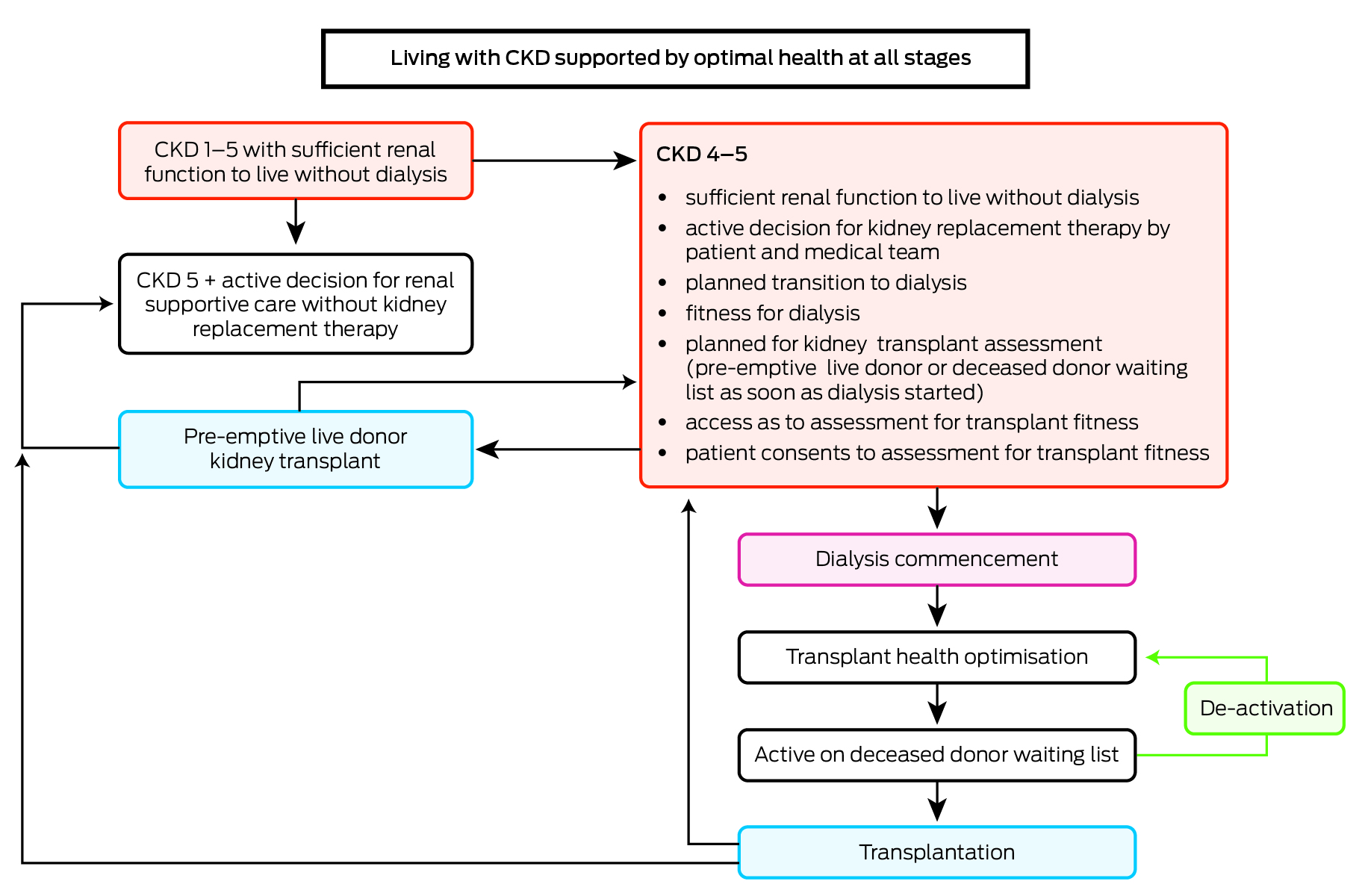
Ipeka's goal was to live within and remain employed in her remote community with every home‐based kidney replacement therapy available to her. She selected peritoneal dialysis, since she previously supported her late brother and father in that treatment. Ipeka proceeded to prepare a backup arteriovenous fistula, and, as no family donor for kidney transplant was identified, Ipeka progressed through the local protocol for waitlisting on the deceased donor kidney transplantation list (Box 1).10
For the next five years, Ipeka received care continuity from her remote primary health care medical officer (who led community‐based care) and her nephrologist and multidisciplinary Renal Home Therapy Unit team. The unit's role was to support clients with advanced CKD, emphasising dialysis planning and transplant suitability assessments through telehealth and in‐person reviews, involving a consultant nephrologist, CKD nurse coordinator, other specialised nurses, occupational therapist, physiotherapist, dietitian, and an Aboriginal Liaison Officer, and a dedicated transport service supporting patients to participate in health‐planning appointments.11 Ipeka attended monthly kidney function tests at her remote primary health clinic, and quarterly in‐person or telehealth specialist renal reviews. A shared understanding that initiation of maintenance dialysis was expected once she developed kidney failure coinciding with persistent uraemic symptoms that could no longer be medically managed. Ipeka learned about and understood the international renal palliative outcomes scale symptoms checklist and could express her symptom rating during clinical reviews. Close collaboration between local and specialist care providers allowed for timely escalation of concerns and prompt transplantation workup. Renal specialty prescriptions were also completed at the unit and dispatched from the central dispensing pharmacy to her local health service. Ipeka was periodically invited to the renal unit for ongoing informed consent discussions related to peritoneal dialysis, surgical placement of the peritoneal dialysis catheter, and assessments for kidney transplant suitability.
