The known: Dysmenorrhea (menstrual pain) affects an estimated 70.8% of young women around the world.
The new: In our longitudinal survey study, about 35% of 14‐year‐old participants had experienced painful periods, as had about 50% when they were surveyed at ages 16 and 18 years. Dysmenorrhea was associated with missing more activities (school, work, social, sport and exercise) during periods. Adolescent girls with dysmenorrhea were three to five times as likely as those without dysmenorrhea to miss school or university.
The implications: The early identification and treatment of dysmenorrhea is important for improving quality of life and reducing school and work absenteeism among adolescents.
Menstrual pain (dysmenorrhea) affects an estimated 70.8% of adolescent girls and young women aged 13–23 years;1 in Australia, it has been reported by 80–93% of those aged 13–25 years.2,3,4,5 Despite the high prevalence, young people who experience dysmenorrhea feel that talking about periods and period pain is stigmatised.6 Women with dysmenorrhea report that their pain is often not considered a legitimate health problem by health care providers or the general community.7 The consequences of dysmenorrhea include more frequent absences from school and work,8 and the likelihood of being diagnosed with endometriosis is greater for women who experienced dysmenorrhea during adolescence.9
Adolescents who experience dysmenorrhea are more likely than those who do not to miss school, their classroom performance is impaired, and they report that pain interferes with social events, sport, and exercise.1,10 The prevalence of menstrual pain and its impact on the school attendance and other activities of Australian adolescents has not been investigated at the population level, nor their experience of period pain over time. In our prospective, population‐based cohort study we assessed the proportion of female adolescents who experience menstrual pain and chronic menstrual pain at ages 14, 16, and 18 years. We also examined associations of dysmenorrhea and period pain severity with adolescents missing regular activities because of their periods.
Methods
The Longitudinal Study of Australian Children (LSAC) has tracked the development and life course trajectories of two nationally representative cross‐sequential samples of Australian children since 2004: the Birth (5107 children aged 0–12 months at enrolment) and Kinder cohorts (4983 children aged 4–5 years at enrolment). Data were collected every two years; nine waves of data had been collected by the end of 2023. The LSAC study design and participant recruitment were described in detail elsewhere.11
For this article, we analysed longitudinal survey data collected during 2014–2018 for Kinder cohort participants at waves 6 (mean age 14 years), 7 (16 years), and 8 (18 years). Surveys at each of these waves included questions about puberty and menstruation. We report our observational study in accordance with the STROBE guidelines.12
Demographic data
The demographic data collected from LSAC participants and their parents at each wave included age, Indigenous status, employment status, and school attendance. Data collection involved interviews; participants and their parents were interviewed together at waves 6 and 7 and separately at wave 8. Socio‐economic status was defined according to the Index of Relative Socio‐economic Advantage and Disadvantage (IRSAD),13 based on the residential postcode of the family (waves 6, 7), or the participant (wave 8).
Survey questions related to menstruation
Participants who indicated that their biological sex was female were asked about menstruation and menstrual pain. They were asked about their menstrual cycles during the preceding three months at waves 6, 7, and 8, including about the regularity of their periods (regular [responses: very, quite] or irregular [a little, not at all]). Participants who reported sexual activity were asked about the method of contraception they used. The LSAC questionnaire did not assess oral contraceptive use for other purposes, such as managing period pain.
Participants were asked to rate their experience of periods during the preceding three months as very, quite, a little, or not at all painful. The proportions of respondents who reported dysmenorrhea (responses: very, or quite painful) or no dysmenorrhea (a little, or not at all painful) were calculated for each wave.
Respondents were asked whether they had missed school or university, work (waves 7, 8 only), social activities, or sport or exercise in the past three months because of their periods (not necessarily because of period pain), and also specifically whether they had not missed any of these activities during the preceding three months (waves 7, 8 only; not missing any activities was deduced for wave 6 from other responses).
