The known: Hypoglycaemia and hyperglycaemia in hospitalised patients is associated with increased morbidity, mortality and length of stay. It is not known how well diabetes is managed in hospitals in Queensland.
The new: Deficits in inpatient diabetes management include high rates of medication error, hospital‐acquired harm (hypoglycaemia, diabetic ketoacidosis), and suboptimal rates of appropriate glycaemic control, particularly in patients treated with insulin. Many patients did not see specialist diabetes team members despite meeting the criteria for doing so.
The implications: The identified deficits should be remedied, including by establishing specialist diabetes teams. Ongoing evaluation of outcomes is needed to monitor improvement in care.
It is estimated that about 1.2 million Australian adults (6% of the population) have diabetes.1 During 2016–17, more than 50 000 people were hospitalised with diabetes‐related complications, and diabetes was an associated diagnosis for 1.1 million admissions (10% of all hospitalisations).1 A total of $598 million was spent on hospital admissions directly related to diabetes during 2015–16.2
Observational studies of hospitalised patients have found that hyperglycaemia is associated with increased mortality and morbidity, and hypoglycaemia with increased mortality and hospital length of stay.3,4 Randomised trials have found that intensive glucose control in hospital and in outpatient care can also increase mortality, probably by increasing hypoglycaemia rates.5,6,7 Further, improved glycaemic control may be associated with fewer post‐operative complications.8
Improving inpatient diabetes management to avoid both hypoglycaemia and excessive hyperglycaemia is consequently an important therapeutic goal. Despite a uniform insulin management chart (electronic insulin prescribing) and statewide point‐of‐care decision support, inpatient diabetes care could be improved in Queensland. The American Diabetes Association (ADA) recommends appropriate quality assurance of inpatient diabetes care,9 but there has been no recent large scale audit of inpatient diabetes care in Australia. The National Inpatient Diabetes Audit (NaDIA) has been undertaken since 2010 in England, and in England and Wales since 2011,10 and it has been followed by substantial practice changes to optimise inpatient care of people with diabetes.11
We audited practice related to managing diabetes in hospitalised patients in Queensland to formally document current practice and to identify aspects of diabetes care that require improvement. Specifically, we aimed to assess the quality of diabetes care, including blood glucose control, rates of hospital‐acquired harm, the incidence of insulin prescription and management errors, and appropriate foot and peri‐operative care.
Methods
The audit was conducted on a single day in each participating public hospital during 18–29 March 2019. Most inpatient hospital care in Queensland is provided by government‐funded public hospitals in 17 hospital and health services. Hospitals range from quaternary teaching hospitals with about 1000 acute care beds to small rural hospitals with fewer than five inpatient beds; most acute care is provided in quaternary, tertiary, and secondary referral hospitals in metropolitan areas or in regional centres. Hospitals generally use paper‐based combined blood glucose and insulin prescription charts, but some use electronic systems for recording blood glucose measurements and insulin prescribing. Each system (paper‐based and electronic) includes associated decision support that assists with initiating insulin therapy, including evidence‐based advice about using basal‐bolus insulin rather than a sliding scale, and adjustment of doses for patients with hypoglycaemia.4,8,9,12
The Queensland Inpatient Diabetes Survey (QuIDS) 2019, adapted from the England–Wales NaDIA, included three components: an audit of hospital characteristics, a bedside audit, and a patient experience survey. In this article we report the outcomes of the bedside audit. All adult patients with diabetes mellitus (at presentation or diagnosed during admission) who were admitted to medical, surgical, mental health, high dependency, or intensive care wards were included; patients in paediatric, obstetric, day case, surgical short stay, or palliative care wards or emergency departments were excluded. The QuIDS Bedside Audit data collection tool, adapted from the NaDIA Bedside Audit data collection tool, included decision support and definitions of outcomes to ensure objective and reproducible data collection (online Supporting Information, part 1).
All members of the Queensland Statewide Diabetes Network — which includes about 300 clinicians in public hospitals, general practices, and private organisations — were invited to participate. Each hospital was required to undertake all data collection on a single day during the audit period. Most data collection was performed by clinicians involved in diabetes care.
