General practice training is provided in geographically diverse locations across Australia to promote the development of the rural and remote medical workforce. Training in rural and remote locations supports learning locally required types of medical practice and builds both social and professional connections that increase the likelihood of trainees later practising in these communities.1,2 The remote learning model appears to be successful,3 but a 2020 scoping review found only limited evidence for the equivalence of learning outcomes after training in remote or less remote locations.4 We therefore compared formative assessment outcomes for general practice trainees in remote locations with those of trainees in rural or regional locations.
We analysed data for James Cook University (JCU) general practice trainees in their first year of community training, during which they undertook two formative assessments twice within a calendar year: the multiple choice questionnaire (MCQ) (2016–2021) and the external clinical teaching (ECT) visit (2019, 2021) (Supporting Information, table 1). Outcome scores were collected at time 1 (during the first three months) and time 2 (during the final three months). Training locations were coded using the Modified Monash Model (MMM) classification,5 with MMM1 and 2 (Sunshine Coast and regional centres) defined as “regional”, MMM3 and 4 (large and medium rural towns) defined as “rural”, and MMM5–7 (small rural towns and remote or very remote communities) defined as “remote”. Some remote and rural locations were recoded according to whether remote placements were fulltime and the practice scope was broader with minimal specialist back‐up, based on the knowledge of two senior medical educators (authors AH, LM). All analyses were conducted in Stata SE 15.1. The JCU human research ethics committee approved the study (H824).
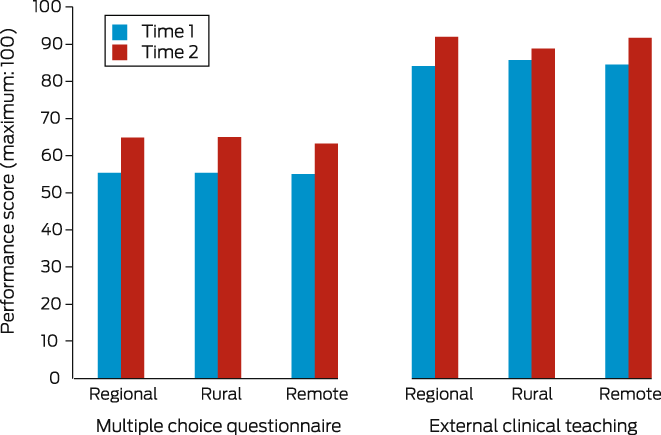
In total, 638 MCQ assessments were included in our analysis: 341 in regional areas (53%), 116 in rural areas (18%), and 181 in remote areas (28%). No significant association between location and MCQ assessment outcome was detected at either time point (Kruskal–Wallis test), nor between location and change in scores between time points (Box 1). The median MCQ scores by location were similar at time 1 and time 2 (Supporting Information, table 2). The median changes in MCQ score were also similar for the three location types: regional, 8.7 (interquartile range [IQR], 3.9–14.8); rural, 8.5 (IQR, 2.5–14.8); and remote, 8.5 (IQR, 2.3–15.2).
Ninety‐seven registrars had at least two ECT visits; 53 were classified as learning in regional locations, 17 in rural locations, and 27 in remote locations. The aggregate ECT visit scores for time 1 and time 2 were similar, regardless of location (Box 1). The median increase in scores was also similar for all locations: 4.7 for regional trainees (IQR, 0.0 to 12.5), 3.4 for rural locations (IQR, –1.1 to 12.9), and 3.9 for remote trainees (IQR, –5.1 to 13.6). In multivariable models (time 2 scores as the dependent variable), the MCQ and ECT visits performance scores were not statistically influenced by training location (Box 2).
We found that learning progression, as indicated by longitudinal MCQ or ECT results, is similar for trainees in remote areas and trainees in rural or regional areas, irrespective of their baseline scores. This finding is consistent with broader evidence supporting the quality and safety of distributed general practice training.6,7 General practice training in remote areas provides equivalent opportunities for learning and progression toward the fellowship, justifying the national strategy to offer general practice training in more remote locations.8 Whether the results are also equivalent in later years of general practice training or in other states should be investigated.
