The known: Treatment rates for basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) (keratinocyte cancers) increased during 2000–2011 both overall and among Australians aged 55 years or older, but they declined among younger people.
The new: During 2012–2021, rates of treatment of younger Australians for histologically confirmed BCC/SCC continued to decline despite increasing biopsy rates. Overall treatment rates increased because of rises for older Australians (men aged 65 years or older, women aged 55 years or older).
The implications: The factors contributing to lower keratinocyte cancer treatment rates among younger Australians require further investigation.
In Australia, at least one in three people are diagnosed with keratinocyte cancers — predominantly cutaneous squamous cell carcinomas (SCCs) and basal cell carcinomas (BCCs) — during their lifetime.1 The cost to the Australian health system of treating these cancers was estimated to be $1.4 billion in 2019–20, or 12.1% of all cancer‐related health expenditure and 1.0% of total health expenditure.2
Reliable estimates of changes in disease incidence are important for designing prevention activities and monitoring their success, and for planning health care services. Keratinocyte cancer incidence statistics are not available in Australia because these cancers are not registered by most state and territory cancer registries (exception: Tasmania3). The incidence of keratinocyte cancers has been increasing by 1–8% per year in countries where they are routinely registered, including the United Kingdom,4 Germany,5 the Netherlands,6 Norway,7 Sweden,8 and Iceland.9,10 In the United States, the incidence of keratinocyte cancers increased during 1990–2004, then stabilised during 2004–2019.11 In Tasmania, the incidence of diagnosed BCCs increased during 1985–2018 by a mean 3% per year and that of SCCs by 4% per year.3
As keratinocyte cancers are not registered in most Australian states, we rely on proxy measures to estimate changes in their national incidence, such as Medicare claims data for services listed on the Medical Benefits Schedule (MBS). Medicare subsidises almost all medical services for treating keratinocyte cancers, apart from the very small proportion of skin cancer procedures undertaken in public hospitals.
Australian clinical practice guidelines recommend surgical excision for most BCCs and SCCs, and non‐surgical options for selected “clinically favourable” lesions.12 Malignancy must be established by histopathology before MBS benefits can be claimed for excisions. For cryotherapy and curettage of malignant lesions, the malignancy must be “confirmed by histopathology or confirmed by the opinion of a specialist in the specialty of dermatology or plastic surgery” (MBS item numbers, 2011–15: 30196, 30197, 30202, 30203, 30205; MBS item numbers, 2016: 30196, 30202). The MBS item codes for excisions and cryotherapy or curettage for malignant lesions are about 97% concordant with histopathologic diagnoses.13
In 2014, we reported that MBS data for excisions of histologically confirmed keratinocyte cancers indicated that the excision rate had increased during 2000–2011 by a mean of 2.2% per year for women and 3.3% for men.14 As the Australian clinical landscape has changed in the decade since this report, we examined more recent changes in the numbers of Medicare‐subsidised keratinocyte cancer excisions, particularly for younger people exposed to primary prevention campaigns since the early 1980s.15
Methods
For our retrospective observational study, we downloaded MBS claims data for the period 1 January 2012 – 31 December 2021 from the Services Australia Medicare Item Reports website (http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp) in February 2023. We identified all item numbers for procedures related to the diagnosis and treatment of skin cancers in two editions of the MBS Book of Therapeutic Procedures, category 3 (those effective 1 January 201216 and 17 January 202017) to ensure that we included all item codes used during 2012–2021 (Supporting Information, 1 and 2). Data were downloaded to Excel (Microsoft), then imported into SAS 9.4 for collation and analysis. In total, we downloaded 140 spreadsheets including ten years of MBS claims data for 41 item numbers.
For each MBS item, we obtained the number of procedures performed in each Australian state and territory during each year of the study period, stratified by age (ten categories) and sex. We report number and number per capita for each calendar year; the population denominator for number per capita was the MBS‐eligible population for the corresponding year. For item codes discontinued in 2016 but still recorded in subsequent years, we added the number of procedures claimed under the discontinued item numbers and that of the corresponding procedures claimed under the new item numbers introduced in 2016. All incidence rates were standardised to the 2001 Australian standard population.18
Statistical analysis
We fitted joinpoint regression models to identify the calendar years in which changes in trends in age‐standardised incidence rates were statistically significant. We separately examined incidence rates by sex and state for first surgical BCC/SCC excisions, Mohs micrographic surgery, surgical excisions of benign lesions, skin biopsies, and other treatments (cryotherapy or serial curettage of premalignant and malignant lesions); we also assessed changes by sex and state for BCC/SCC excisions and biopsies. Changes in the rates of claims for skin biopsies and other treatments of benign lesions were undertaken to determine whether changes in BCC/SCC excision rates were specific to the treatment of keratinocyte cancers, or reflected broader changes in the diagnosis and treatment of skin conditions. Finally, we examined changes in age‐specific rates of BCC/SCC excisions, cryotherapy or curettage of confirmed malignant lesions, and biopsies by age group (six age groups) and sex.
