Pain and pain‐related conditions are a leading cause of disability and disease burden globally,1 with one in five adults aged 45 years and over reporting persistent, ongoing pain.2 Opioids are commonly prescribed for the management of pain, and increases in the use of prescription opioids have been observed globally over recent decades, particularly in Organisation for Economic Co‐operation and Development (OECD) countries.3 In Australia, over 1.9 million adults initiate opioid therapies each year,4 with the majority of prescriptions in primary care issued for maintenance therapy in chronic non‐cancer pain.5,6 Although shown to be an effective component of the management of acute pain, opioids may not provide longer term clinically important improvements in pain or function compared with placebo or non‐opioid medications.7,8 Further, opioid use presents a significant risk of harm, with about 80% of people who take opioids for three months or more experiencing adverse effects.9
Escalating opioid use and subsequent harm has been recognised as an international public health concern. The World Health Organization has set a global goal of reducing severe avoidable medication‐related harm through its Medication Without Harm Global Patient Safety Challenge.10 Australia's response to Medication Without Harm, published in 2020, identifies opioids as one of the four medicines of focus for the Australian context.11 Health care professionals across a range of disciplines acknowledge that opioid deprescribing is a complex and challenging practice, with continued prescribing the default behaviour.12 Deprescribing is the process for medication dose reduction or cessation, supervised by a health care professional, with the goal of improving outcomes and, where relevant, managing polypharmacy.13 In Australia, existing clinical guidance focuses primarily on pain management and the prescription of analgesia.14 However, there is a need for evidence‐based guidelines that focus on the safe and effective reduction and cessation of prescribed opioids in primary care. Emerging evidence of an association between precipitous opioid tapering and overdose, suicide, and mental health crises15,16 further highlights that additional advice on deprescribing is required.
These guidelines aim to provide evidence‐based recommendations on when and how to deprescribe opioids for adults prescribed opioids for pain in primary care settings. To our knowledge, these are the first evidence‐based opioid deprescribing guidelines, offering recommendations based on the most recent scientific evidence, informed by expert opinion and stakeholder and public input.
Methods
We followed the process of developing class‐specific medication deprescribing guidelines,17 and the Appraisal of Guidelines for Research and Evaluation (AGREE) II criteria.18 We complied with the Australian 2016 National Health and Medical Research Council (NHMRC) standards for guidelines,19 and the procedures and requirements for meeting the 2011 NHMRC standard for clinical practice guidelines.20 The guideline methods are summarised hereafter (Supporting Information), with complete guideline methods available online.21,22
The Guideline Development Group was composed of 17 members who were health care professionals (general practitioners, pain specialists, addiction specialists, registered nurses, pharmacists, physiotherapists) with experience in caring for persons taking opioids and with research expertise in the field of deprescribing in Australia and internationally; methodologists with expertise in the areas of guideline development, conducting systematic reviews, and the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach; implementation experts; and organisational (NPS MedicineWise) and consumer representatives.
Two qualitative studies were conducted with health care professionals12 and with persons taking opioids23 to elucidate their beliefs and attitudes towards opioid deprescribing and identify perceived facilitators and barriers to achieving successful outcomes. The guideline development group then defined three key clinical questions for the guideline:
- Does deprescribing of opioids result in benefits or harms compared with continuation?
- What is the evidence on how to deprescribe opioids?
- Which interventions are effective to facilitate opioid deprescribing?
Systematic evidence retrieval and synthesis was conducted via an overview of systematic reviews (containing both randomised clinical trials and observational studies).24 Five databases — Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library, Excerpta Medica Database (EMBASE), Medical Literature Analysis and Retrieval System Online (MEDLINE) and PsycINFO — were searched for systematic reviews published in the past ten years examining one or more interventions for deprescribing opioids in adult populations (aged ≥ 18 years). The search strategy was intentionally broad, placing no restrictions on the type of pain, characteristics of participants, dose or duration of opioid use, or intervention setting. A supplemental search of guidelines was conducted to inform the benefits and harms of opioid deprescribing for individuals with opioid use disorders, and a supplemental search of primary literature was conducted to locate additional evidence on how to deprescribe opioids.22 The GRADE approach was applied to assess the certainty of the evidence.25 Before guideline meetings, evidence summaries with GRADE certainty of evidence ratings were circulated to the guideline development group members. The evidence was reviewed by all group members and during meetings, the group collaboratively and iteratively refined the GRADE Evidence to Decision frameworks,26 systematically considering the certainty of the evidence, the risks and benefits of deprescribing, stakeholder values and preferences, acceptability, feasibility, equity, and resource requirements. The direction (for or against) and strength of the recommendation (recommendation or conditional recommendation) were determined by consensus, and the wording of the recommendations was formulated. Where there was insufficient direct evidence to generate an evidence‐based recommendation but the guideline development group still considered it important to provide a recommendation, a consensus recommendation was formulated by the expert panel.
