Action to incorporate evidence‐based nutrition concepts in medical education programs is essential
Nutrition is a fundamental tenet of good health, and the coronavirus disease 2019 (COVID‐19) pandemic has highlighted the need for urgent attention to ensuring sustainable food systems and access to nutrition care.1 This perspective article presents critical actions required for the legitimate incorporation of evidence‐based nutrition concepts in medical education programs, including:
- to cultivate a shift in medical education principles to embrace health promotion and disease prevention, including nutrition;
- to identify the essential nutrition knowledge and skills required in medical education programs; and
- to revise accreditation standards to include a mandated framework of minimum nutrition standards to underpin preventive care and treatment of disease.
Dietary risk — especially diets high in sodium, low in whole grain, and those with low fruit intake — is third in its contribution to preventable disease in Australia, contributing 5.4% to total disease burden.2,3 In Australia, general practices provide more than 189 million services each year, and almost 90% of the population see a general practitioner at least once each year.4 International studies estimate that 16–24% of general practice consultations feature some aspect of nutrition,5 and there is evidence that individuals may have a preference for dietary intervention before the use of medication for conditions such as type 2 diabetes.6 Brief training in nutrition care can improve health professionals’ practice,7 and nutrition is highlighted as a key outcome in the recently published Australian National Preventive Health Strategy,8 which seeks to develop a health professional workforce competent in preventive health strategies.
The global COVID‐19 pandemic and climate‐related natural disasters have revealed increasing health and social inequalities, such as food security. Food security is dramatically affected by socio‐economic status and includes access to sufficient, safe and nutritious food that is culturally appropriate. To minimise dietary risk from non‐communicable diseases (NCDs), all health professionals should consider the effects of climate change and social inequity on food systems and food security, and the role of nutrition in chronic disease, as part of their practice.9
Despite long‐standing recognition, evidence and multiple efforts, nutrition has not entered mainstream medical education in measurable and sustainable ways. In 2012, a letter published in The Medical Journal of Australia urged medical schools to adopt a nutrition competency framework.10 The framework aligned with the Medical Graduate Competency Framework11 developed at that time by Medical Deans Australia and New Zealand, and aimed to improve both prevention and treatment of nutrition‐related diseases.12 A decade on, a systematic review highlighted that, internationally, nutrition content is still limited within medical education.13 Multiple studies of both medical students and practitioners show that doctors see nutrition care as part of their job and have a desire to engage in this care. However, many still lack confidence in their nutrition skills, which acts as a significant barrier to taking a proactive approach to nutrition as a component of comprehensive health care.14,15,16 The most concerning aspect of contemporary research on this topic is the almost total reliance on personal experience rather than effective medical education to inform nutrition care.16
Efforts to embed nutrition in medical curricula and practice have been met with multiple barriers, including perceived lack of time and a low priority for nutrition education, inadequate teaching materials, lack of knowledge and skills, inadequate remuneration, lack of confidence to provide nutrition care, and lack of nutrition expert teachers.16,17 The barriers, especially where expert teachers may not sit within medical schools, may have also limited advocacy for inclusion of content in accreditation standards. Despite mandated nutrition education in the United States since 1990,18 it was still deemed necessary that Congress set a precedent, calling on medical schools and other health education providers to cover meaningful content on nutrition and diet, related to the mounting personal and financial burden of diet‐related disease.19 The accreditation standards for primary medical courses in Australia and New Zealand20 specify that medical practitioners need only to “explain environmental and lifestyle choices and advocate for healthy lifestyle choices” and dietary investigation may be implied in words around eliciting thorough histories including “lifestyle features”. Having a medical workforce equipped with evidence‐based knowledge and skills in nutrition would align with the objectives of the National Preventive Health Strategy to significantly decrease the overall burden of disease by addressing the wider determinants of health, including access to, and consumption of, a healthy diet. Critically, this would improve population health outcomes, contributing to economic and social benefits, including gross domestic productivity.8 Therefore, future medical education must incorporate a focus on nutrition as both prevention and treatment for disease.
