Hip fractures are devastating for older people. The incidence of hip fracture declined in Australia by 9.5% between 2006–07 and 2015–16.1 However, the number of older people with hip fractures is expected to increase as the population ages,2 particularly among the oldest old (aged 80 years or more) and those with conditions such as dementia, increasing the complexity and costs of care.3 Mortality associated with hip fracture is higher for men, people of more advanced age, and those with greater comorbidity.4
Quality care can reduce morbidity and mortality among people with hip fractures. In Australia, the development of hip fracture care guidelines, a national clinical care standard, and a clinical quality registry commenced in 2012.5,6 In a retrospective study, we examined 30‐day and 12‐month mortality for people aged 50 years or more with index (first) acute admissions with hip fractures to New South Wales hospitals during 1 January 2011 – 30 November 2018.
We identified hospitalisation records in the Admitted Patient Data Collection for emergency admissions of people with hip fracture as the primary diagnosis (International Classification of disease, tenth revision, Australian modification [ICD‐10‐AM] codes S72.0–S72.2) with an external cause of low fall (ICD‐10‐AM codes W00–W08, W18, W19). These records were linked with NSW Registry of Births, Deaths and Marriages mortality data. Comorbid conditions during the 12 months preceding hospitalisation were identified using the Charlson Comorbidity Index (CCI). We assessed changes in mortality rates during 2011–2018 in negative binomial regression models, both unadjusted and adjusted for age, sex, and comorbidity; we report changes as percentage annual changes (PACs) with 95% confidence intervals (CIs). All analyses were performed in SAS Enterprise Guide 7.1. The NSW Population and Health Services Research Ethics Committee approved the study (HREC/17/CIPHS/45).
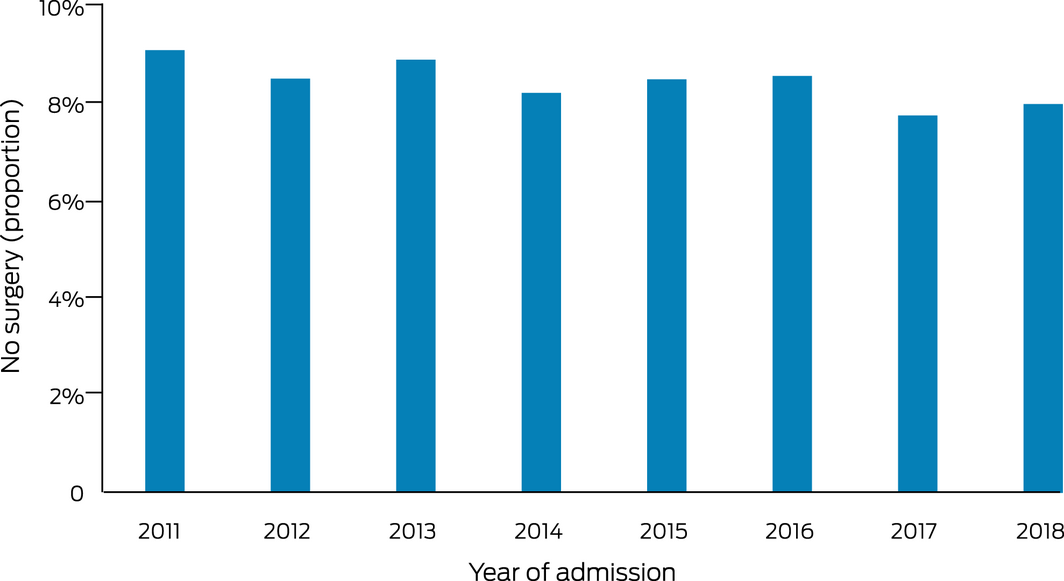
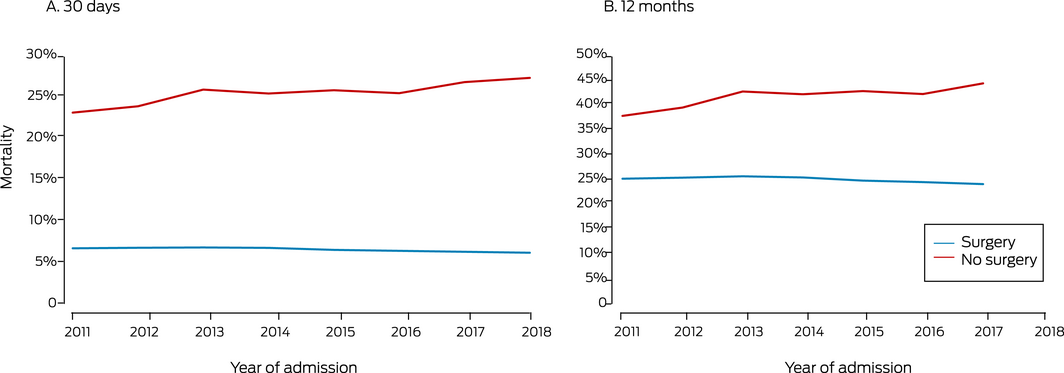
A total of 40 744 people were admitted to hospital with hip fractures during 2011–2018, 3450 of whom (8.5%) did not undergo surgery. Larger proportions of patients who did not undergo surgery were aged 95 years or more (300, 8.7%; < 95 years: 2264, 6.1%), had CCI scores of 3 or more (807, 23.4%; < 3: 6652, 17.8%), or had peri‐trochanteric fractures (2239, 64.9%; other fracture types: 15 400, 41.3%; each comparison: P < 0.001). A total of 3403 people (8.4%) died within 30 days of admission to hospital (surgery group, 2522 patients [6.8%]; no surgery group, 3403 [25.5%]); 9644 of the 36 088 people (26.7%) for whom 12‐month follow‐up data were available had died within 12 months (surgery group, 8356 of 33 011 [25.3%]; no surgery group, 1288 of 3077 [41.9%]) (Supporting Information).
