After the World Health Organization declared the international coronavirus disease 2019 (COVID‐19) pandemic on 11 March 2020, Australian governments introduced stringent public health measures, including stay‐at‐home orders, school and business closures, and interstate border closures. During the initial restrictions period (11 March – 30 June 2020), the number of emergency department (ED) presentations in Queensland was 19.4% (95% confidence interval [CI], 17.9–20.1%) lower than predicted by pre‐pandemic data.1 We assessed the effects of these restrictions on ED presentations by three groups who experience health care inequity to determine whether specific public health approaches are required in future outbreaks to ensure that they receive appropriate emergency care.
Our retrospective observational study was part of the COVERED‐COVID project, which examined routinely collected administrative health data (Emergency Data Collection2) for presentations to 108 Queensland public EDs during 1 January 2018 – 30 June 2021.1 Here we report on presentations by three specific groups of people: Aboriginal and Torres Strait Islanders (First Nations) people (Indigenous status as listed in the Emergency Data Collection, with 99.3% data completeness; Supporting Information, part 1), people attending the 27 most remote Queensland EDs (by postcode; Australian Statistical Geography Standard Remoteness Structure3), and children under five years of age. We have previously described our analytic methods.1 Briefly, we used time series analysis to predict daily ED presentation counts on the basis of pre‐pandemic data (1 January 2018 – 10 March 2020); we report differences between predicted and actual presentation numbers during the COVID‐19 restrictions period as proportions with 95% CIs. The Gold Coast Health (LNR/2020/QGC/65436) and Griffith University (2020/567) human research ethics committees approved the COVERED‐COVID project, and our analysis of public health data complied with Public Health Act 2005 (Qld) requirements. We report our study according to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines.4
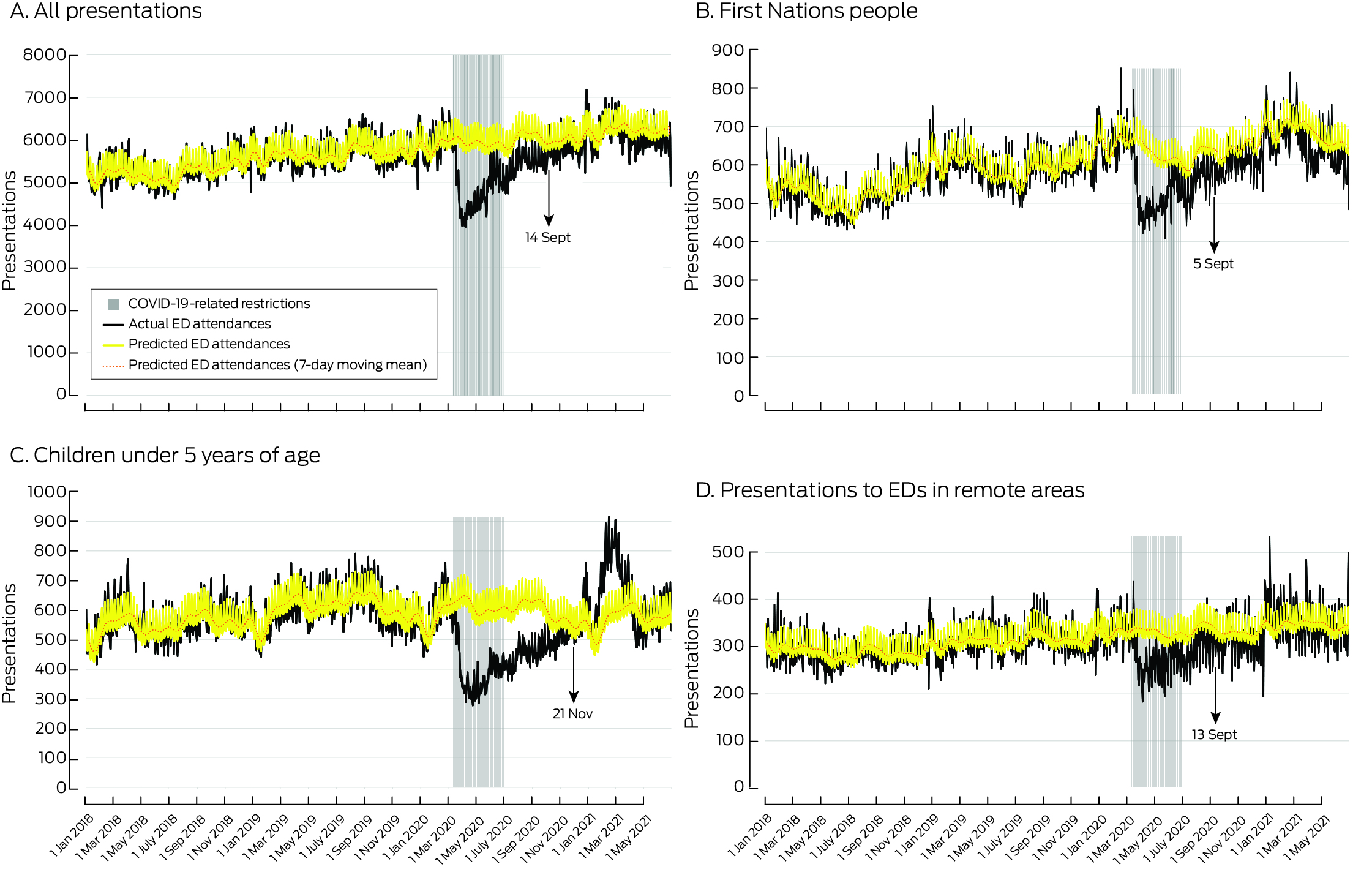
During 11 March – 30 June 2020, the daily number of ED presentations by First Nations people was 17.8% (95% CI, 12.2–22.8%) lower than predicted, and that of people in remote areas 17.8% (95% CI, 9.8–24.5%) lower; these differences were similar to the overall decline in presentations in Queensland (19.4%).1 The numbers returned to the predicted levels on 5 September for presentations by First Nations people, and on 13 September for presentations by residents of remote areas, similar to the date for the overall ED presentation number (14 September 20201). The daily number of ED presentations by children under five years of age, however, was 36.3% (95% CI, 31.0–40.9%) lower than predicted during the restrictions period, and did not return to the predicted level until 21 November 2020 (Box 1, Box 2).