Analyses were undertaken in Joinpoint 4.8.0.1 (Statistical Research and Applications Branch, National Cancer Institute), which uses Monte Carlo permutation to identify statistically significant changes in temporal slope (P < 0.05) and calculates the average annual percentage change in rate (with the 95% confidence interval [CI]) for each segment between points of change.19 To test for differences in average annual percentage change by sex, we used the pairwise comparison option in Joinpoint, which uses a classic approximate F test to compare two sets of trend data.20
Ethics approval
The QIMR Berghofer Medical Research Institute Human Research Ethics Committee approved our study (P3631).
Results
Selected demographic characteristics of the Medicare population and the numbers of claims for the diagnosis and treatment of skin cancers in 2012 are provided in Box 1. During 2012–2019, age‐standardised claims rates for first BCC/SCC excisions, Mohs surgery (2012–2021), cryotherapy or serial curettage of malignant lesions (men: 2012–2018), and biopsies increased for both sexes, then stabilised (BCC/SCC excisions, women; biopsies, both sexes) or declined (BCC/SCC excisions, men; cryotherapy or serial curettage of malignant lesions, both sexes) during 2019–2021. Benign lesion excision rates declined during 2014–2021; those of cryotherapy or serial curettage of premalignant lesions declined throughout 2012–2021, most rapidly during 2019–2021. The differences between men and women in the rates of change for surgical excisions of BCC/SCC and of benign lesions were statistically significant across 2012–2021 (Box 2; Box 3).
Excisions of histologically confirmed BCCs/SCCs
In men, the age‐standardised rate of BCC/SCC excisions increased by 1.9% (95% CI, 1.4–2.4%) per year during 2012–2019 (from 2931 to 3371 per 100 000 men) and then declined by 3.8% (95% CI, 0.5–7.0%) per year during 2019–2021 (to 3152 per 100 000). In women, the age‐standardised rate increased by 2.2% (95% CI, 1.7–2.8%) per year during 2012–2019 (from 1798 to 2093 per 100 000 women); the decline to 1967 excisions per 100 000 women in 2021 was not statistically significant (Box 2).
Age‐standardised BCC/SCC excision rates were highest in Queensland (2021: 5809 per 100 000 men; 3700 per 100 000 women) and lowest in Victoria (2021: 1911 per 100 000 men; 1221 per 100 000 women). BCC/SCC excision rates increased during 2012–2021 in Tasmania, the Australian Capital Territory (both sexes), and South Australia (women); they increased during 2012–2018 or 2019 in Queensland, Victoria, Western Australia, the Northern Territory (both sexes), and South Australia (men), then stabilised (Victoria, Western Australia, South Australia) or declined (Queensland, Northern Territory) to 2021. In New South Wales, the rates increased slightly during 2012–2019, then stabilised. The differences between men and women in rates of change were statistically significant across 2012–2021, except in Victoria, the Northern Territory, and the Australian Capital Territory (Box 4).
Mohs surgery and cryotherapy or serial curettage for histologically confirmed BCCs/SCCs
For men, the age‐standardised rate of Mohs surgery increased by 4.4% (95% CI, 4.1–4.7%) per year during 2012–2021 (from 48 to 68 per 100 000 men); for women, it also increased by 4.4% (95% CI, 4.1–4.7%) per year (from 38 to 56 per 100 000 women). During 2012–2018, The age‐standardised rate of cryotherapy or serial curettage of malignant lesions increased by 1.9% (95% CI, 1.1–2.7%) per year for men (from 1054 to 1212 per 100 000 men) and by 2.4% (95% CI, 1.7–3.1%) per year for women (from 642 to 719 per 100 000 women); during 2018–2021 it declined for both men (by 8.5% [95% CI, 3.3–13.5%] per year) and women (by 5.4% [95% CI, 3.6–7.2%] per year) (Box 2).
Other diagnostic procedures
For men, the age‐standardised skin biopsy rate increased during 2012–2019 by 6.0% (95% CI, 5.1–6.9%) per year (from 3337 to 5180 per 100 000 men) and for women by 5.3% (95% CI, 4.6–6.1%) per year (from 3270 to 4798 per 100 000 women). The benign lesion excision rate did not change significantly during 2012–2014 and declined during 2014‐2021; rates of cryotherapy or serial curettage for premalignant lesions declined throughout 2012–2021 (Box 2).
Diagnostic procedure rate changes, by sex and age group
Age‐standardised biopsy rates increased during 2012–2021 in all age groups (by 2.8–6.9% per year). BCC/SCC excision rates increased only for men and women aged 65–74 years or 75 years or older; the rates declined for men under 55 years of age (by 1.0–3.4% per year) and for women under 45 years of age (by 1.7–2.3% per year). Age‐standardised rates of cryotherapy/curettage for malignant lesions increased for men aged 75 years or older (1.9% [95% CI, 0.1–3.7%] per year) and declined for those under 55 years of age (by 1.6–6.0% per year); the rates did not change significantly for women aged 55 years or older, and declined among younger women (by 1.9–5.7% per year) (Box 5).