Data obtained by review of patient medical records and, when necessary, of state pathology system data included basic demographic information, type of diabetes, complications, current diabetes treatments, and glycosylated haemoglobin (HbA1c) measurements during admission or within the preceding three months. We assessed the incidence of hospital‐acquired patient harm, including hypoglycaemia and the development of diabetic ketoacidosis or hyperosmolar hyperglycaemic state, as identified by the treating team during the admission (further details: Supporting Information, part 1).
Glycaemic control data were collected for the 24 hours to five days of care preceding the audit. “Good diabetes day” was defined as a day on which the patient had appropriate blood glucose monitoring, no hypoglycaemia, and no more than one blood glucose level measurement outside the Australian Diabetes Society target range of 5–10 mmol/L12 (further details: Supporting Information, part 1). Patients for whom symptomatic management was deemed more appropriate (eg, those in palliative care) were excluded from this analysis. Hypoglycaemia was defined as a blood glucose level below 4.0 mmol/L (moderate hypoglycaemia, 3.0–3.9 mmol/L; severe hypoglycaemia, < 3 mmol/L).
We calculated the proportion of patients who experienced one or more medication errors. Medication errors included prescription errors (any anti‐diabetic agent order that might lead to an incorrect dose being administered; eg, unclear name or dose) and management errors (failure to appropriately adjust therapy in response to hyper‐ or hypoglycaemia). Insulin errors were prescription or management errors related to insulin use (Supporting Information, part 2). We also assessed the management of insulin infusions, inpatient diabetic foot care and peri‐operative care planning, whether patient review by a specialist diabetes team (endocrinologist, diabetes educator, dietitian, podiatrist) was warranted and provided, and patient self‐management.
Statistical analysis
Data were collected in Survey Monkey, exported to Excel (Microsoft), and analysed in Stata 12.1. Descriptive statistics were generated: means with standard deviations (SDs) or medians with interquartile ranges (IQRs) as appropriate. Rates of good diabetes days and hypoglycaemia are presented as episodes per 100 patient‐days with 95% confidence intervals (CIs) calculated using Poisson confidence interval methods. The statistical significance of differences in proportions between groups was assessed in ?2 tests, and differences in rates for count variables by Poisson regression. We performed a subgroup analysis by diabetes mellitus type and treatment.
Ethics approval
As our study was considered an audit of practice, exemption from formal hospital human research ethics review was granted for all sites by the chair of the Royal Brisbane and Women’s Hospital Human Research Ethics Committee.
Results
Twenty‐seven of 115 hospitals that provide acute inpatient services supplied bedside audit data, including four of five tertiary/quaternary referral centres (equivalent to service capability framework level 6), four of seven large regional or outer metropolitan hospitals (service capability level 5), seven of 13 smaller outer metropolitan or small regional hospitals (service capability level 4), and 12 of 88 hospitals in rural or remote locations (service capability level 2 or 3) (Supporting Information, part 3). The median number of beds occupied in wards that met inclusion criteria on the day of audit, per hospital, was 122 (IQR, 10–230 beds; range, 4–667 beds). A total of 4265 occupied beds were eligible for inclusion (of 6652 across all Queensland hospitals), of which 4175 could be audited (98%); 1003 patients had diabetes (24%), for 850 of whom (85%) data were collected for our study. Blood glucose level monitoring charts were available for 800 patients, with median coverage of five days (IQR, 3–5 days). The mean age of the 850 patients was 65.9 years (SD, 15.1 years), 357 were women (42%), and their mean HbA1c level was 66 mmol/mol (SD, 26 mmol/mol) (Box 1).
