Cardiovascular disease (CVD) accounts for significant morbidity and premature mortality in Australia. In 2020, ischaemic heart disease and cerebrovascular disease were two of the top three most common causes of death nationally.1,2
A person's risk of developing CVD depends on the combined effect of multiple factors influencing risk, including a broad range of social and environmental determinants within and across populations. Risk assessment integrating multiple factors is fundamental to the primary prevention of CVD and superior in predicting risk compared with assessment of single risk factors in isolation.2 It supports shared decision making with patients about their cardiovascular risk, helps target pharmacotherapy to those who will benefit most, and informs clinical decision making.
It has been more than a decade since the guideline for the assessment of absolute CVD risk was released in 2012. It used a Framingham‐based risk equation,3 which now overestimates risk in the general population and underestimates risk in First Nations populations.4 Although use of country‐specific CVD risk equations is increasingly favoured globally, Australia does not have a contemporary representative dataset with linkage to outcomes of sufficient scale and detail for developing an Australian‐specific risk equation.5
The Australian Government Department of Health and Aged Care contracted the National Heart Foundation of Australia on behalf of the Australian Chronic Disease Prevention Alliance (represented in this project by the National Heart Foundation of Australia, Diabetes Australia, Kidney Health Australia, and the Stroke Foundation) in June 2020 to develop the new guideline, including a contemporary CVD risk prediction equation.
The new Australian guideline for assessing and managing CVD risk, together with the Aus CVD Risk Calculator, provides:
- recommendations for when and how to assess CVD risk;
- guidance and tools for using the new Aus CVD Risk Calculator;
- practical advice on how to apply the recommendations;
- tools to support communicating CVD risk;
- recommendations on how to manage CVD risk;
- a summary of the available evidence supporting the recommended approaches to risk assessment and management, together with the rationale for how evidence has been interpreted for the Australian setting; and
- specific recommendations, resources and practice points for assessing and managing CVD risk in First Nations people.
Methods
The guideline development was informed by the 2016 National Health and Medical Research Council (NHMRC) Standards for Guidelines.6 This does not imply NHMRC's formal approval of this guideline. The project was overseen by a Guideline Expert Steering Group with direct content expertise via six Expert Subgroups, and additional input from a Consumer Advisory Panel (Box 1). Expertise was sourced across the disciplines of cardiology, general practice, primary care, nephrology, neurology, endocrinology, stroke care, epidemiology, Indigenous health, nutrition, behavioural science, communication, nursing and pharmacy. Special attention was given to First Nation people's health, with both advice and oversight from the Indigenous Health Expert Subgroup and from First Nations representation on the Consumer Advisory Panel, who advised on every aspect of the guideline content development. Specific recommendations, resources and practice points for First Nations people are embedded throughout the guideline.
The Guideline Expert Steering Group determined the clinical scope of the project — primarily atherosclerotic CVD and associated consequences — and formulated the evidence review questions in the PICO (population, intervention, comparator and outcomes) framework, addressing areas of relevance to primary care in Australia, greatest uncertainties, value to current practice and significant developments in research since the publication of the previous guideline (the list of PICO questions can be accessed in the Appendix at www.cvdcheck.org.au). Teams from the Sax Institute and Bond University conducted independent clinical evidence reviews of all PICO questions, and evidence summaries were presented, reviewed and then approved by the Expert Subgroups.
Guideline recommendations were based on Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology and the evidence generated by the clinical evidence review. Strength of a recommendation for or against an intervention was determined by considering the quality of evidence, balance between benefits and harms, trade‐offs between improving survival and quality of life, uncertainty or variability in patient values and preferences, and resource considerations.8
Recommendations were assigned to the GRADE categories “high”, “moderate”, “low” or “very low” for certainty of evidence depending on the research quality and certain factors for downgrading or upgrading a GRADE category, or to the “consensus” category where supporting evidence was insufficient or of low quality and the recommendation was based on consensus and opinion of the Expert Subgroups.
The GRADE method also considered the importance of the recommendation. This allowed for a strong recommendation to be made even if the certainty of the evidence was low.8 More information about the process for developing the guideline and the recommendations is available at www.cvdcheck.org.au.
Public consultation
A public consultation process was conducted over four weeks, from 29 August to 28 September 2022. The purpose was to improve the guideline's quality, legitimacy and acceptability to end users and the public. A combination of both open and targeted consultation methods was used. Over 260 pieces of feedback were received from key health stakeholders as well as individuals. These were influential in changes made to the draft guideline.
Adapting the New Zealand PREDICT‐1° equation for Australia
Assessing and managing CVD risk using a validated risk equation is international best practice. Because of the population‐level changes in risk factors and behaviours leading to lower age‐specific incidence and prevalence of CVD, the Framingham risk equation used in the 2012 guideline's CVD risk calculator tended over time to overestimate CVD risk in the general population and underestimate CVD risk in First Nations people.5
Although it would be ideal to develop a validated risk equation derived from Australian data, there is currently a lack of large‐scale representative data on risk factors and CVD outcomes and empirical data as bases for recalibration. Consequently, we undertook a scoping of international risk prediction equations, generated data to recalibrate the selected equation, gathered evidence to guide decisions on appropriate risk treatment thresholds, and generated data for recalibrating the new risk prediction equation.5
A 2023 review used a systematic approach to evaluate the appropriateness of existing international CVD risk equations for use in Australia.5 CVD risk equations recommended in international guidelines were assessed against the following selection criteria to identify those that best meet Australia's needs:5
- use of contemporary data sources;
- incorporation of established CVD risk factors such as cholesterol, blood pressure, diabetes and smoking;
- consideration of ethnicity and social deprivation measures (to improve health equity);
- use of global CVD events and deaths as outcomes;
- population representativeness, either of the general population or the primary care population;
- excellent model performance;
- external validation in populations similar to Australia; and
- the ability to be recalibrated and modified based on Australian disease incidence and risk factor prevalence.