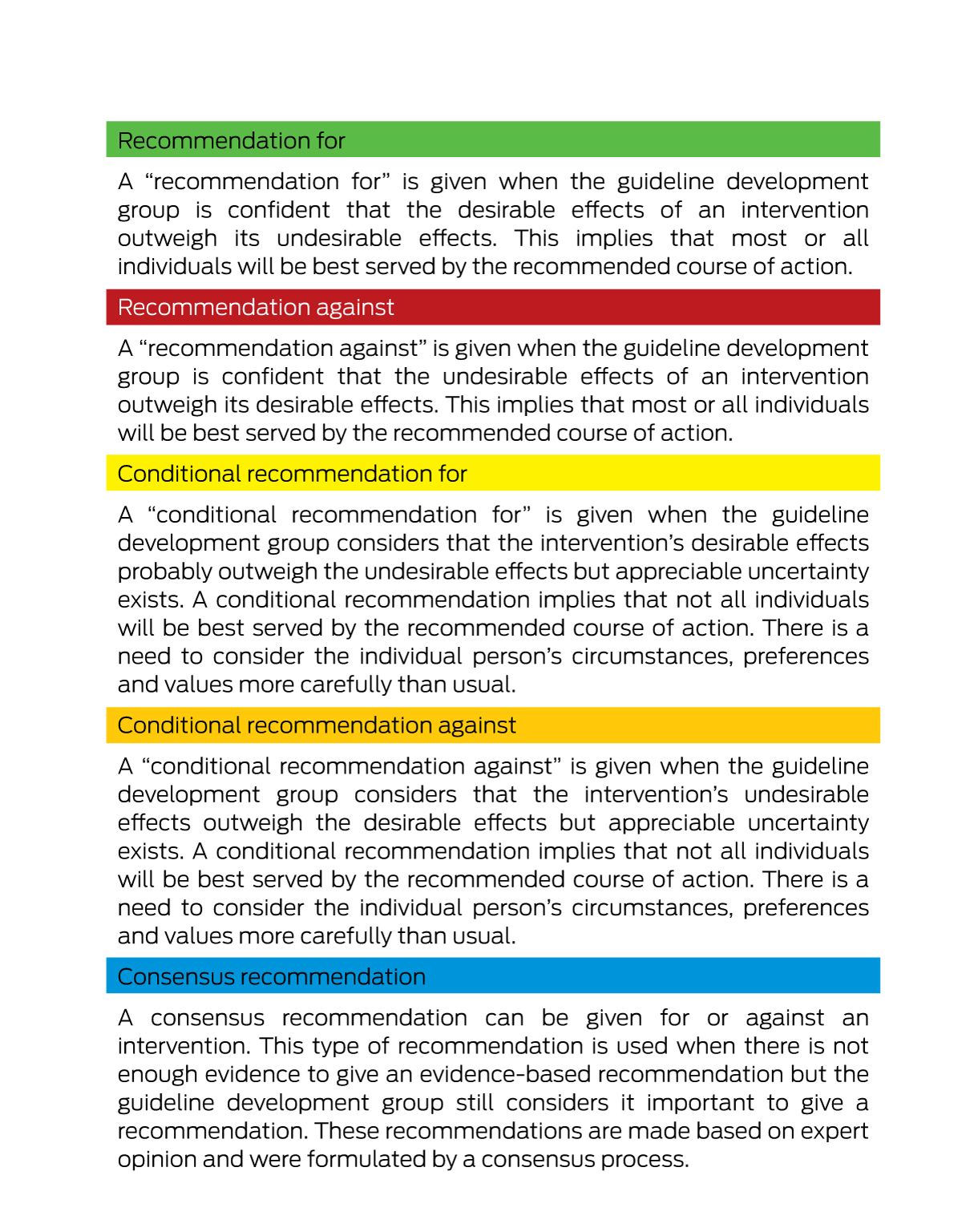
Box 1 provides an overview of each recommendation type contained within this guideline. The terminology “we recommend” is used for recommendations, and “we suggest” is used for conditional and consensus‐based recommendations.26
Three independent expert reviewers appraised the draft guideline using the AGREE II approach before its release for public consultation. Given the importance of the guideline to a wide variety of stakeholders, public consultation was undertaken for a period of 60 days from 2 February to 3 April 2022 to optimise the recommendations’ specificity, applicability, and ease of implementation. Following public consultation and externally commissioned expert and methodological review, the guideline was refined, and the final guideline recommendations were approved by the NHMRC in September 2022.
Recommendations
The eleven recommendations and accompanying practice points (Box 2) provide advice about when, how and for whom opioid deprescribing may be appropriate, while noting the need to consider the recommendations within the context of the person and their goals, values and preferences. The guideline target population is adults (≥ 18 years old) prescribed one or more opioids for any type of pain (eg, acute, chronic, cancer‐related, end‐of‐life). Persons with opioid use disorders, those with prescribed opioid substitution therapy, or people taking illicit opioids (eg, heroin) are not the target population, although there may be overlap of clinical characteristics between the identified populations. The target care setting is community primary care; however, the recommendations may be relevant to other care settings (residential care, inpatient and outpatient). Overall, the certainty of evidence informing recommendations was rated as predominantly very low to low.21,24 The full guideline28 and supporting documents are available online at www.opioiddeprescribingguideline.com/guideline.