Statistical analysis
Analyses were undertaken in Stata 17. Categorical variables are summarised as frequencies and proportions, continuous variables as means with 95% confidence intervals (CIs). The relationship between period pain severity and use of the oral contraceptive pill was assessed in a χ2 test of independence. Associations between dysmenorrhea and missed activities at each wave were assessed in binomial logistic regression analyses adjusted for socio‐economic status and dysmenorrhea status at each of the earlier study waves included in this analysis (eg, the analysis of missed activity at wave 7 was adjusted for dysmenorrhea reported at wave 6). We report adjusted odds ratios (aORs) with 95% CIs. P < 0.01 was deemed statistically significant because of the number of analyses.
Estimated prevalence was adjusted for sample attrition and non‐response using the relevant sample weight for the cohort at each wave. Missing data were typically attributable to participants not participating in a particular wave or not responding to certain questions; no pattern of missing data was detected.
Ethics approval
The Longitudinal Study of Australian Children was approved by the Australian Institute of Family Studies Ethics Committee (13‐04, 15‐01, 17‐01).
Results
Of the 1835 female members of the LSAC Kinder cohort who participated during at least one of waves 6 to 8 of the study, 1600 (87%) responded to questions about puberty and menstruation during at least one of waves 6 to 8 (Box 1). At wave 6, 183 of 644 participants did not have regular periods (28%; 95% CI, 25–32%), 290 of 1339 participants (22%; 95% CI, 20–24%) at wave 7, and 240 of 1117 participants (22%; 95% CI, 20–24%) at wave 8.
Of the participants who reported sexual activity and responded to the question about whether they used oral contraception, 14 of 57 (25%) said they did at wave 6, 186 of (45%) at wave 7, and 465 of 192 (59%) at wave 8.
Prevalence of menstrual pain
Dysmenorrhea was reported by 227 of 644 respondents at wave 6 (35%; 95% CI, 30–37%), 675 of 1341 (50%; 95% CI, 46–52%) at wave 7, and 518 of 1115 (46%; 95% CI, 42–48%) at wave 8 (Box 2). Among Aboriginal or Torres Strait Islander participants, four of fifteen (27%) at wave 6, 13 of 29 (45%) at wave 7, and 12 of 28 (43%) at wave 8 reported dysmenorrhea.
Very painful periods were reported by 79 of 644 participants (12%) at wave 6, 307 of 1341 (23%) at wave 7, and 203 of 1115 (18%) at wave 8. Quite painful periods were reported by 148 participants (23%) at wave 6, 369 (28%) at wave 7, and 315 (28%) at wave 8. Conversely, periods that were not at all painful were reported by 196 participants at wave 6 (3%), 198 (15%) at wave 7, and 158 (14%) at wave 8; periods that were a little painful were reported by 221 participants (34%) at wave 6, 468 (35%) at wave 7, and 439 (39%) at wave 8 (Box 2).
No significant associations between oral contraceptive pill use and period pain severity were detected at any wave (Supporting Information, table 1).
Chronic menstrual pain
Of the 366 participants who reported period pain severity at all three waves, 137 reported no dysmenorrhea at all three waves (37%) and 66 reported dysmenorrhea at all three waves (18%). Eighty‐nine respondents reported increasing period pain over time (24%), and 38 declining pain over time (10%) (Supporting Information, figure 1).
Activities missed because of periods
At wave 6, 223 of 647 participants reported missing at least one activity because of their periods (34%), 454 of 1341 at wave 7 (34%), and 344 of 1111 at wave 8 (31%). At wave 6, 115 participants reported missing school (18%), 293 at wave 7 (22%), and 154 at wave 8 (14%). At wave 7, 67 participants reported missing work (5%), and 101 at wave 8 (9%). At wave 6, 123 participants reported missing social activities (19%), 168 at wave 7 (13%), and 173 at wave 8 (16%); 148 participants reported missing sport or exercise activities at wave 6 (23%), 151 at wave 7 (11%), and 170 at wave 8 (15%) (Box 3).
The distribution of the number of activity types missed differed by period pain severity; in each wave, the distribution was shifted to the right (more activity types missed) as the degree of period pain increased (Supporting Information, tables 2–4). In adjusted binomial logistics regression analyses, respondents who reported dysmenorrhea were more likely than those who did not to miss school or university, social activities, and sport or exercise (Box 4).
