The known: Population‐level information on longitudinal patterns of psychotropic medication dispensing to children and adolescents in Australia is limited.
The new: The dispensing of psychotropic medications to Australian children and adolescents doubled during 2013–2021, as did the prevalence of psychotropic polypharmacy. Dispensing rates for several psychotropic classes increased even more during the COVID‐19 pandemic, particularly for adolescent girls.
The implications: Increased dispensing of psychotropic medications to children and adolescents is concerning, given the uncertain balance between benefits and harms of these agents for young people. The appropriateness of psychotropic prescribing should be further investigated.
Psychotropic drugs — antipsychotic, antidepressant, psychostimulant, anxiolytic, and sedative and hypnotic agents — can be prescribed for children and adolescents with mental disorders, including schizophrenia, attention deficit/hyperactivity disorder (ADHD), autism, depression, and anxiety. Although psychotropic drugs can benefit children and adolescents with mental disorders, their efficacy and safety in young people is debated.1,2
Marked increases in the prescribing of psychotropic drugs for children and adolescents in recent decades3 have been attributed to the growing prevalence and incidence of mental health disorders, and to their increased diagnosis and treatment.4 However, recently reported differences between countries in prescribing rates suggests that they are not directly correlated with the prevalence of mental disorders.3 As evidence for the adverse effects of psychotropic drugs has also increased,5 concerns about potential overtreatment of children and adolescents have been expressed, particularly for those with mild illness, for whom non‐pharmacological approaches might be more appropriate.6
Given the negative psychological and behavioural effects on children and adolescents of the coronavirus disease 2019 (COVID‐19) pandemic, knowledge of patterns of psychotropic drug use has become even more pertinent.7 Increased dispensing to children and adolescents of psychotropic agents, particularly antidepressants, has been reported overseas.8,9,10
Population‐based information on longitudinal patterns of psychotropic agent dispensing for children and adolescents in Australia is limited. Evidence for increasing psychotropic use is restricted to particular types (antidepressants11 or psychostimulants12) or is based on analyses of general practice data.13 The objective of our study was therefore to determine longitudinal patterns of dispensing of antidepressant, anxiolytic, antipsychotic, psychostimulant, and hypnotic and sedative medicines to children and adolescents in Australia during 2013–2021.
Methods
We analysed data for people aged 18 years or younger in the Pharmaceutical Benefits Scheme (PBS) 10% sample dataset, a nationally representative, individual‐level extract including all PBS dispensing data for a random 10% sample of Australians eligible for PBS‐subsidised medicines.14 The PBS subsidises a broad range of medications for Australian citizens, permanent residents, and people from countries with reciprocal health care agreements.14 PBS data have been widely used in drug use research.15
Measures and statistical analysis
Psychotropic medications were identified according to Anatomical Therapeutic Chemical (ATC) classification system codes: antidepressants (N06A), anxiolytics (N05B), antipsychotics (N05A), psychostimulants (N06B), and hypnotics and sedatives (N05C) (Supporting Information, table 1).
We defined prevalent use as at least one dispensing of a medication during a calendar year, and incident use as dispensing after no dispensing of an agent from the same class during the preceding twelve months. We calculated rates of prevalent and incident use for each calendar year using the Australian Bureau of Statistics mid‐year population estimates by age.16 For incident rates, we adjusted the denominator by subtracting the number of prevalent users. People dispensed several medications from the same psychotropic class were counted only once per calendar year for estimating overall class‐specific prevalence and incidence, but each dispensing was counted for estimating the prevalence for individual medications. Analyses were stratified by gender (boys, girls) and age group (0–6 years, 7–12 years, 13–18 years). We also calculated the proportion of people dispensed a psychotropic agent from each class only once during the study period. Psychotropic polypharmacy was defined as being dispensed agents from at least two psychotropic classes within 90 days.
To evaluate changes in psychotropic use during the COVID‐19 pandemic, we initially examined longitudinal trends in annual rates, averting the need to model seasonality in dispensing and autocorrelation. We fitted linear models to the 2013–2019 annual rates, and predicted rates for 2020 and 2021 (with 95% confidence intervals, CIs); actual prevalence or incidence rates for 2020 or 2021 outside the 95% CIs were deemed statistically significant. We also calculated the proportional differences in prevalent and incident use during 2021 from the predicted values.
As the numbers of COVID‐19 cases were higher and the lockdowns more extensive in Victoria and New South Wales than in other states, we compared changes in prevalent use in these states with those elsewhere in Australia.
All analyses were conducted in SAS 9.4 and Stata/SE 16. Graphs were produced in R 4.0.4 (R Core Team 2021).
Ethics approval
This study was approved by the Monash University human research ethics committee (22877) and the Services Australia external requests evaluation committee (RMS2349).
Results
A total of 16 388 children and adolescents were dispensed at least one PBS‐subsidised psychotropic medication in 2013 (9598 boys, 59%), and 32 351 in 2021 (18 367 boys, 57%) (Supporting Information, table 2). The prevalence of psychotropic medication dispensing was 33.8 per 1000 boys and 25.2 per 1000 girls in 2013; in 2021, the prevalence was 60.0 per 1000 boys and 48.3 per 1000 girls. The prevalence of psychotropic polypharmacy was 5.4 per 1000 boys and 3.7 per 1000 girls in 2013, and 10.4 per 1000 boys and 8.3 per 1000 girls in 2021 (Box 1, Box 2).
Dispensing by psychotropic drug class: estimated prevalence, 2013 and 2021
The antidepressant dispensing rate was 11.7 per 1000 boys and 18.0 per 1000 girls in 2013; it was 20.4 per 1000 boys and 33.8 per 1000 girls in 2021. In both years, the antidepressant dispensing rate was similar for boys and girls aged 12 years or younger, but was higher for girls than boys aged 13–18 years (2013: 51.9 v 28.1 per 1000; 2021: 97.3 v 49.6 per 1000). Fluoxetine was the most frequently dispensed antidepressant (2021: boys, 53%; girls, 49% of antidepressant dispensing) (Box 1, Box 2).