Summary of evidence informing recommendations
The evidence informing recommendations is predominantly very low to low certainty. In the absence of high certainty evidence, guideline development groups should not fail to make a recommendation; rather, the benefits and harms of interventions, as well as patients’ values, acceptability, feasibility, equity and resource considerations, should be considered to recommend a course of action.29 Recognising the low certainty evidence informing recommendations, further research on the effectiveness and outcomes of opioid deprescribing is required.
Key clinical question 1: benefits and harms of opioid deprescribing
About 5% of opioid‐naïve patients who fill an opioid prescription transition to long term use.30 When initiating opioids, prescribing less than seven days of medication could mitigate the chance of unintentional chronic use,31 highlighting the importance of planning for deprescribing (Recommendation 1). A systematic review of opioid treatment agreements found weak evidence to support the effectiveness of patient–prescriber agreements in the reduction and mitigation of opioid misuse.32 However, there is insufficient evidence to determine whether the implementation of a deprescribing plan at the point of opioid initiation reduces use or opioid‐related harms.
Consistent low certainty evidence suggests that mean pain scores and functional measures improved, or did not significantly change, for most persons with chronic non‐cancer pain who reduced or discontinued opioids.33,34,35,36,37,38 Pain reduction following opioid deprescribing was greater for those taking higher baseline opioid doses compared with those with lower baseline doses.35 Reporting of quality of life measures was heterogeneous across reviews, but very low certainty evidence suggests that quality of life may improve with opioid deprescribing (Recommendation 2).33,35,39 Some reviews reported decreased opioid‐related adverse effects such as dry mouth for intervention groups compared with control groups,37 but serious harms relating to opioid deprescribing remain uncertain. There is emerging evidence that opioid tapering, particularly when precipitous or involuntary in nature, may increase the risk of substance use, emotional dysregulation, opioid overdose, and suicide.15,16,35
Relevant literature on opioid use in cancer‐survivor populations (those with a history of cancer who are beyond the acute diagnosis and treatment phase) provided limited evidence to support the safety and efficacy of long term opioid use.40 Adverse effects from long term opioid use, including sexual dysfunction, immune system effects, fatigue and osteoporosis have been identified in this population,41 as well as similar rates of prescription opioid misuse when compared with individuals without cancer (Recommendation 3).42 Although there is a paucity of evidence regarding the benefits and harms of opioid deprescribing in specific populations (eg, individuals with comorbid conditions that may increase the risk of opioid‐related harms, such as chronic obstructive pulmonary disease; concomitant use of medicines or substances with sedating effects; high doses of prescribed opioids), there is evidence of increased risk of opioid‐related harms in each of the identified populations (Recommendation 4).43,45
Opioids are used to relieve pain and/or breathlessness for persons nearing the end of life, and there is insufficient evidence to inform the benefits and harms of opioid deprescribing for this population (Recommendation 5).24 Existing clinical practice guidelines recommend against opioid deprescribing as a stand‐alone strategy for individuals with opioid use disorders.46,47,48 Moderate certainty evidence indicates that for people with severe opioid use disorders, opioid deprescribing, when performed without providing access to long term opioid maintenance treatment and care, is associated with elevated risk of harm and death from drug overdose.46 Further, opioid agonist or partial agonist treatment with methadone or buprenorphine maintenance therapy has been shown to be more effective in preventing relapse than opioid withdrawal and cessation (Recommendation 6).49,50
Key clinical question 2: how to deprescribe opioids
Withdrawal signs and symptoms (eg, craving, anxiety, insomnia, abdominal pain, vomiting, diarrhoea, diaphoresis, mydriasis, tremor, tachycardia) are likely to occur when opioids are withdrawn abruptly.51 The adverse physical, psychological and social outcomes of abrupt reduction or discontinuation of opioids include withdrawal effects, pain exacerbation, related loss of function and quality of life, psychological distress, hospitalisation, accidental overdose, and suicide.52,53,54 One cohort study of people prescribed 120 mg oral morphine equivalent daily dose or more of long term opioid therapy found each additional week of gradual tapering to discontinuation was associated with a 7% reduction in risk of an opioid‐related emergency department visit or hospitalisation (Recommendation 7).53
There is insufficient evidence to determine which individual or tapering characteristics are associated with greater success of opioid deprescribing.24 Given the heterogeneity of studies examining opioid deprescribing and the limited reporting of deprescribing protocols and participant baseline characteristics, we were unable to assess the comparative effectiveness of different opioid tapering approaches. Many of the tapering schedules were not well defined,34 with some studies and reviews reporting that the tapering approach was tailored to the specific participant's needs (Recommendation 8).35,55 There was limited evidence regarding the management of individuals who experienced unsuccessful opioid deprescribing attempts or did not complete tapers, as these populations were often excluded from study analysis.