Integration of traditional healing and the biomedical approach
When asked about traditional healing practices and bush medicines used to look after herself, Ipeka stated:
Just only the obo [fruit] one. The old people used to tell us it's a good medicine for any sicknesses. Taking that every day made me come this far. Every night before bed and wake up every day before I go to work … Only when I started learning about my condition, [I] found out that [obo fruit] and now I feel really close to it (that medicine) (laughing). After … they sent me in [to the tertiary hospital] and then going back [to community], it was like I didn't have a kidney problem. I just went about my normal day, going to work. I didn't think I had the problem. I would never have the problem. I think that bush tucker made me keep going for how many years maybe three years or four years. My kidney was stable for that long. I thought my kidney would give away, but it took me this long til I came in to start my [dialysis] training.
This quote demonstrates that advanced CKD can have no external symptoms, and, for Ipeka, the combination of obo fruit with biomedical therapy advised by her health teams was effective for many years.
Holistic and high value care
Following the first year of stabilised health, in‐person review was organised by the renal home therapies team to ensure preference for peritoneal dialysis and confirm ongoing informed consent and waitlisting for peritoneal dialysis catheter insertion. Those visits were opportune for annual review of health, maintaining relationships between renal home therapies staff, Ipeka and family support persons, and recency of investigations for transplant suitability. Early in year 5, Ipeka was observed to have reduced mobility and exercise tolerance due to chronic lower back pain. A renal physiotherapy assessment, co‐located at the renal home therapies unit,12 confirmed chronic lumbar back pain and functional impairment within her daily living activities. We considered this a potential obstacle to peritoneal dialysis, which requires lifting and moving two‐litre dialysate bags, and the ability to tolerate increased intra‐abdominal pressure from dialysis fluid itself. A computed tomography (CT) scan revealed the presence of multilevel facet joint arthropathy with nerve impingement.
Pain management included physiotherapy‐guided home exercises and avoidance of prolonged sitting periods by scheduling more frequent movement activity in daily home and work life. While Ipeka preferred simple analgesia, we avoided non‐steroidal anti‐inflammatory analgesics as they are contraindicated in CKD,13 and avoided opioids as toxic metabolite accumulation occurs in very low kidney function, and chronic constipation may have an impact on future peritoneal dialysis exchanges. We considered radiofrequency nerve ablation due to its similar risk profile to corticosteroid‐guided injections but far superior analgesic effect, with some studies showing 50% or more reduction in pain up to 24 months after a single treatment.13,14,15 Studies reported better analgesic response for patients of older age who had increased severity of degenerative change.15 Radiofrequency nerve ablation was only locally available as a private paying patient in a private hospital; the public hospital provided approval to cover out‐of‐pocket costs based on it being a medically recommended procedure to aid analgesia and functional improvement, patient‐preferred care, and Care Close to Home using peritoneal dialysis. However, in the interim, Ipeka experienced lessening in pain intensity and improvement in functional ability from incorporating the physiotherapy‐directed exercise and movement program into her daily life. She was therefore confident to decline invasive procedures which were recommended to multiple nerve roots and removed any challenges of health‐related remote travel and interruptions to her work schedules.