Glycaemic control and medication errors
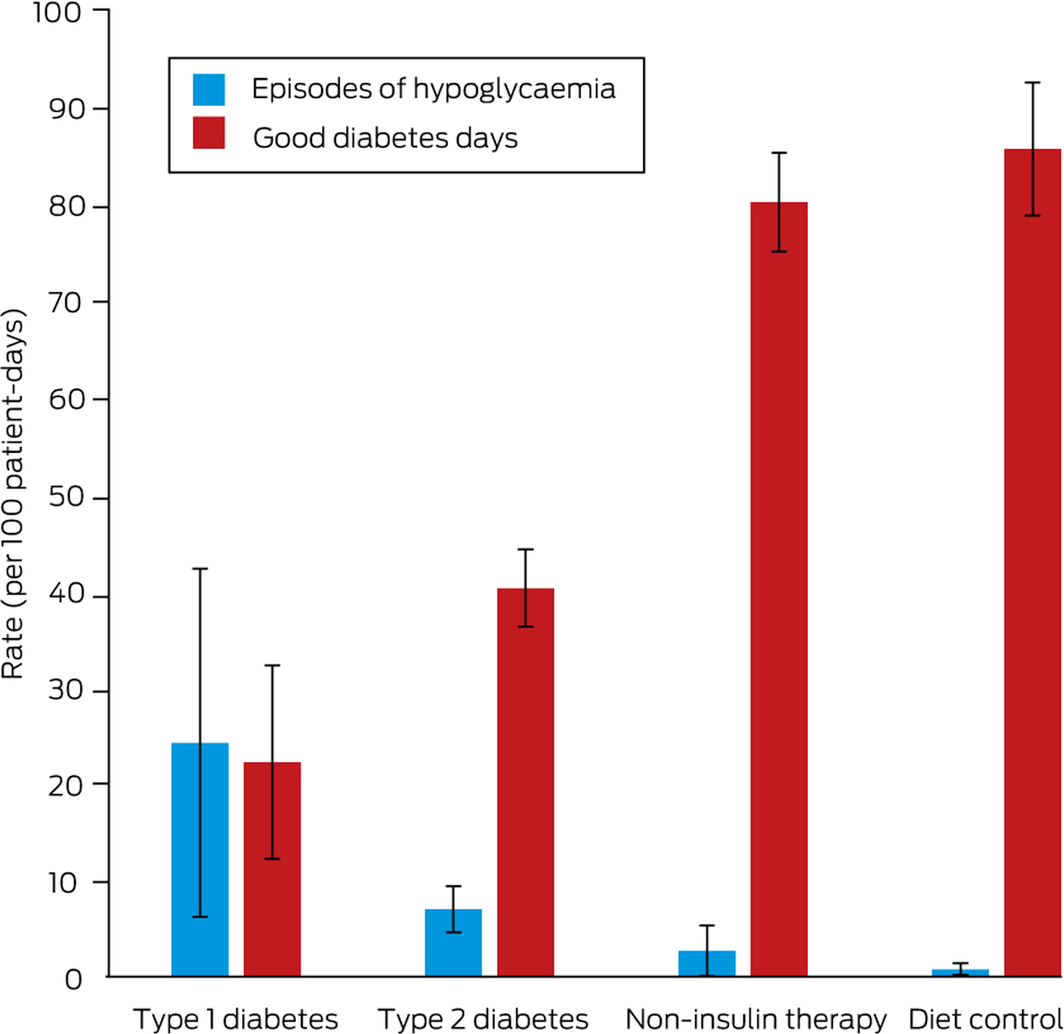
Appropriate blood glucose level monitoring was undertaken on 3005 of 3240 audited days (93%). The good diabetes day rate was 59.4 per 100 patient‐days (95% CI, 56.1–62.9 per 100 patient‐days); it was lower for patients with type 1 diabetes mellitus (22.1 per 100 patient‐days; 95% CI, 12.1–32.1 per 100 patient‐days) than for patients with type 2 diabetes (61.3 per 100 patient‐days; 95% CI, 57.9–64.8 per 100 patient‐days), among whom it was in turn lower for those treated with insulin (40.1 per 100 patient‐days; 95% CI, 36.1–45.2 per 100 patient‐days) than for those receiving non‐insulin or dietary treatments (81.3 per 100 patient‐days; 95% CI, 77.4–85.2 per 100 patient‐days) (Box 2).