The evidence informing the benefits and harms of opioid deprescribing, which demonstrated improvements in pain, function and quality of life, were largely derived from studies involving voluntary opioid deprescribing.33,35 Evidence of increased harms (suicide, overdose, illicit opioid use) in the context of involuntary opioid deprescribing informed the need for voluntary opioid deprescribing where possible.56 There is emerging evidence of an association between opioid deprescribing and overdose, suicide and mental health crises due to cognitive and psychological withdrawal effects.15,16,52 Therefore, frequent and close monitoring throughout the opioid deprescribing process is warranted to prevent or minimise potential harms (Recommendation 9).
Key clinical question 3: interventions to facilitate opioid deprescribing
Interdisciplinary, multidisciplinary and multimodal care that emphasised non‐pharmacological and self‐management strategies showed the greatest evidence for effective opioid deprescribing.33,35 Non‐pharmacological interventions in these programs included cognitive behavioural therapy and physical and occupational therapy. People receiving long term opioid therapy who voluntarily participated in intensive multidisciplinary pain management interventions that incorporated opioid tapering experienced improvements in pain severity and function.33,34,35,36,37,38 In contrast, those who tapered opioids with less intensive co‐interventions were more likely to experience unchanged pain and function (Recommendation 10).33,35
Evidence for the effectiveness of different co‐interventions to achieve opioid deprescribing for the management of chronic pain was inconclusive and varied substantially across the interventions examined.24 Consistent low certainty evidence suggests that regardless of intervention, mean pain scores and functional measures improved or did not significantly change for most persons who reduced or discontinued opioids.33,34,35,36,37,38,39,57,58,59 Improved quality of life may accompany opioid dose reduction when using deprescribing co‐interventions, but the evidence is very low certainty (Recommendation 11).24,33,35,39
Additional considerations
The full guideline28 addresses a range of additional relevant considerations, including how to engage a person in deprescribing, stakeholder values and preferences, cost and resources, opioid‐related stigma, characteristics of opioids, equivalent and equianalgesic opioid doses, opioid withdrawal symptoms and management, opioid‐induced hyperalgesia, legal and ethical considerations, opioid‐related harm minimisation strategies, and specific population considerations.
Implementation
We are working to translate the guideline into user‐friendly materials for distribution and use by health care professionals, health service users, professional and health service user organisations, and public health departments. An implementation toolkit is under development, and, to date, we have created a health provider‐directed conversation guide27 and a one‐page (double‐sided) guideline algorithm (Box 3).60 A health service user‐directed information leaflet is under development.
At the system level, a lack of accessible pain management services for end‐users in the face of a fragmented health system and limited resources is an ongoing barrier for the guideline recommendations to be implemented. Initiatives that may assist their implementation include increased funding and coverage for non‐pharmacological pain management treatments, improved access to medication‐assisted treatment for individuals with opioid use disorder, reimbursable time for patient counselling and payment models that improve geographical and financial access to multidisciplinary, interdisciplinary or multimodal coordinated care.
Conclusion
To our knowledge, the Evidence‐based clinical practice guideline for deprescribing opioid analgesics is the first international guideline focused on opioid deprescribing and contains NHMRC‐approved recommendations to assist general practitioners with deprescribing opioids for adults with pain. This guideline's recommendations and supporting information contribute to existing literature and guidelines on the quality use of opioids by providing explicit and evidence‐based recommendations, developed by a multidisciplinary team through a systematic and rigorous development process. Very low to low certainty evidence suggests that in specific populations, it is possible to reduce opioid use and harms without worsening pain, while maintaining or improving function and quality of life. Additional high certainty evidence is needed to strengthen existing recommendations and inform future recommendations on when, how and for whom opioid deprescribing is appropriate.