Most changes in presentations by First Nations people and remote residents during 11 March – 30 June 2020 by urgency of condition (Australasian Triage Scale category, ATS5) were similar to those noted for all people attending EDs. The numbers of more urgent presentations (ATS 1 or 2) returned more quickly to expected levels than less urgent presentations, and the largest declines were in ATS 4 presentations. However, the change in the numbers of least urgent presentations (ATS 5) were smaller for First Nations people and remote residents than overall (Supporting Information, table 1, figures 1–3).
The reductions in the number of presentations by children under five years of age in the two categories of greatest urgency were larger than for the three less urgent categories: ATS 1, 40.5% (95% CI, 35.0–46.2%); ATS 2, 39.1% (95% CI, 38.2–40.0%); ATS 3, 37.2% (95% CI, 36.7–37.8%); ATS 4, 32.6% (95% CI, 32.0–33.2%); ATS 5, 23.1% (95% CI, 21.8–24.5%); Supporting Information, table 1). The number of ATS 1 presentations for children did not return to the predicted weekly level until 17 January 2021, and the number of ATS 2–4 presentations exceeded predicted levels during early 2021 (Box 2; Supporting Information, figures 4 and 5).
The effect of COVID‐19 and associated public health measures on access to Queensland public EDs was similar for all Queenslanders, First Nations people, and residents of remote areas. The fall in presentations by children under five years of age was much greater and more protracted, as also reported in other countries.6 The decline in the frequency of respiratory conditions and trauma early in the COVID‐19 pandemic1 could partially explain the reduction in ED presentation numbers. The reduced number of ED visits by children may also reflect their parents’ fear of contracting the virus and the impact of social distancing and lockdown measures.6 The large declines for more urgent ED presentations by children could reflect the effect of social distancing on the spread of respiratory pathogens. The decline in ED presentations by children was followed in January 2021 by a rise beyond pre‐pandemic levels.
Our study was performed in a country with universal health care, and our findings may not be generalisable to countries where this is not the case. Further, limitations associated with prediction models based on small daily or weekly numbers apply to some sub‐analyses (eg, ATS 1 presentations by children).