The anxiolytic dispensing rate was consistently higher for girls than boys, and the respective rates were similar in 2013 and 2021. Diazepam was the most frequently dispensed anxiolytic (2021: boys and girls, 94% of anxiolytic dispensing) (Box 1, Box 2).
The psychostimulant dispensing rate was consistently higher for boys than girls (2013: 21.4 v 5.8 per 1000 in 2013; 2021: 44.0 v 17.4 per 1000). The largest differences between 2013 and 2021 were for dispensing to boys aged 0–6 years (2013: 3.2 per 1000; 2021: 7.3 per 1000) and girls aged 13–18 years (2013: 8.3 per 1000; 2021: 26.5 per 1000). The most frequently dispensed psychostimulant was methylphenidate (2013: boys, 84%, girls, 85%; 2021: boys, 71%, girls, 69% of psychostimulant dispensing) (Box 1, Box 2).
The antipsychotic dispensing rate was 5.0 per 1000 boys and 2.7 per 1000 girls in 2013; it was 6.4 per 1000 boys and 3.8 per 1000 girls in 2021. The largest differences were for dispensing to boys aged 0–6 years (2013: 0.9 per 1000; 2021: 1.3 per 1000) and girls aged 7–12 years (2013: 1.6 per 1000; 2021: 2.7 per 1000). The most frequently dispensed antipsychotics in 2021 were risperidone (boys, 78%; girls, 42%) and quetiapine (boys, 11%; girls, 39% of antipsychotic dispensing) (Box 1, Box 2).
The sedative/hypnotic dispensing rate was 0.72 per 1000 boys and 1.23 per 1000 girls in 2013; it was 0.30 per 1000 boys and 0.78 per 1000 girls in 2021. The most frequently dispensed sedative/hypnotic was temazepam (2021: boys and girls, 93% of sedative/hypnotic dispensing) (Box 1, Box 2).
Changes in incident and prevalent use, 2013–2020
The proportions of boys and girls dispensed a psychotropic medicine for whom only one dispensing was recording during 2013–2020 declined for all drug classes; the declines were most marked in boys for antidepressants (from 15% to 7%) and in girls for anxiolytics (from 70% to 60%) (Supporting Information, figure 1). The proportions of prevalent users in a given year deemed to also be incident users were relatively stable, except for the increases with respect to psychostimulant dispensing (boys: from 24% to 30%; girls: from 29% to 40%) (Supporting Information, figure 2).
Changes in prevalent use during the COVID‐19 pandemic
The prevalence of dispensing was higher during 2021 than predicted by 2013–2019 data for antidepressants (boys: +6.1%; 95% CI, 1.1–11.1%; girls: +22.2%; 95% CI, 17.4–26.9%) and psychostimulants (boys: +14.5%; 95% CI, 8.0–21.1%; girls: +27.7%; 95% CI, 18.9–36.6%), as was that of psychotropic polypharmacy for girls (+26.9%; 95% CI, 24.1–29.7%). The increases were highest among girls aged 13–18 years (antidepressants: +20.3%; 95% CI, 16.9–23.7%; psychostimulants: +39.0%; 95% CI, 27.9–50.0%; psychotropic polypharmacy: +30.9%; 95% CI, 27.8–34.0%). The prevalence of dispensing of antipsychotics was also higher than predicted for girls (+19.9%; 95% CI, 16.5–23.3%) but lower for boys (–3%; 95% CI, –5.9% to –0.2%) (Box 3, Box 4). The changes in prevalent use in Victoria and New South Wales were similar to those in other parts of Australia (Supporting Information, figures 3 to 7).
Differences in incident dispensing to girls were similar to those for prevalent dispensing. For incident dispensing to boys, The reduction in incident dispensing of antipsychotics (–14.2%; 95% CI, –21.6% to –6.9%) was larger than for prevalent dispensing, as was the increase in incident psychostimulant dispensing (+19.2%; 95% CI, 11.6–26.9%) (Box 3, Box 5).
Discussion
In our national study, we found that the prevalence of dispensing of psychotropic medication to children and adolescents was about twice as high in 2021 as in 2013 for both boys (2021: 60.0 per 1000) and girls (48.3 per 1000), as was the prevalence of psychotropic polypharmacy (2021: 10.4 per 1000 boys; 8.3 per 1000 girls). The prevalence of psychotropic dispensing was statistically significantly higher in 2021 than predicted by rates during 2013–2019, particularly for girls aged 13–18 years. Increases in incident (new) dispensing were especially marked, particularly of psychostimulants.
Our findings are similar to those of earlier Australian6,13 and overseas studies17,18 which found that the overall use of psychotropic medications by children and adolescents had increased prior to the COVID‐19 pandemic. One Australian study reported that increased prescribing of psychostimulants was the largest contributor to the increase in psychotropic dispensing to children and adolescents during 2011–2018.13 We found that the largest increases in prevalent dispensing were for psychostimulants, antidepressants, and antipsychotics. The earlier Australian study found that prescribing of sedatives/hypnotics had declined and that of anxiolytics was unchanged during 2011–2018.13 The reduction in prevalent dispensing of sedatives/hypnotics may reflect a move from prescribing psychotropic drugs to medications such as melatonin.13
We also found that increases in prevalent dispensing to children and adolescents partly reflected longer treatment duration, as indicated by marked increases in the proportions dispensed psychotropic drugs more than once during the study period.
