People in residential aged care facilities (RACFs) were disproportionately affected by the coronavirus disease 2019 (COVID‐19) pandemic; a systematic review found a pooled attack rate based on all included studies of 28% (95% confidence interval [CI], 18–40%) and case fatality rate of 23% (95% CI, 18–28%).1 COVID‐19 outbreaks have occurred in RACFs throughout Australia, particularly in Victoria; 44 residents died in one centre.2 Many RACF residents are frail, have multiple medical conditions, and have not been represented in COVID‐19 vaccine phase 3 safety and efficacy trials because of study exclusion criteria. Monitoring the safety of COVID‐19 vaccines for RACF residents is therefore important, both for their own welfare and for maintaining confidence in the vaccination program.
Hospitalisations and deaths soon after vaccination may cause alarm, but they are both more common among RACF residents than among older people living in the community. Recent overseas experience has underlined the importance of understanding health events after vaccination of people living in RACFs.3 Estimating the expected background rates of hospital transfer and death can inform analyses of vaccine safety and reduce the risk of coincidental events being inappropriately linked with vaccination.4
We analysed de‐identified RACF point‐of‐care data obtained from HealthMetrics (healthmetrics.com.au; the largest RACF electronic health record provider in Australia) for 101 RACFs providing more than 16 000 resident beds in New South Wales, South Australia, Victoria, and Queensland. Hospital transfer and death count data for 1 January 2015 – 31 December 2019, covering 706 350 residential bed‐months, were aggregated by year, month, and RACF postcode. We calculated monthly incidence rates of hospital transfer and death with 95% confidence intervals (CIs), assuming 100% or 90% bed occupancy. We estimated the expected numbers of hospital transfers and deaths within one week of COVID‐19 vaccination, assuming no association with vaccination. Analyses were undertaken in Stata 16.0; the study was approved by the Human Research Ethics Committee of the Royal Children’s Hospital, Melbourne (37194A).
The estimated mean aggregated hospital transfer rate for RACF residents was 5.55 (95% CI, 5.48–5.59) per 100 bed‐months; the estimated mean aggregated death rate was 2.53 (95% CI, 2.49–2.57) per 100 bed‐months. Mean monthly rates of hospital transfer and death were higher in 2017, during which the influenza season in Australia was severe5 (Box 1). The incidence of both hospital transfer and death were higher during mid‐winter (July/August; Box 2).
On the basis of the data for 2015–2019, we estimate that 1.27 (95% CI, 1.10–1.51) hospital transfers per 100 vaccinated residents and 0.58 (95% CI, 0.44–0.75) deaths per 100 vaccinated residents would be expected. That is, for each 10 000 RACF residents who receive COVID‐19 vaccines, 127 hospital transfers and 58 deaths would be expected within one week of vaccination if the assumption of no association with vaccination is appropriate.
These estimated background rates can be used to help evaluate the safety of COVID‐19 vaccines administered to people in RACFs, providing information about the expected rates of health events and assisting detection of changes above these levels.