Box 1 – Classification of recommendations, adapted from the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) handbook25
Box 2 – Summary of guideline recommendations and practice points
|
Recommendation |
Key practice points |
||||||||||||||
|
|
|||||||||||||||
|
1. We suggest developing and implementing a deprescribing plan for persons being prescribed opioids at the point of opioid initiation. |
Consensus recommendation |
|
|||||||||||||
2. We suggest initiating deprescribing for persons taking opioids for chronic non‐cancer pain if (any of the following):
|
Conditional recommendation for (very low certainty evidence) |
|
|||||||||||||
3. We suggest initiating deprescribing for persons taking opioids for chronic cancer‐survivor pain if (any of the following):
|
Consensus recommendation |
|
|||||||||||||
4. We suggest considering deprescribing for persons taking opioids for chronic pain with one or more of the following clinical characteristics:
|
Consensus recommendation |
|
|||||||||||||
|
5. We suggest avoiding deprescribing for persons taking opioids for pain or dyspnoea who are nearing the end of life. |
Consensus recommendation |
|
|||||||||||||
|
6. We suggest avoiding opioid deprescribing for persons taking opioids with a severe opioid use disorder and suggest that evidence‐based care, such as transition to, or referral for, medication‐assisted treatment of opioid use disorder is provided. |
Conditional recommendation against (moderate certainty evidence) |
|
|||||||||||||
|
7. We recommend gradual tapering of opioids. Abrupt cessation of opioids without prior dose reduction may increase risks of harm. |
Recommendation for (low certainty evidence) |
|
|||||||||||||
|
8. We recommend tailoring the deprescribing plan based on the person's clinical characteristics, goals, and preferences. |
Recommendation for (very low certainty evidence) |
|
|||||||||||||
|
9. We suggest conducting regular monitoring and review of a person taking opioids throughout the opioid deprescribing process. Response against agreed therapeutic goals contained in a deprescribing plan should be regularly assessed. |
Consensus recommendation |
|
|||||||||||||
|
10. When available, we suggest the use of interdisciplinary or multidisciplinary care, or a multimodal approach that emphasises non‐pharmacological and self‐management strategies to deprescribe opioids. |
Conditional recommendation for (low certainty evidence) |
|
|||||||||||||
|
11. We suggest the consideration of evidence‐based co‐interventions to support opioid deprescribing. |
Conditional recommendation for (very low certainty evidence) |
|
|||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – Opioid deprescribing guideline algorithm60
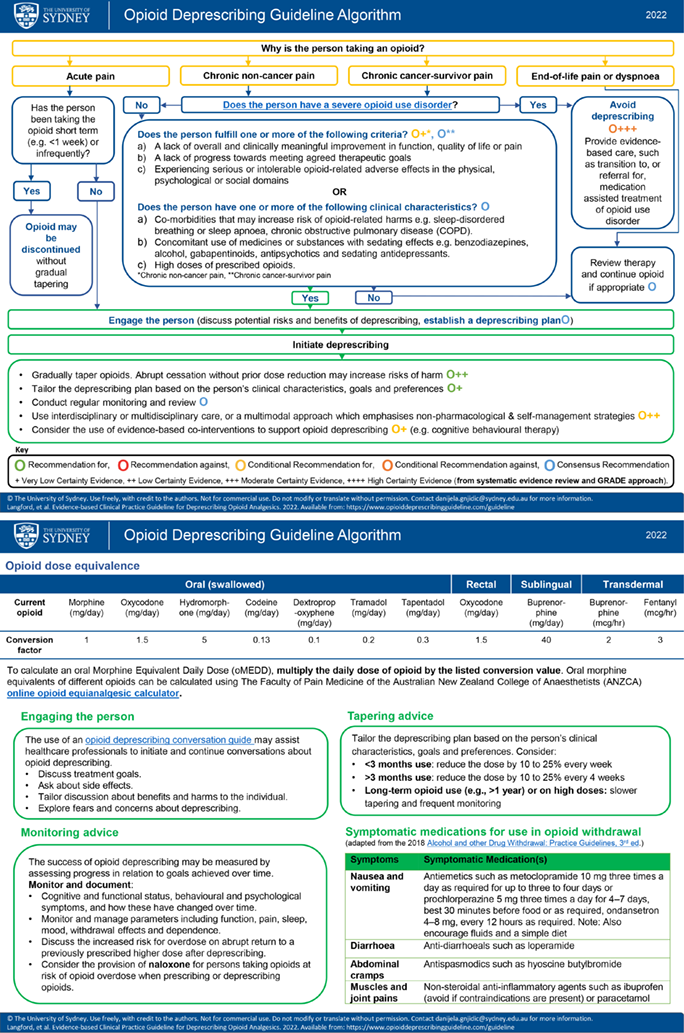
Source: Figure adapted and reproduced with permission from the Faculty of Pain Medicine, Australian and New Zealand College of Anaesthetists — Opioid Calculator (http://www.opioidcalculator.com.au/).
Provenance: Not commissioned; externally peer reviewed.
- Aili V Langford1,2
- Christine CW Lin3
- Lisa Bero4
- Fiona M Blyth2
- Jason Doctor5
- Simon Holliday6
- Yun‐Hee Jeon2
- Joanna Moullin7
- Bridin Murnion2,8
- Suzanne Nielsen9
- Rawa Osman10
- Jonathan Penm2,11
- Emily Reeve1,12
- Sharon Reid2
- Janet Wale13
- Carl R Schneider*2
- Danijela Gnjidic*2
- 1 Centre for Medicine Use and Safety, Monash University, Melbourne, VIC
- 2 University of Sydney, Sydney, NSW
- 3 Institute for Musculoskeletal Health, University of Sydney, Sydney, NSW
- 4 Center for Bioethics and Humanities, University of Colorado, Aurora (CO), USA
- 5 University of Southern California, Los Angeles (CA), USA
- 6 University of Newcastle, Newcastle, NSW
- 7 Curtin University, Perth, WA
- 8 Western Sydney Local Health District, Sydney, NSW
- 9 Monash Addiction Research Centre, Monash University, Melbourne, VIC
- 10 NPS MedicineWise, Sydney, NSW
- 11 Prince of Wales Hospital and Community Health Services, Sydney, NSW
- 12 University of South Australia, Adelaide, SA
- 13 Melbourne, VIC
Open access:
Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
Aili Langford was funded by a Research Training Program Scholarship and Supplementary Scholarship from the University of Sydney throughout her PhD candidature. The research team were awarded a 2019 Sydney Pharmacy School, Faculty of Medicine and Health, University of Sydney Research Support Grant. Christine Lin is funded by a National Health and Medical Research Council (NHMRC) Investigator Grant (1193939). Danijela Gnjidic is funded by the NHMRC Dementia Leadership Fellowship (1136849). Emily Reeve is funded by an NHMRC Investigator Grant (1195460). Suzanne Nielsen is funded by an NHMRC Career Development Fellowship (1163961). The funding bodies/sources had no role in the planning, writing or publication of this work.