Earlier Australian studies did not assess the prevalence of psychotropic polypharmacy,6,13 which was relatively frequent in our study (17% of people dispensed psychotropic medications in 2021). Overseas studies have reported estimated rates of psychotropic polypharmacy in children of 38% in the United States,19 45% in Finland,20 and 29% in Botswana.21 High rates of psychotropic polypharmacy raise concerns about potential drug interactions and cumulative side effects.22
Physical distancing and travel restrictions during the COVID‐19 pandemic have been profoundly disruptive, causing school closures and service interruptions, reducing access to educational, social, and wider family support networks. The significance of these disruptions is reflected by the high rates of mental health symptoms reported early in the pandemic by parents and carers of Australian children aged 4–17 years23 and the increased use of mental health support services by young people.24
Less well understood is the impact of disruptions on mental health care and the prescribing of psychotropic medications. We found no differences in dispensing rates between Victoria and New South Wales and other Australian states and territories. Differences in lockdown restrictions might have been expected to influence the dispensing of psychotropic drugs because of the correspondingly different effects on mental health and access to diagnostic and support services. One Australian study found that both prevalent (+11.7%) and new (+15.6%) antidepressant use by girls aged 10–17 years increased during the first year of the pandemic (2020).11 Our findings indicate that these increases continued into the second year of the pandemic. The prevalence of dispensing of anxiolytics, antipsychotics, and hypnotics/sedatives to girls aged 13–18 years also rose, but these rates have not been examined by other Australian population studies. Overseas, changes in psychotropic use during the pandemic include rate increases of 8–39% for some drug classes,8,9 no differences,10 and rate reductions.10
The reasons for gender‐ and age‐related differences in changes for different psychotropic classes are unclear. Higher rates of antidepressant dispensing to adolescent girls, for example, may indicate that the mental health burden of the pandemic was particularly marked in this group. Alternatively, our findings may reflect changes in prescribing behaviour during the pandemic related to more restricted access to non‐pharmacological support services.
We did not examine the appropriateness of psychotropic prescribing, but reasons for the increasing rates should be investigated to determine whether their benefits outweigh their harms, and whether these agents are being used as substitutes for mental health services and other non‐pharmacological support. Although a recent review of 48 psychotropic medications, evaluated across 52 mental disorders in children and adolescents, found considerable controlled trial evidence for their efficacy in many disorders, much of the evidence was of low quality, and effect sizes small.25 Further, both the frequent inaccessibility of primary trial data and study protocols and potential publication bias have been criticised.26 A similar review found that many psychotropic drugs, including antidepressants, antipsychotics, and psychostimulants, are associated with high rates of adverse events and medication discontinuation; for some psychotropic drugs, no or very insufficient high quality adverse event data is available,5 making assessment of the balance of their benefits and harms difficult.