The opportunity for doctors to support patients with their diet is critical in primary care, given doctors’ greater contact over time with patients compared with other health professionals. Patients perceive doctors as a trusted source of information and express preference to receive their nutrition information from doctors rather than other professionals, even dietitians.14 Teaching nutrition within the medical education environment sensitises students to the relevance of nutrition in the prevention and treatment of disease.21 It provides opportunities to recognise when referral to experts such as dietitians is required, and empowers doctors to advocate for and reinforce the importance of nutrition to patients.22 Although there are systemic barriers to such care in general practice, such as consultation time and limited access to dietetic services,23 including nutrition care in primary health settings has been found to be cost‐effective for a range of clinical outcomes, warranting increased investments into primary prevention.24
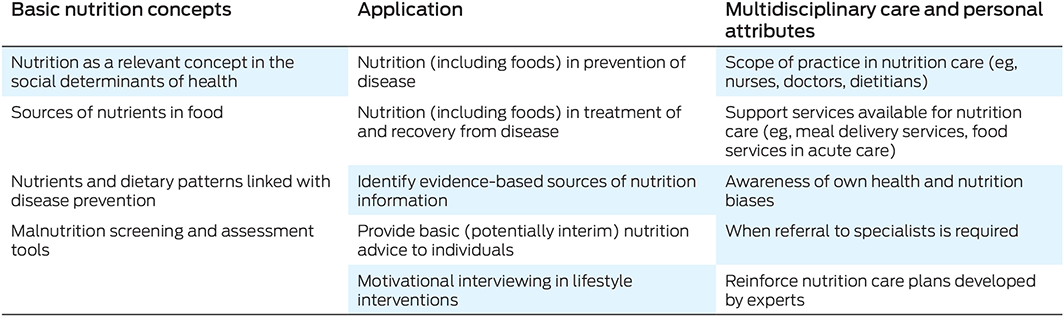
Consensus on essential nutrition knowledge and skills for doctors is progressing. The international literature describes that many of the potential areas of nutrition competency fall into themes of clinical practice, health promotion and disease prevention, communication, working as a multidisciplinary team, and professional practice.17 These themes are broader than nutrition, yet could incorporate relevant nutrition context. The inclusion of nutrition in existing elements of topics would limit additional content in busy curricula and would integrate concepts of nutrition which underpin both prevention and treatment of disease. There is opportunity for vertical and horizontal integration of nutrition into existing medical curricula without adding time or material, and successful examples of this have been implemented.25 If taught by nutrition‐trained academics such as dietitians, this would enhance understanding of scope of practice. Specifically, competencies may include the need for doctors to be able to identify when an individual might benefit from referral for specialist advice and to provide support as part of a multidisciplinary approach to nutrition care. Underpinning concepts must include food knowledge — and the relationship of nutrients and, therefore, food with disease — and nutrition could be used as an integrated example in teaching evidence‐based practice (Box).23 Consensus on nutrition knowledge and skills may be furthered by engaging in discussion with medical and health care professionals to integrate interprofessional and multidisciplinary approaches into nutrition education. Consensus on nutrition competencies will provide a benchmark for development of accreditation mechanisms to address the dearth in nutrition education in medical training.
Two factors identified as critical to the success of nutrition in medical education include i) demonstrated relevance of nutrition course material to the practice of medicine, and ii) positive role modelling.21 Yet, students in medical schools identify that they do not have medical nutrition role models.16 Nutrition is not a recognised medical specialty training program in Australia, limiting potential mentors, and the contributions of dietitians to nutrition education is somewhat ad hoc.14 For successful teaching and role modelling, strong relationships are required between dietitians and medical professionals who will model nutrition care at universities and in practice.