Of the respondents who missed school because of their periods, 75 of 114 (65%) reported dysmenorrhea at wave 6, 229 of 293 at wave 7 (78%), and 117 of 154 at wave 8 (76%). Of the respondents who missed social activities because of their periods, 66 of 121 reported dysmenorrhea at wave 6 (55%), 138 of 168 at wave 7 (82%), and 141 of 173 at wave 8 (81%). Of the respondents who missed sport or exercise because of their periods, 77 of 146 reported dysmenorrhea at wave 6 (53%), 104 of 150 at wave 7 (69%), and 118 of 171 at wave 8 (69%). Of the respondents who missed work because of their periods, 56 of 67 reported dysmenorrhea at wave 7 (84%), and 88 of 101 at wave 8 (87%) (Box 5).
For all waves, the proportion of participants who reported not missing any activities because of period pain declined with increasing period pain severity, and the proportions reporting one or more missed activities increased. Of the participants who experienced very painful periods, 72% (wave 6), 63% (wave 7), and 65% (wave 8) missed at least one activity type because of their periods, as did 45% (wave 6), 36% (wave 7), and 40% (wave 8) of those who experienced quite painful periods (Box 6).
Discussion
We found that a large proportion of Australian adolescent girls experience significant period pain. Those with dysmenorrhea at a young age continue to experience it throughout adolescence, impairing their engagement with school, work, and social activities. Highlighting the prevalence of these experiences is critical for reducing the stigmatisation of female pain, as well as for increasing awareness among medical professionals of how common it is and identifying the young women at greater risk of conditions such as endometriosis.
Thirty‐five percent of participants at 14 years of age, 50% at 16 years, and 46% at 18 years reported dysmenorrhea (very or quite painful periods). In earlier studies, 80–93% of adolescent girls and young women aged 13–25 years reported period pain in Australia,2,3,4,5 but these studies included participants with mild pain2,4,5 or did not assess pain severity.3 Including all participants in our cohort who reported any degree of period pain yielded proportions similar to those reported by other studies (wave 6, 70%; wave 7, 85%; wave 8, 86%).
One of our most striking findings was the consistency in reported period pain severity over time. Most participants with dysmenorrhea at 14 or 16 years of age also reported it in subsequent study waves, and very few of these girls later reported no period pain. Further, 20% of participants who reported no pain at 14 years of age later reported quite or very painful periods. The relationship between early chronic period pain and later endometriosis is increasingly recognised;14 one in five Australian women develop some form of chronic pain during their lifetime.15 Identifying people at risk of developing chronic conditions as early as possible is critical for ensuring that they receive early intervention and support.
In our cohort, 25% of participants aged 14 years, 45% of those aged 16 years, and 59% of participants aged 18 years reported using oral contraception for birth control. The oral contraceptive pill can reduce the severity of period pain and is often prescribed as a first‐line treatment for this indication.16,17 Given its widespread use in the age groups examined, we may have underestimated the prevalence of dysmenorrhea and the severity of period pain. We need more information about adolescents who use the oral contraceptive pill for managing period pain.
At each wave of data collection, about one‐third of respondents reported missing at least one activity type (school or university, work, social, sport or exercise) in the preceding three months because of their periods, and the proportions were larger for those reporting more severe period pain. Participants with dysmenorrhea were three to five times as likely to miss school or university as those without dysmenorrhea. Given the general impact of missing school,18,19 dysmenorrhea may have a negative impact on school outcomes, mental health, and general psychological wellbeing. Further, 14‐ and 18‐year‐old participants with dysmenorrhea were about three times as likely to have missed sporting or exercise activities because of their periods as those without dysmenorrhea. Engaging in regular sport and exercise during adolescence is important for general wellbeing, and protects against mental health problems.20
The experiences of dysmenorrhea in specific groups of Australian adolescents require investigation, including those with different gender identities, cultural backgrounds, and disabilities. Further, assessing the knowledge of adolescents and their parents and carers about dysmenorrhea, including treatment options, would be valuable.