Of the ten risk equations reviewed based on the criteria listed above, the New Zealand (NZ) PREDICT‐1° equation9,10 was found to be the most suitable equation for assessing CVD risk in Australia.5
Recalibration of the NZ PREDICT‐1° equation for the Australian CVD risk calculator used CVD mortality data for Australia and New Zealand that were compared on age‐ and sex‐specific differences. The mortality data were defined as death due to myocardial infarction, unstable angina, other coronary artery disease, ischaemic stroke, haemorrhagic stroke, transient ischaemic attack, peripheral vascular disease, congestive heart failure, and other ischaemic CVD‐related deaths.5
Refer to Evidence supporting the choice of a new CVD risk equation5 and Appendix 4 of the guideline7 for details of evidence and processes for selecting and adapting the NZ PREDICT‐1° equation for Australia.
Recommendations
The guideline recommendations are summarised in Box 2. The full Australian guideline for assessing and managing cardiovascular disease risk and the Aus CVD Risk Calculator are available at www.cvdcheck.org.au. Significant updates since the 2012 guidelines for the management of absolute CVD risk are listed in Box 3.
Implementation
There are infographics available for health care professionals (an overview of CVD risk assessment and management is presented in Box 4, and a guideline summary is available at https://cvdcheck.org.au/for‐health‐professionals) and for the general population (https://cvdcheck.org.au/for‐the‐general‐public) to help them understand what the new guideline means for them and how their medical consultations might change as a result.
Continuing professional development activities to increase knowledge and awareness (eg, webinars for health professionals, including live demonstration of how to use the Aus CVD Risk Calculator, www.cvdcheck.org.au/calculator) have been, and will continue to be, offered to primary care providers in the months following the publication of the guideline (eg, the on‐demand webinar “CVD risk redefined: unveiling Australia's new CVD risk guideline and calculator” produced by the Heart Foundation: www.youtube.com/watch?v=1QW83BTdvfM&list=PLhrygLMD00EseWGm1t9vGgSaepKa0kd0t).
Conclusion
CVD is highly preventable with appropriate measures targeted to individuals most likely to benefit. The 2023 Australian guideline for assessing and managing cardiovascular disease risk marks a major milestone in CVD prevention in the Australian population. It represents a more accurate pathway for the early detection, clinical assessment and management of CVD risk in the Australian population. The new Aus CVD Risk Calculator and consideration of reclassification factors captures a broader range of risk factors representative of the growing evidence for personalised and effective risk prediction.
The recommendations contained in the new guideline establish an evidence‐based standard for assessing, communicating and managing CVD risk in Australia and, properly implemented, will save lives and prevent significant suffering caused by CVD.
The full the guideline and the Aus CVD Risk Calculator are available at www.cvdcheck.org.au.
Box 1 – Governance structure for the development of the Australian guideline for assessing and managing cardiovascular disease risk
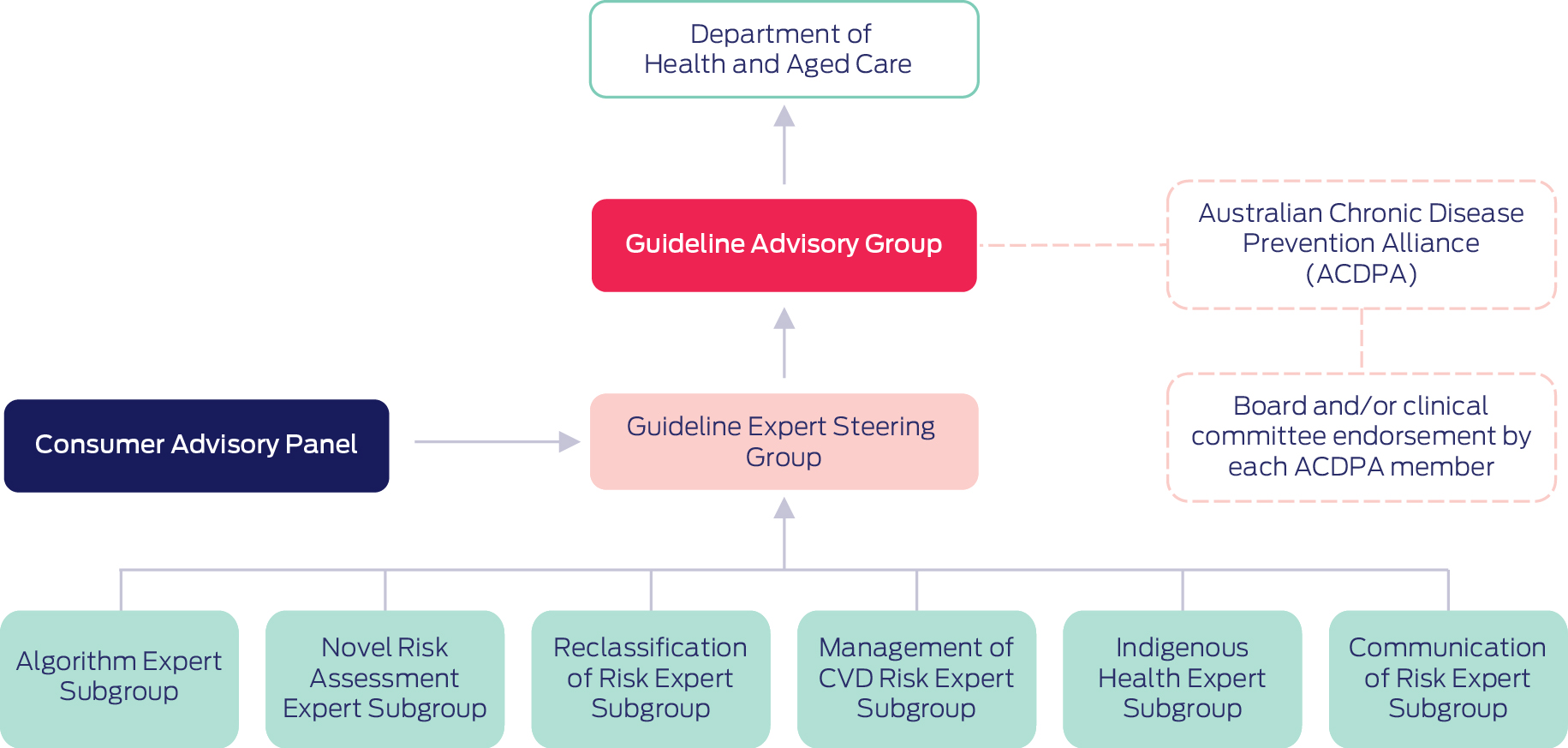
CVD = cardiovascular disease. Source: Department of Health and Aged Care, Commonwealth of Australia.7
Box 2 – Summary of guideline recommendations
|
Recommendation |
Strength* |
Certainty of evidence* |
|||||||||||||
|
|
|||||||||||||||
|
Approach to assessing CVD risk |
|||||||||||||||
|
Age ranges for assessing CVD risk |
For all people without known CVD, assess CVD risk at age 45–79 years |
Conditional |
† |
||||||||||||
|
For people with diabetes without known CVD, assess CVD risk from age 35 years |
Conditional |
† |
|||||||||||||
For First Nations people without known CVD:
|
Consensus |
|
|||||||||||||
|
Identify people at clinically determined high risk |
Assess CVD risk as high for people with moderate to severe CKD meeting any of these criteria:
|
Consensus |
|
||||||||||||
|
Assess CVD risk as high for people with a confirmed diagnosis of familial hypercholesterolaemia |
Consensus |
|
|||||||||||||
|
CVD risk assessment frequency and intervals using the Aus CVD Risk Calculator |
Intervals between reassessments of CVD risk using the Aus CVD Risk Calculator should be determined from the most recent estimated risk level |
Conditional |
Moderate |
||||||||||||
|
For people receiving pharmacological treatment to manage CVD risk, including those previously assessed as being at high risk (≥ 10%) of a cardiovascular event within 5 years, formal reassessment of CVD risk is not generally recommended, and management should be guided by the clinical context |
Conditional |
Very low |
|||||||||||||
In people with an intermediate risk (5% to < 10%) of a cardiovascular event within 5 years who are not receiving pharmacological treatment to reduce CVD risk, reassess after 2 years. Reassess earlier if any of the following apply:
|
Conditional |
Very low |
|||||||||||||
In people with a low risk (< 5%) of a cardiovascular event within 5 years who are not receiving pharmacological treatment to reduce CVD risk, reassess after 5 years. Reassess earlier if any of the following apply:
|
Conditional |
Low |
|||||||||||||
|
For First Nations people, reassess every year as part of an annual health check (or opportunistically), or at least every 2 years |
Consensus |
|
|||||||||||||
|
Consider reclassification factors |
|
|
|
||||||||||||
|
Ethnicity |
For First Nations people, consider reclassifying estimated CVD risk to a higher risk category after assessing the person's clinical, psychological and socio‐economic circumstances and community CVD prevalence |
Conditional |
Moderate |
||||||||||||
|
In people whose estimated CVD risk is close to the threshold for a higher risk category, consider reclassifying estimated CVD risk to a higher risk category for the following groups:
|
Conditional |
Moderate |
|||||||||||||
|
For people whose estimated CVD risk is close to the threshold for a lower risk category, consider reclassifying estimated CVD risk to a lower risk for people of East Asian ethnicity (Chinese, Japanese, Korean, Taiwanese or Mongolian ethnicities) |
Conditional |
Moderate |
|||||||||||||
|
Family history of premature CVD |
For people with a family history of premature CVD, consider reclassifying estimated CVD risk to a higher risk category, particularly if calculated risk is close to a higher risk threshold‡ |
Conditional |
Moderate |
||||||||||||
|
CKD |
People with moderate to severe CKD, defined as sustained eGFR < 45 mL/min/1.73 m2) or a persistent uACR > 25 mg/mmol (men) or > 35 mg/mmol (women), are at clinically determined high risk and the Aus CVD Risk Calculator should not be used. Manage as high CVD risk |
Consensus |
|
||||||||||||
|
For people who do not have diabetes§ with sustained eGFR 45–59 mL/min/1.73 m2 and/or persistent uACR > 2.5–25 mg/mmol (men) or > 3.5–35 mg/mmol (women), strongly consider reclassifying estimated CVD risk to a higher risk category, particularly if calculated risk is close to a threshold |
Strong |
High |
|||||||||||||
|
Severe mental illness |
For people living with severe mental illness, consider reclassifying estimated CVD risk to a higher risk category, particularly if calculated risk is close to a higher risk threshold¶ |
Conditional |
Moderate |
||||||||||||
|
CAC score |
CAC score is not recommended for generalised population screening for CVD risk |
Strong |
Moderate |
||||||||||||
|
Do not consider measuring CAC if:
|
Conditional |
Moderate |
|||||||||||||
|
Treatment to reduce risk is indicated in these people, regardless of the CAC result |
|||||||||||||||
When assessing CVD risk, reclassifying risk level due to CAC score can be considered when treatment decisions are uncertain, for example:
|
Conditional |
Moderate |
|||||||||||||
|
Other risk considerations |
The ankle‐brachial index should not be measured as part of a CVD risk assessment as it provides very little discrimination value beyond that of traditional CVD risk calculators |