Timely intervention for arteriovenous fistula complications and dialysis commencement
Late in year 5, Ipeka noticed reduced blood flow in her arteriovenous fistula during routine self‐assessment suggestive of thrombus. Promptly seeking help at the local health care clinic, she was transferred to the tertiary hospital and obtained a same‐day outpatient nephrology‐delivered percutaneous intervention, which prevented fistula occlusion. This was the third hospitalisation in five years since her hypertensive nephropathy diagnosis in 2017 (the second being same‐day surgical procedure for arteriovenous fistula creation).
Also in year 5, a sustained increase in serum creatinine from previous stable baseline was noted along with increasing uraemic symptoms self‐identified by Ipeka. She agreed to insertion of the peritoneal dialysis catheter and commencement of peritoneal dialysis. Escalated antihypertensives and diuretics were deprescribed as no longer needed with achieved euvolemia. Starting self‐care with continuous ambulatory peritoneal dialysis marked a significant milestone in managing advanced CKD. Ipeka was referred to the visiting specialist transplant service who recommended waitlisting for transplantation, pending assessment and treatment, if needed, for latent tuberculosis, and reduction in excess iliac fossa skinfold overlying the proposed transplant site, as this would predispose to wound dehiscence and related complications. Subsequently, she was referred to a multidisciplinary obesity clinic and plastics surgery team, with apronectomy recommended to address these concerns.
Complications requiring cessation of peritoneal dialysis
Four weeks after commencing peritoneal dialysis, and prior to returning home to her remote community, Ipeka developed escalating dyspnoea and presented to emergency care where a pleural effusion was identified, indicating a peritoneal pleural defect. This is a rare complication of peritoneal dialysis occurring in less than 2% of patients.16 Diagnostic efforts included an inconclusive CT scan with contrast in the dialysate. Ipeka took a four‐week hiatus from peritoneal dialysis, during which she remained well and did not require interval haemodialysis. Peritoneal dialysis was retrialled with the same result and, thus, was discontinued. If the pleuroperitoneal defect does not self‐heal after a period of rest, options include pleurodesis or attempted repair of the defect.16 As Ipeka preferred to avoid invasive intervention and pleurodesis may have compromised lung function critical for anaesthetic safety for transplant, we agreed to recommence with haemodialysis once uraemic symptoms returned. She returned to her home community, living well and rejoining integrative community‐based care for another 12 months, when her uraemic symptoms intensified and intermittent maintenance haemodialysis via her arteriovenous fistula was commenced. She gained access to home haemodialysis training within six weeks, and Ipeka reflected on this modality change in terms of her family:
I thought that well this [peritoneal dialysis] was not working so I'm going to die, yeah. But that day Dr brought me in, told me about haemo[dialysis] at home; I thought there are other ways [now available to me]. Cause I am thinking about my Dad and my brother — they didn't make it. I thought the same would happen for me.
The first thing I thought about was my kids and grannies. I want to see my grannies, I want to see them graduate and turn 18, 21 (tearing up). I am doing this for them, my children and grandchildren. So, I am taking this journey for the transplant so I can be a bit longer with them. I am taking all these tests and now I have to do tests for my tummy, surgery with my tummy, I think that's the last one, then they can put me on the list, so I am going to do that.
Knowledge and support that enables patient independence
In the face of changing dialysis modalities and navigating unforeseen complications, the multidisciplinary team actively supported Ipeka's desire to sustain employment and reside within her community. The team prioritised Ipeka's learning needs, which was crucial to her decision making, and facilitated timely access to home haemodialysis training to ensure Ipeka's return home. Furthermore, the team supplied medical letters, certificates, and guidance on job training, demonstrating a commitment to the overarching objective of patient‐centred care closer to home.
My dad and brother both had kidney problems. But I didn't know how and what to do when you have that disease until I did the training now. I am doing the (home dialysis) training now and I know how important it is to do these things now.
Reflection
This case report illustrates a model of care grounded in Indigenous health ethics principles that emphasises the Aboriginal definition of health that encompasses individual and collective cultural, social and environmental wellbeing beyond the absence of illness.17 Achieving health requires acknowledging and addressing social and cultural determinants of health, environmental health, and health care access which have an impact on health outcomes independent of biomedical risk factors.18,19,20 Cultural determinants of health include Indigenous knowledge and Indigenous medicine, language, kinship, expression of culture (such as Storying), and autonomy, and access to and living on Country.19,20,21 A determinants‐informed health care model uses a strengths‐based approach, moving away from the historical colonisation context of undermining Indigenous culture and individual victim blaming for poor health outcomes.18,19,20,21,22,23 This can be seen in our model of care, where by prioritising care closer to home and respecting the significance of family and community participation, trust was fostered, leading to positive health outcomes and broader impacts of Ipeka's ongoing presence in her community and family.21,22 The impact of this model of care is summarised in Box 2 and extrapolated further below.