Limitations
As our analyses were restricted by the questions included in the LSAC surveys, we could not determine age of menarche, how frequently participants missed activities because of their periods, or whether missing activities was related to period pain or another problem. Second, the LSAC surveys include a question about biological sex only until wave 7, and one about gender identity only from wave 8. Our findings therefore reflect the experiences of participants who reported that they were biologically female, and may not reflect the experiences of other people who have periods. Third, the LSAC surveys ask only about the use of the oral contraceptive pill for birth control; as it is widely used to manage period pain, we do not know how many participants used the oral contraceptive pill for this purpose rather than for pregnancy prevention.
Conclusion
A large proportion of adolescent girls in Australia experience period pain that affects their engagement in regular activities. Further, those who have painful periods at a young age continue to experience painful periods throughout their adolescence. Health education about menstruation for both adolescents and health professionals should be improved, and views that period pain is normal challenged. Adolescents experiencing pain should be identified and provided with early interventions to minimise its impact on schooling and other activities, and early screening for chronic health conditions, such as chronic pelvic pain, should be promoted.
Box 1 – Characteristics of the 1835 Longitudinal Study of Australian Children Kinder cohort female participants at waves 6 to 8 of data collection, and of the 1600 who answered menstrual pain questions at one or more waves*
|
|
Longitudinal Study of Australian Children Kinder cohort female participants |
Participants who provided information on menstrual pain at one or more waves |
|||||||||||||
|
Characteristic |
Wave 6 |
Wave 7 |
Wave 8 |
Wave 6 |
Wave 7 |
Wave 8 |
|||||||||
|
|
|||||||||||||||
|
Participants [proportion of original cohort] |
1739 [71.0%] |
1513 [71.0%] |
1486 [60.7%] |
644 [26.3%] |
1341 [54.8%] |
1115 [45.6%] |
|||||||||
|
Age (years), mean (SD) |
14.4 (0.49) |
16.5 (0.50) |
18.4 (0.50) |
14.4 (0.48) |
16.5 (0.50) |
18.2 (0.50) |
|||||||||
|
Aboriginal or Torres Strait Islander people |
44 (2%) |
34 (2%) |
30 (2%) |
15 (2%) |
28 (2%) |
28 (2%) |
|||||||||
|
Socio‐economic status† |
|
|
|
|
|
|
|||||||||
|
IRSAD score, mean (SD) |
1012 (74) |
1012 (78) |
1019 (77) |
1006 (76) |
1005 (77) |
1011 (77) |
|||||||||
|
IRSAD score, range |
720–1180 |
730–1180 |
730–1180 |
740–1180 |
770–1180 |
800–1180 |
|||||||||
|
IRSAD decile, mean (SD) |
5.9 (2.8) |
5.9 (2.8) |
6.2 (2.8) |
5.7 (2.9) |
5.7 (2.8) |
5.9 (2.8) |
|||||||||
|
School attendance |
|
|
|
|
|
|
|||||||||
|
Attends school |
1680 (99%) |
1347 (93%) |