Conditional |
Moderate |
||||||||||||
|
The high sensitivity C‐reactive protein test should not be routinely performed as part of a CVD risk assessment as it provides very little discrimination value beyond that of traditional CVD risk calculators |
Conditional |
Moderate |
|||||||||||||
|
Do not reclassify CVD risk solely due to the presence of rheumatoid arthritis |
Conditional |
Moderate |
|||||||||||||
|
Communicate risk |
|||||||||||||||
|
|
Use a relevant decision aid to support effective risk communication and enable informed decisions about reducing CVD risk |
Strong |
Moderate |
||||||||||||
|
|
Combine risk communication tools with behavioural strategies (eg, motivational interviewing, personalised goal setting and health coaching), repeated over time, to reduce overall CVD risk |
Conditional |
Low |
||||||||||||
|
|
Communicate CVD risk using a variety of formats (eg, percentages, 100‐person charts) to enable people with varying health literacy needs and learning styles to understand their risk |
Consensus |
|
||||||||||||
|
Manage CVD risk |
|||||||||||||||
|
Lifestyle** modification |
|
|
|
||||||||||||
|
Smoking cessation |
Encourage, support and advise people who smoke to quit, and refer them to a behavioural intervention (such as a smoking cessation counselling program) combined with a TGA‐approved pharmacotherapy, where clinically indicated |
Strong |
Moderate |
||||||||||||
|
Nutrition |
Advise people to follow a healthy eating pattern that is low in saturated and trans fats and incorporates plenty of vegetables, fruit and wholegrains; a variety of healthy protein‐rich foods from animal and/or plant sources; unflavoured milk, yoghurt and cheese; foods that contain healthy fats and oils (eg, olive oil, nuts, seeds and fish) |
Consensus |
|
||||||||||||
|
Consider recommending restriction of salt intake to reduce blood pressure |
Conditional |
Moderate |
|||||||||||||
|
Consider recommending the Dietary Approaches to Stop Hypertension (DASH) diet to reduce blood pressure |
Conditional |
Moderate |
|||||||||||||
|
Consider recommending a Mediterranean‐style diet to reduce risk of CVD or stroke |
Conditional |
Low/moderate†† |
|||||||||||||
|
Recommend regular consumption of oily fish to reduce risk of CHD and death due to CHD |
Strong |
Low |
|||||||||||||
|
Physical activity |
Encourage, support and advise people to do regular sustainable physical activity, such as exercise programs, to reduce their risk of CVD |
Conditional |
Low |
||||||||||||
|
Healthy weight |
Encourage, support and advise people to achieve and maintain a healthy weight |
Consensus |
|
||||||||||||
|
Alcohol reduction |
Encourage, support and advise people who consume alcohol to reduce their consumption where necessary, in line with national guidelines, to reduce health risks from drinking alcohol |
Conditional |
Low |
||||||||||||
|
Pharmacotherapy |
|
|
|
||||||||||||
|
Managing risk according to treatment thresholds |
For people at high CVD risk (estimated 5‐year risk ≥ 10% determined using the Aus CVD Risk Calculator), encourage, support and advise a healthy lifestyle** |
Conditional |
‡‡ |
||||||||||||
|
After discussing the benefits and harms of treatment, prescribe blood pressure‐lowering and lipid‐modifying pharmacotherapy, unless contraindicated or clinically inappropriate |
|||||||||||||||
|
For people at intermediate CVD risk (estimated 5‐year CVD risk 5% to < 10% determined using the Aus CVD Risk Calculator), encourage, support and advise a healthy lifestyle** |
Conditional |
‡‡ |
|||||||||||||
|
After discussing the benefits and harms of treatment, consider blood pressure‐lowering and lipid‐modifying pharmacotherapy, unless contraindicated or clinically inappropriate |
|||||||||||||||
|
|
|||||||||||||||
|
For people at low CVD risk (estimated 5‐year CVD risk < 5% determined using the Aus CVD Risk Calculator), encourage, support and advise a healthy lifestyle** |
Conditional |
‡‡ |
|||||||||||||
|
Pharmacological treatment is not routinely recommended |
|||||||||||||||
|