Self‐determination in health care decision making
Indigenous self‐determination was upheld in this model of care. As per the United Nations Declaration on the Rights of Indigenous Peoples,24,25 “Indigenous peoples have the right to self‐determination. By virtue of that right they freely determine their political status and freely pursue their economic, social and cultural development”. Moreover, Article 4 of the Declaration24,25 emphasises that Indigenous peoples, while exercising their right to self‐determination, possess the entitlement to autonomy or self‐government in matters concerning their internal and local affairs. Self‐determination requires Indigenous input at every stage of decision making, which ensures they are the leaders in their care.22
Ipeka was an active leader in proactive health‐maintaining care, avoided unplanned acute dialysis initiation, and was supported to make informed decisions aligned with her health care goals. Those decisions encompassed pivotal care milestones, such as sustaining employment, maintaining life participation for herself and her family, determining dialysis commencement dates, and prioritising home dialysis and transplantation as primary objectives. Notably, when the rare complication of pleuroperitoneal defect arose, the commitment to community‐based dialysis guided management to home haemodialysis training, where proactive outpatient follow‐up facilitated the formation of an arteriovenous fistula over a year before the commencement of dialysis, ensuring ready access once needed.
Culturally safe practice and collaborative care
The model of care established an environment wherein the patient actively determined her own culturally safe boundaries. Central to cultural safety is acknowledging the ongoing impact of colonisation on Indigenous health outcomes and striving to minimise or rebalance power gradients in favour of health care recipients.18,26 This is achieved by implementing principles such as self‐determination, leadership, mutual respect, inclusivity, and recognition of Indigenous health principles.26 This clinic achieved this by establishing links with the patient's local community health provider, where the patient already had a therapeutic relationship, and utilising tools such as telehealth to minimise disruption to Ipeka's life. The NT health network uses telemedicine to provide outpatient care in the face of vast geographical distance, extreme weather conditions, and socio‐economic barriers that affect regular health‐related travel. Primary health care providers in the community are equipped with telehealth equipment and nurses and Aboriginal health workers to support clinics, which eliminates the need for individual patient access to infrastructure and ensures handover of patient management to the primary care provider.
Cultural respect was again shown through the use of medical pluralism, or the integrated use of both Indigenous healing practices and western medicines.27 Indigenous people, as highlighted in a Canadian study by Auger and colleagues,27 find ease in accessing traditional health care, empowering them to seek other health care types, including western medicine, as is seen in this health journey.27
A reflection from a health appointment, accompanied by the health practitioner whose role was to assist, if required, with treatment explanations and advocacy, underscored Ipeka's experience of living with fear within medical consultations, and subsequent relief.
At first, I was scared about the questions I was going to ask and the answers [the doctor] would give me. Now [that the appointment is completed], I feel okay. It's all for my kids, myself, and my grandchildren.
Ipeka expressed her apprehension, “Visiting doctors is always the frightening bit,” citing challenges when medical language is used for decisions, despite her proficient command of English. Notably, the familiarity with her doctor, who is a Torres Strait doctor, provided a level of comfort and underscored the significance of a cultural‐knowing and culturally capable health care provision by Torres Strait Islander and Aboriginal health care professionals within the multidisciplinary team.
An instruction for willing learners
Just to stay healthy and do the right thing to eat the right food and just to take your medication and find out if you have that sickness (high blood pressure). And back home there in Badu [island, Torres Strait] it would be good to build a health/renal health and education building back there … for family down here [in the mainland] … to go back for family gatherings and events. We need a renal building so that we can go back.
Families back home get to know the Drs. But also, for our people [to] be Drs, nurses, health practitioners and renal nurses. Get the younger ones to train, so they will stay on the islands and then we will have our own Dr and nurses, who won't leave.
Conclusion
This lessons from practice article demonstrates effectively integrated Indigenous self‐determination, cultural safety, and patient‐centricity within health care allowing for achievement of patient‐preferred health care outcomes, and was aligned with local health policy to support Care Close to Home.4,5 Storying revealed an expressed need for dialysis access in very remote Australia, and high value of fostering a clinically proficient and culturally respectful health care environment.
Lessons from practice
- Torres Strait Islander and Aboriginal people of Australia face health disparities, notably in chronic kidney disease (CKD) outcomes.