NA |
635 (98%) |
1234 (92%) |
NA |
|||||||||
|
Not attending school |
19 (1%) |
103 (7%) |
NA |
5 (2%) |
72 (8%) |
NA |
|||||||||
|
Missing data |
40 |
63 |
NA |
4 |
35 |
NA |
|||||||||
|
Employment |
|
|
|
|
|
|
|||||||||
|
Employed |
NA |
757 (53%) |
964 (73%) |
NA |
712 (53%) |
802 (72%) |
|||||||||
|
Unemployed |
NA |
NA |
166 (13%) |
NA |
NA |
142 (13%) |
|||||||||
|
Looking for work |
NA |
155 (11%) |
NA |
NA |
146 (11%) |
NA |
|||||||||
|
Not looking for work |
NA |
514 (36%) |
195 (15%) |
NA |
460 (34%) |
157 (14%) |
|||||||||
|
Missing data |
— |
87 |
161 |
— |
23 |
14 |
|||||||||
|
Have you ever menstruated? |
|
|
|
|
|
|
|||||||||
|
Yes |
1547 (95%) |
1431 (99%) |
1333 (99%) |
644 (100%) |
1341 (100%) |
1115 (100%) |
|||||||||
|
No |
88 (5%) |
10 (1%) |
7 (1%) |
0 |
0 |
0 |
|||||||||
|
Missing data |
104 |
72 |
146 |
0 |
0 |
0 |
|||||||||
|
Have you had any periods in the past three months? |
|
|
|
|
|
|
|||||||||
|
Yes |
641 (87%) |
1324 (95%) |
1111 (91%) |
644 (100%) |
1341 (100%) |
1115 (100%) |
|||||||||
|
No |
99 (13%) |
74 (5%) |
113 (9%) |
0 |
0 |
0 |
|||||||||
|
Missing data |
999 |
115 |
262 |
0 |
0 |
0 |
|||||||||
|
Currently using oral contraceptive pill (for birth control) |
21 (1%) |
209 (14%) |
446 (30%) |
4 (1%) |
185 (14%) |
376 (34%) |
|||||||||
|
|
|||||||||||||||
|
IRSAD = Index of Relative Socio‐Economic Advantage and Disadvantage; NA = not available (question not asked); SD = standard deviation. * Proportions are weighted by cross‐sectional sample weights. † Missing data: wave 6, one participant. |
|||||||||||||||
Box 2 – “During the last 3 months, how painful were your periods?”, by use of oral contraception*
|
|
Wave 6 (age 14 years)† |
Wave 7 (age 16 years)† |
Wave 8 (age 18 years)† |
||||||||||||
|
Period pain severity |
Oral contraception‡ |
No oral contraception |
Oral contraception‡ |
No oral contraception |
Oral contraception‡ |
No oral contraception |
|||||||||
|
|
|||||||||||||||
|
Number of respondents |
4 |
640 |
191 |
1151 |
374 |
741 |
|||||||||
|
Very painful |
1 (25%) |
78 (12%) |
58 (30%) |
249 (22%) |
63 (17%) |
140 (19%) |
|||||||||
|
Quite painful |
1 (25%) |
147 (23%) |
47 (25%) |
322 (28%) |
107 (29%) |
208 (28%) |
|||||||||
|
A little painful |
1 (25%) |
220 (34%) |
65 (34%) |
403 (35%) |
149 (40%) |
290 (39%) |
|||||||||
|
Not at all painful |
1 (25%) |
195 (30%) |
21 (11%) |
177 (16%) |
55 (15%) |
103 (14%) |
|||||||||
|
|
|||||||||||||||
|
* Proportions are weighted by cross‐sectional sample weights. † Ages are approximate mean ages for all Longitudinal Study of Australian Children Kinder cohort participants at the data collection wave. ‡ Only participants who reported sexual activity were asked about birth control methods used. “No oral contraception” could therefore include some who used oral contraception but had denied sexual activity or not yet commenced sexual activity. |