Box 1 – Numbers and mean monthly incidence rates of hospital transfer and death for residents of 101 Australian residential aged care facilities, 2015–2019, by year and assumed bed occupancy
|
|
|
Hospital transfers |
Deaths |
||||||||||||
|
|
|
|
Mean monthly rate, per 100 beds (95% CI) |
|
Mean monthly rate, per 100 beds (95% CI) |
||||||||||
|
Year |
Beds |
Number |
100% bed occupancy |
90% bed occupancy |
Number |
100% bed occupancy |
90% bed occupancy |
||||||||
|
|
|||||||||||||||
|
2015 |
90 083 |
4301 |
4.77 (4.63–4.92) |
5.30 (5.15–5.47) |
2348 |
2.61 (2.50–2.71) |
2.90 (2.78–3.02) |
||||||||
|
2016 |
119 421 |
6333 |
5.30 (5.17–5.44) |
5.89 (5.75–6.04) |
3001 |
2.51 (2.42–2.60) |
2.79 (2.69–2.89) |
||||||||
|
2017 |
144 045 |
8497 |
5.89 (5.77–6.03) |
6.55 (6.42–6.70) |
3973 |
2.76 (2.67–2.85) |
3.06 (2.97–3.16) |
||||||||
|
2018 |
165 354 |
9169 |
5.55 (5.43–5.66) |
6.16 (6.04–6.29) |
4084 |
2.47 (2.39–2.55) |
2.74 (2.66–2.83) |
||||||||
|
2019 |
187 447 |
10 768 |
5.74 (5.64–5.85) |
6.38 (6.26–6.50) |
4453 |
2.38 (2.31–2.45) |
2.64 (2.56–2.72) |
||||||||
|
2015–2019 |
706 350 |
39 068 |
5.55 (5.48–5.59) |
6.15 (6.08–6.21) |
17 859 |
2.53 (2.49–2.57) |
2.81 (2.77–2.85) |
||||||||
|
|
|||||||||||||||
|
CI = confidence interval. |
|||||||||||||||
Box 2 – Mean monthly rates of hospital transfer and death for residents of 101 Australian residential aged care facilities (assuming 100% bed occupancy), 2015–2019*
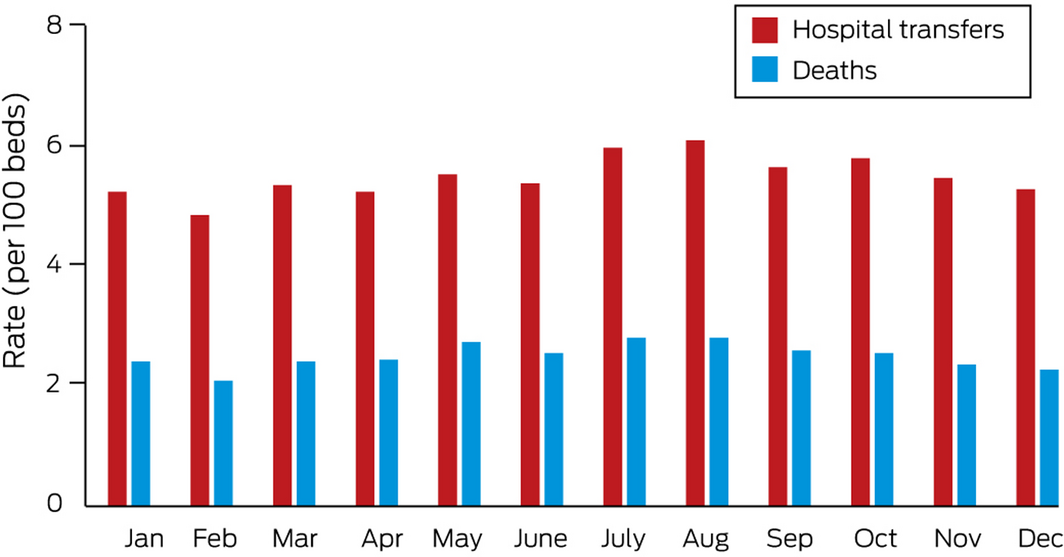
* The numbers of hospitals transfers and deaths are included in the online Supporting Information.
Received 16 March 2021, accepted 15 June 2021
- 1. Hashan MR, Smoll N, King C, et al. Epidemiology and clinical features of COVID‐19 outbreaks in aged care facilities: a systematic review and meta‐analysis. EClinicalMedicine 2021; 33: 100771.
- 2. Australian Department of Health. COVID‐19 outbreaks in Australian residential aged care facilities. National snapshot. 11 Sept 2020. https://www.health.gov.au/sites/default/files/documents/2020/09/covid-19-outbreaks-in-australian-residential-aged-care-facilities-11-september-2020.pdf (viewed Mar 2021).
- 3. Torjesen I. Covid‐19: doctors in Norway told to assess severely frail patients for vaccination. BMJ 2021; 372: n167.
- 4. Black S, Eskola J, Siegrist CA, et al. Importance of background rates of disease in assessment of vaccine safety during mass immunisation with pandemic H1N1 influenza vaccines. Lancet 2009; 374: 2115–2122.
- 5. Grant KA, Carville KS, Sullivan SG, et al. A severe 2017 influenza season dominated by influenza A(H3N2), Victoria, Australia. Western Pac Surveill Response J 2018; 9 (5 Suppl 1): 18–26.





Hazel Clothier is seconded to the Victorian Department of Health, who provide a salary for her services.