Limitations
Diagnosis information was not available, and only dispensed medications subsidised by the PBS were included in our analysis. Whether dispensed medications were taken cannot be determined, but dispensing data more accurately reflect medication use than prescribing data. Changes in the proportions of medications within specific psychotropic classes dispensed may have been influenced by COVID‐19‐related medication shortages. Finally, the uncertainty of predicted dispensing rates for 2020 and 2021 based on data for 2013–2019 (broad 95% CIs) affected the ability to identify meaningful differences.
Conclusion
The prevalence of psychotropic dispensing and psychotropic polypharmacy among Australian children and adolescents were each higher in 2021 than 2013. The impact of the COVID‐19 pandemic on the prevalence of antidepressant, antipsychotic, and psychostimulant dispensing was most marked for girls aged 13–18 years. The reasons for changes in psychotropic dispensing for particular groups of young people should be further investigated, particularly in light of questions about the safety and benefit of psychotropic medications for children and adolescents.
Data availability
The study data cannot be publicly shared for reasons of ethics and privacy. Access, however, may be granted upon request to Luke Grzeskowiak if deemed appropriate. All authors had full access to all study data (including statistical reports and tables).
Box 1 – Estimated prevalence of the dispensing of psychotropic medications to boys and young men (per 1000), Australia, 2013–2021, by age group
|
|
Age group (years) |
||||||||||||||
|
|
0–6 |
7–12 |
13–18 |
All ages |
|||||||||||
|
Medication |
2013 |
2021 |
2013 |
2021 |
2013 |
2021 |
2013 |
2021 |
|||||||
|
|
|||||||||||||||
|
Any psychotropic |
4.90 |
8.62 |
45.7 |
82.3 |
57.7 |
97.3 |
33.8 |
60.0 |
|||||||
|
Psychotropic polypharmacy |
0.47 |
0.79 |
6.46 |
12.2 |
10.5 |
20.1 |
5.41 |
10.4 |
|||||||
|
Antidepressants |
1.10 |
0.76 |
8.39 |
15.2 |
28.1 |
49.6 |
11.7 |
20.4 |
|||||||
|
Amitriptyline |
0.23 |
0.11 |
1.23 |
0.77 |
2.21 |
2.21 |
1.15 |
0.97 |
|||||||
|
Escitalopram |
0.10 |
0.06 |
0.38 |
0.58 |
3.72 |
6.29 |
1.31 |
2.14 |
|||||||
|
Fluoxetine |
0.25 |
0.44 |
3.63 |
9.6 |
9.97 |
24.3 |
4.30 |
10.8 |
|||||||
|
Fluvoxamine |
0.06 |
0.03 |
1.09 |
1.20 |
2.51 |
3.27 |
1.14 |
1.40 |
|||||||
|
Sertraline |
0.12 |
0.13 |
1.20 |
3.29 |
5.64 |
12.44 |
2.16 |
4.94 |
|||||||
|
Other |
0.38 |
0.04 |
1.59 |
0.73 |
8.84 |
7.83 |
3.38 |
2.65 |
|||||||
|
Anxiolytics |
0.16 |
0.13 |
0.54 |
0.49 |
3.86 |
3.39 |
1.43 |
1.25 |
|||||||
|
Diazepam |
0.16 |
0.13 |
0.48 |
0.46 |
3.35 |
3.15 |
1.25 |
1.17 |
|||||||
|
Oxazepam |
0 |
0 |
0.05 |
0.02 |
0.45 |
0.28 |
0.15 |
0.09 |
|||||||
|
Alprazolam |
0.01 |
0 |
0.02 |
0.01 |
0.15 |
0.01 |
0.06 |
0.01 |
|||||||
|
Psychostimulants |
3.15 |
7.29 |
37.6 |
72.6 |
27.8 |
57.2 |
21.4 |
44.0 |
|||||||
|
Atomoxetine |
0.09 |
0.12 |
3.36 |
2.00 |
2.52 |
2.45 |
1.85 |
1.45 |
|||||||
|
Dexamphetamine |
0.70 |
1.41 |
4.17 |
6.03 |
3.45 |
4.61 |
2.61 |
3.91 |
|||||||
|
Lisdexamfetamine |
0 |
0.69 |
0 |
18.7 |
0 |
20.2 |
0 |
12.6 |
|||||||
|
Methylphenidate |
2.60 |
5.85 |
32.3 |
54.6 |
23.0 |
35.9 |
18.0 |
31.0 |
|||||||
|
Modafinil |
0 |
0 |
0.03 |
0 |
0.01 |
0.06 |
0.01 |
0.02 |
|||||||
|
Other |
0 |