|||||||||||||||
Box 3 – Participants who reported missing activities during the past three months because of their periods*
|
Activity type missed |
Wave 6 (age 14 years)†,‡ |
Wave 7 (age 16 years)† |
Wave 8 (age 18 years)† |
||||||||||||
|
Number |
Proportion (95% CI) |
Number |
Proportion (95% CI) |
Number |
Proportion (95% CI) |
||||||||||
|
|
|||||||||||||||
|
Respondents |
647 |
|
1341 |
|
1111 |
|
|||||||||
|
School/university |
115 |
18% (13–19%) |
293 |
22% (19–23%) |
154 |
14% (12–16%) |
|||||||||
|
Work |
NA |
— |
67 |
5% (3–5%) |
101 |
9% (6–10%) |
|||||||||
|
Social activities |
123 |
19% (15–20%) |
168 |
13% (12–15%) |
173 |
16% (14–18%) |
|||||||||
|
Sports or exercise |
148 |
23% (18–25%) |
151 |
11% (11–14%) |
170 |
15% (15–19%) |
|||||||||
|
Number of activity types missed |
|
|
|
|
|
|
|||||||||
|
None |
424 |
66% (62–69%) |
887 |
66% (65–70%) |
767 |
69% (66–72%) |
|||||||||
|
One |
122 |
19% (17–23%) |
293 |
22% (18–22%) |
163 |
15% (13–17%) |
|||||||||
|
Two |
61 |
9% (8–12%) |
107 |
8% (7–9%) |
125 |
11% (9–13%) |
|||||||||
|
Three |
40 |
6% (4–7%) |
42 |
3% (3–5%) |
40 |
4% (3–5%) |
|||||||||
|
Four |
NA |
— |
11 |
1% (1–2%) |
16 |
1% (1–2%) |
|||||||||
|
|
|||||||||||||||
|
CI = confidence interval; NA = not applicable. * Proportions are weighted by cross‐sectional sample weights. † Ages are approximate mean ages for all Longitudinal Study of Australian Children Kinder cohort participants at the data collection wave. ‡ For Wave 6, three participants responded to the questions about missing activities but did not respond to questions about period pain. |
|||||||||||||||
Box 4 – Missing activities for respondents with or without dysmenorrhea: adjusted binomial logistics regression analyses
|
|
Dysmenorrhea v no dysmenorrhea: adjusted odds ratio (95% CI)* |
||||||||||||||
|
Activity missed |
Wave 6 (age 14 years)† |
Wave 7 (age 16 years)† |
Wave 8 (age 18 years)† |
||||||||||||
|
|
|||||||||||||||
|
Total number of respondents |
644 |
513 |
361 |
||||||||||||
|
School/university |
4.90 (3.13–7.66) |
3.36 (1.95–5.80) |
3.93 (1.58–9.81) |
||||||||||||
|
Social activities |
2.88 (1.89–4.38) |
2.21 (1.19–4.13) |
4.86 (2.33–10.2) |
||||||||||||
|
Sport/exercise |
2.78 (1.89–4.09) |
1.47 (0.79–2.75) |
3.61 (1.85–7.07) |
||||||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * Adjusted for socio‐economic status and dysmenorrhea reported at previous waves. † Ages are approximate mean ages for all Longitudinal Study of Australian Children Kinder cohort participants at the data collection wave. |
|||||||||||||||
Box 5 – Period pain severity for participants who reported missing selected activities because of their periods, by activity type and study wave*
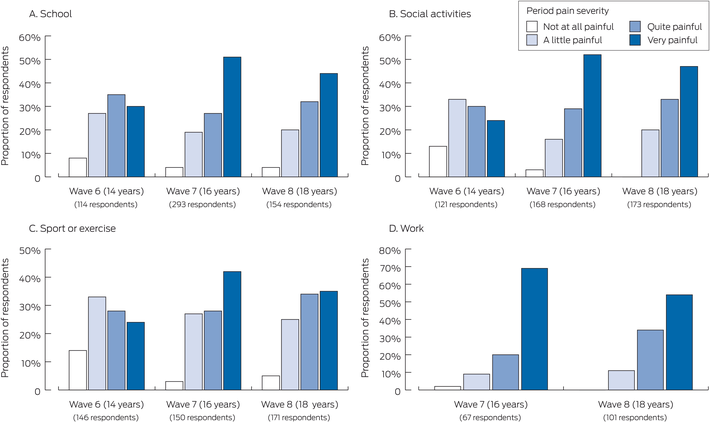
* The data underlying this graph are provided in the Supporting Information, table 5.