- This article reveals a care model rooted in Indigenous health ethics and showcases significant positive outcomes over a sustained period of time consequent of the CKD management approach. By prioritising culturally safe health care, Indigenous self‐determination, and acknowledging sociocultural determinants of health, the model advances health outcomes and positions this care model as a new standard of health care delivery.
- Emphasising culturally sensitive care and patient autonomy within clinical care, this model underscores pathways to enhance health outcomes for Indigenous communities. It urges sustained support for Indigenous self‐determination in achieving health care equity, and the cultivation of a diverse health care workforce to address Indigenous health needs comprehensively.
Box 2 – Summary of achieved health outcomes and contributing care attributes
|
|
Clinical services |
Patient involved in care |
|||||||||||||
|
|
|||||||||||||||
|
Achieved health outcomes |
|
|
|||||||||||||
|
Care attributes |
|
|
|||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
- 1. Zhao Y, You J, Wright J, et al. Health inequity in the Northern Territory, Australia. Int J Equity Health 2013; 12: 79.
- 2. Yashadhana A, Fields T, Burnett A, Zwi AB. Re‐examining the gap: a critical realist analysis of eye health inequity among Aboriginal and Torres Strait Islander Australians. Soc Sci Med 2021; 284: 114‐230.
- 3. Marmot M; Commission on Social Determinants of Health. Achieving health equity: from root causes to fair outcomes. Lancet 2007; 370: 1153‐1163.
- 4. Department of Health Strategy, Policy and Planning Branch. Northern Territory health strategic plan 2018–2022. Darwin: Northern Territory Department of Health, 2018. https://digitallibrary.health.nt.gov.au/entities/publication/173bf4fb‐c8fb‐428c‐986f‐f09ca3bf1cf1/details (viewed Jan 2022).
- 5. Chondur R, Guthridge S. Health gains planning — fact sheet: Northern Territory demography. Darwin: Northern Territory Department of Health, 2015. https://digitallibrary.health.nt.gov.au/nthealthserver/api/core/bitstreams/a800c5fe‐797f‐4b07‐9d6f‐a51222fa1668/content (viewed Jan 2022).
- 6. Gorham G, Majoni S, Lawton P, et al. Interesting times — evolution of dialysis in Australia's Northern Territory (1980–2014). Renal Society of Australasia Journal 2018; 14: 108‐116.
- 7. Hughes JT, Freeman N, Beaton B, et al. My experiences with kidney care: a qualitative study of adults in the Northern Territory of Australia living with chronic kidney disease, dialysis and transplantation. PLoS One 2019; 14: e0225722.
- 8. Phillips L, Bunda T. Research through, with and as storying, 1st ed. Abingdon (UK): Routledge, 2018.
- 9. Tunnicliffe DJ, Bateman S, Arnold‐Chamney M, et al. Recommendations for culturally safe clinical kidney care for First Nations Australians: a guideline summary. Med J Aust 2023; 219: 374‐385. https://www.mja.com.au/journal/2023/219/8/recommendations‐culturally‐safe‐clinical‐kidney‐care‐first‐nations‐australians
- 10. Majoni SW, Dole K, Hughes JT, Pain C. Review of current pathways to wait‐listing for kidney transplantation for Aboriginal and Torres Strait Islander peoples with end‐stage kidney disease in the Top End of Northern Australia. Aust Health Rev 2021; 45: 185‐193.
- 11. Zabeen S, Eades A‐M, Paolucci O, et al. Evaluation of an innovative Live Strong COVID‐mitigating healthcare delivery for adults after starting dialysis in the Northern Territory: a qualitative study. Lowitja Journal 2023; 1; https://doi.org/10.1016/j.fnhli.2023.100001.
- 12. Modderman R, Paolucci O, Zabeen S, et al. Physiotherapy‐led restorative care enabling improved frailty measures in adults after starting dialysis in Northern Territory of Australia: the “Frailty‐to‐Fit” pilot study. Lowitja Journal 2024; https://doi.org/10.1016/j.fnhli.2024.100020.
- 13. Hashemi M, Hashemian M, Mohajerani SA, Sharifi G. Effect of pulsed radiofrequency in treatment of facet‐joint origin back pain in patients with degenerative spondylolisthesis. Eur Spine J 2014; 23: 1927‐1932.
- 14. Perolat R, Kastler A, Nicot B, et al. Facet joint syndrome: from diagnosis to interventional management. Insights Imaging 2018; 9: 773‐789.