Discussion
We analysed national MBS claims data to assess changes during 2012–2021 in the numbers of procedures for diagnosing and treating keratinocyte cancers in Australia. While the overall age‐standardised BCC/SCC excision rate increased by about 2% per year for both men and women, the increases were restricted to men aged 65 years or older and women aged 55 years or older; BCC/SCC excision rates declined in younger age groups. Similarly, rates of cryotherapy or curettage of malignant lesions rose for men aged 75 years or older, but declined for men and women under 55 years of age. In contrast, the overall age‐standardised biopsy rate increased during 2012–2019 (men: by 6.0% per year; women: by 5.3% per year), and during 2012–2021 increased in all age groups, and the rate increase rose with age. As the MBS item code for biopsy does not distinguish between benign and malignant lesions, the interpretability of this finding is limited. However, the rates of excisions of benign lesions and cryotherapy or curettage for premalignant lesions generally declined during 2012–2021.
The mean increase in the BCC/SCC excision rate for men during 2012–2019 (1.9% per year) was smaller than during 2000–2011 (3.3% per year), but the mean rate of increase for women was fairly constant throughout 2000–2019 (about 2.2% per year).15 It is likely that very recent declines (2019–2021) in skin cancer procedure rates reflect the impact of the coronavirus disease 2019 (COVID‐19) pandemic, which in Australia commenced in March 2020; similar reductions in the number of skin cancers diagnosed during the pandemic have been reported in other countries.21,22,23 We might therefore expect a rebound in diagnostic and treatment services for people with skin cancer, as has been reported for other cancer screening.24
While overall keratinocyte cancer treatment rates rose during 2012–2021, among younger and middle‐aged Australians they steadily declined. These declines were accompanied by rising biopsy rates in all age groups, including people under 55 years of age. Taken together, these findings indicate that many more Australians are having skin lesions assessed, but fewer keratinocyte cancers are being detected; that is, we are looking more and finding less. This strongly suggests that reported findings of declines in the incidence of keratinocyte cancers among younger people14 are robust. This contrasts with reports of increasing incidence in most other world regions,4,5,6,7,8,9,10 and may reflect the success of Australian primary prevention campaigns since the early 1980s25 that have changed sun exposure behaviours.26 Other factors that probably contribute to declining rates of BCC/SCC treatment for younger Australians include the general shift to more time spent indoors (including longer periods of screen time) and changing demographic characteristics (eg, an increase in the population proportion of migrants and their offspring who are physiologically at lower risk of skin cancer than Australians in earlier studies27). The relative contributions of each of these factors to the declines in the incidence of keratinocyte cancer treatment for younger Australians awaits investigation.
Limitations
We analysed national administrative data, based on the reliability of MBS item claims as a proxy measure of histologically confirmed BCC/SCC.13 The validity of this proxy measure is important, as keratinocyte cancers are not registered nationally in Australia, and the most recent national incidence survey was undertaken in 2002.28 However, analyses of aggregated claims data cannot take multiple events into account; the rates we estimated are event rates, not per person rates. Some skin lesions are treated destructively and without histological confirmation; further, MBS claims data do not include treatment of skin cancers in public hospitals. The Australian Institute of Health and Welfare recorded 114 722 keratinocyte cancer‐related hospitalisations during 2013–14,29 but this included treatments provided in private hospitals that were also included in the MBS database. Of 18 477 episodes of care for excision of a histologically confirmed keratinocyte cancer during 2011–15 for people in a Queensland population cohort (43 794 participants aged 40–69 years at baseline), only 2.4% were in public hospitals; 7.8% were undertaken in private hospitals, and 89.7% in private clinics or rooms.30 Nevertheless, our estimated treatment rates probably underestimate the incidence of keratinocyte cancers. Finally, MBS item codes do not discriminate between treatments for BCCs and SCCs, and changes in the diagnosis and treatment of the two cancer types may differ.
Conclusions
The burden of keratinocyte cancers in Australia is high and increasing, but it is encouraging that skin cancer treatment rates are declining among younger Australians. How much of this effect is attributable to skin cancer prevention campaigns is unknown. Future changes in skin cancer incidence will be determined by event rates in recent birth cohorts as they age; these people will probably have been exposed to less sunlight than earlier generations because of the combined effects of public health interventions and population‐wide lifestyle changes related to technology use. They will also include a smaller proportion of people highly susceptible to skin cancer, given demographic changes in the Australian population. We therefore predict continued reductions in the incidence of skin cancer among younger people. However, we also expect that these reductions will be more than offset by continued increases in skin cancer among older people, probably for the next two decades. We advocate further quantification of the factors that contribute to reductions in skin cancer incidence and continued monitoring, with the aim of ensuring that future Australians enjoy relief from these preventable cancers.