Box 6 – Numbers of selected activities missed by participants because of their periods, by study wave and period pain severity*
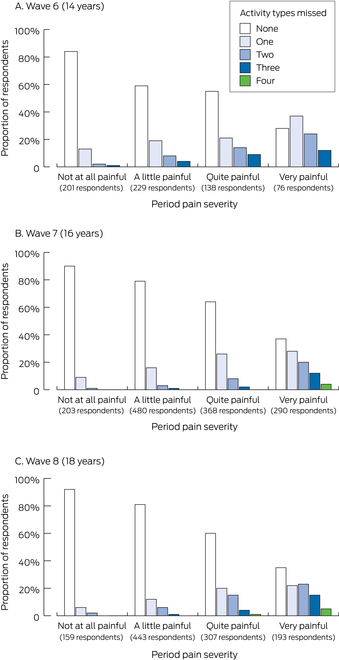
* The data underlying this graph are provided in the Supporting Information, table 6.
Received 8 December 2022, accepted 23 November 2023
- Lauren Cameron1,2
- Antonina Mikocka‐Walus1
- Emma Sciberras1
- Marilla Druitt3,4
- Katherine Stanley5
- Subhadra Evans1
- 1 Deakin University, Melbourne, VIC
- 2 Monash University, Melbourne, VIC
- 3 Deakin University, Geelong, VIC
- 4 University Hospital Geelong, Geelong, VIC
- 5 Endo Help Foundation, Point Lonsdale, VIC
Open access:
Open access publishing facilitated by Deakin University, as part of the Wiley – Deakin University agreement via the Council of Australian University Librarians.
The study was funded by the Endo Help Foundation (https://endohelp.com.au), a not‐for‐profit advocacy organisation. This article uses unit record data from the Longitudinal Study of Australian Children (LSAC), conducted by the Australian Government Department of Social Services (DSS) (doi: 10.26193/QR4L6Q). The findings and views reported in this article, however, are those of the authors and should not be attributed to the Australian government, DSS, or any of contractors or partners of DSS.
No relevant disclosures.
- 1. Armour M, Parry K, Manohar N, et al. The prevalence and academic impact of dysmenorrhea in 21 573 young women: a systematic review and meta‐analysis. J Women's Health 2019; 28: 1161‐1171.
- 2. Armour M, Ferfolja T, Curry C, et al. The prevalence and educational impact of pelvic and menstrual pain in Australia: a national online survey of 4202 young women aged 13–25 years. J Pediatr Adolesc Gynecol 2020; 33: 511‐518.
- 3. Hillen TIJ, Grbavac SL, Hohnston PJ, et al. Primary dysmenorrhea in young Western Australian women: prevalence, impact, and knowledge of treatment. J Adolesc Health 1999; 25: 40‐45.
- 4. Parker MA, Sneddon AE, Arbon P. The menstrual disorder of teenagers (MDOT) study: determining typical menstrual patterns and menstrual disturbance in a large population‐based study of Australian teenagers. BJOG 2010; 117: 185‐192.
- 5. Subasinghe AK, Happo L, Jayasinghe YL, et al. Prevalence and severity of dysmenorrhea, and management options reported by young Australian women. Aust Fam Physician 2016; 45: 829‐834.
- 6. Li A, Bellis EK, Girling JE, et al. Unmet needs and experiences of adolescent girls with heavy menstrual bleeding and dysmenorrhea: a qualitative study. J Pediatr Adolesc Gynecol 2020; 33: 278‐284.
- 7. Chen CX, Draucker CB, Carpenter JS. What women say about their dysmenorrhea: a qualitative thematic analysis. BMC Womens Health 2018; 18: 47.
- 8. De Sanctis V, Soliman ST, Elsedfy H, et al. Dysmenorrhea in adolescents and young adults: a review in different countries. Acta Biomed 2016; 87: 233–246.
- 9. Treloar SA, Bell TA, Nagle CM, et al. Early menstrual characteristics associated with subsequent diagnosis of endometriosis. Am J Obstet Gynecol 2010; 202: 534. e1‐e6.
- 10. Knox B, Ong YC, Bakar MA, Grover SR. A longitudinal study of adolescent dysmenorrhea into adulthood. Eur J Ped 2019; 178: 1325‐1332.
- 11. Soloff C, Lawrence D, Johnstone R. LSAC technical paper No. 1: sample design. Australian Institute of Family Studies, May 2005. https://growingupinaustralia.gov.au/sites/default/files/tp1.pdf (viewed Aug 2022).