We acknowledge Jack Collins (Postdoctoral Research Associate, University of Sydney) and Benita Suckling (Master of Philosophy Candidate, University of Sydney, and Pharmacist at Caboolture Hospital, Queensland Health, Brisbane) for their contributions to the synthesis and appraisal of evidence informing this guideline. We also acknowledge Steven Agiasotis (undergraduate pharmacy student, University of Sydney) for his contribution to the development of the guideline algorithm.
Emily Reeve receives royalties from UpToDate (Wolters Kluwer) for writing a chapter on deprescribing. Suzanne Nielsen has received untied educational grants from Seqirus to study prescription opioid poisoning, and was a named investigator on a buprenorphine depot implementation trial funded by Indivior, both unrelated to this work. Simon Holliday was provided an honorarium by Indivior for two presentations unrelated to this work.
- 1. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396: 1204‐1222.
- 2. Australian Institute of Health and Welfare. Chronic pain in Australia [Cat. No. PHE 267]. AIHW, 2020. https://www.aihw.gov.au/reports/chronic‐disease/chronic‐pain‐in‐australia/contents/summary (viewed June 2021).
- 3. Organisation for Economic Co‐operation and Development. Addressing problematic opioid use in OECD countries. Paris: OECD Publishing, 2019. https://www.oecd‐ilibrary.org/sites/a18286f0‐en/index.html?itemId=/content/publication/a18286f0‐en (viewed Mar 2023).
- 4. Lalic S, Ilomäki J, Bell JS, et al. Prevalence and incidence of prescription opioid analgesic use in Australia. Br J Clin Pharmacol 2019; 85: 202‐215.
- 5. Holliday S, Morgan S, Tapley A, et al. The pattern of opioid management by Australian general practice trainees. Pain Med 2015; 16: 1720‐1731.
- 6. Reid S, Day C, White N, et al. Opioid prescribing in general practice: an Australian cross‐sectional survey. BMC Prim Care 20222; 23: 171.
- 7. Busse JW, Wang L, Kamaleldin M, et al. Opioids for chronic noncancer pain: a systematic review and meta‐analysis. JAMA 2018; 320: 2448‐2460.
- 8. Krebs EE, Gravely A, Nugent S, et al. Effect of opioid vs nonopioid medications on pain‐related function in patients with chronic back pain or hip or knee osteoarthritis pain: the SPACE randomized clinical trial. JAMA 2018; 319: 872‐882.
- 9. Kalso E, Edwards JE, Moore AR, McQuay HJ. Opioids in chronic non‐cancer pain: systematic review of efficacy and safety. Pain 2004; 112: 372‐380.
- 10. World Health Organization. Medication without harm — WHO Global Patient Safety Challenge. WHO, 2017. https://www.who.int/publications/i/item/WHO‐HIS‐SDS‐2017.6 (viewed Mar 2023).
- 11. Australian Commission on Safety and Quality in Health Care. Medication without harm — WHO Global Patient Safety Challenge: Australia's response. ACSQHC, 2020. https://www.safetyandquality.gov.au/publications‐and‐resources/resource‐library/medication‐without‐harm‐who‐global‐patient‐safety‐challenge‐australias‐response (viewed Mar 2022).
- 12. Langford AV, Gnjidic D, Lin CWC, et al. Challenges of opioid deprescribing and factors to be considered in the development of opioid deprescribing guidelines: a qualitative analysis. BMJ Qual Saf 2020; 30: 133‐140.
- 13. Reeve E, Gnjidic D, Long J, Hilmer S. A systematic review of the emerging definition of ‘deprescribing’ with network analysis: implications for future research and clinical practice. Br J Clin Pharmacol 2015; 80: 1254‐1268.
- 14. Therapeutic Guidelines. Pain and Analgesia. [website]. Melbourne: Therapeutic Guidelines Limited, 2021. https://www.tg.org.au (viewed Feb 2022).
- 15. Agnoli A, Xing G, Tancredi DJ, et al. Association of dose tapering with overdose or mental health crisis among patients prescribed long‐term opioids. JAMA 2021; 326: 411‐419.
- 16. Oliva EM, Bowe T, Manhapra A, et al. Associations between stopping prescriptions for opioids, length of opioid treatment, and overdose or suicide deaths in US veterans: observational evaluation. BMJ 2020; 368: m283.
- 17. Farrell B, Pottie K, Rojas‐Fernandez CH, et al. Methodology for developing deprescribing guidelines: using evidence and GRADE to guide recommendations for deprescribing. PLoS One 2016; 11: e0161248.
- 18. Brouwers MC, Kho ME, Browman GP, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ 2010; 182: e839‐e842.