0 |
0 |
0 |
0 |
0.04 |
0 |
0.01 |
|||||||
|
Antipsychotics |
0.88 |
1.30 |
6.35 |
8.27 |
8.66 |
10.5 |
4.97 |
6.40 |
|||||||
|
Aripiprazole |
0.02 |
0.01 |
0.10 |
0.31 |
0.48 |
0.92 |
0.19 |
0.39 |
|||||||
|
Olanzapine |
0.02 |
0 |
0.09 |
0.25 |
1.40 |
1.04 |
0.47 |
0.40 |
|||||||
|
Other |
0.01 |
0.01 |
0.17 |
0.21 |
0.79 |
1.00 |
0.30 |
0.38 |
|||||||
|
Periciazine |
0.05 |
0.03 |
0.15 |
0.13 |
0.35 |
0.20 |
0.17 |
0.11 |
|||||||
|
Quetiapine |
0.08 |
0.01 |
0.23 |
0.17 |
2.08 |
2.01 |
0.75 |
0.68 |
|||||||
|
Risperidone |
0.74 |
1.28 |
5.80 |
7.53 |
5.04 |
6.65 |
3.62 |
4.97 |
|||||||
|
Sedative/hypnotics |
0.09 |
0.02 |
0.20 |
0.05 |
2.03 |
0.89 |
0.72 |
0.30 |
|||||||
|
Nitrazepam |
0.01 |
0.02 |
0.02 |
0.02 |
0.15 |
0.02 |
0.06 |
0.02 |
|||||||
|
Temazepam |
0.08 |
0 |
0.17 |
0.03 |
1.91 |
0.87 |
0.68 |
0.28 |
|||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 2 – Estimated prevalence of the dispensing of psychotropic medications to girls and young women (per 1000), Australia, 2013–2021, by age group
|
|
Age group (years) |
||||||||||||||
|
|
0–6 |
7–12 |
13–18 |
All ages |
|||||||||||
|
Medication |
2013 |
2021 |
2013 |
2021 |
2013 |
2021 |
2013 |
2021 |
|||||||
|
|
|||||||||||||||
|
Any psychotropic |
1.92 |
3.03 |
14.8 |
34.4 |
64.1 |
117 |
25.2 |
48.2 |
|||||||
|
Psychotropic polypharmacy |
0.19 |
0.27 |
1.62 |
5.17 |
10.1 |
21.1 |
3.72 |
8.27 |
|||||||
|
Antidepressants |
0.72 |
0.64 |
5.06 |
11.2 |
51.9 |
97.3 |
18.0 |
33.8 |
|||||||
|
Amitriptyline |
0.17 |
0.14 |
0.88 |
0.80 |
3.96 |
4.97 |
1.57 |
1.84 |
|||||||
|
Escitalopram |
0.07 |
0.05 |
0.23 |
0.64 |
9.46 |
16.7 |
3.04 |
5.36 |
|||||||
|
Fluoxetine |
0.10 |
0.29 |
1.86 |
6.87 |
17.8 |
46.4 |
6.15 |
16.6 |
|||||||
|
Fluvoxamine |
0.07 |
0.04 |
0.39 |
0.94 |
3.41 |
5.65 |
1.21 |
2.06 |
|||||||
|
Sertraline |
0.10 |
0.09 |
0.80 |
2.47 |
11.0 |
26.6 |
3.70 |
9.02 |
|||||||
|
Other |
0.27 |
0.08 |
1.31 |
0.49 |
16.3 |
17.8 |
5.57 |
5.66 |
|||||||
|
Anxiolytics |
0.16 |
0.06 |
0.72 |
0.47 |
6.04 |
7.11 |
2.16 |
2.36 |
|||||||
|
Diazepam |
0.15 |
0.05 |
0.63 |
0.47 |
5.21 |
6.64 |
1.87 |
2.21 |
|||||||
|
Oxazepam |
0 |
0.01 |
0.06 |
0 |
0.82 |
0.48 |
0.27 |
0.15 |
|||||||
|
Alprazolam |
0.01 |
0 |
0.02 |
0 |
0.21 |
0.07 |
0.08 |
0.02 |
|||||||
|
Psychostimulants |
0.90 |
2.15 |
9.29 |
25.9 |
8.32 |
26.5 |
5.77 |
17.4 |
|||||||
|
Atomoxetine |
0.03 |
0.05 |
0.85 |
1.03 |
0.75 |
1.45 |
0.50 |
0.80 |
|||||||
|
Dexamphetamine |
0.19 |
0.42 |
0.84 |
2.12 |
1.10 |
2.89 |
0.67 |
1.74 |
|||||||
|
Lisdexamfetamine |
0 |
0.20 |
0 |
6.14 |
0 |
10.4 |
0 |
5.29 |
|||||||
|
Methylphenidate |
0.78 |
1.67 |
8.17 |
19.7 |
6.73 |
15.8 |
4.89 |
11.9 |
|||||||
|
Modafinil |
0 |
0 |
0 |
0.01 |
0.07 |
0.03 |
0.02 |
0.01 |
|||||||
|
Other |
0 |
0 |
0 |
0 |
0 |
0.01 |
0 |
0 |
|||||||
|
Antipsychotics |
0.29 |
0.46 |
1.56 |
2.66 |
6.78 |
8.91 |
2.70 |
3.78 |
|||||||
|
Aripiprazole |
0.01 |
0.02 |
0.05 |
0.06 |
0.51 |
1.15 |
0.18 |
0.38 |
|||||||
|
Olanzapine |
0.01 |
0 |
0.06 |
0.08 |
0.95 |
1.44 |
0.32 |
0.47 |
|||||||
|
Other |
0 |
0.02 |
0.07 |
0.04 |
0.50 |
1.14 |
0.18 |
0.37 |
|||||||
|
Periciazine |
0.02 |
0 |
0.07 |
0.07 |
0.30 |
0.16 |
0.12 |
0.07 |
|||||||
|
Quetiapine |
0.03 |
0 |
0.16 |
0.17 |
3.91 |
4.57 |
1.28 |
1.46 |
|||||||
|
Risperidone |
0.24 |
0.43 |
1.20 |
2.33 |
1.62 |
2.21 |
0.96 |
1.60 |
|||||||
|
Sedative/hypnotics |
0.06 |
0.03 |
0.15 |
0.16 |
3.74 |
2.35 |
1.23 |
0.78 |
|||||||
|
Nitrazepam |
0.03 |
0.03 |
0.02 |
0.08 |
0.18 |