- 12. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med 2007; 4: e297.
- 13. Australian Bureau of Statistics. IRSAD. In: Census of Population and Housing: Socio‐Economic Indexes for Areas (SEIFA), Australia, 2016 (2033.0.55.001). 27 Mar 2018. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2033.0.55.001~2016~Main%20Features~IRSAD~20 (viewed Nov 2022).
- 14. Gutman G, Nunez AT, Fisher M. Dysmenorrhea in adolescents. Curr Probl Pediatr Adolesc Health Care 2022; 52: 101186.
- 15. Australian Institute of Health and Welfare. Chronic pain in Australia (cat. no. PHE 267). 7 May 2020. https://www.aihw.gov.au/reports/chronic‐disease/chronic‐pain‐in‐australia/summary (viewed Nov 2022).
- 16. Schindler AE. Non‐contraceptive benefits of oral hormonal contraceptives. Int J Endocrinol Metab 2013; 11: 41‐47.
- 17. Harel Z. Dysmenorrhea in adolescents and young adults: etiology and management. J Pediatr Adolesc Gynecol 2006; 19: 363‐371.
- 18. Finning K, Ukoumunne OC, Ford T, et al. The association between child and adolescent depression and poor attendance at school: a systematic review and meta‐analysis. J Affect Disord 2019; 245: 928‐938.
- 19. Epstein S, Roberts E, Sedgwick R, et al. School absenteeism as a risk factor for self‐harm and suicidal ideation in children and adolescents: a systematic review and meta‐analysis. Eur Child Adolesc Psychiatry 2019; 29: 1175‐1194.
- 20. Belcher BR, Zink J, Azad A, et al. The roles of physical activity, exercise, and fitness in promoting resilience during adolescence: effects on mental well‐being and brain development. Biol Psychiatry Cogn Neurosci Neuroimaging 2021; 6: 225‐237.






Abstract
Objectives: To determine the proportion of Australian adolescent girls who experience menstrual pain (dysmenorrhea); to assess associations of dysmenorrhea and period pain severity with adolescents missing regular activities because of their periods.
Study design: Prospective, population‐based cohort study; analysis of Longitudinal Study of Australian Children (LSAC) survey data.
Setting, participants: Female adolescents in the nationally representative cross‐sequential sample of Australian children recruited in 2004 for the Kinder cohort (aged 4–5 years at enrolment). Survey data from waves 6 (mean age 14 years), wave 7 (16 years) and wave 8 (18 years) were analysed.
Main outcome measures: Severity of period pain during the preceding three months (very, quite, a little, or not at all painful); number of activity types missed because of periods; relationship between missing activities and period pain severity.
Results: Of the 1835 participating female members of the LSAC Kinder cohort at waves 6 to 8, 1600 (87%) responded to questions about menstruation during at least one of waves 6 to 8 of data collection. At wave 6 (14 years), 227 of 644 respondents (35%) reported dysmenorrhea, 675 of 1341 (50%) at wave 6 (16 years), and 518 of 1115 (46%) at wave 8 (18 years). Of the 366 participants who reported period pain severity at all three waves, 137 reported no dysmenorrhea at all three waves (37%), 66 reported dysmenorrhea at all three waves (18%), 89 reported increasing period pain over time (24%), and 38 reported declining pain (10%). At wave 6, 223 of 647 participants reported missing at least one activity because of their periods (34%), 454 of 1341 at wave 7 (34%), and 344 of 1111 at wave 8 (31%). Of the participants who experienced very painful periods, 72% (wave 6), 63% (wave 7), and 65% (wave 8) missed at least one activity type because of their periods, as did 45% (wave 6), 36% (wave 7), and 40% (wave 8) of those who experienced quite painful periods.
Conclusions: A large proportion of adolescent girls in Australia experience period pain that affects their engagement in regular activities, including school attendance. Recognising adolescent period pain is important not only for enhancing their immediate quality of life with appropriate support and interventions, but also as part of early screening for chronic health conditions such as endometriosis.