Until we have strategies to reduce the barriers of video consultations, Australia needs long telephone consultations
The coronavirus disease 2019 (COVID‐19) pandemic drove an expansion of telehealth subsidisation in March 2020. As of October 2022, there have been over 99 million standard general practitioner consultations delivered via telehealth.1 The Medicare Benefits Schedule (MBS) GP telehealth items were initially introduced as temporary measures to facilitate remote delivery of care and reduce the transmission of COVID‐19 in the community. Most telehealth consultations were telephone based; only 3% were video based. The federal government announced the continued expiry of the Medicare rebate for long (over 20 minutes) MBS telephone items from 1 July 2022. This means that patients who require long telephone consultations must now switch to video consultations, travel to see their GP in person, or self‐fund their long telephone consultations. Note, long telephone consultations were still available for patients seeking advice on COVID‐19 antivirals until 31 December 2022, and for those living in remote and very remote areas.2 As the context of the pandemic shifts, re‐examination of MBS items is appropriate, and changes should be based on available evidence.
Do all telehealth long consultations require video?
The evidence that underpins the removal of MBS items for telephone consultations longer than 20 minutes is unclear, and indirectly suggests that patients who require long telehealth consultations can only achieve better outcomes through video consultations.
Qualitative data from community health centres in the United States suggest that video consultations have several advantages, including the ability to obtain visual cues (eg, a patient's social support and living conditions) and enable better rapport building between patient and provider.3 A systematic review of eight studies conducted before the COVID‐19 pandemic, encompassing acute, home‐based and specialised care, also found that video consultation is superior in terms of diagnostic and decision‐making accuracy compared with telephone consultation.4 However, the quality of consultation for both telephone and video consultations has been rated similarly by patients, and the types of health problems addressed in both modalities were similar, as found in primary care and speciality care research conducted before and during the pandemic.5,6 A 2021 study from St Vincent's Hospital Melbourne also showed no difference in emergency related outcomes between video and telephone consultations for cardiology visits.7 Notably, despite positive feedback about video consultations, GPs have identified limited utility of video compared with telephone or face‐to‐face for most consultations.8 More evidence is needed to compare telephone and video consultations in the context of primary care.
Although clinicians in the United Kingdom acknowledged the benefits of video consultations, uptake has been low compared with telephone consultations;3,9 uptake by GPs in Australia has been similarly low.10,11 Indeed, a major caveat of video consultations is the complex setup process.3,7,12 A recent qualitative study found that Australian GPs preferred telephone consultations because they are simpler to do, and the Medicare rebate was the same as for video consultations.10 However, there is a lack of evidence to inform the appropriate reimbursement of different telehealth modalities. Another study reported GPs preferred photograph plus telephone consultations to video consultations for specific issues that required visual assessment, to minimise technological delays.8 In the US, uptake of video consultations for primary and speciality care was predominantly driven by practice and clinician factors, such as telehealth infrastructure and clinician preference and biases regarding their ability or willingness to conduct video consultations.12
Telephone consultations may allow for greater privacy.3 Vulnerable patients are also more likely to use telephone consultations.3,7,12 Indeed, older adults, minority groups, those in non‐metropolitan areas, and individuals on low incomes are less likely to have access to the internet and digital devices, and have poorer digital literacy.13,14 These factors can together contribute to disparities in access to health care, in particular among vulnerable groups who experience barriers to accessing face‐to‐face care, and who have limited digital literacy and access.
Overall, the removal of telephone consultations potentially disadvantages groups of patients who tend to have higher health care needs, such as those from rural and regional areas, those facing socio‐economic disadvantage, older Australians, and some minority or priority groups.13,14 These groups are also more likely to have lower capacity to access video consultations through reduced digital health literacy and access to digital technologies, and high costs of digital technologies and data.13,14
Use of long telephone versus video consultations in regional areas: insights from Western Victoria
We analysed utilisation of GP telephone consultations of longer than 20 minutes using data from 140 regional primary care practices in Western Victoria.15 There was no difference in utilisation of MBS items for telephone consultations longer than 20 minutes across various geographical characteristics (Box 1). While there was an immediate increase after the telehealth expansion policy was introduced in March 2020, and during lockdowns, utilisation had declined since August 2020 and tapered to around 10% of GP consultations by June 2021. These findings suggest long telephone consultations are still being used in the region, and there is as yet insufficient evidence that long video consultations are an appropriate alternative.