The proportion of patients who did not undergo surgery declined from 9.1% in 2011 (5218 patients) to 8.0% in 2018 (4656 patients; PAC, –1.9%; 95% CI, –3.5% to –0.4%) (Box 1). Unadjusted 30‐day mortality, overall and by surgery group, was unchanged across the study period (data not shown). After adjusting for age, sex and comorbidity, 30‐day mortality declined from 8.4% in 2011 to 8.1% in 2018 (PAC, –2.3%; 95% CI, –3.9% to –0.7%). As the interaction between surgery group and year was statistically significant, we estimated separate models for the surgery and no surgery groups; among patients who underwent surgery, mortality declined from 6.9% in 2011 to 6.4% in 2018 (PAC, –3.0%; 95% CI, –4.7% to –1.2%), but the rate for those who did not undergo surgery did not decline significantly (PAC, –2.6%; 95% CI, –6.4% to 1.0%). Changes in adjusted 12‐month mortality were similar: overall decline, from 26.6% in 2011 to 26.0% in 2017; PAC, –2.3% (95% CI, –3.5% to –1.0%); surgery group, –2.8% (95% CI, –4.1% to –1.5%); no surgery group, 3.7% (95% CI, –0.3 to 7.8%) (Box 2).
In our large population‐based study, we found that 30‐day and 12‐month mortality after hip fracture surgery, adjusted for age, sex, and comorbidity, declined in NSW during 2011–2018, but not for patients who were hospitalised without undergoing surgery. Reductions in 30‐day and 12‐month mortality after hip fracture surgery have also been reported in other countries where guidelines, care standards, and hip fracture audits have been introduced.7,8 Our findings may also reflect the impact of factors such as improved peri‐ and post‐operative management, as reported for other major orthopaedic procedures.9 The factors underlying improved survival and their dependence on the care provided, geographic location of patients, and the treating hospital should be further investigated.
Box 1 – Proportion of patients admitted to hospital in New South Wales with hip fracture during 2011–2018 who did not undergo surgery
Received 5 August 2021, accepted 6 January 2022
- 1. Australian Institute of Health and Welfare. Hip fracture incidence and hospitalisation in Australia 2015–16 (Cat. no. PHE 226). 23 Oct 2018. https://www.aihw.gov.au/reports/injury/hip‐fracture‐incidence‐in‐australia‐2015‐16 (viewed Feb 2022).
- 2. Stephens A, Toson B, Close JCT. Current and future burden of incident hip fractures in New South Wales, Australia. Arch Osteoporos 2014; 9: 200.
- 3. Mitchell R, Draper B, Brodaty H, et al. An 11‐year review of hip fracture hospitalisations, health outcomes and predictors of access to in‐hospital rehabilitation for adults ≥ 65 years living with and without dementia: a population‐based cohort study. Osteoporos Int 2020; 31: 465–474.
- 4. Liu Y, Wang Z, Xiao W. Risk factors for mortality in elderly patients with hip fractures: a meta‐analysis of 18 studies. Aging Clin Exp Res 2018; 30: 323–330.
- 5. Australian and New Zealand Hip Fracture Registry Steering Group. Australian and New Zealand guideline for hip fracture care: improving outcomes in hip fracture management of adults. Sept 2014. https://anzhfr.org/wp‐content/uploads/sites/1164/2021/12/ANZ‐Guideline‐for‐Hip‐Fracture‐Care.pdf (viewed Feb 2022).
- 6. Australian Commission on Safety and Quality in Health Care. Hip fracture care clinical care standard. Sept 2016. https://www.safetyandquality.gov.au/sites/default/files/migrated/Hip‐Fracture‐Care‐Clinical‐Care‐Standard_tagged.pdf (viewed Feb 2022).
- 7. Metcalfe D, Zogg CK, Judge A. Pay for performance and hip fracture outcomes: an interrupted time series and difference in difference analysis in England and Scotland. Bone Joint J 2019; 101: 1015–1023.
- 8. Downey C, Kelly M, Quinlan J. Changing trends in the mortality rate at 1‐year post hip fracture: a systematic review. World J Orthop 2019; 10: 166–175.
- 9. Harris IA, Hatton A, de Steiger R, et al. Declining early mortality after hip and knee arthroplasty. ANZ J Surg 2020; 90: 119–122.





This study was supported by a NSW Agency for Clinical Innovation Grant and a National Health and Medical Research Council Project Grant (GNT1164680). We thank the NSW Ministry of Health and the NSW Registry of Births Deaths and Marriages for providing the hospitalisation and death data extracts, and the Centre for Health Record Linkage (CHeReL) for providing the unique patient identifier (PPN) used to link the datasets.
No relevant disclosures.