- 19. National Health and Medical Research Council. Guidelines for guidelines handbook. https://www.nhmrc.gov.au/guidelinesforguidelines (viewed Sept 2022).
- 20. National Health and Medical Research Council. Procedures and requirements for meeting the 2011 NHMRC standard for clinical practice guidelines [May 2011, version 1.1.] https://www.nhmrc.gov.au/sites/default/files/documents/reports/clinical%20guidelines/meeting‐clinical‐practice‐guidelines.pdf (viewed June 2022).
- 21. Langford AV, Schneider CR, Lin CWC, et al. Evidence‐based clinical practice guideline for deprescribing opioid analgesics: administrative report. Sydney: University of Sydney, 2022. https://www.opioiddeprescribingguideline.com/guideline (viewed Mar 2022).
- 22. Langford AV, Schneider CR, Lin CWC, et al. Evidence‐based clinical practice guideline for deprescribing opioid analgesics: technical report. Sydney: University of Sydney, 2022. https://www.opioiddeprescribingguideline.com/guideline (viewed Mar 2022).
- 23. Langford AV, Gnjidic D, Lin CWC, et al. “The lesser of two evils”: a framework analysis of consumers’ perspectives on opioid deprescribing and the development of opioid deprescribing guidelines. Pain 2021; 162: 2686‐2692.
- 24. Langford AV, Schneider CR, Lin CC, et al. Patient‐targeted interventions for opioid deprescribing: an overview of systematic reviews. Basic Clin Pharmacol Toxicol 2023; https://doi.org/10.1111/bcpt.13844 [Epub ahead of print].
- 25. Schünemann H, Brożek J, Guyatt G, Oxman A; editors. GRADE handbook [updated Oct 2013]. GRADE Working Group, 2013. https://gdt.gradepro.org/app/handbook/handbook.html (viewed Nov 2022).
- 26. Andrews JC, Schünemann HJ, Oxman AD, et al. GRADE guidelines: 15. Going from evidence to recommendation — determinants of a recommendation's direction and strength. J Clin Epidemiol 2013; 66: 726‐735.
- 27. Langford AV, Gnjidic D, Schneider CR. Communication techniques for opioid analgesic tapering conversations. Sydney: University of Sydney, 2020. https://imh.org.au/wp‐content/uploads/2021/07/Communication‐techniques‐for‐opioid‐analgesic‐tapering‐conversations.pdf (viewed Sept 2022).
- 28. Langford AV, Schneider CR, Lin CWC, et al. Evidence‐based clinical practice guideline for deprescribing opioid analgesics. Sydney: University of Sydney, 2022. https://www.opioiddeprescribingguideline.com/guideline (viewed Mar 2022).
- 29. Neumann I, Schünemann HJ. Guideline groups should make recommendations even if the evidence is considered insufficient. CMAJ 2020; 192: E23‐E24.
- 30. Deyo RA, Hallvik SE, Hildebran C, et al. Association between initial opioid prescribing patterns and subsequent long‐term use among opioid‐naïve patients: a statewide retrospective cohort study. J Gen Intern Med 2017; 32: 21‐27.
- 31. Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long‐term opioid use — United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017; 66: 265‐269.
- 32. McAuliffe Staehler TM, Palombi LC. Beneficial opioid management strategies: a review of the evidence for the use of opioid treatment agreements. Subst Abus 2020; 41: 208‐215.
- 33. Frank JW, Lovejoy TI, Becker WC, et al. Patient outcomes in dose reduction or discontinuation of long‐term opioid therapy: a systematic review. Ann Intern Med 2017; 167: 181‐191.
- 34. Fishbain DA, Pulikal A. Does opioid tapering in chronic pain patients result in improved pain or same pain vs increased pain at taper completion? A structured evidence‐based systematic review. Pain Med 2019; 20: 2179‐2197.
- 35. Mackey K, Anderson J, Bourne D, et al. Benefits and harms of long‐term opioid dose reduction or discontinuation in patients with chronic pain: a rapid review. J Gen Intern Med 2020; 35: 935‐944.
- 36. Garland EL, Manusov EG, Froeliger B, et al. Mindfulness‐oriented recovery enhancement for chronic pain and prescription opioid misuse: results from an early‐stage randomized controlled trial. J Consult Clin Psychol 2014; 82: 448‐459.
- 37. Hassan S, Zheng Q, Rizzolo E, et al. Does integrative medicine reduce prescribed opioid use for chronic pain? A systematic literature review. Pain Med 2020; 21: 836‐859.
- 38. Pollard EM, Lamer TJ, Moeschler SM, et al. The effect of spinal cord stimulation on pain medication reduction in intractable spine and limb pain: A systematic review of randomized controlled trials and meta‐analysis. J Pain Res 2019; 12: 1311‐1324.
- 39. Mathieson S, Maher CG, Ferreira GE, et al. Deprescribing opioids in chronic non‐cancer pain: systematic review of randomised trials. Drugs 2020; 80: 1563‐1576.