Some clinical situations may warrant initiation of pharmacotherapy based on individual risk factors. Very high blood pressure (ie, blood pressure > 160/100 mmHg) or very high cholesterol (ie, total cholesterol > 7.5 mmol/L) warrant initiation of blood pressure‐lowering and lipid‐modifying pharmacotherapy respectively. Refer to specific hypertension and lipid guidelines for management guidance |
Consensus |
|
|||||||||||||
|
Blood pressure‐lowering treatment |
For people at high risk of CVD (estimated 5‐year risk ≥ 10% determined using the Aus CVD Risk Calculator), prescribe blood pressure‐lowering medicines to reduce CVD risk, unless contraindicated or clinically inappropriate |
Strong |
Moderate |
||||||||||||
|
Explain the potential benefits and harms of treatment to the person and encourage shared decision making |
|||||||||||||||
|
Encourage, support and advise a healthy lifestyle** |
|||||||||||||||
|
For people at intermediate risk of CVD (estimated 5‐year CVD risk 5% to < 10% determined using the Aus CVD Risk Calculator), consider prescribing blood pressure‐lowering medicines, unless contraindicated or clinically inappropriate, to reduce CVD risk |
Strong |
Moderate |
|||||||||||||
|
Explain the potential benefits and harms of treatment to the person and encourage shared decision making |
|||||||||||||||
|
Encourage, support and advise a healthy lifestyle** |
|||||||||||||||
|
Lipid‐modifying treatment |
For people at high risk of CVD (estimated 5‐year risk ≥ 10% determined using the Aus CVD Risk Calculator), prescribe lipid‐modifying medicines to reduce CVD risk, unless contraindicated or clinically inappropriate |
Strong |
Moderate |
||||||||||||
|
Explain the potential benefits and harms of treatment to the person and encourage shared decision making |
|||||||||||||||
|
Encourage, support and advise a healthy lifestyle** |
|||||||||||||||
|
For people at intermediate risk of CVD (estimated 5‐year CVD risk 5% to < 10% determined using the Aus CVD Risk Calculator), consider prescribing lipid‐modifying medicines to reduce CVD risk, unless contraindicated or clinically inappropriate |
Strong |
Moderate |
|||||||||||||
|
Explain the potential benefits and harms of treatment to the person and encourage shared decision making |
|||||||||||||||
|
Encourage, support and advise a healthy lifestyle** |
|||||||||||||||
|
|
|||||||||||||||
|
CAC = coronary artery calcium; CHD = coronary heart disease; CKD = chronic kidney disease; CVD = cardiovascular disease; eGFR = estimated glomerular filtration rate; TGA = Therapeutic Goods Administration; uACR = urine albumin to creatinine ratio. * See Appendices at www.cvdcheck.org.au for Grading of Recommendations Assessment, Development and Evaluation (GRADE) definitions for strength and certainty of evidence. † Due to a lack of studies specifically addressing starting age, a linked evidence approach was used. ‡ Family history of premature CVD: CHD or stroke in a first degree female relative aged < 65 years or a first degree male relative aged < 55 years. § For people with diabetes, eGFR and uACR are included in the Aus CVD Risk Calculator.9,10 Suitable data were not available to include eGFR and uACR in the calculation for people without diabetes. ¶ Severe mental illness: a current or recent mental health condition requiring specialist treatment, whether received or not, in the five years prior to the CVD risk assessment. Derived from PREDICT cohort.11 ** This guideline refers to certain modifiable risk factors as “lifestyle” factors. However, it is recognised that these behaviours are not necessarily an individual's choice, but reflect the complex interplay of social, cultural and environmental factors, which may be further influenced by clinical conditions. Use of the term “lifestyle” does not attribute blame to a person. †† Low for CVD and moderate for stroke. ‡‡ The literature review found no randomised trials comparing outcomes according to different risk thresholds. Therefore, a linked evidence approach was used to answer proxy PICO questions (see Report 1: Evidence synthesis to support the development of the guidelines for absolute cardiovascular disease risk; https://d35rj4ptypp2hd.cloudfront.net/pdf/7.‐Report‐1‐Evidence‐Synthesis‐Report‐Bond‐University.pdf). |