Box 1 – Median multiple choice questionnaire (MCQ) and external clinical teaching (ECT) scores for first year general practice trainees, by location
Box 2 – Multiple choice questionnaire (MCQ) and external clinical teaching (ECT) scores for first year general practice trainees: multivariable linear regression analysis*
|
Characteristic |
Time 2 MCQ score:† β (95% CI) |
Time 2 ECT score: β (95% CI) |
|||||||||||||
|
|
|||||||||||||||
|
Assessments |
624 |
97 |
|||||||||||||
|
Location |
|
|
|||||||||||||
|
Rural v regional |
–0.07 (–1.98 to 1.84) |
–0.04 (–5.00 to 4.91) |
|||||||||||||
|
Remote v regional |
–1.03 (–2.88 to 0.82) |
1.17 (–3.66 to 6.00) |
|||||||||||||
|
Time 1 score |
|
|
|||||||||||||
|
Multiple choice questionnaire |
0.50 (0.43 to 0.58) |
— |
|||||||||||||
|
External clinical teaching |
— |
0.26 (0.10 to 0.42) |
|||||||||||||
|
Age: 40 years or more v under 40 years |
–3.70 (–5.23 to –2.16) |
–1.85 (–5.77 to 2.08) |
|||||||||||||
|
Gender: men v women |
–0.59 (–1.93 to 0.75) |
–4.39 (–7.83 to –0.95) |
|||||||||||||
|
Training |
|
|
|||||||||||||
|
Rural (RACGP) v general (RACGP) |
–1.33 (–3.14 to 0.49) |
–2.14 (–6.57 to 2.30) |
|||||||||||||
|
Rural (ACRRM) v general (RACGP) |
1.20 (–1.22 to 3.62) |
–3.73 (–9.68 to 2.22) |
|||||||||||||
|
Australian medical school (no rural training) v overseas medical school (no rural training) |
1.05 (–0.75 to 2.85) |
2.74 (–2.25 to 7.74) |
|||||||||||||
|
Australian medical school (yes rural training) v overseas medical school (no rural training) |
–0.84 (–2.73 to 1.06) |
5.88 (0.83 to 10.9) |
|||||||||||||
|
Constant |
38.4 (33.5 to 43.3) |
68.3 (54.3 to 82.3) |
|||||||||||||
|
|
|||||||||||||||
|
ACRRM = Australian College of Rural and Remote Medicine; CI = confidence interval; RACGP = Royal Australian College of General Practitioners. * β value indicates the degree of change in time 2 score with respect to the predictor characteristic. † Model excludes fourteen trainees who completed both the RACGP and ACRRM fellowships. |
|||||||||||||||
Received 27 July 2022, accepted 27 March 2023
- 1. Kanakis K, Young L, Reeve C, et al. How does GP training impact rural and remote underserved communities? Exploring community and professional perceptions. BMC Health Serv Res 2020; 20: 812.
- 2. McGrail MR, Russell DJ, Campbell DG. Vocational training of general practitioners in rural locations is critical for the Australian rural medical workforce. Med J Aust 2016; 205: 216‐221. https://www.mja.com.au/journal/2016/205/5/vocational‐training‐general‐practitioners‐rural‐locations‐critical‐australian
- 3. Giddings P, McLaren J. Rural medical training via distance education and remote supervision. In: Chater AB, Rourke J, Couper ID, et al (eds). WONCA rural medical education guidebook. World Organization of Family Doctors, Apr 2014. https://www.globalfamilydoctor.com/site/DefaultSite/filesystem/documents/ruralGuidebook/RMEG.pdf (viewed Apr 2023).
- 4. Reeve C, Johnston K, Young L. Health profession education in remote or geographically isolated settings: a scoping review. J Med Educ Curric Dev 2020; 7: 2382120520943595.
- 5. Australian Department of Health and Aged Care. Modified Monash Model. Updated 14 Dec 2021. https://www.health.gov.au/topics/rural‐health‐workforce/classifications/mmm (viewed Mar 2023).
- 6. Young L, Peel R, O'Sullivan B, Reeve C. Building general practice training capacity in rural and remote Australia with underserved primary care services: a qualitative investigation. BMC Health Serv Res 2019; 19: 338.
- 7. Couch D, O'Sullivan B, Russell D, McGrail M. “It's so rich, you know, what they could be experiencing”: rural places for general practitioner learning. Health Sociol Rev 2020; 29: 76‐91.
- 8. Australian Department of Health and Aged Care. National medical workforce strategy 2021–2031. Updated 20 Jan 2022. https://www.health.gov.au/our‐work/national‐medical‐workforce‐strategy‐2021‐2031 (viewed Mar 2023).






Open access
Open access publishing facilitated by James Cook University, as part of the Wiley – James Cook University agreement via the Council of Australian University Librarians.
This project was funded by an Education Research Grant from the Australian College of Rural and Remote Medicine (salaries and research costs).
No relevant disclosures.