- 40. LeVoir A, Lee M, Fitzgibbon D, et al. Chronic opioid therapy in cancer survivors at a specialty oncology pain clinic: opioid dosing, efficacy, and safety during five years of pain management. J Pain Symptom Manage 2021; 61: 1080‐1087.
- 41. Paice JA, Portenoy R, Lacchetti C, et al. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 2016; 34: 3325‐3345.
- 42. Jairam V, Yang DX, Verma V, et al. National patterns in prescription opioid use and misuse among cancer survivors in the United States. JAMA Netw Open 2020; 3: e2013605.
- 43. Webster LR, Cochella S, Dasgupta N, et al. An analysis of the root causes for opioid‐related overdose deaths in the United States. Pain Med 2011; 12 (Suppl): S26‐S35.
- 44. Le TT, Park S, Choi M, et al. Respiratory events associated with concomitant opioid and sedative use among Medicare beneficiaries with chronic obstructive pulmonary disease. BMJ Open Respir Res 2020; 7: e000483.
- 45. Campbell G, Nielsen S, Larance B, et al. Pharmaceutical opioid use and dependence among people living with chronic pain: associations observed within the Pain and Opioids in Treatment (POINT) cohort. Pain Med 2015; 16: 1745‐1758.
- 46. Bruneau J, Ahamad K, Goyer MÈ, et al. Management of opioid use disorders: a national clinical practice guideline. CMAJ 2018; 190: E247‐E257.
- 47. Gowing L, Ali R, Dunlop A, et al. National guidelines for medication‐assisted treatment of opioid dependence. Canberra: Commonwealth of Australia, 2014. https://www.health.gov.au/resources/publications/national‐guidelines‐for‐medication‐assisted‐treatment‐of‐opioid‐dependence (viewed Feb 2022).
- 48. Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) national practice guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med 2015; 9: 358‐367.
- 49. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain — United States, 2016. JAMA 2016; 315: 1624‐1645.
- 50. Nielsen S, Larance B, Degenhardt L, et al. Opioid agonist treatment for pharmaceutical opioid dependent people. Cochrane Database Syst Rev 2016; (5): CD011117.
- 51. Lerner A, Klein M. Dependence, withdrawal and rebound of CNS drugs: an update and regulatory considerations for new drugs development. Brain Commun 2019; 1: fcz025.
- 52. Hallvik SE, El Ibrahimi S, Johnston K, et al. Patient outcomes after opioid dose reduction among patients with chronic opioid therapy. Pain 2022; 163: 83‐90.
- 53. Mark TL, Parish W. Opioid medication discontinuation and risk of adverse opioid‐related health care events. J Subst Abuse Treat 2019; 103: 58‐63.
- 54. Pergolizzi Jr JV, Raffa RB, Rosenblatt MH. Opioid withdrawal symptoms, a consequence of chronic opioid use and opioid use disorder: current understanding and approaches to management. J Clin Pharm Ther 2020; 45: 892‐903.
- 55. Bienek N, Maier C, Kaisler M, et al. Intensity of withdrawal symptoms during opioid taper in patients with chronic pain‐individualized or fixed starting dosage? Pain Med 2019; 20: 2438‐2449.
- 56. Darnall BD, Juurlink D, Kerns RD, et al. International stakeholder community of pain experts and leaders call for an urgent action on forced opioid tapering. Pain Med 2018; 20: 429‐433.
- 57. He Y, Guo X, May BH, et al. Clinical evidence for association of acupuncture and acupressure with improved cancer pain: a systematic review and meta‐analysis. JAMA Oncol 2019; 6: 271‐278.
- 58. Nielsen S, Sabioni P, Trigo JM, et al. Opioid‐sparing effect of cannabinoids: a systematic review and meta‐analysis. Neuropsychopharmacology 2017; 42: 1752‐1765.
- 59. Ratnayake CB, Bunn A, Pandanaboyana S, Windsor JA. Spinal cord stimulation for management of pain in chronic pancreatitis: a systematic review of efficacy and complications. Neuromodulation 2020; 23: 19‐25.
- 60. Langford AV, Schneider CR, Lin CWC, et al. Evidence‐based clinical practice guideline for deprescribing opioid analgesics: treatment algorithm. Sydney: University of Sydney, 2022. https://www.opioiddeprescribingguideline.com/resources (viewed Mar 2022).






Abstract
Introduction: Long term opioids are commonly prescribed to manage pain. Dose reduction or discontinuation (deprescribing) can be challenging, even when the potential harms of continuation outweigh the perceived benefits. TheEvidence‐based clinical practice guideline for deprescribing opioid analgesics was developed using robust guideline development processes and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) methodology, and contains deprescribing recommendations for adults prescribed opioids for pain.
Main recommendations: Eleven recommendations provide advice about when, how and for whom opioid deprescribing should be considered, while noting the need to consider each person's goals, values and preferences. The recommendations aim to achieve:
Changes in management as a result of these guidelines: To our knowledge, these are the first evidence‐based guidelines for opioid deprescribing. The recommendations intend to facilitate safe and effective deprescribing to improve the quality of care for persons taking opioids for pain.