|||||||||||||||
Box 3 – Summary of what is new in the 2023 Australian guideline for assessing and managing cardiovascular disease risk
|
What is new in the 2023 guideline? |
Details |
What the new recommendations mean for clinical practice? |
|||||||||||||
|
|
|||||||||||||||
|
Different age groups for risk assessment |
|
|
|||||||||||||
|
New Australian CVD risk calculator (Aus CVD Risk Calculator) |
|
|
|||||||||||||
|
Redefined risk categories and reassessment periods |
|
|
|||||||||||||
|
Reclassification factors |
|
|
|||||||||||||
|
Communicating risk |
|
|
|||||||||||||
|
Considerations for First Nations people |
|
|
|||||||||||||
|
Pregnancy complications |
|
||||||||||||||
|
|
|||||||||||||||
|
BMI = body mass index; CAC = coronary artery calcium; CKD = chronic kidney disease; CVD = cardiovascular disease; eGFR = estimated glomerular filtration rate; HbA1c = glycated haemoglobin; uACR = urinary albumin to creatinine ratio. * Severe mental illness: current or recent mental health condition requiring specialist treatment, whether received or not, in the five years prior to the CVD risk assessment. Derived from PREDICT cohort.11 † Family history of premature CVD: coronary heart disease or stroke in a first degree female relative aged < 65 years or a first degree male relative aged < 55 years. |
|||||||||||||||
Box 4 – Overview of cardiovascular disease (CVD) risk assessment and management
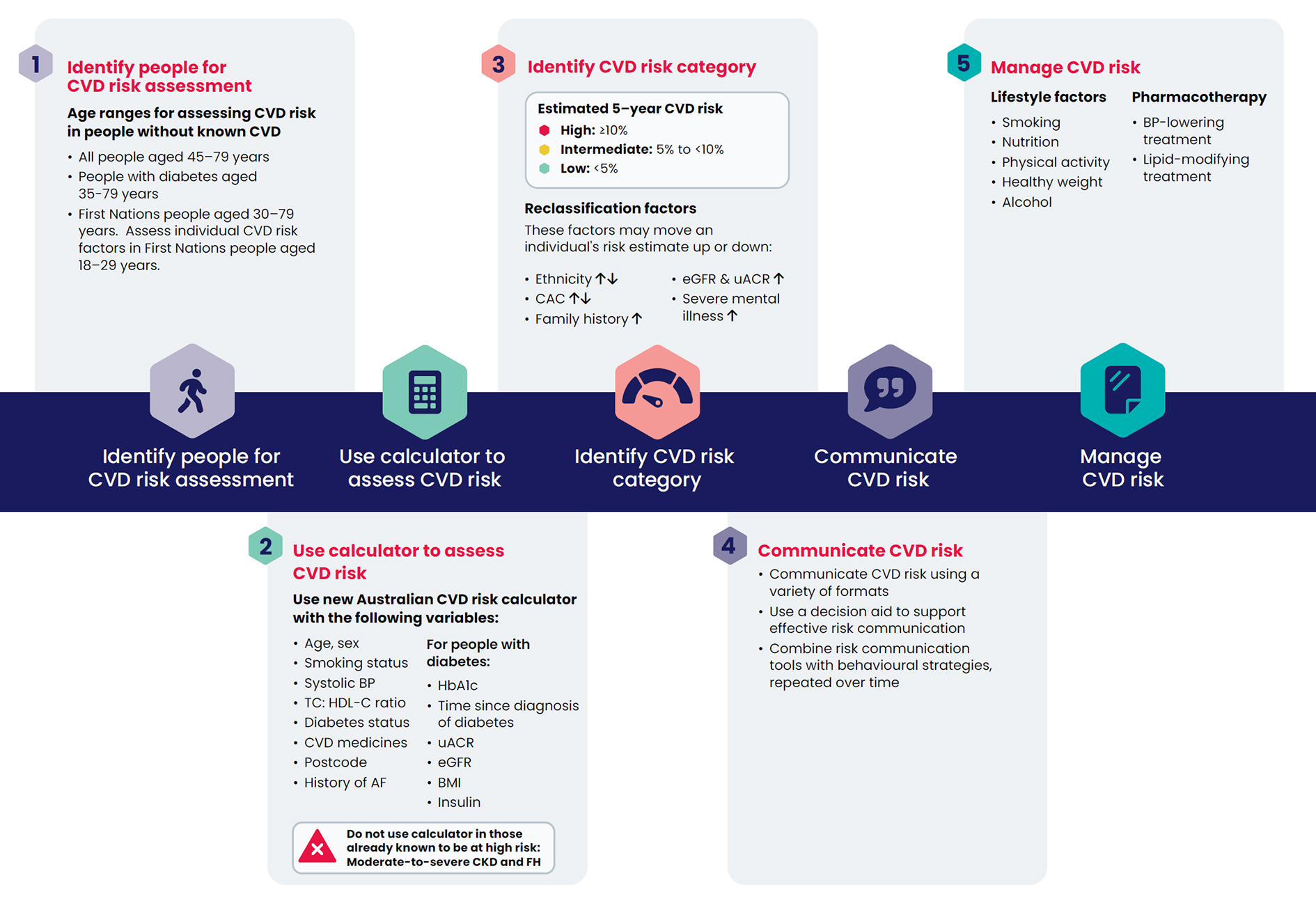
AF = atrial fibrillation; BMI = body mass index; BP = blood pressure; CAC = coronary artery calcium; CKD = chronic kidney disease; eGFR = estimated glomerular filtration rate; FH = familial hypercholesterolaemia; HbA1c = glycated haemoglobin; HDL‐C = high‐density lipoprotein cholesterol; TC = total cholesterol; uACR = urine albumin to creatinine ratio. Family history: coronary heart disease or stroke in a first degree female relative aged < 65 years or a first degree male relative aged < 55 years. Severe mental illness: a current or recent mental health condition requiring specialist treatment, whether received or not, in the five years prior to the CVD risk assessment. Derived from PREDICT cohort.11 This guideline refers to certain modifiable risk factors as “lifestyle” factors. However, it is recognised that these behaviours are not necessarily an individual's choice, but reflect the complex interplay of social, cultural and environmental factors, which may be further influenced by clinical conditions. Use of the term “lifestyle” does not attribute blame to a person. Source: Department of Health and Aged Care, Commonwealth of Australia.7
Provenance: Not commissioned; externally peer reviewed.
- Mark R Nelson1
- Emily Banks2
- Alex Brown3
- Clara K Chow4,5
- David P Peiris6
- Nigel P Stocks7
- Rebecca Davies AO8,9
- Natalie Raffoul9
- Lisa Kalman9
- Emily Bradburn9
- Garry Jennings9
- 1 University of Tasmania, Hobart, TAS
- 2 National Centre for Epidemiology and Population Health, Australian National University, Canberra, ACT
- 3 Aboriginal Health Grand Challenge, Telethon Kids Institute, Adelaide, SA
- 4 University of Sydney, Sydney, NSW
- 5 Westmead Hospital, Sydney, NSW
- 6 George Institute for Global Health, University of New South Wales, Sydney, NSW
- 7 University of Adelaide, Adelaide, SA
- 8 University of Notre Dame Australia, Sydney, NSW
- 9 Heart Foundation, Sydney, NSW
Open access:
Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
The 2023 guideline was funded by the Australian Government Department of Health and Aged Care. The Australian Government Department of Health and Aged Care contracted the National Heart Foundation of Australia (NHFA), on behalf of the Australian Chronic Disease Prevention Alliance (ACDPA) to develop the 2023 Australian guideline for assessing and managing cardiovascular disease risk. We thank Tina Garcia, Senior Medical Writer at the NHFA for providing medical writing support/editorial support in accordance with Good Publication Practice (GPP3) guidelines (www.ismpp.org/gpp3).
