Climate change has been declared the public health emergency of the 21st century. Globally, the health sector is responsible for 4.4% of greenhouse gas emissions (GHG), and 7% of national carbon emissions.1 Australia's first National Health and Climate Strategy presents a whole‐of‐government approach for addressing the health impacts of climate change and emphasises health system decarbonisation to build a net zero health system.2
In Delivering a “net zero” national health service by England's National Health Service (NHS), the authors use “scopes” to provide a useful framework to categorise GHG emissions according to their source (Box 1).3 Scope 1 emissions are directly controlled or owned by the health care facility; scope 2 emissions are indirectly generated through purchased energy, mostly electricity; and scope 3 includes all other indirect emissions from the supply chain, including production and transport of goods and services across the full supply chain.3 At present in the Australian health sector, there is a focus on transitioning to renewable energy. Although this is important, it only addresses the direct and indirect scope 1 and 2 emissions from health care's owned assets, for example, buildings and purchased operations (eg, gas for hot water, and electricity for heating and cooling).4 Modelled estimates suggest scope 1 and 2 emissions contribute approximately 30% of the emissions (of which natural gas is nearly half of a public hospital's energy supply, particularly in Victoria, New South Wales and South Australia).1,5 The remaining approximately 70% of emissions originate from the health care supply chain, including pharmaceuticals, transport and procurement, which are all examples of scope 3 emissions.1
The MJA–Lancet Countdown on health and climate change tracks progress in Australia across 37 indicators. Indicator 3.7 (Mitigation in the health sector) sets clear targets across the supply chain categories of transport, food production and consumption.6 Our analysis builds on the results of the Countdown report and discusses how the transition of the Australian health care sector to renewable energy needs to include opportunities to reduce its emissions across the health sector's supply chain (scope 3) in addition to its owned and purchased operations (scope 1 and 2).
Reducing scope 1 and 2 emissions but not scope 3 emissions
There are credible commitments and targets to transition to electric power consumption with no gas infrastructure in new Australian hospital builds in Canberra, Adelaide, Melbourne and Geelong. These goals largely address scope 1 and 2 emissions.5 Additionally, there are well established clinical examples to reduce direct emissions, including elimination of high impact anaesthetic gases (scope 1)7 and transition to low carbon asthma propellants (scope 3).3
However, health services lack critical evidence to inform decision‐making on each of the scope 3 areas (ie, supply chain aspects; pharmaceuticals, transport, procurement).6 In Australia, fewer than 50 studies have assessed the carbon footprint of items used for clinical activities and even fewer studies have incorporated purchased products and supplies.4 Among the fewer than 50 studies assessing carbon footprint, a subset comprised high quality life‐cycle analyses (LCAs), while others were of lower quality, often marked by estimations, data omissions, or erroneous application of LCA methodologies leading to imprecise comparisons.1 Thus, the current evidence surrounding health care GHG emissions is methodologically insufficient for the effective identification and prioritisation of carbon intensive scope 3 areas and mitigation strategies.
To help identify the feasibility and cost‐effectiveness of scope 3 reduction opportunities, in addition to scope 1 and 2 emissions, two key research opportunities exist. First, LCAs for categories across the health sector supply chain (scope 3) are required for baseline data.4 Second, we must integrate comprehensive environmental impact into health economic evaluations.1
Opportunities to reduce scope 3 in renewably powered health services
There is increasing recognition of the potential co‐benefits of introducing renewable energy to scope 3 areas. For example, emissions from medical equipment could be reduced in renewably powered health services by shifting from single‐use to reusable instruments. Use of infrastructural changes, such as using large washers for sterilisation purposes,8 results in economic benefits by reduced procurement costs over the life cycle of single‐use equipment9 and reduced single‐use packaging waste.8,9 Using renewable energy to power large washers can optimise the decontamination process for reusable equipment, potentially offsetting increased resource and energy consumption associated with their frequent treatment. This was demonstrated by a study revealing a reversal in greenhouse gas emissions impact when using energy mixes from the United Kingdom/European Union or the United States, instead of the assumed coal‐based Australian energy mix.8
Chemicals and gases contribute to scope 3 emissions through their procurement, transport and storage. To model the associated emission reduction potential, research is needed regarding renewably powered on‐site production of gases such as medical‐grade oxygen, and chemicals such as hydrogen peroxide for cleaning purposes.10
To reduce scope 3 emissions from staff and patient travel, there needs to be increased uptake of electric vehicles (EVs) in this sector. EVs with uncoordinated charging and network investment may inadvertently increase total electricity system costs. To best complement a renewably powered health service, there is an opportunity to optimise infrastructure and management software for EV charging with some on‐site solar capacity and battery storage.11
Food and catering services contribute up to 10% of total emissions within the health care sector.3 Renewably powered health services may develop a more sustainable approach to food services by:
- decreasing the reliance on fossil fuels to power kitchen equipment;
- reducing scope 1 and 2 emissions;
- procuring locally sourced food; and
- cooking food on‐site in kitchens powered by renewable energy to reduce scope 3 emissions associated with food transport, storage and waste across the supply chain.12
Box 2 highlights the paucity of literature and presents a review of best available evidence on priorities to reduce scope 3 emissions in renewably powered health services. The opportunities listed are adapted from the NHS.3 Box 2 is informed by relevant peer‐reviewed literature,8,9,10 sustainable health care policy frameworks, health service case studies, and policy letters.5,8,11,12,13
Recommendations and next steps
In Australia, renewable energy accounts for only 2.3% of energy used by public hospitals.14 Globally, health systems are beginning a transition to renewable energy supply. As part of this system transformation, it is in the best interest of health services to explore the many opportunities to reduce scope 3 emissions.