Analysis of GP video consultations longer than 20 minutes tells a different story. There was high uptake of video consultations at the onset of COVID‐19, but only in areas of higher socio‐economic advantage and located closer to urban centres (Box 2). These data indicate that there is a barrier to increasing the uptake of video‐based items in socio‐economically and geographically disadvantaged areas. By June 2021, use of video consultations longer than 20 minutes was minimal (< 0.2% of GP consultations). Together, these data do not support the continued expiry of Medicare rebate for telephone items for consultations longer than 20 minutes at present, particularly in the absence of significant investment of resources and time in improving video uptake in disadvantaged areas.
While long telephone consultations remain available for remote and very remote towns (Modified Monash Model classification, MM6–7), many medium and small rural towns (MM4–5 classified areas) are limited in internet and mobile telephone service infrastructure that would enable video calling capability. Many rural and remote areas also have higher proportions of older people who may have reduced digital literacy and increased barriers to accessing face‐to‐face care. During the pandemic, many older people chose to cancel face‐to‐face appointments because of complex medical vulnerabilities for which they still required care. The increased cost of travel for face‐to‐face appointments creates a situation of reduced health care equity for those who are both socio‐economically and geographically disadvantaged. We suggest there is need for further examination of long telephone consultations Australia‐wide, to gain a fuller picture of the risks and benefits of long telephone consultations in various contexts.
What is next for Australia?
Long telephone consultations have been critical in supporting Australians to receive health care they need. Rather than reducing the availability of MBS telephone items for consultations longer than 20 minutes to remote regions and for COVID‐19 antiviral issues, we need to recognise that there was evidence of substantial use of this MBS item and there is little evidence to support a change, including consideration of potential problems such as over‐servicing and adverse health and experience outcomes in different contexts. Understanding patient and GP perspectives on optimal consultation lengths will be critical to inform further evolution of MBS item numbers.
To make video consultations a more mainstream form of telehealth services, we should:
- establish plans to reduce the gaps in access to video infrastructure, including assessment and improvement of digital maturity of GPs and digital literacy and infrastructure for patients;
- generate evidence on the contexts in which face‐to‐face or video are clinically and experientially better than telephone consultations; and
- understand how different consultation patterns may differ depending on health conditions and other factors.
Box 1 – Monthly utilisation of general practitoner telephone consultations longer than 20 minutes in Western Victoria, stratified by geographic characteristics15
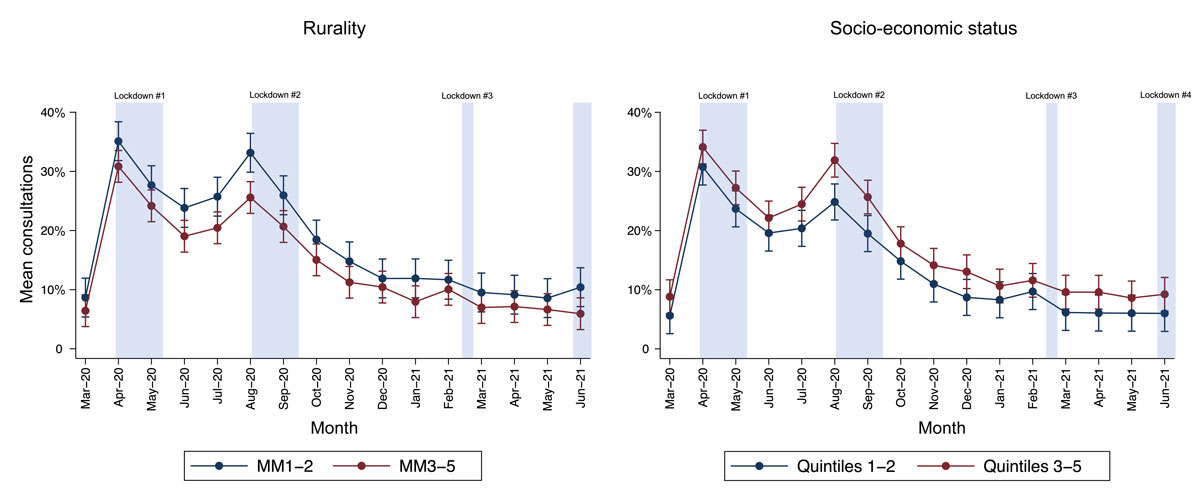
Monthly utilisation data was analysed using generalised linear mixed models. Data were provided at Statistical Area Level 2 (SA2), comprising 60 SA2 areas within the Western Victorian region. Data represent mean utilisation and 95% confidence intervals. Statistical significance for interaction by month was set at P > 0.05 for both factors. Lockdown periods follow pandemic rulings for regional Victoria. Rurality of each SA2 area was matched to the corresponding Modified Monash Model classification: MM1: metropolitan; MM2: regional centres; MM3: large rural towns; MM4: medium rural towns; MM5: small rural towns. Socio‐economic status of each SA2 area was derived from the Index of Relative Advantage and Disadvantage. Quintiles 1–2 represent areas of higher socio‐economic disadvantage and quintiles 3–5 represent areas of lower socio‐economic disadvantage.