Box 1 – Selected demographic characteristics of people eligible to receive Medicare services,* and MBS claims for skin cancer‐related treatments, Australia, 2012 calendar year†
|
Characteristic |
Number |
||||||||||||||
|
|
|||||||||||||||
|
Age group (years) |
|
||||||||||||||
|
0–4 |
1 500 791 (6.5%) |
||||||||||||||
|
5–14 |
2 880 208 (12.5%) |
||||||||||||||
|
15–24 |
2 960 563 (12.9%) |
||||||||||||||
|
25–34 |
3 232 960 (14.1%) |
||||||||||||||
|
35–44 |
3 339 361 (14.5%) |
||||||||||||||
|
45–54 |
3 160 084 (13.7%) |
||||||||||||||
|
55–64 |
2 668 043 (11.6%) |
||||||||||||||
|
65–74 |
1 796 985 (7.8%) |
||||||||||||||
|
75–84 |
1 024 648 (4.5%) |
||||||||||||||
|
85 or older |
429 953 (1.9%) |
||||||||||||||
|
Sex |
|
||||||||||||||
|
Male |
11 544 676 (50.2%) |
||||||||||||||
|
Female |
11 448 920 (49.8%) |
||||||||||||||
|
State/territory |
|
||||||||||||||
|
New South Wales |
7 456 089 (32.4%) |
||||||||||||||
|
Victoria |
5 694 579 (24.8%) |
||||||||||||||
|
Queensland |
4 637 934 (20.2%) |
||||||||||||||
|
South Australia |
1 669 089 (7.3%) |
||||||||||||||
|
Western Australia |
2 403 064 (10.5%) |
||||||||||||||
|
Tasmania |
521 804 (2.3%) |
||||||||||||||
|
Australian Capital Territory |
380 739 (1.7%) |
||||||||||||||
|
Northern Territory |
230 298 (1.0%) |
||||||||||||||
|
MBS skin cancer‐related treatment claims |
|
||||||||||||||
|
Biopsy |
811 899 (3.5%) |
||||||||||||||
|
Cutaneous squamous cell and basal cell carcinoma excisions |
590 306 (2.6%) |
||||||||||||||
|
Mohs surgery |
10 612 (0.05%) |
||||||||||||||
|
Excision of benign lesions (to exclude melanoma) |
561 101 (2.4%) |
||||||||||||||
|
Cryotherapy/curettage: premalignant lesions |
643 622 (2.8%) |
||||||||||||||
|
Cryotherapy/curettage: malignant lesions |
211 874 (0.9%) |
||||||||||||||
|
|
|||||||||||||||
|
MBS = Medical Benefits Schedule. * Citizens or permanent residents of Australia; citizens of New Zealand; citizens or permanent residents of Norfolk Island, Cocos Islands, Christmas Island, or Lord Howe Island; people applying for permanent residency; temporary residents covered by a ministerial order. Prisoners, asylum seekers who have applied for a protection visa and whose bridging visa has expired, and veterans who qualify for Department of Veterans’ Affairs National Treatment Account benefits are excluded. † Sources of demographic data and claims data: Services Australia Medicare Item Reports website (http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp) Medicare resident population denominators were calculated as the product of numbers of services by the inverse of the rate of service per 100 000 persons. Procedure numbers by age group and sex are reported in the Supporting Information, table 3. |
|||||||||||||||
Box 2 – MBS‐subsidised skin cancer‐related services: age‐standardised procedure rates, 2012 and 2021, and average annual percentage change, 2012–2021
|
Procedure |
Age standardised rate* (per 100 000) |
|
|||||||||||||
|
Women |
Men |
Women |
Men |
|
|||||||||||
|
2012 |
2021 |
2012 |
2021 |
Period† |
AAPC (95% CI) |
Period† |
AAPC (95% CI) |
P ‡ |
|||||||
|
|
|||||||||||||||
|
Surgical excision |
|
|
|