Emily Banks, on behalf of the Australian National University, received a National Health and Medical Research Council of Australia (NHMRC) Investigator Grant (2017742). Mark Nelson participated in the Novartis Lipid Advisory Board. Alex Brown was recipient of an NHMRC Senior Research Fellowship (APP1137563) and a Viertel Senior Medical Research Fellowship; received honoraria for AMGEN Cardiometabolic Assembly; participated in several advisory boards such as the Australian Strep A Vaccine Initiative (ASAVI), TTRA/MTPConnect Indigenous CVD and Diabetes Advisory Panel, Medical Research Future Fund (MRFF) Indigenous Health Research Fund, Rheumatic Heart Disease (RHD) Australia Novartis Incliseran Implementation Advisory Board, on the Independent Data Safety and Monitoring Board (DSMB) of INFERR (Intravenous Iron for Indigenous patients with High Ferritin Levels on Haemodialysis); board member of the Cardiac Society of Australia and New Zealand. Clara Chow is recipient of an NHMRC Investigator grant (APP1195326); was a speaker for educational events funded or organised by Novartis, Eli Lilly, Amgen, NovoNordisk, The Limbic; holds a patent for compositions for the treatment of hypertension (Patent No. 10369156); was an advisory board member for Eli Lilly; was the President of the Cardiac Society of Australia and New Zealand; was a board member of the Australian Cardiac Outcomes Registry; was Chair of the New South Wales Get Healthy Clinical Governance Committee on Adult Health Issues; was a contributor to the National Heart Foundation of Australia (NHFA)'s position statement on calcium scoring. David Peiris received Fellowship grants from the Heart Foundation (101890) and the NHMRC (1136682; 2026765); received sitting fees for participation in Heart Foundation Committee responsible for development of the 2023 Australian guideline for assessing and managing cardiovascular disease risk; and is a chief scientist at the George Institute for Global Health. Nigel Stocks received international educational grant from Pfizer to improve influenza and pneumococcal vaccination in general practice for at‐risk groups; accepted consulting fees from Pfizer in relation to treatment of cancer‐associated venous thromboembolism; was a member of Sanofi's advisory board on influenza vaccines; and was a Sequiris advisory board member. Rebecca Davies receives coaching fees from the Australian Medical Association, Catholic Cemeteries and Crematoria; serves as volunteer Director at the National Heart Foundation, Medtech Actuator, Transparency International; receives board fees as Director of Catholic Healthcare and Defence Health; is past Director of the Chris O'Brien Lifehouse; is member of boards and committees of the Catholic Archdiocese of Sydney; has personal self‐managed superannuation fund. Natalie Raffoul accepted speaker fees for presentation at educational events sponsored by Amgen and Novartis; received speaker fees and travel for Novartis Cardiology Congress (NCC); employed by the NHFA as Healthcare Programs Manager (NHFA, on behalf of the Australian Chronic Disease Prevention Alliance, received funding from the Australian Government Department of Health and Aged Care to develop and implement the 2023 Australian guideline for assessing and managing CVD risk. Lisa Kalman received funding from the NHFA to attend the Cardiac Society Conference 2023; is honorary council member of Australian Information Industry Association (AIIA); is honorary advisor to Health Policy Advisory Network of AIIA; is employed by the NHFA as Project Manager CVD Risk. Emily Bradburn is Senior Project Officer, Healthcare Programs at the NHFA; her CVD Risk Guideline project development role from 5 May 2021 to 31 July 2023 was funded by the Department of Health and Aged Care; received funding from the NHFA for attending the 71st Annual Scientific Meeting of the Cardiac Society of Australia and New Zealand in 2023. Garry Jennings is employed by the NHFA as Chief Medical Advisor; and is senior advisor to Sydney Health Partners.
- 1. Australian Bureau of Statistics. Causes of death, Australia (2021). Canberra: ABS, 2022. https://www.abs.gov.au/statistics/health/causes‐death/causes‐death‐australia/2022 (viewed Oct 2023).
- 2. Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts. Canberra: AIHW, 2023. https://www.aihw.gov.au/reports/heart‐stroke‐vascular‐disease/hsvd‐facts/contents/disease‐types (viewed Oct 2023).
- 3. National Vascular Disease Prevention Alliance. Guidelines for the management of absolute cardiovascular disease risk, 2012. https://www.heartfoundation.org.au/getmedia/4342a70f‐4487‐496e‐bbb0‐dae33a47fcb2/Absolute‐CVD‐Risk‐Full‐Guidelines_2.pdf (viewed Oct 2023).
- 4. Doust JA, Bonner C, Bell KJL. Future directions in cardiovascular disease risk prediction. Aust J Gen Pract 2020; 49: 488‐494.