HbA1c measurements during the admission or from the preceding three months were available for 333 participants (39%). Two hundred and twenty‐nine patients (27%) had been seen by a member of a diabetes team, and 121 (14%) met criteria for review by a diabetes team without this being undertaken.
We identified medication errors for 201 patients (32%), including 121 with prescription errors (19%) and 123 with management errors (19%) (Box 3). At least one prescription error was identified for 79 of 353 patients receiving insulin (22%) and 50 of 478 patients receiving oral hypoglycaemic agents (10%), and at least one management error for 91 patients receiving insulin (26%) and 52 patients receiving oral hypoglycaemic agents (11%).
Thirty‐four patients had received intravenous insulin infusions; for 32 it was deemed appropriate for the duration of use, but for six patients the transition to subcutaneous or oral diabetes therapy was not managed appropriately. A total of 291 blood glucose levels were recorded for patients who had received intravenous insulin during the preceding 24 hours; 130 values (45%) exceeded 10 mmol/L, and nine (3%) were below 4 mmol/L.
Hospital‐acquired harm
Seventy‐six patients (9.5%; 95% CI, 7.6–12%) experienced a total of 169 episodes of hypoglycaemia (6.0 episodes per 100 patient‐days; 95% CI, 3.4–6.6 episodes per 100 patient‐days), including 62 outside usual working hours of 93 episodes for which the time of episode was recorded (67%). Most hypoglycaemia episodes were moderate (125 episodes, 74%); 44 were severe (26%). Six patients (1%) required intravenous treatment for hypoglycaemia.
In patients with type 1 diabetes mellitus, the rate of hypoglycaemia (24.1 episodes per 100 patient‐days; 95% CI, 6.1–42 episodes per 100 patient‐days) was higher than for patients with type 2 diabetes mellitus receiving insulin (7.4 episodes per 100 patient‐day; 95% CI, 0–22 episodes per 100 patient‐day); each of these rates were higher than for patients not treated with insulin (Box 2). Four of 49 patients with type 1 diabetes mellitus (8%) developed diabetic ketoacidosis during their admission.
Foot disease management
Ninety‐six patients were admitted with active foot disease, 69 of whom had seen a member of the multidisciplinary foot team within 24 hours of admission. Of the 721 patients admitted without active foot disease, 47 (7%) had a documented foot examination. No patients developed a foot lesion during their admission.
Peri‐operative management
In total, 208 patients (24%) had at least one operation during their admission. The surgery was elective in 90 cases (43%) and urgent or emergency surgery in 117 (56%). Pre‐operative records were available for 135 patients (65%); diabetes was mentioned in 111 of these records (82%). Sixty patients who had surgery (29%) had clearly documented peri‐operative diabetes management plans.
Patient self‐management
Fifty‐three hospitalised patients with diabetes were monitoring their own blood glucose levels (6.2%), 72 self‐administering insulin (8.5%), and 23 adjusting their own insulin doses (2.7%).
Discussion
The Queensland Inpatient Diabetes Survey (QuIDS) 2019 is the largest, most comprehensive clinical audit of inpatient diabetes care that has been conducted in Australia. We found that 24% of hospitalised patients had diabetes, comparable with Australian data from 2014 (24.7%).13 Our bedside audit identified several deficits in inpatient diabetes management that require attention to avoid patient harm and improve care. Management deficits included high rates of hospital‐acquired diabetic ketoacidosis (8%), hypoglycaemia (9.5%; 6.0 episodes per 100 patient‐days), and diabetes medication errors (32%), and low rates of achieving glycaemic targets (59 good diabetes days per 100 patient‐days), particularly in patients treated with insulin. Fewer than one‐third of patients with diabetes had been seen by specialist diabetes practitioners, and HbA1c levels had been recently assessed in fewer than half the patients, despite respective grade C and B recommendations in the ADA Standards of Medical Care.9 Further, a documented peri‐operative diabetes management plan was available for fewer than one‐third of patients who underwent surgery.