|
|
|
|
|
|
||||||
|
Squamous cell/basal cell carcinoma excisions (first excisions) |
1798 |
1967 |
2931 |
3152 |
2012–2019 |
2.2% (1.7 to 2.8%) |
2012–2019 |
1.9% (1.4 to 2.4%) |
0.003 |
||||||
|
|
|
|
|
|
2019–2021 |
–3.4% (–6.9 to 0.2%) |
2019–2021 |
–3.8% (–7.0 to –0.5%) |
|
||||||
|
Mohs surgery |
38 |
56 |
48 |
68 |
2012–2021 |
4.4% (4.1 to 4.7%) |
2012–2021 |
4.4% (4.1 to 4.7%) |
0.15 |
||||||
|
Benign lesions |
2405 |
1760 |
2304 |
1734 |
2012–2014 |
0.8% (–6.3 to 8.5%) |
2012–2014 |
2.2% (–5.8 to 10.8%) |
0.006 |
||||||
|
|
|
|
|
|
2014–2021 |
–4.5% (–5.5 to –3.6%) |
2014–2021 |
–4.4% (–5.4 to –3.3%) |
|
||||||
|
Cryotherapy or serial curettage |
|
|
|
|
|
|
|
|
|
||||||
|
Premalignant lesion |
1958 |
1570 |
3197 |
2640 |
2012–2019 |
–1.1% (–1.4 to –0.8%) |
2012–2019 |
–1.1% (–1.4 to –0.8%) |
0.15 |
||||||
|
|
|
|
|
|
2019–2021 |
–6.8% (–8.8 to –4.8%) |
2019–2021 |
–6.8% (–8.8 to –4.8%) |
|
||||||
|
Malignant lesion |
642 |
632 |
1054 |
1028 |
2012–2019 |
2.4% (1.7 to 3.1%) |
2012–2018 |
1.9% (1.1 to 2.7%) |
0.043 |
||||||
|
|
|
|
|
|
2019–2021 |
–5.4% (–7.2 to –3.6%) |
2018–2021 |
–8.5% (–13.5 to –3.3%) |
|
||||||
|
Biopsy |
3270 |
4798 |
3337 |
5079 |
2012–2019 |
5.3% (4.6 to 6.1%) |
2012–2019 |
6.0% (5.1 to 6.9%) |
0.002 |
||||||
|
|
|
|
|
|
2019–2021 |
0.8% (–3.8 to 5.6%) |
2019–2021 |
0.2% (–4.7 to 5.3%) |
|
||||||
|
|
|||||||||||||||
|
AAPC = average annual percentage change; CI = confidence interval; MBS = Medical Benefits Schedule. * Age‐specific MBS rates standardised to the Australia 2001 standard population.18 † Segments determined by joinpoint regression. ‡ Men v women, trend for the period 2012–2021. |
|||||||||||||||
Box 3 – MBS‐subsidised skin cancer‐related services: age‐standardised rates of basal cell carcinoma/squamous cell carcinoma excisions and cryotherapy or curettage of confirmed malignant lesions, 2012– 2021, by sex*
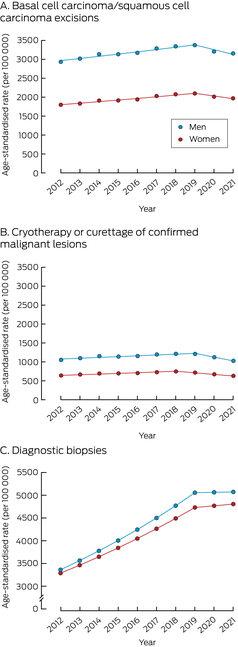
* Segments determined by joinpoint regression. See Box 1 for average annual percentage change estimates.
Box 4 – MBS‐subsidised skin cancer‐related services: age‐standardised squamous cell/basal cell carcinoma excision and biopsy rates, 2012 and 2021, and average annual percentage change, 2012–2021, by sex and state
|
Procedure |
Age standardised rate* (per 100 000) |
|
|||||||||||||
|
Women |
Men |
Women |
Men |
|
|||||||||||
|
2012 |
2021 |
2012 |
2021 |
Period† |
AAPC (95% CI) |
Period† |
AAPC (95% CI) |
P ‡ |
|||||||
|
|
|||||||||||||||
|
Squamous cell/basal cell carcinoma excisions (first excisions) |
|
|
|
|
|
|
|
|
|
||||||
|
Queensland |
3529 |
3700 |
5651 |
5809 |
2012–2019 |
1.8% (1.3 to 2.3%) |
2012–2019 |
1.4% (0.8 to 2.0%) |
0.001 |
||||||
|
|
|
|
|
|
2019–2021 |
–3.7% (–7.1 to –0.3%) |
2019–2021 |
–4.2% (–7.8 to –0.4%) |
|
||||||
|
New South Wales |
1700 |
1718 |
2822 |
2821 |
2012–2019 |
1.3% (0.4 to 2.3%) |
2012–2019 |
1.1% (0.1 to 2.1%) |
0.037 |
||||||
|
|
|
|
|
|
2019–2021 |
–4.6% (–10.8 to 2.0%) |
2019–2021 |
–4.4% (–11.0 to 2.6%) |
|
||||||
|
Victoria |
1001 |
1221 |
1548 |
1911 |
2012–2018 |
3.6% (2.7 to 4.6%) |
2012–2018 |
3.7% (2.7 to 4.6%) |
0.58 |
||||||
|
|
|
|
|
|
2018–2021 |
–1.3% (–3.6 to 1.0%) |