- 5. Brown S, Banks E, Woodward M, et al. Evidence supporting the choice of a new cardiovascular risk equation for Australia. Med J Aust 2023; 219: 173‐186. https://www.mja.com.au/journal/2023/219/4/evidence‐supporting‐choice‐new‐cardiovascular‐risk‐equation‐australia
- 6. Australian Government Department of Health and Aged Care. Australian guideline for assessing and managing cardiovascular disease risk, 2023. About the Guideline and Calculator. How the Guideline was developed. Canberra: Commonwealth of Australia, 2023. https://www.cvdcheck.org.au/how‐the‐guideline‐was‐developed (viewed Mar 2024).
- 7. Australian Government Department of Health and Aged Care. Australian guideline for assessing and managing cardiovascular disease risk, 2023. Canberra: Commonwealth of Australia, 2023. https://www.cvdcheck.org.au/ (viewed Jan 2024).
- 8. Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE handbook [updated Oct 2013] — handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. https://gdt.gradepro.org/app/handbook/handbook.html (viewed Mar 2024).
- 9. Pylypchuk R, Wells S, Kerr A, et al. Cardiovascular disease risk prediction equations in 400 000 primary care patients in New Zealand: a derivation and validation study. Lancet 2018; 391: 1897‐1907.
- 10. Wells S, Riddell T, Kerr A, et al. Cohort profile: the PREDICT cardiovascular disease cohort in New Zealand primary care (PREDICT‐CVD 19). Int J Epidemiol 2017; 46: 22.
- 11. Cunningham R, Poppe K, Peterson D, et al. Prediction of cardiovascular disease risk among people with severe mental illness: a cohort study. PLoS One 2019; 14: e0221521.
- 12. Matsushita K, Coresh J, Sang Y, et al. Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta‐analysis of individual participant data. Lancet Diabetes Endocrinol 2015; 3: 514‐525.
- 13. Institute for Evidence‐Based Healthcare, Bond University. Evidence synthesis to support the development of guideline for cardiovascular disease risk, 2021. https://d35rj4ptypp2hd.cloudfront.net/pdf/7.‐Report‐1‐Evidence‐Synthesis‐Report‐Bond‐University.pdf (viewed Oct 2023).
- 14. National Aboriginal Community Controlled Health Organisation; Royal Australian College of General Practitioners. National guide to a preventive health assessment for Aboriginal and Torres Strait Islander people, 3rd ed. Melbourne: RACGP, 2018. https://www.racgp.org.au/FSDEDEV/media/documents/Clinical%20Resources/Resources/National‐guide‐3rd‐ed‐Sept‐2018‐web.pdf (viewed Oct 2023).
- 15. Closing the Gap. National Agreement on Closing the Gap. https://www.closingthegap.gov.au/national‐agreement (viewed Mar 2024).
- 16. Arnott C, Nelson M, Ramirez MA, et al. Maternal cardiovascular risk after hypertensive disorder of pregnancy. Heart 2020; 106: 1927‐1933.
- 17. Lo CCW, Lo ACQ, Leow SH, et al. Future cardiovascular disease risk for women with gestational hypertension: a systematic review and meta‐analysis. J Am Heart Assoc 2020; 9: e013991.






Abstract
Introduction: The 2023 Australian guideline for assessing and managing cardiovascular disease risk provides updated evidence‐based recommendations for the clinical assessment and management of cardiovascular disease (CVD) risk for primary prevention. It includes the new Australian CVD risk calculator (Aus CVD Risk Calculator), based on an equation developed from a large New Zealand cohort study, customised and recalibrated for the Australian population. The new guideline replaces the 2012 guideline that recommended CVD risk assessment using the Framingham risk equation.
Main recommendations: The new guideline recommends CVD risk assessment in people without known CVD: all people aged 45–79 years, people with diabetes from 35 years, and First Nations people from 30 years. The new Aus CVD Risk Calculator should be used to estimate and categorise CVD risk into low (< 5% risk over five years), intermediate (5% to < 10% risk over five years) or high risk (≥ 10% over five years). The following reclassification factors may be applied to recategorise calculated risk to improve accuracy of risk prediction, particularly in individuals close to a risk threshold: Indigenous status/ethnicity, estimated glomerular filtration rate, urine albumin to creatinine ratio measurements, severe mental illness, coronary artery calcium score and family history of premature CVD.
A variety of communication formats is available to communicate CVD risk to help enable shared decision making. Healthy lifestyle modification, including smoking cessation, nutrition, physical activity and limiting alcohol, is encouraged for all individuals. Blood pressure‐lowering and lipid‐modifying pharmacotherapies should be prescribed for high risk and considered for intermediate risk individuals, unless contraindicated or clinically inappropriate.
Reassessment of CVD risk should be considered within five years for individuals at low risk and within two years for those with intermediate risk. Reassessment of CVD risk is not recommended for individuals at high risk.
Changes in assessment and management as a result of the guideline: The updated guideline recommends assessment over a broader age range and uses the Aus CVD Risk Calculator, which replaces the previous Framingham‐based equation. It incorporates new variables: social disadvantage, diabetes‐specific risk markers, diagnosis of atrial fibrillation and use of blood pressure‐lowering and lipid‐modifying therapies. Reclassification factors are also a new addition.
Updated risk categories and thresholds are based on the new Aus CVD Risk Calculator. The proportion of the population in the high risk category (≥ 10% over five years) is likely to be broadly comparable to more than 15% risk from the Framingham‐based equation.
The full guideline and Aus CVD Risk Calculator can be accessed at www.cvdcheck.org.au.