The quality of inpatient diabetes management in Queensland appears to be similar to, if not poorer than recorded in England and Wales by the NaDIA. The good diabetes days rate (59%), which takes into account both hypo‐ and hyperglycaemia and the appropriateness of blood glucose level monitoring, was lower than found by NaDIA (65% in 2017).14 The proportions of patients subject to diabetes medication prescription and management errors were similar (NaDIA, 31%;14 QuIDS, 32%), with similar rates of prescription and glucose management errors. However, we identified a substantially higher proportion of patients with insulin errors (NaDIA, 18%;14 QuIDS, 137 patients, 39%). The proportion of patients with hypoglycaemia episodes was lower in our audit (NaDIA, 18%;14 QuIDS, 9.5%), but the rate of hospital‐acquired diabetic ketoacidosis was higher (NaDIA, 4.3%;14 QuIDS, 8%).
Methodological differences between NaDIA and QuIDS included the fact that we audited up to five preceding practice days (facilitated by combined blood glucose level/insulin charts), whereas NaDIA assesses the preceding seven days. We would therefore expect that numbers of some outcomes, including medication errors, would be lower in our study. Further, electronic blood glucose monitoring in hospital was less common than in NaDIA (12% v 61.6%11), which would make identification of hypoglycaemia more difficult. The rates of medication errors and hypoglycaemia we report may consequently be underestimates in comparison with data for England and Wales.
The deficiencies in practice we found exist despite a standard insulin prescription and blood glucose monitoring form and statewide digital prescribing and glucose monitoring; both systems are linked with point‐of‐care decision support that provides evidence‐based advice about safe prescribing of basal‐bolus insulin for hospitalised patients.4,8,9,12 Alternative approaches are needed to reduce patient harm associated with inpatient diabetes management. The first national inpatient audit of practice in England and Wales, undertaken in 2011, identified substantial deficiencies.10 Increased funding has since facilitated continuously increasing availability of specialist inpatient diabetes staff and more patients being seen by specialist diabetes teams, so that successive audits have documented improvements in practice, including reductions in medication errors and hospital‐acquired harm (eg, hypoglycaemia, need for intravenous rescue therapy for patients with hypoglycaemia, foot ulcers).14 Specialist diabetes teams improve glycaemic control and reduce hospital length of stay, rates of re‐admission, and hospital‐acquired harm,15,16,17,18,19 but are only infrequently available in Queensland hospitals; 14% of patients in our survey met criteria for specialist team care, but were not been seen by any diabetes specialists (medical, nursing or allied health). To improve inpatient diabetes care in Queensland, expanding the availability of specialist diabetes teams should be considered.
An increasing number of hospitals surveyed by NaDIA use electronic prescribing (34.6%) and remote blood glucose monitoring (61.6%),11 compared with 12% for each in Queensland. Virtual blood glucose monitoring is associated with better glycaemic control in hospitalised patients, although more evidence is required in this regard.20 Queensland is currently rolling out an electronic health record system21 that could enable electronic prescribing and remote blood glucose monitoring, and this could be an opportunity to improve inpatient diabetes care.
Limitations
Although our hospital sample included a broad representation of sizes and geographic locations, our findings may not reflect practice in hospitals throughout Queensland or the rest of Australia. A national survey, similar to the NaDIA in England and Wales, would provide better quality, representative data; in the absence of such a survey, we plan to repeat our audit of practice during 2021. Secondly, the number of patients included in our audit was small compared with NaDIA (more than 16 000 in 2017). Further, as we adapted the NaDIA questions to better reflect practice in Queensland, direct comparability of our data with those from England and Wales may not be possible. Finally, patients were identified as having diabetes, complications, treatments, and HbA1c measurements by reviewing their medical records, but these may not be complete or accurate, and independent adjudication of outcomes (such as diabetic ketoacidosis) was not undertaken. Finally, as blood glucose measurements were obtained from a combination of paper and computer‐based meters, errors in bedside recording of blood glucose measurements were possible.
Conclusion
The Queensland Inpatient Diabetes Survey 2019 identified several deficits in inpatient diabetes management, including high rates of medication error and hospital‐acquired harm, and low rates of peri‐operative diabetes management planning and appropriate glycaemic control, particularly for patients treated with insulin. These deficits require attention, and ongoing evaluation of outcomes is necessary.