0.07 |
0.07 |
0.06 |
|||||||
|
Temazepam |
0.03 |
0 |
0.12 |
0.07 |
3.59 |
2.28 |
1.16 |
0.72 |
|||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – Prevalent and incident psychotropic dispensing: difference (with 95% confidence interval, CI) between 2021 rates and rates predicted by data for 2013–2019, by gender and age*
|
|
Prevalent dispensing |
Incident dispensing |
|||||||||||||
|
Psychotropic class |
Girls |
Boys |
Girls |
Boys |
|||||||||||
|
|
|||||||||||||||
|
Antidepressants |
22.2% (17.4 to 26.9%) |
1% (1.1 to 11.1%) |
20.3% (16.3 to 24.2%) |
–1.9% (–8.0 to 4.2%) |
|||||||||||
|
6 years or younger |
–16.7% (–39.6 to 6.2%) |
–28.0% (–43.2 to –12.7%) |
–16.5% (–46.6 to 13.6%) |
–30.8% (–40.6 to –21.0%) |
|||||||||||
|
7–12 years |
15.3% (8.2 to 22.4%) |
–3.9% (–5.9 to –1.8%) |
10% (4.26 to 13.9%) |
–8.7% (–21.9 to 4.4%) |
|||||||||||
|
13–18 years |
20.3% (16.9 to 23.7%) |
6.8% (2.1 to 11.5%) |
21.0% (16.0 to 26.0%) |
–1.2% (–6.3 to 3.9%) |
|||||||||||
|
Anxiolytics |
5.6% (–10.2 to 21.4%) |
–6.5% (–14.9 to 1.9%) |
5.8% (–20.9 to 32.4%) |
–4.9% (–17.3 to 7.5%) |
|||||||||||
|
6 years or younger |
NR |
19.6% (–58.8 to 98.1%) |
NR |
44.8% (–35.7 to 125%) |
|||||||||||
|
7–12 years |
–14.1% (–56.8 to 28.7%) |
–43.9% (–74.0 to –13.9%) |
–38.6% (–76.0 to –1.19%) |
–25.9% (–53.7 to 1.9%) |
|||||||||||
|
13–18 years |
3.1% (–17.6 to 23.8%) |
–6.5% (–16.0 to 3.0%) |
4.13% (–28.4 to 36.6%) |
–7.7% (–19.6 to 4.2%) |
|||||||||||
|
Antipsychotics |
9% (16.5 to 23.3%) |
–3.0% (–5.9 to –0.2%) |
19.5% (13.4 to 25.6%) |
–14.2% (–21.6 to –6.86%) |
|||||||||||
|
6 years or younger |
–17.4% (–30.3 to –4.4%) |
–14.8% (–34.7 to 5.1%) |
–11.8% (–42.6 to 18.9%) |
–31.4% (–67.4 to 4.6%) |
|||||||||||
|
7–12 years |
5.5% (–3.2 to 14.1%) |
1.5% (–1.9 to 4.8%) |
–21.6% (–38.3 to –4.93%) |
0.26% (–13.0 to 13.5%) |
|||||||||||
|
13–18 years |
23.7% (20.2 to 27.3%) |
–8.1% (–14.9 to –1.4%) |
26.8% (18.4 to 35.2%) |
–26.3% (–44.8 to –7.8%) |
|||||||||||
|
Psychostimulants |
27.7% (18.9 to 36.6%) |
14.5% (8.0 to 21.1%) |
35.7% (29.6 to 41.7%) |
19.2% (11.6 to 26.9%) |
|||||||||||
|
6 years or younger |
19.3% (10.3 to 28.3%) |
17.2% (1.5 to 32.8%) |
6.94% (–3.14 to 17.0%) |
13.2% (–6.0 to 32.4%) |
|||||||||||
|
7–12 years |
15.8% (9.6 to 22.1%) |
11.1% (7.8 to 14.4%) |
24.5% (20.8 to 28.2%) |
18.2% (14.8 to 21.7%) |
|||||||||||
|
13–18 years |
39.0% (27.9 to 50.0%) |
16.7% (8.2 to 25.1%) |
52.1% (44.0 to 60.3%) |
27.8% (15.7 to 40.0%) |
|||||||||||
|
Sedative/hypnotics |
18.6% (–0.8 to 38.0%) |
–31.4% (–67.5 to 4.7%) |
16.0% (–5.70 to 37.8%) |
–25.8% (–75.2 to 23.4%) |
|||||||||||
|
6 years or younger |
NR |
NR |
NR |
NR |
|||||||||||
|
7–12 years |
18.1% (–34.2 to 70.3%) |
NR |
23.8% (–25.6 to 73.2%) |
NR |
|||||||||||
|
13–18 years |
18.3% (–5.0 to 41.7%) |
–22.4% (–46.8 to 1.9%) |
12.8% (–12.1 to 37.6%) |
–17.5% (–40.0 to 5.0%) |
|||||||||||
|
|
|||||||||||||||
|
NR = not reported (number in 2021 less than ten). * Annual prevalence and incidence during 2013–2021 are respectively depicted in Box 4 and Box 5. |
|||||||||||||||
Box 4 – Prevalent dispensing of psychotropic medications to children and adolescents, Australia, 2013–2021, by medication class, gender, and age group*
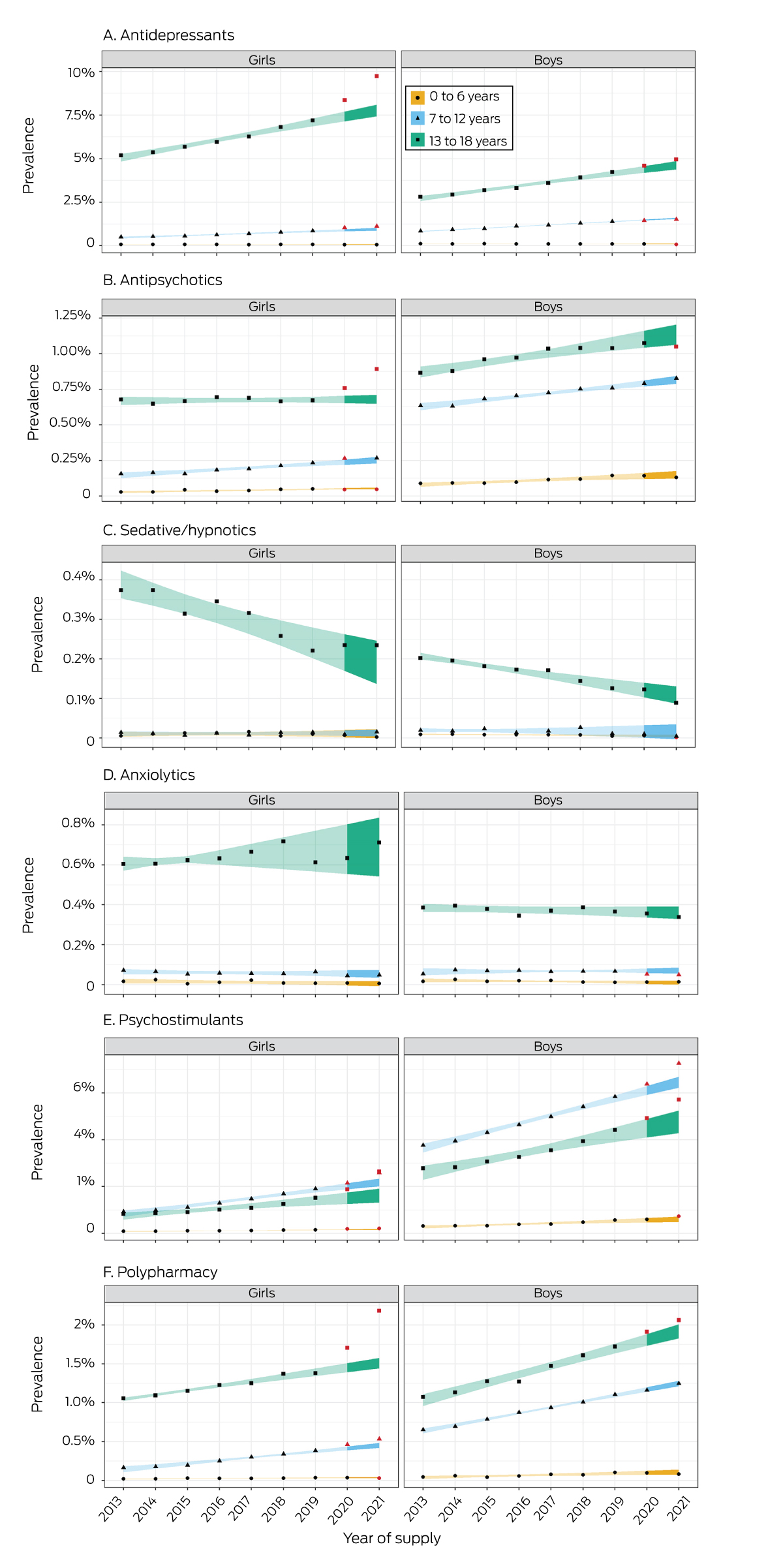
* Shaded areas: 95% confidence intervals for rates (2013–2019) or predicted rates (2020, 2021). Red points: actual rates during 2020 and 2021 outside the confidence intervals for the predicted values.