Health services need to develop standardised policies and metrics that incorporate environmental impacts into economic evaluations, including performing or having access to LCA data across a broad range of scope 3 areas.4 Scope 3 emissions data are important in developing evidence‐based procurement decisions as emphasised in the National Health and Climate Change Strategy.2 This is the next crucial step in the assessment and comparison of scope 3 mitigation strategies and will become increasingly relevant as the social cost of carbon is increased to better reflect real‐world impact.15
Efficient and effective decarbonisation and transition to a circular economy model will require innovation and capacity building by enhancing partnerships between health services and universities. These partnerships will allow health workers and leaders to codevelop solutions with academics from engineering, material science, implementation and system science, health economics and many other sectors. To reduce transport‐related emissions, health services should leverage their purchasing power as important fleet operators and delivery customers by opting for sustainable modes of transport and on‐site charging options powered by renewable energy.13
Collaboratively planned, renewably powered health services need to be designed to reduce the scope 3 footprint. To realise this, we urgently need to generate LCA data, foster innovation, and test mitigation strategies. The solutions will require active stewardship by health service leaders and systematic support by policy makers through national sustainability policies, their monitoring and implementation.3 Using the National Health and Climate Change Strategy, the newly established National Health Sustainability and Climate Unit may play a crucial role in establishing health, research, industry and government partnerships through strategic financial investment to bear the upfront costs and to guide regular asset replacement cycles (saving future costs to the health system).2 This perspective article outlines the need to address scope 3 decarbonisation efforts, including those related to infrastructure and the health care supply chain in Australia, in addition to scope 1 and 2 emissions.
Box 1 – Greenhouse gas emissions categorisation in the context of England's National Health Service (NHS)
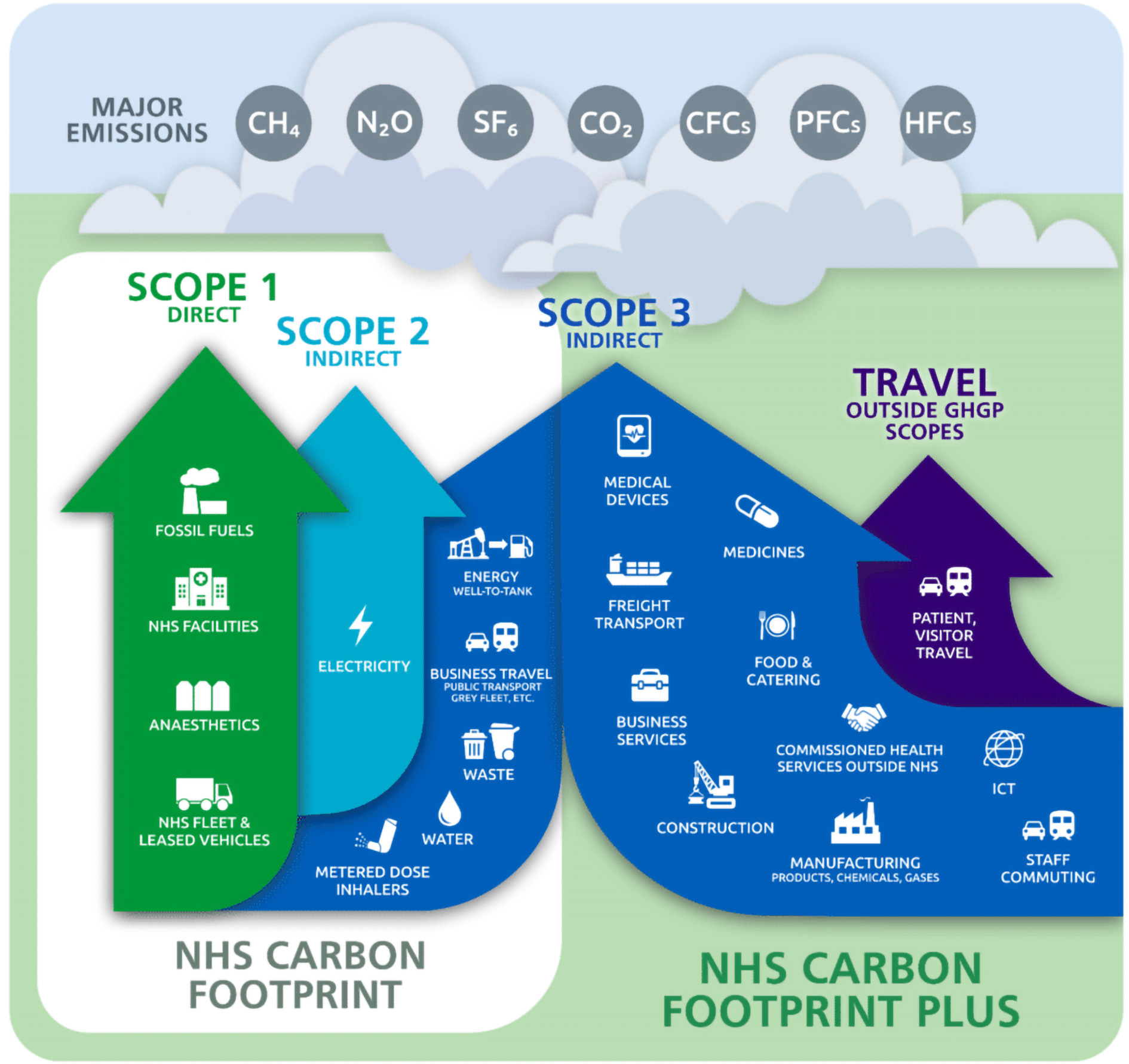
GHGP = greenhouse gas protocol; ICT = information and communications technology. Source: Figure reproduced from the NHS, England.3