Box 1 – Demographic characteristics, diabetes treatments, complications, and glycated haemoglobin (HbA1c) values for the 850 patients in the 2019 Queensland Inpatient Diabetes Survey
|
Characteristic |
Number |
||||||||||||||
|
|
|||||||||||||||
|
Number of patients |
850 |
||||||||||||||
|
Age (years), mean (SD) |
65.9 (15.1) |
||||||||||||||
|
Sex (women) |
357 (42%) |
||||||||||||||
|
Indigenous status |
|
||||||||||||||
|
Aboriginal |
61 (7%) |
||||||||||||||
|
Torres Strait Islander |
16 (2%) |
||||||||||||||
|
Aboriginal and Torres Strait Islander |
10 (1%) |
||||||||||||||
|
Smoking status |
|
||||||||||||||
|
Current |
108 (18%) |
||||||||||||||
|
Ex‐smoker |
227 (38%) |
||||||||||||||
|
Never smoked |
265 (44%) |
||||||||||||||
|
Nights in hospital, median (IQR) |
6 (3–18) |
||||||||||||||
|
Diabetes mellitus |
|
||||||||||||||
|
Type 1 |
49 (6%) |
||||||||||||||
|
Type 2 |
788 (93%) |
||||||||||||||
|
Other |
7 (1%) |
||||||||||||||
|
Duration of diabetes |
|
||||||||||||||
|
< 5 years |
96 (11%) |
||||||||||||||
|
5–9 years |
100 (12%) |
||||||||||||||
|
10–14 years |
102 (12%) |
||||||||||||||
|
15–29 years |
153 (19%) |
||||||||||||||
|
> 30 years |
48 (9%) |
||||||||||||||
|
Diagnosed during admission |
9 (2%) |
||||||||||||||
|
HbA1c level (mmol/mol), mean (SD) |
66 (26) |
||||||||||||||
|
Diabetes complications |
|
||||||||||||||
|
Foot disease |
137 (16%) |
||||||||||||||
|
Diabetic neuropathy |
161 (19%) |
||||||||||||||
|
Diabetic eye disease |
116 (14%) |
||||||||||||||
|
Peripheral vascular disease |
226 (27%) |
||||||||||||||
|
Ischaemic heart disease |
304 (36%) |
||||||||||||||
|
Previous stroke or transient ischaemic attack |
139 (16%) |
||||||||||||||
|
Chronic kidney disease |
341 (40%) |
||||||||||||||
|
Stage 1 or 2 |
99 (12%) |
||||||||||||||
|
Stage 3 |
143 (17%) |
||||||||||||||
|
Stage 4 |
50 (6%) |
||||||||||||||
|
Stage 5 |
18 (2%) |
||||||||||||||
|
Renal replacement therapy |
31 (4%) |
||||||||||||||
|
Diabetic therapies (on presentation) |
|
||||||||||||||
|
Insulin |
367 (43%) |
||||||||||||||
|
Oral diabetic agents |
546 (64%) |
||||||||||||||
|
Non‐insulin injectable medications |
13 (2%) |
||||||||||||||
|
Diet and lifestyle modification only |
187 (22%) |
||||||||||||||
|
Insulin regimens (on presentation) |
|
||||||||||||||
|
Basal |
264/367 (72%) |
||||||||||||||
|
Prandial |
213/367 (58%) |
||||||||||||||
|
Pre‐mixed |
79/367 (22%) |
||||||||||||||
|
Insulin pump |
0 |
||||||||||||||
|
Primary reason for admission |
|
||||||||||||||
|
Medical: not diabetes‐related |
544 (64%) |
||||||||||||||
|
Non‐medical (eg, surgery, orthopaedics, mental health) |
196 (23%) |
||||||||||||||
|
Active diabetic foot disease |
65 (8%) |
||||||||||||||
|
Hyperglycaemia with established diabetes |
18 (2%) |
||||||||||||||
|
Diabetic ketoacidosis |
13 (2%) |
||||||||||||||
|
Hypoglycaemia |
6 (1%) |
||||||||||||||
|
Hyperglycaemic hyperosmolar state |
1 (< 1%) |
||||||||||||||
|
Admission ward |
|
||||||||||||||
|
Diabetes or endocrinology |
18 (2%) |
||||||||||||||
|
Acute or general medicine |
231 (28%) |
||||||||||||||
|
Geriatrics or rehabilitation |
123 (15%) |
||||||||||||||