Box 2 – Monthly utilisation of general practitioner video consultations longer than 20 minutes in Western Victoria, stratified by geographic characteristics15
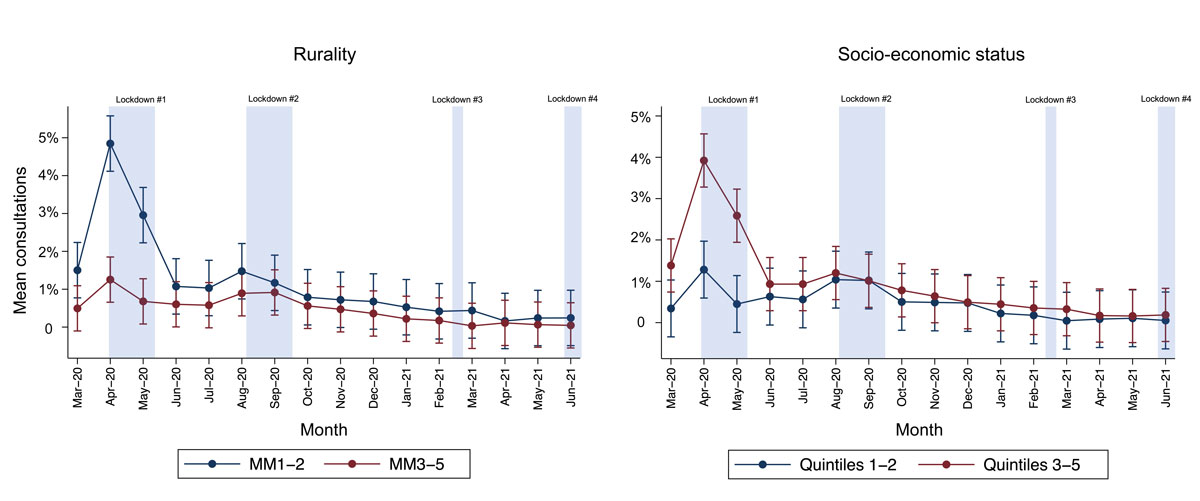
Monthly utilisation data was analysed using generalised linear mixed models. Data was provided at Statistical Area Level 2 (SA2), comprising 60 SA2 areas within the Western Victorian region. Data represent mean utilisation and 95% confidence intervals. Statistical significance for interaction by month was set at P > 0.001 for both factors. Lockdown periods follow pandemic rulings for regional Victoria. Rurality of each SA2 area was matched to the corresponding Modified Monash Model classification: MM1: metropolitan; MM2: regional centres; MM3: large rural towns; MM4: medium rural towns; MM5: small rural towns. Socio‐economic status of each SA2 area was derived from the Index of Relative Advantage and Disadvantage. Quintiles 1–2 represent areas of higher socio‐economic disadvantage and quintiles 3–5 represent areas of lower socio‐economic disadvantage.
Provenance: Not commissioned; externally peer reviewed.