Box 5 – Incident dispensing of psychotropic medications to children and adolescents, Australia, 2013–2021, by medication class, gender, and age group*
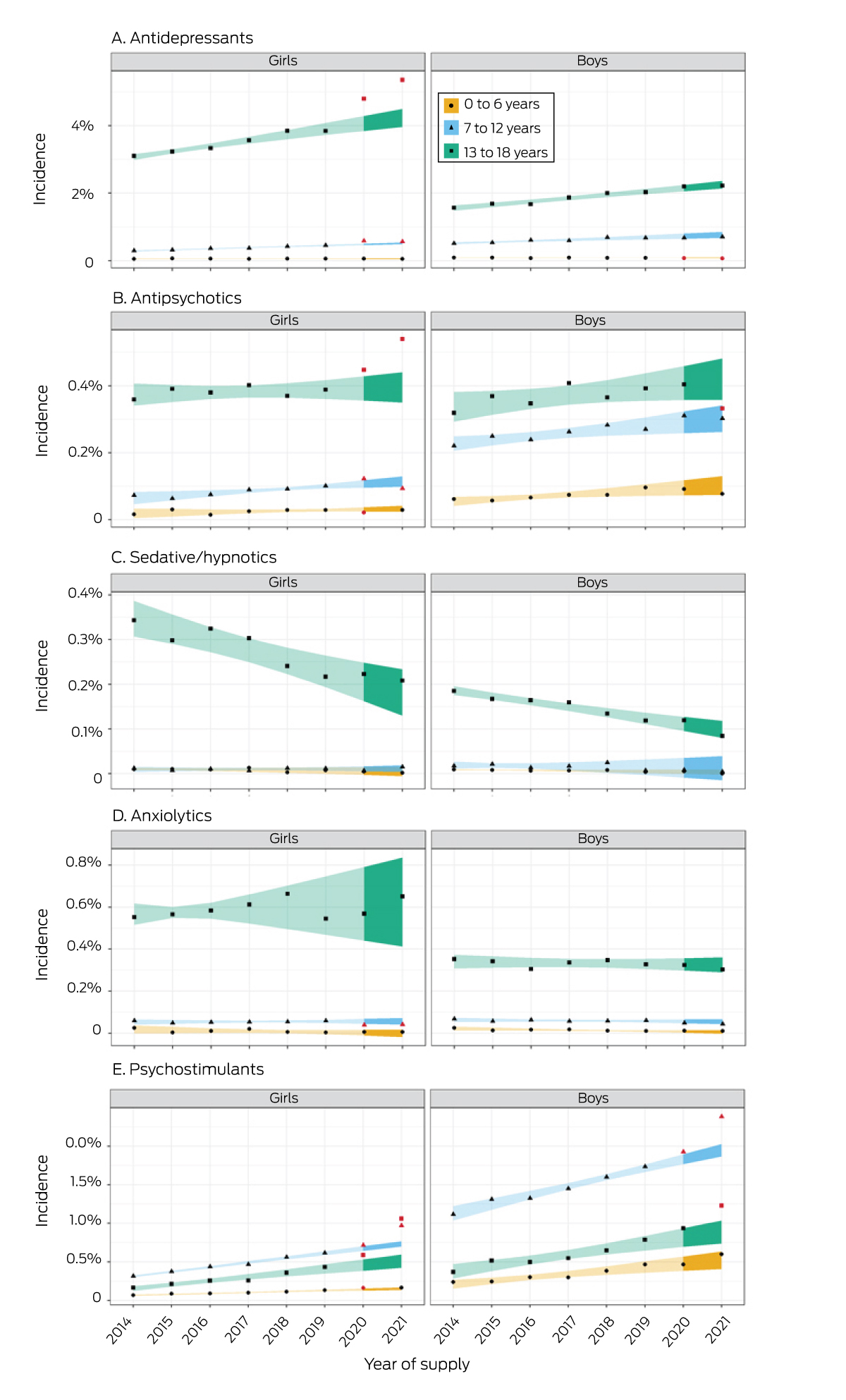
* Shaded areas: 95% confidence intervals for rates (2013–2019) or predicted rates (2020, 2021). Red points: actual rates during 2020 and 2021 outside the confidence intervals for the predicted values.
Received 25 November 2022, accepted 1 March 2023
- Stephen J Wood1
- Jenni Ilomäki1,2
- Jacqueline Gould3,4
- George SQ Tan1
- Melissa Raven4
- Jon N Jureidini4
- Luke E Grzeskowiak1,5
- 1 Centre for Medicine Use and Safety, Monash University, Melbourne, VIC
- 2 School of Public Health and Preventive Medicine, Monash University, Melbourne, VIC
- 3 South Australian Health and Medical Research Institute, Adelaide, SA
- 4 Robinson Research Institute, University of Adelaide, Adelaide, SA
- 5 College of Medicine and Public Health, Flinders University, Adelaide, SA
Open access
Open access publishing facilitated by Flinders University, as part of the Wiley – Flinders University agreement via the Council of Australian University Librarians.
This study was funded by a competitive grant from the Channel 7 Children's Research Foundation (CRF‐20647510). Luke Grzeskowiak receives salary support by a Channel 7 Children's Research Foundation Fellowship (CRF‐210323). The funders had no involvement in study design, data collection, analysis or interpretation, reporting or publication.
Jenni Ilomäki has previously received grant funding from AstraZeneca and Amgen for purposes unrelated to this study.
- 1. Hetrick SE, McKenzie JE, Bailey AP, et al. New generation antidepressants for depression in children and adolescents: a network meta‐analysis. Cochrane Database Syst Rev 2021; 5: CD013674.
- 2. Vitiello B, Correll C, van Zwieten‐Boot B, et al. Antipsychotics in children and adolescents: increasing use, evidence for efficacy and safety concerns. Eur Neuropsychopharmacol 2009; 19: 629‐635.
- 3. Piovani D, Clavenna A, Bonati M. Prescription prevalence of psychotropic drugs in children and adolescents: an analysis of international data. Eur J Clin Pharmacol 2019; 75: 1333‐1346.
- 4. Leung BMY, Kellett P, Youngson E, et al. Trends in psychiatric disorders prevalence and prescription patterns of children in Alberta, Canada. Soc Psychiatry Psychiatr Epidemiol 2019; 54: 1565‐1574.
- 5. Solmi M, Fornaro M, Ostinelli EG, et al. Safety of 80 antidepressants, antipsychotics, anti‐attention‐deficit/hyperactivity medications and mood stabilizers in children and adolescents with psychiatric disorders: a large scale systematic meta‐review of 78 adverse effects. World Psychiatry 2020; 19: 214‐232.
- 6. Karanges EA, Stephenson CP, McGregor IS. Longitudinal trends in the dispensing of psychotropic medications in Australia from 2009–2012: focus on children, adolescents and prescriber specialty. Aust N Z J Psychiatry 2014; 48: 917‐931.
- 7. Panda PK, Gupta J, Chowdhury SR, et al. Psychological and behavioral impact of lockdown and quarantine measures for COVID‐19 pandemic on children, adolescents and caregivers: a systematic review and meta‐analysis. J Trop Pediatr 2021; 67: fmaa122.
- 8. Kuitunen I. Psychotropic medication use in pediatric population during COVID‐19 pandemic. Acta Psychiatr Scand 2022; 146: 381‐383.
- 9. Bliddal M, Rasmussen L, Andersen JH, et al. Psychotropic medication use and psychiatric disorders during the COVID‐19 pandemic among Danish children, adolescents, and young adults. JAMA Psychiatry 2023; 80:176‐180.