|
Other medical |
214 (26%) |
||||||||||||||
|
Surgical |
193 (23%) |
||||||||||||||
|
Intensive care or high dependency unit |
12 (1%) |
||||||||||||||
|
Mental health |
28 (3%) |
||||||||||||||
|
Gynaecology |
5 (1%) |
||||||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range; SD = standard deviation. |
|||||||||||||||
Received 13 August 2020, accepted 24 March 2021
- Peter Donovan1,2
- Jade Eccles-Smith1
- Nicola Hinton3
- Clare Cutmore1
- Kerry Porter4
- Jennifer Abel5
- Lee Allam4
- Alexis Dermedgoglou3
- Gaurav Puri3
- 1 Royal Brisbane and Women's Hospital, Brisbane, QLD
- 2 The University of Queensland, Brisbane, QLD
- 3 Cairns and Hinterland Hospital and Health Service, Cairns, QLD
- 4 Princess Alexandra Hospital, Brisbane, QLD
- 5 Logan Hospital, Logan, QLD
We acknowledge Jay Leckie, Heike Krausse, Hua Bing Yong, Roisine Warwick, and Kay Dean for their contributions to designing the survey, and the support of the Queensland Statewide Diabetes Network, Clinical Excellence Queensland, in conducting the survey.
No relevant disclosures.
- 1. Australian Institute of Health and Welfare. Diabetes (AIHW cat. no. CVD 82). Updated 24 June 2020. https://www.aihw.gov.au/reports-data/health-conditions-disability-deaths/diabetes/overview (viewed June 2020).
- 2. Australian Institute of Health and Welfare. Disease expenditure in Australia (AIHW cat. no. HWE 76). Updated 13 June 2019. https://www.aihw.gov.au/reports/health-welfare-expenditure/disease-expenditure-australia/data (viewed June 2020).
- 3. Turchin A, Matheny ME, Shubina M, et al. Hypoglycemia and clinical outcomes in patients with diabetes hospitalized in the general ward. Diabetes Care 2009; 32: 1153–1157.
- 4. Moghissi ES, Korytkowski MT, DiNardo M, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care 2009; 32: 1119–1131.
- 5. Action to Control Cardiovascular Risk in Diabetes Study Group; Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008; 358: 2545-2559.
- 6. ADVANCE Collaborative Group; Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008; 358: 2560-2572.
- 7. NICE-SUGAR Study Investigators; Finfer S, Chittock DR, Shuo SYS, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med 2009; 360: 1283-1297.
- 8. Umpierrez GE, Smiley D, Jacobs S, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care 2011; 34: 256–261.
- 9. American Diabetes Association. Diabetes care in the hospital: Standards of medical care in diabetes, 2020. Diabetes Care 2020; 43 (Suppl 1): S193–S202.
- 10. Health and Social Care Information Centre. National Diabetes Inpatient Audit (NaDIA), 2011. 17 May 2012. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-inpatient-audit/national-diabetes-inpatient-audit-nadia-2011 (viewed June 2020).
- 11. Health and Social Care Information Centre. National Diabetes Inpatient Audit (NaDIA), 2018. 9 May 2019. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-inpatient-audit/2018 (viewed June 2020).
- 12. Australian Diabetes Society. Guideline for routine glucose control in hospital. 2012. https://diabetessociety.com.au/documents/ADSGuidelinesforRoutineGlucoseControlinHospitalFinal2012.pdf (viewed June 2020).