- 1. Services Australia. Requested Medicare items processed from March 2020 to October 2022 (91790, 91795, 91800, 91801, 91802, 91809, 91810, 91811, 91890, 91891, 92746). http://medicarestatistics.humanservices.gov.au/statistics/do.jsp?_PROGRAM=%2Fstatistics%2Fmbs_item_standard_report&DRILL=ag&group=91790%2C+91800%2C+91801%2C+91802%2C+91795%2C+91809%2C+91810%2C+91811%2C+91890%2C+91891%2C+92746&VAR=services&STAT=count&RPT_FMT=by+state&PTYPE=month&START_DT=202003&END_DT=202210 (viewed Nov 2022).
- 2. MBS Online. MBS telehealth services from 1 July 2022. http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Factsheet‐telehealth‐1July22 (viewed July 2022).
- 3. Chang JE, Lindenfeld Z, Albert SL, et al. Telephone vs video visits during COVID‐19: safety‐net provider perspectives. J Am Board Fam Med 2021; 34: 1103‐1114.
- 4. Rush KL, Howlett L, Munro A, Burton L. Videoconference compared to telephone in healthcare delivery: a systematic review. Int J Med Inform 2018; 118: 44‐53.
- 5. Hammersley V, Donaghy E, Parker R, et al. Comparing the content and quality of video, telephone, and face‐to‐face consultations: a non‐randomised, quasi‐experimental, exploratory study in UK primary care. Br J Gen Pract 2019; 69: e595.
- 6. Allen AZ, Zhu D, Shin C, et al. Patient satisfaction with telephone versus video‐televisits: a cross‐sectional survey of an urban, multiethnic population. Urology 2021; 156: 110‐116.
- 7. Rowe SJ, Paratz ED, Fahy L, et al. Telehealth in Australian cardiology: insight into factors predicting the use of telephone versus video during the COVID‐19 pandemic. Intern Med J 2021; 51: 1229‐1235.
- 8. Murphy M, Scott LJ, Salisbury C, et al. Implementation of remote consulting in UK primary care following the COVID‐19 pandemic: a mixed‐methods longitudinal study. Br J Gen Pract 2021; 71: e166‐e177.
- 9. Saint‐Lary O, Gautier S, Le Breton J, et al. How GPs adapted their practices and organisations at the beginning of COVID‐19 outbreak: a French national observational survey. BMJ Open 2020; 10: e042119.
- 10. De Guzman KR, Snoswell CL, Giles CM, et al. GP perceptions of telehealth services in Australia: a qualitative study. BJGP Open 2022; 6: BJGPO.2021.0182.
- 11. Wabe N, Thomas J, Sezgin G, et al. Medication prescribing in face‐to‐face versus telehealth consultations during the COVID‐19 pandemic in Australian general practice: a retrospective observational study. BJGP Open 2022; 6: BJPO.2021.0132.
- 12. Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID‐19 pandemic. Am J Manag Care 2021; 27: 21‐26.
- 13. Ng BP, Park C, Silverman CL, et al. Accessibility and utilisation of telehealth services among older adults during COVID‐19 pandemic in the United States. Health Soc Care Community 2022; 30: e2657‐e2669.
- 14. Kemp E, Trigg J, Beatty L, et al. Health literacy, digital health literacy and the implementation of digital health technologies in cancer care: the need for a strategic approach. Health Promot J Austr 2021; 32 Suppl 1: 104‐114.
- 15. Savira F, Orellana L, Hensher M, et al. Utilisation of general practitioner telehealth services during the COVID‐19 pandemic in regional Victoria, Australia: a retrospective analysis [accepted article]. J Med Internet Res 39384; 27 Nov 2022. https://preprints.jmir.org/preprint/39384/accepted (viewed Dec 2022).






Open access
Open access publishing facilitated by Deakin University, as part of the Wiley ‐ Deakin University agreement via the Council of Australian University Librarians.
Feby Savira is supported by an Alfred Deakin Postdoctoral Research Fellowship (Deakin University). Eva Yuen is supported by an Executive Dean Health Research Fellowship (Deakin University). Anna Ugalde is supported by a Victorian Cancer Agency Mid‐Career Research Fellowship. Anna Peeters is supported by a National Health and Medical Research Council Investigator Grant Fellowship. This study was funded by the Western Alliance. The funders had no role in the planning, writing or publication of this work. We thank Western Victoria Primary Health Network for their intellectual input.
No relevant disclosures.