2018–2021 |
–1.5% (–3.7 to 0.8%) |
|
||||||
|
South Australia |
1148 |
1308 |
2010 |
2174 |
2012–2021 |
1.9% (1.1 to 2.7%) |
2012–2019 |
2.1% (1.3 to 2.9%) |
0.015 |
||||||
|
|
|
|
|
|
|
|
2019–2021 |
–2.9% (–7.7 to 2.2%) |
|
||||||
|
Western Australia |
1589 |
1923 |
2545 |
3051 |
2012–2018 |
5.1% (3.7 to 6.5%) |
2012–2018 |
4.3% (3.3 to 5.4%) |
<0.001 |
||||||
|
|
|
|
|
|
2018–2021 |
–2.2% (–5.4 to 1.2%) |
2018–2021 |
–2.5% (–4.9 to 0.0%) |
|
||||||
|
Tasmania |
1285 |
1706 |
1861 |
2403 |
2012–2021 |
3.1% (2.8 to 3.5%) |
2012–2021 |
3.1% (2.8 to 3.5%) |
0.07 |
||||||
|
Australian Capital Territory |
1119 |
1288 |
1925 |
2108 |
2012–2021 |
1.6% (1.1 to 2.2%) |
2012–2021 |
1.6% (1.1 to 2.2%) |
0.42 |
||||||
|
Northern Territory |
1835 |
1785 |
3329 |
3008 |
2012–2018 |
4.3% (2.5 to 6.1%) |
2012–2018 |
4.3% (2.5 to 6.1%) |
0.24 |
||||||
|
|
|
|
|
|
2018–2021 |
–9.8% (–13.8 to –5.5%) |
2018–2021 |
–9.8% (–13.8 to –5.5%) |
|
||||||
|
Biopsy |
|
|
|
|
|
|
|
|
|
||||||
|
Queensland |
5950 |
9136 |
6040 |
9651 |
2012–2021 |
5.0% (4.1 to 6.0%) |
2012–2021 |
5.6% (4.4 to 6.8%) |
0.004 |
||||||
|
New South Wales |
3217 |
4269 |
3455 |
4643 |
2012–2021 |
3.4% (2.7 to 4.1%) |
2012–2021 |
3.6% (2.7 to 4.4%) |
0.030 |
||||||
|
Victoria |
2096 |
3201 |
1942 |
3235 |
2012–2018 |
6.6% (4.8 to 8.4%) |
2012–2018 |
8.0% (5.6 to 10.4%) |
0.035 |
||||||
|
|
|
|
|
|
2018–2021 |
0.7% (–3.4 to 4.9%) |
2018–2021 |
0.8% (–4.3 to 6.2%) |
|
||||||
|
South Australia |
2126 |
2614 |
2037 |
2680 |
2012–2021 |
3.0% (2.6 to 3.4%) |
2012–2021 |
3.0% (2.6 to 3.4%) |
0.12 |
||||||
|
Western Australia |
2557 |
4378 |
2651 |
4581 |
2012–2019 |
7.8% (6.4 to 9.1%) |
2012–2019 |
8.0% (6.7 to 9.3%) |
0.042 |
||||||
|
|
|
|
|
|
2019–2021 |
1.4% (–5.7 to 9.1%) |
2019–2021 |
–0.2% (–7.2 to 7.3%) |
|
||||||
|
Tasmania |
2678 |
3251 |
2434 |
3241 |
2012–2015 |
7.7% (2.4 to 13.3%) |
2012–2015 |
7.7% (2.4 to 13.3%) |
0.22 |
||||||
|
|
|
|
|
|
2015–2021 |
1.3% (–0.2 to 2.8%) |
2015–2021 |
1.3% (–0.2 to 2.8%) |
|
||||||
|
Australian Capital Territory |
1805 |
2540 |
1803 |
2762 |
2012–2021 |
3.8% (2.3 to 5.3%) |
2012–2019 |
6.3% (4.5 to 8.2%) |
0.011 |
||||||
|
|
|
|
|
|
|
|
2019–2021 |
–1.0% (–10.9 to 10.1%) |
|
||||||
|
Northern Territory |
2007 |
2763 |
2505 |
3296 |
2012–2019 |
8.4% (6.2 to 10.7%) |
2012–2019 |
8.4% (6.2 to 10.7%) |
0.06 |
||||||
|
|
|
|
|
|
2019–2021 |
–9.2% (–20.4 to 3.4%) |
2019–2021 |
–9.2% (–20.4 to 3.4%) |
|
||||||
|
|
|||||||||||||||
|
AAPC = average annual percentage change; CI = confidence interval; MBS = Medical Benefits Schedule. * Age‐specific MBS rates standardised to the Australia 2001 standard population.18 † Segments determined by joinpoint regression. ‡ Men v women, trend for the period 2012–2021. |
|||||||||||||||
Box 5 – MBS‐subsidised skin cancer‐related services: age‐standardised rates and average annual percentage changes in rates of squamous cell/basal cell carcinoma excision, cryotherapy/curettage of malignant lesions, and diagnostic biopsy, 2012–2021, by age group and sex*
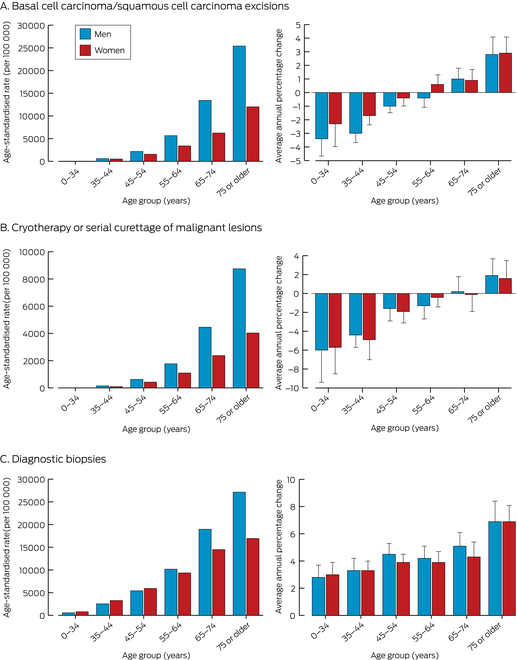
* The data for the average annual changes in rates are included in the Supporting Information, table 4.