Box 2 – Review of opportunities to reduce scope 3 emissions in a renewably powered health service
|
Scope 3 reduction opportunities |
Example of actions to reduce scope 3 emissions in renewably powered health services |
||||||||||||||
|
Peer‐reviewed literature |
Policy and planning frameworks |
Health service plans |
|||||||||||||
|
|
|||||||||||||||
|
Medical equipment |
Low carbon energy for sterilisation purposes: investigate the development of large washers for optimising decontamination of reusable equipment.9 |
Reusable equipment leading to waste reduction: reusable equipment sterilised in renewably powered sterilisers could also have flow‐on advantages for waste reduction.5 |
Renewable energy lower carbon footprint of processing reusable equipment: due to Australia's reliance on coal, cleaning reusable equipment in an Australian health service increases CO2 equivalent emissions by almost 10%.8 |
||||||||||||
|
Waste |
Renewable energy for combating medical waste: 100% renewable energy is a vital step in combating medical waste and tipping the balance in favour of reusables.8 |
|
|
||||||||||||
|
Manufacturing |
|
|
|
||||||||||||
|
Gases |
Medical‐grade oxygen from renewable hydrogen: oxygen is a critical health care gas and its on‐site production in health services from water as a by‐product of producing hydrogen with electrolysis in a multigeneration system is another opportunity to save costs from renewable technologies.10 |
|
|
||||||||||||
|
Chemicals |
Disinfectants for cleaning:
|
|
|
||||||||||||
|
Staff and patient commute |
|
Vehicle‐to‐grid technology for grey fleet: Hitachi chargers allow EVs to give back electricity to the grid while charging at cheaper off‐peak times.11 |
EV charging stations at hospital sites: the Royal Berkshire Hospital has set up six EV charging stations encouraging staff uptake of EVs.13 |
||||||||||||
|
Food and catering |
|
|
Reducing food miles through renewably powered on‐site kitchens: 100% renewably powered new Women's and Children's hospital (Adelaide) will include local food cooked on‐site in renewably powered kitchens to reduce emissions associated with food transport.12 |
||||||||||||
|
|
|||||||||||||||
|
CO2 = carbon dioxide; EV = electric vehicle. |
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
- 1. Malik A, Lenzen M, McAlister S, McGain F. The carbon footprint of Australian health care. Lancet Planet Health 2018; 2: 27‐35.