- 13. Bach LA, Ekinci EI, Engler D, et al. The high burden of inpatient diabetes mellitus: the Melbourne Public Hospitals Diabetes Inpatient Audit. Med J Aust 2014; 201: 334–338. https://www.mja.com.au/journal/2014/201/6/high-burden-inpatient-diabetes-mellitus-melbourne-public-hospitals-diabetes
- 14. Health and Social Care Information Centre. National Diabetes Inpatient Audit (NaDIA), 2017. 14 Mar 2018. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-inpatient-audit/national-diabetes-inpatient-audit-nadia-2017 (viewed June 2020).
- 15. Wang YJ, Seggelke S, Hawkins RM, et al. Impact of glucose management team on outcomes of hospitalization in patients with type 2 diabetes admitted to the medical service. Endocr Pract 2016; 22: 1401–1405.
- 16. Garg R, Schuman B, Bader A, et al. Effect of preoperative diabetes management on glycemic control and clinical outcomes after elective surgery. Ann Surg 2018; 267: 858–862.
- 17. Bansal V, Mottalib A, Pawar TK, et al. Inpatient diabetes management by specialized diabetes team versus primary service team in non-critical care units: impact on 30-day readmission rate and hospital cost. BMJ Open Diabetes Res Care 2018; 6: e000460.
- 18. Ostling S, Wyckoff J, Ciarkowski SL, et al. The relationship between diabetes mellitus and 30-day readmission rates. Clin Diabetes Endocrinol 2017; 3: 3.
- 19. Kyi M, Colman PG, Wraight PR, et al. Early intervention for diabetes in medical and surgical inpatients decreases hyperglycemia and hospital-acquired infections: a cluster randomized trial. Diabetes Care 2019; 42: 832–840.
- 20. Rushakoff RJ, Sullivan MM, MacMaster HW, et al. Association between a virtual glucose management service and glycemic control in hospitalized adult patients: an observational study. Ann Intern Med 2017; 166: 621–627.
- 21. Queensland Health. Integrated electronic medical record (ieMR). Updated 9 Oct 2019. https://www.health.qld.gov.au/clinical-practice/innovation/digital-health-initiatives/queensland/integrated-electronic-medical-record-iemr (viewed April 2021).






Abstract
Objectives: To assess the quality of care for patients with diabetes in Queensland hospitals, including blood glucose control, rates of hospital‐acquired harm, the incidence of insulin prescription and management errors, and appropriate foot and peri‐operative care.
Design, setting: Cross‐sectional audit of 27 public hospitals in Queensland: four of five tertiary/quaternary referral centres, four of seven large regional or outer metropolitan hospitals, seven of 13 smaller outer metropolitan or small regional hospitals, and 12 of 88 hospitals in rural or remote locations.
Participants: 850 adult inpatients with diabetes mellitus in medical, surgical, mental health, high dependency, or intensive care wards.
Results: Twenty‐seven of 115 public hospitals that admit acute inpatients participated in the audit, including 4175 of 6652 eligible acute hospital beds in Queensland. A total of 1003 patients had diabetes (24%), and data were collected for 850 (85%). Their mean age was 65.9 years (SD, 15.1 years), 357 were women (42%), and their mean HbA1c level was 66 mmol/mol (SD, 26 mmol/mol). Rates of good diabetes days (appropriate monitoring, no more than one blood glucose measurement greater than 10 mmol/L, and none below 5 mmol/L) were low in patients with type 1 diabetes (22.1 per 100 patient‐days) or type 2 diabetes treated with insulin (40.1 per 100 patient‐days); hypoglycaemia rates were high for patients with type 1 diabetes mellitus (24.1 episodes per 100 patient‐days). One or more medication errors were identified for 201 patients (32%), including insulin prescribing errors for 127 patients (39%). Four patients with type 1 diabetes experienced diabetic ketoacidosis in hospital (8%); 121 patients (14%) met the criteria for review by a specialist diabetes team but were not reviewed by any diabetes specialist (medical, nursing, allied health).
Conclusions: We identified several deficits in inpatient diabetes management in Queensland, including high rates of medication error and hospital‐acquired harm and low rates of appropriate glycaemic control, particularly for patients treated with insulin. These deficits require attention, and ongoing evaluation of outcomes is necessary.