Received 27 April 2023, accepted 30 November 2023
- Catherine M Olsen1,2
- Nirmala Pandeya1,2
- Rachel E Neale1,2
- David C Whiteman1,2
- 1 QIMR Berghofer Medical Research Institute, Brisbane, QLD
- 2 The University of Queensland, Brisbane, QLD
Open access:
Open access publishing facilitated by the University of Queensland, as part of the Wiley – the University of Queensland agreement via the Council of Australian University Librarians.
Data sharing:
The data we analysed are publicly from MBS online (http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp).
This study was supported by grants from the National Health and Medical Research Council (NHMRC; APP1073898, APP1063061, APP1185416). David Whiteman is supported by an NHMRC Research Fellowship (APP11554130). The funder played no role in the design, execution, analysis or interpretation of this study.
No relevant disclosures.
- 1. Olsen CM, Pandeya N, Green AC, et al. Keratinocyte cancer incidence in Australia: a review of population‐based incidence trends and estimates of lifetime risk. Public Health Res Pract 2022; 32: 3212203.
- 2. Australian Institute of Health and Welfare. Disease expenditure in Australia 2019–20 [here: table 5]. Updated 2 Dec 2022. https://www.aihw.gov.au/reports/health‐welfare‐expenditure/disease‐expenditure‐in‐australia‐2019‐20/data (viewed Jan 2023).
- 3. Ragaini BS, Blizzard L, Newman L, et al. Temporal trends in the incidence rates of keratinocyte carcinomas from 1978 to 2018 in Tasmania, Australia: a population‐based study. Discov Oncol 2021; 12: 30.
- 4. Kwiatkowska M, Ahmed S, Ardern‐Jones M, et al. An updated report on the incidence and epidemiological trends of keratinocyte cancers in the United Kingdom 2013–2018. Skin Health Dis 2021; 1: e61.
- 5. Stang A, Khil L, Kajüter H, et al. Incidence and mortality for cutaneous squamous cell carcinoma: comparison across three continents. J Eur Acad Dermatol Venereol 2019; 33 (Suppl 8): 6‐10.
- 6. Tokez S, Hollestein L, Louwman M, et al. Incidence of multiple vs first cutaneous squamous cell carcinoma on a nationwide scale and estimation of future incidences of cutaneous squamous cell carcinoma. JAMA Dermatol 2020; 156: 1300‐1306.
- 7. Robsahm TE, Helsing P, Veierød MB. Cutaneous squamous cell carcinoma in Norway 1963–2011: increasing incidence and stable mortality. Cancer Med 2015; 4: 472‐480.
- 8. Kappelin J, Green AC, Ingvar Å, et al. Incidence and trends of basal cell carcinoma in Sweden: a population‐based registry study. Br J Dermatol 2022; 186: 963‐969.
- 9. Adalsteinsson JA, Olafsdottir E, Ratner D, et al. Invasive and in situ squamous cell carcinoma of the skin: a nationwide study in Iceland. Br J Dermatol 2021; 185: 537‐547.
- 10. Adalsteinsson JA, Ratner D, Olafsdóttir E, et al. Basal cell carcinoma: an emerging epidemic in women in Iceland. Br J Dermatol 2020; 183: 847‐856.
- 11. Aggarwal P, Knabel P, Fleischer AB. United States burden of melanoma and non‐melanoma skin cancer from 1990 to 2019. J Am Acad Dermatol 2021; 85: 388‐395.
- 12. Cancer Council Australia. Surgical treatment. In: Clinical practice guidelines for keratinocyte cancer. Oct 2020. https://www.cancer.org.au/clinical‐guidelines/skin‐cancer/keratinocyte‐cancer (viewed Jan 2023).
- 13. Thompson BS, Olsen CM, Subramaniam P, et al. Medicare claims data reliably identify treatments for basal cell carcinoma and squamous cell carcinoma: a prospective cohort study. Aust N Z J Public Health 2016; 40: 154‐158.
- 14. Olsen CM, Williams PF, Whiteman DC. Turning the tide? Changes in treatment rates for keratinocyte cancers in Australia 2000 through 2011. J Am Acad Dermatol 2014; 71: 21‐26.
- 15. Montague M, Borland R, Sinclair C. Slip! Slop! Slap! and SunSmart, 1980–2000: skin cancer control and 20 years of population‐based campaigning. Health Educ Behav 2001; 28: 290‐305.
- 16. Australian Department of Health and Ageing. Medical Benefits Schedule book. Operating from 01 January 2012 (D0557). 2011. https://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/E137A6BDE8494881CA2585FF000A72FF/$File/201201‐MBS.pdf (viewed Jan 2023).