We examined ED presentations in Queensland during the initial 16 months of the COVID‐19 pandemic. Given concerns about the longer term impact of COVID‐19 on the health of children, especially those experiencing adversity, public health responses that take a community child health approach should be considered.7
Box 1 – Actual and predicted numbers of presentations to 108 public emergency departments in Queensland, 11 March – 30 June 2020: summary, overall and by specific group
|
Population group* |
Actual number |
Predicted number |
Absolute difference |
Reduction (95% CI) |
Return to predicted level† |
||||||||||
|
|
|||||||||||||||
|
All presentations1 |
4786 |
5935 |
1149 |
19.4% (17.9–20.9%) |
14 Sept 2020 |
||||||||||
|
First Nations people |
519 |
631 |
112 |
17.8% (12.2–22.8%) |
5 Sept 2020 |
||||||||||
|
Most remote emergency departments |
272 |
331 |
59 |
17.8% (9.8–24.5%) |
13 Sept 2020 |
||||||||||
|
Children under five years of age |
389 |
612 |
223 |
36.3% (31.0–40.9%) |
21 Nov 2020 |
||||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * These are not exclusive groups: individual people can be included in more than one group. † First day after initial sustained decline that was followed by ten consecutive days on which the number of presentations was within 10% of the predicted value. |
|||||||||||||||
Received 4 July 2023, accepted 16 January 2024
- 1. Sweeny AL, Keijzers G, Marshall A, et al. Emergency department presentations during the COVID‐19 pandemic in Queensland (to June 2021): interrupted time series analysis. Med J Aust 2023; 218: 120‐125. https://www.mja.com.au/journal/2023/218/3/emergency‐department‐presentations‐during‐covid‐19‐pandemic‐queensland‐june‐2021
- 2. Queensland Government. Emergency Data Collection (EDC). In: Queensland Health Information Knowledgebase (QHIK). Updated 21 Sept 2021. https://qhdd.health.qld.gov.au/apex/f?p=103:MS_DETAIL::KW:::P4_MD_ID,P4_SEQ_ID:2,26040&cs=102FA19CEDE790750706FC33BB51B42F2 (viewed Apr 2023).
- 3. Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS), volume 5: remoteness structure, July 2016 (1270.0.55.005). 16 Mar 2018. https://www.abs.gov.au/ausstats/abs@.nsf/7d12b0f6763c78caca257061001cc588/197264d1f636feb7ca258251000c8cca!OpenDocument (viewed Apr 2023).
- 4. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147: 573‐577.
- 5. Australasian College for Emergency Medicine. Triage. Undated. https://acem.org.au/Content‐Sources/Advancing‐Emergency‐Medicine/Better‐Outcomes‐for‐Patients/Triage (viewed Apr 2023).
- 6. Roland D, Gardiner A, Razzaq D, et al. REPEM network (Research in European Paediatric Emergency Medicine). Influence of epidemics and pandemics on paediatric ED use: a systematic review. Arch Dis Child 2023; 108: 115‐122.
- 7. Goldfeld S, O'Connor E, Sung V, et al. Potential indirect impacts of the COVID‐19 pandemic on children: a narrative review using a community child health lens. Med J Aust 2022; 216: 364‐372. https://www.mja.com.au/journal/2022/216/7/potential‐indirect‐impacts‐covid‐19‐pandemic‐children‐narrative‐review‐using






Open access:
Open access publishing facilitated by Griffith University, as part of the Wiley – Griffith University agreement via the Council of Australian University Librarians.
Data sharing:
The data underlying this report will be shared upon reasonable request following determination that the intended analysis complies with the ethics approval for our study.
This study was supported by the Emergency Medicine Foundation (EMSF‐008COV‐2020). The funder was not involved in any aspect of the design or conduct of the study. We acknowledge the other COVERED‐COVID study investigators: Benjamin Gerhardy (NSW Health), Gary Grant (Griffith University), David Green (Gold Coast Health), Jaimi Greenslade (Royal Brisbane and Women's Hospital and Queensland University of Technology), Emma Hall (Gold Coast Health), Ya‐Ling Huang (Southern Cross University), Philip Jones (Gold Coast Health), Andrea P Marshall (Griffith University and Gold Coast Health), Anthony Padowitz (Gold Coast Private Hospital), Jamie Ranse (Griffith University), YD Teng (Harvard Medical School, United States of America), Benjamin Walters (John Flynn Hospital and Pindara Private Hospital), and Ping Zhang (Griffith University).
All authors were employed at Gold Coast Health or Griffith University, where this study was undertaken. The views and findings presented in the article are those of the investigators and do not represent those of collaborating organisations.