To achieve delivery of appropriate nutrition care by medical practitioners, including an understanding of when to refer to experts such as dietitians, medical programs must have mandated nutrition knowledge and skills as part of the curricula. International reviews identify that only 44% of regulatory standards for medicine, such as curriculum guidance and accreditation standards, include nutrition content or requirements.26 Therefore, where there is an opportunity for a mandated framework of minimum nutrition standards to provide incentives, most countries do not include such regulation. Without incentive, it is unlikely that medical education providers will pursue curriculum changes. Accreditation bodies need to ensure nutrition is included in accreditation requirements in entry‐level medical programs so that the nutrition curricula are adequate, authentic, inclusive and evidence‐based. The review of the Australian Medical Council accreditation standards — being undertaken at the time of writing — may provide such opportunities.
Challenges in health care include an ageing population, rising health care costs with improving technology and new drugs, predominance of NCDs, and health‐related effects of climate change, including inequity. There is a need to focus on cost‐effective strategies to prevent NCDs, and to keep people with NCDs well. Medical professionals are in a prime position to signal the importance of nutrition in health and wellbeing as well as working within multidisciplinary teams to provide nutrition care. Even though experience provides opportunities to learn, mandating minimum standards will ensure a threshold of nutrition learning to build on in practice. Nutrition education should be prioritised in order to educate medical professionals who are competent to practise in the current health environment.
Provenance: Not commissioned; externally peer reviewed.
- 1. United Nations. UN calls for urgent action to feed the world's growing population healthily, equitably and sustainably [website]. https://www.un.org/en/desa/un‐calls‐urgent‐action‐feed‐world%E2%80%99s‐growing‐population‐healthily‐equitably‐and‐sustainably (viewed June 2022).
- 2. GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019; 393: 1958‐1972.
- 3. Australian Institute of Health and Welfare. Australian Burden of Disease Study 2018 — key findings [Cat. No. BOD 30]. Canberra: AIHW, 2021. https://www.aihw.gov.au/reports/burden‐of‐disease/burden‐of‐disease‐study‐2018‐key‐findings (cited Sept 2022).
- 4. Department of Health and Aged Care. Annual Medicare statistics: financial year 1984–85 to 2020–21. https://www1.health.gov.au/internet/main/publishing.nsf/Content/Medicare%20Statistics‐1 (viewed Nov 2022).
- 5. MacDonald Werstuck M, Buccino J. Dietetic staffing and workforce capacity planning in primary health care. Can J Diet Pract Res 2018; 79: 181‐185.
- 6. Ball L, Hughes R, Desbrow B, Levitt M. Patients’ perceptions of nutrition care provided by general practitioners: focus on type 2 diabetes. Fam Pract 2012; 29: 719‐725.
- 7. Edwards EJ, Stapleton P, Williams K, Ball L. Building skills, knowledge and confidence in eating and exercise behavior change: Brief motivational interviewing training for healthcare providers. Patient Educ Couns 2015; 98: 674‐676.
- 8. Department of Health. National Preventive Health Strategy 2021–2030. Canberra: Commonwealth of Australia, 2021. https://www.health.gov.au/sites/default/files/documents/2021/12/national‐preventive‐health‐strategy‐2021‐2030.pdf (viewed Nov 2022).
- 9. Boak R, Palermo C, Beck EJ, et al. A qualitative exploration of the future of nutrition and dietetics in Australia and New Zealand: implications for the workforce. Nutr Diet 2022; 79: 427‐437.
- 10. Nowson C, Roshier‐Taks M, Crotty B. Nutrition competencies for the prevention and treatment of disease in Australian medical courses. Med J Aust 2012; 197: 147. https://www.mja.com.au/journal/2012/197/3/nutrition‐competencies‐prevention‐and‐treatment‐disease‐australian‐medical
- 11. Hays R, Hourn M. Medical Graduate Competency Framework stage 2 — final report. Medical Deans Australia and New Zealand and Health Workforce Australia, 2012. https://medicaldeans.org.au/md/2018/07/Stage‐2‐Competencies‐Final‐Report‐August‐2012.pdf (viewed Dec 2022).
- 12. Nowson C, Rooney K, Lindley J, et al. A web‐based nutrition competency implementation toolkit for entry‐level medical courses. Sydney: Office for Learning and Teaching, 2015. https://www.deakin.edu.au/__data/assets/pdf_file/0007/500776/ID12‐2361_Deakin_Nowson_Final‐report‐2‐1.pdf (viewed Nov 2022).