- 10. Leong C, Katz LY, Bolton JM, et al. Psychotropic drug use in children and adolescents before and during the COVID‐19 pandemic. JAMA Pediatr 2022; 176: 318‐320.
- 11. de Oliveira Costa J, Gillies MB, Schaffer AL, et al. Changes in antidepressant use in Australia: a nationwide analysis (2015–2021). Aust N Z J Psychiatry 2023; 57: 49‐57.
- 12. Bruno C, Havard A, Gillies MB, et al. Patterns of attention deficit hyperactivity disorder medicine use in the era of new non‐stimulant medicines: a population‐based study among Australian children and adults (2013–2020). Aust N Z J Psychiatry 2023; 57: 675‐685.
- 13. Klau J, Bernardo CO, Gonzalez‐Chica DA, et al. Trends in prescription of psychotropic medications to children and adolescents in Australian primary care from 2011 to 2018. Aust N Z J Psychiatry 2022: 56: 1477‐1490.
- 14. Mellish L, Karanges EA, Litchfield MJ, et al. The Australian Pharmaceutical Benefits Scheme data collection: a practical guide for researchers. BMC Res Notes 2015; 8: 634.
- 15. Pearson SA, Pesa N, Langton JM, et al. Studies using Australia's Pharmaceutical Benefits Scheme data for pharmacoepidemiological research: a systematic review of the published literature (1987–2013). Pharmacoepidemiol Drug Saf 2015; 24: 447‐455.
- 16. Australian Bureau of Statistics. National, state and territory population; reference period: June 2022. 15 Dec 2022. https://www.abs.gov.au/statistics/people/population/national‐state‐and‐territory‐population/jun‐2022 (viewed Jan 2023).
- 17. Hartz I, Skurtveit S, Steffenak AKM, et al. Psychotropic drug use among 0–17 year olds during 2004–2014: a nationwide prescription database study. BMC Psychiatry 2016; 16: 12.
- 18. Barczyk ZA, Rucklidge JJ, Eggleston M, Mulder RT. Psychotropic medication prescription rates and trends for New Zealand children and adolescents 2008–2016. J Child Adolesc Psychopharmacol 2020; 30: 87‐96.
- 19. Lohr WD, Creel L, Feygin Y, et al. Psychotropic polypharmacy among children and youth receiving Medicaid, 2012–2015. J Manag Care Spec Pharm 2018; 24: 736‐744.
- 20. Varimo E, Saastamoinen LK, Rättö H, Aronen ET. Polypharmacy in children and adolescents initiating antipsychotic drug in 2008–2016: a nationwide register study. Nord J Psychiatry 2023; 77: 14‐22.
- 21. Olashore A, Ayugi J, Opondo P. Prescribing pattern of psychotropic medications in child psychiatric practice in a mental referral hospital in Botswana. Pan Afr Med J 2017; 26: 83.
- 22. Zito JM, Zhu Y, Safer DJ. Psychotropic polypharmacy in the US pediatric population: a methodologic critique and commentary. Front Psychiatry 2021; 12: 644741.
- 23. Sicouri G, March S, Pellicano E, et al. Mental health symptoms in children and adolescents during COVID‐19 in Australia. Aust N Z J Psychiatry 2023; 57: 213‐229.
- 24. Batchelor S, Stoyanov S, Pirkis J, Kõlves K. Use of Kids Helpline by children and young people in Australia during the COVID‐19 pandemic. J Adolesc Health 2021; 68: 1067‐1074.
- 25. Correll CU, Cortese S, Croatto G, et al. Efficacy and acceptability of pharmacological, psychosocial, and brain stimulation interventions in children and adolescents with mental disorders: an umbrella review. World Psychiatry 2021; 20: 244‐275.
- 26. Le Noury J, Nardo JM, Healy D, et al. Restoring Study 329: efficacy and harms of paroxetine and imipramine in treatment of major depression in adolescence. BMJ 2015; 351: h4320.






Abstract
Objective: To determine longitudinal patterns of dispensing of antidepressant, anxiolytic, antipsychotic, psychostimulant, and hypnotic/sedative medications to children and adolescents in Australia during 2013–2021.
Design: Retrospective cohort study; analysis of 10% random sample of Pharmaceutical Benefits Scheme (PBS) dispensing data.
Participants, setting: People aged 18 years or younger dispensed PBS‐subsidised psychotropic medications in Australia, 2013–2021.
Main outcome measures: Population prevalence of dispensing of psychotropic medications to children and adolescents, by psychotropic class, gender, and age group (0–6, 7–12, 13–18 years).
Results: The overall prevalence of psychotropic dispensing to children and adolescents was 33.8 per 1000 boys and 25.2 per 1000 girls in 2013, and 60.0 per 1000 boys and 48.3 per 1000 girls in 2021. The prevalence of psychotropic polypharmacy was 5.4 per 1000 boys and 3.7 per 1000 girls in 2013, and 10.4 per 1000 boys and 8.3 per 1000 girls in 2021. Prevalent dispensing during 2021 was highest for psychostimulants (boys, 44.0 per 1000; girls, 17.4 per 1000) and antidepressants (boys, 20.4 per 1000; girls, 33.8 per 1000). During 2021, the prevalence of dispensing was higher than predicted by extrapolation of 2013–2019 data for many classes, including antidepressants (boys: +6.1%; 95% CI, 1.1–11.1%; girls: +22.2%; 95% CI, 17.4–26.9%), and psychostimulants (boys: +14.5%; 95% CI, 8.0–21.1%; girls: +27.7%; 95% CI, 18.9–36.6%). The increases were greatest for girls aged 13–18 years (antidepressants: +20.3%; 95% CI, 16.9–23.7%; psychostimulants: +39.0%; 95% CI, 27.9–50.0%).
Conclusions: The prevalence of both psychotropic dispensing and psychotropic polypharmacy for children and adolescents were twice as high in 2021 as in 2013. The reasons and appropriateness of the marked increases in psychotropic dispensing during the COVID‐19 pandemic, particularly to adolescent girls, should be investigated.