- 17. Australian Department of Health. Medicare Benefits Schedule book. Operating from 1 January 2020 (revised 17 January 2020 to include 36 new items). 2020. https://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/8F3FA58ED97DCA35CA2584BE00111151/$File/202001‐MBS%2017Jan2020.pdf (viewed Jan 2023).
- 18. Australian Bureau of Statistics. Standard population for use in age‐standardisation statistics. In Australian demographic statistics, Mar 2013 (3101.0). 26 Sept 2013. https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3101.0Mar%202013?OpenDocument (viewed Jan 2023).
- 19. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19: 335‐351.
- 20. Kim HJ, Fay MP, Yu B, et al. Comparability of segmented line regression models. Biometrics 2004; 60: 1005‐1014.
- 21. Dinmohamed AG, Visser O, Verhoeven RHA, et al. Fewer cancer diagnoses during the COVID‐19 epidemic in the Netherlands. Lancet Oncol 2020; 21: 750‐751.
- 22. Kleemann J, Meissner M, Özistanbullu D, et al. Impact of the Covid‐19 pandemic on melanoma and non‐melanoma skin cancer inpatient treatment in Germany: a nationwide analysis. J Eur Acad Dermatol Venereol 2022; 36: 1766‐1773.
- 23. Marson JW, Maner BS, Harding TP, et al. The magnitude of COVID‐19's effect on the timely management of melanoma and nonmelanoma skin cancers. J Am Acad Dermatol 2021; 84: 1100‐1103.
- 24. Oakes AH, Boyce K, Patton C, Jain S. Rates of routine cancer screening and diagnosis before vs after the COVID‐19 pandemic. JAMA Oncol 2023; 9: 145‐146.
- 25. Iannacone MR, Green AC. Towards skin cancer prevention and early detection: evolution of skin cancer awareness campaigns in Australia. Melanoma Manag 2014; 1: 75‐84.
- 26. Tabbakh T, Volkov A, Wakefield M, Dobbinson S. Implementation of the SunSmart program and population sun protection behaviour in Melbourne, Australia: results from cross‐sectional summer surveys from 1987 to 2017. PLoS Med 2019; 16: e1002932.
- 27. Czarnecki D. The incidence of melanoma is increasing in the susceptible young Australian population. Acta Derm Venereol 2014; 94: 539‐541.
- 28. Staples MP, Elwood M, Burton RC, et al. Non‐melanoma skin cancer in Australia: the 2002 national survey and trends since 1985. Med J Aust 2006; 184: 6‐10. https://www.mja.com.au/journal/2006/184/1/non‐melanoma‐skin‐cancer‐australia‐2002‐national‐survey‐and‐trends‐1985
- 29. Australian Institute of Health and Welfare. Skin cancer in Australia (Cat. no. CAN 96). 13 July 2016. https://www.aihw.gov.au/reports/cancer/skin‐cancer‐in‐australia (viewed Jan 2023).
- 30. Thompson BS, Pandeya, N, Olsen CM, et al. Keratinocyte cancer excisions in Australia: who performs them and associated costs. Australas J Dermatol 2019; 60: 294‐300.






Abstract
Objectives: To examine recent changes in the numbers of Medicare‐subsidised keratinocyte cancer excisions, particularly for younger people exposed to primary prevention campaigns since the early 1980s.
Study design: Retrospective cohort study; analysis of administrative data.
Setting, participants: Analysis of Medicare Benefits Schedule (MBS) claims data for procedures related to the diagnosis and treatment of keratinocyte cancer in Australia, 2012–2021.
Main outcome measures: Age‐standardised rates for MBS‐subsidised claims for first surgical squamous cell carcinoma (SCC) and basal cell carcinoma (BCC) excisions, Mohs surgery, surgical excisions of benign lesions, skin biopsies, and cryotherapy or serial curettage of premalignant and malignant lesions, overall, and by sex, state/territory, and age group; average annual percentage change in rate for time intervals determined by joinpoint regression.
Results: In men, the age‐standardised rate of BCC/SCC excisions increased by 1.9% (95% confidence interval [CI], 1.4–2.4%) per year during 2012–2019 (from 2931 to 3371 per 100 000 men) and then declined by 3.8% (95% CI, 0.5–7.0%) per year during 2019–2021 (to 3152 per 100 000). In women, the age‐standardised rate increased by 2.2% (95% CI, 1.7–2.8%) per year during 2012–2019 (from 1798 to 2093 per 100 000 women); the decline to 1967 excisions per 100 000 women in 2021 was not statistically significant. BCC/SCC excision rates declined for men under 55 years of age (by 1.0–3.4% per year) and women under 45 years of age (by 1.7–2.3% per year). Age‐standardised biopsy rates increased during 2012–2021 in all age groups (by 2.8–6.9% per year).
Conclusions: Rates of MBS‐subsidised treatment for keratinocyte cancers increased during 2012–2019, but BCC/SCC treatment rates declined among younger Australians, who have probably been exposed to less sunlight than earlier generations because of public health interventions and population‐wide lifestyle changes related to technology use.