- 2. Department of Health and Aged Care. National health and climate strategy. Canberra: Commonwealth of Australia, 2023. https://www.health.gov.au/sites/default/files/2023‐12/national‐health‐and‐climate‐strategy.pdf (viewed Dec 2023).
- 3. National Health Service England. Delivering a ‘net zero’ National Health Service. London: NHS, 2020. https://www.england.nhs.uk/greenernhs/publication/delivering‐a‐net‐zero‐national‐health‐service/ (viewed Mar 2023).
- 4. Pickles K, Haddock R. Decarbonising clinical care in Australia: Deeble Issues Brief No.48, Canberra: Australian Healthcare and Hospitals Association, 2022. https://ahha.asn.au/system/files/docs/publications/deeble_issues_brief_no_48_decarbonising_clinical_care_final_0.pdf (viewed May 2023).
- 5. Dunne B, Forrester M, Kayak E. It's time for Australian hospitals to be all‐electric (and powered by 100% renewable energy). Med J Aust 2023; 219: 559. https://www.mja.com.au/journal/2023/219/11/its‐time‐australian‐hospitals‐be‐all‐electric‐and‐powered‐100‐renewable‐energy
- 6. Beggs PJ, Zhang Y, McGushin A, et al. The 2021 report of the MJA–Lancet Countdown on health and climate change: Australia increasingly out on a limb. Med J Aust 2021; 215: 390‐392. https://www.mja.com.au/journal/2021/215/9/2021‐report‐mja‐lancet‐countdown‐health‐and‐climate‐change‐australia
- 7. Trainee‐Led Research and Audit in Anaesthesia for Sustainable Healthcare. Desflurane is a potent greenhouse gas. Australia: TRASH, 2022. https://www.tra2sh.org/refuse‐desflurane (viewed May 2024).
- 8. McGain F, Story D, Lim T, McAlister S. Financial and environmental costs of reusable and single‐use anaesthetic equipment. Br J Anaesth 2017; 118: 862‐869.
- 9. Rizan C, Lillywhite R, Reed M, Bhutta MF. Minimising carbon and financial costs of steam sterilisation and packaging of reusable surgical instruments. Br J Surg. 2022; 109: 200‐210.
- 10. Gurieff N, Green D, Koskinen I, et al. Healthy power: reimagining hospitals as sustainable energy hubs. Sustainability 2020; https://doi.org/10.3390/su12208554
- 11. Hitachi. Hospital vehicles give back to the grid [website]. Manchester: Hitachi, 2020. https://social‐innovation.hitachi/en‐eu/stories/energy/manchester‐energy‐market/ (viewed May 2023).
- 12. Women's and Children's Health Network. New Women's and Children's Hospital Project [website]. Adelaide: Government of South Australia, 2023. https://www.newwch.sa.gov.au/timeline/nwch‐project‐reaches‐an‐australia‐first‐milestone (viewed Mar 2023).
- 13. Royal Berkshire National Health Service Foundation Trust. Our green plan 2022 to 2025. Berkshire: NHS, 2022. https://www.berkshirehealthcare.nhs.uk/media/109514074/green‐plan‐net‐zero‐n‐green‐apr‐2022‐berkshire‐healthcare.pdf (viewed June 2023).
- 14. Burch H, Anstey MH, McGain F. Renewable energy use in Australian public hospitals. Med J Aust 2021; 215: 160‐163. https://www.mja.com.au/journal/2021/215/4/renewable‐energy‐use‐australian‐public‐hospitals
- 15. Sharma S, Bressler R, Bhopal A, Norheim O. The global temperature‐related mortality impact of earlier decarbonization for the Australian health sector and economy: a modelling study. PloS One 2022; 17: 1‐10.






Open access:
Open access publishing facilitated by Deakin University, as part of the Wiley ‐ Deakin University agreement via the Council of Australian University Librarians.
No relevant disclosures.