- 15. Conger A, Burnham T, Salazar F, et al. The effectiveness of radiofrequency ablation of medial branch nerves for chronic lumbar facet joint syndrome in patients selected by guideline‐concordant dual comparative medial branch blocks. Pain Med 2020; 21: 902‐909.
- 16. Puri V, Orellana FA, Singer GG, Wald MS. Diaphragmatic defect complicating peritoneal dialysis. Ann Thorac Surg 2011; 92: 1527.
- 17. Australian Institute of Health and Welfare. Australia's health 2018 (Cat. No. AUS 221). Canberra: AIHW, 2018. https://www.aihw.gov.au/getmedia/7c42913d‐295f‐4bc9‐9c24‐4e44eff4a04a/aihw‐aus‐221.pdf?v=20230605094401&inline=true (viewed Apr 2024).
- 18. Cooper D. Closing the gap in cultural understanding: social determinants of health in Indigenous policy in Australia. Darwin: Aboriginal Medical Services Alliance of the Northern Territory, 2001. https://healthinfonet.ecu.edu.au/key‐resources/policies‐and‐strategies/23289/?title=Closing+the+gap+in+cultural+understanding++social+determinants+of+health+in+Indigenous+policy+in+Australia&contentid=23289_1 (viewed Apr 2024).
- 19. Dockery AM. Culture and wellbeing: the case of Indigenous Australians. Perth: Centre for Labour Market Research, Curtin University of Technology, 2009. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=1351633 (viewed Apr 2024).
- 20. Olson R, Mutch A, Fitzgerald L, Hickey S. The social and cultural determinants of health. In: Dune T, McLeod K, Williams R; editors. Culture, diversity and health in Australia: towards culturally safe health care, 1st ed. United Kingdom: Routledge, 2021; pp15‐35.
- 21. Dudgeon P, Blustein S, Bray A, et al. Connection between family, kinship and social and emotional wellbeing [Cat. No. IMH 4]. Canberra: Australian Institute of Health and Welfare, 2021. https://www.indigenousmhspc.gov.au/getattachment/e129c621‐58a4‐4966‐8730‐dcf6e3a533a8/dudgeon‐et‐al‐2021‐family‐kinship.pdf?v=1071 (viewed Apr 2024).
- 22. Verbunt E, Luke J, Paradies Y, et al. Cultural determinants of health for Aboriginal and Torres Strait Islander people — a narrative overview of reviews. Int J Equity Health 2021; 20: 181‐190.
- 23. Dudgeon P, Milroy H, Walker R. Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. Canberra: Commonwealth of Australia, 2014. https://www.telethonkids.org.au/globalassets/media/documents/aboriginal‐health/working‐together‐second‐edition/working‐together‐aboriginal‐and‐wellbeing‐2014.pdf (viewed Apr 2024).
- 24. Roach P, McMillan F. Reconciliation and Indigenous self‐determination in health research: a call to action. PLOS Glob Public Health 2022; 2: e0000999.
- 25. United Nations General Assembly. Declaration on the Rights of Indigenous Peoples. New York: UN, 2007. https://www.un.org/development/desa/indigenouspeoples/wp‐content/uploads/sites/19/2018/11/UNDRIP_E_web.pdf (viewed Jan 2022).
- 26. Smye V, Josewski V, Kendall E. Cultural safety: an overview. Ottawa: Mental Health Commission of Canada, 2010. https://mdsc.ca/documents/Publications/CULTURAL%20SAFETY%20AN%20OVERVIEW%20(draft%20mar%202010).pdf (viewed Jan 2022).
- 27. Auger M, Howell T, Gomes T. Moving toward holistic wellness, empowerment and self‐determination for Indigenous peoples in Canada: Can traditional Indigenous health care practices increase ownership over health and health care decisions? Can J Public Health 2016; 107: e393‐e398.






Open access:
Open access publishing facilitated by Flinders University, as part of the Wiley – Flinders University agreement via the Council of Australian University Librarians.
Jaquelyne Hughes holds an Australian National Health and Medical Research Council Emerging Leaders Fellowship (#1174758). We acknowledge the clinical staff of Top End Renal Service Renal Home Therapy Unit for their role in delivering patient care in partnership with the patient, family, and primary care, summarised in this health journey. We also thank Professor Simone Ulalka Tur for her advice on the Storying method. We acknowledge the Indigenous knowledges of Aboriginal and Torres Strait Islander peoples that informed this work and cited herein: 7–12 and 21–25.
No relevant disclosures.