- 13. Crowley J, Ball L, Hiddink GJ. Nutrition in medical education: a systematic review. Lancet Planet Health 2019; 3: E379‐E389.
- 14. Burch E, Crowley J, Laur C, et al. Dietitians’ perspectives on teaching nutrition to medical students. J Am Coll Nutr 2017; 36: 415‐421.
- 15. Crowley J, Ball L, Han D, et al. Doctors’ attitudes and confidence towards providing nutrition care in practice: Comparison of New Zealand medical students, GP registrars and GPs. J Prim Health Care 2015; 7: 244‐250.
- 16. Lepre B, Crowley J, Mpe D, et al. Australian and New Zealand medical students’ attitudes and confidence towards providing nutrition care in practice. Nutrients 2020; 12: 598.
- 17. Lepre B, Mansfield KJ, Ray S, Beck EJ. Nutrition competencies for medicine: an integrative review and critical synthesis. BMJ Open 2021; 11: e043066.
- 18. National Nutrition Monitoring and Related Research Act of 1990, Pub L No. 101‐445, Stat 101‐445 (1990). https://www.congress.gov/bill/101st‐congress/house‐bill/1608 (viewed Nov 2022).
- 19. 117th Congress HRes 784. Expressing the sense of the House of Representatives that the United States recognizes the mounting personal and financial burden of diet‐related disease in the United States and calls on medical schools, graduate medical education programs, and other health professional training programs to provide meaningful physician and health professional education on nutrition and diet; 2021–2022. https://www.congress.gov/bill/117th‐congress/house‐resolution/784?s=1&r=30 (viewed June 2022).
- 20. Medical School Accreditation Committee. Standards for assessment and accreditation of primary medical programs by the Australian Medical Council 2012. Canberra: Australian Medical Council, 2012. https://www.amc.org.au/wp‐content/uploads/2019/10/Standards‐for‐Assessment‐and‐Accreditation‐of‐Primary‐Medical‐Programs‐by‐the‐Australian‐Medical‐Council‐2012.pdf (viewed Nov 2022).
- 21. Weinsier R. Medical‐nutrition education‐factors important for developing a successful program. Am J Clin Nutr 1995; 62: 837‐840.
- 22. Peniamina R, Davies C, Moata'ane L, et al. Food, nutrition and cancer: perspectives and experiences of New Zealand cancer survivors. N Z Med J 2021; 134: 1545.
- 23. Lepre B, Mansfield KJ, Beck EJ. Attitudes, work roles and barriers to nutrition care — interviews with Australian and UK‐based medical doctors. J Hum Nutr Dietet 2022; doi: https://doi.org/10.1111/jhn.13079 [Epub ahead of print].
- 24. Barnes KA, Szewczyk Z, Kelly JT, et al. How cost‐effective is nutrition care delivered in primary healthcare settings? A systematic review of trial‐based economic evaluations. Nutr Rev 2022; 80: 1480‐1496.
- 25. Bradley A, Crowley J, Bhoopatkar H, et al. Let's talk about diet — nutrition skills in medical education. Med Educ 2022; 56: 564‐565.
- 26. Lepre B, Mansfield KJ, Ray S, Beck EJ. Reference to nutrition in medical accreditation and curriculum guidance: a comparative analysis. BMJ Nutr Prev Health 2021; 4: 307‐318.






Open access
Open access publishing facilitated by University of Wollongong, as part of the Wiley ‐ University of Wollongong agreement via the Council of Australian University Librarians.
This work is undertaken in partnership with the Australian and New Zealand Network, and Virtual Core of the NNEdPro Global Institute for Food, Nutrition and Health (Cambridge, UK), linked with its Nutrition Education Policy in Healthcare Practice (NEPHELP) initiative. We acknowledge the specific contributions of NNEdPro colleagues and collaborators, including Sumantra Ray, to this article.
No relevant disclosures.