Complementary medicines are used by more than half the people in Australia, incurring out‐of‐pocket health expenses of about $5.2 billion in 2019.1 Information about their use by older adults in Australia is more than a decade old.2 Given subsequent demographic changes and doubling in sales of vitamins and supplements,1 we should update our knowledge in this area.
We analysed data from the ASPirin in Reducing Events in the Elderly (ASPREE) Longitudinal Study of Older Persons (ALSOP) to assess self‐reported use (every day, occasionally, never) of complementary medicines (fish oil, glucosamine, ginkgo, coenzyme Q10, calcium, zinc, vitamins B, C, D and E, multivitamins, Chinese or herbal) by healthy people over 70 years of age residing in metropolitan or regional Victoria, South Australia, Tasmania, the Australian Capital Territory or southern New South Wales, recruited through their usual general practitioners.3 We summarised data as descriptive statistics; we assessed differences between groups in χ2 tests (categorical variables). Analyses were conducted in SPSS Statistics 23 (IBM). ALSOP was approved by the Monash University Human Research Ethics Committee (reference, CF11/1100).
During January 2012 – July 2015, 14 757 of 16 703 ASPREE participants returned ALSOP Baseline Medical Questionnaires3 with at least partial responses to the questions on complementary medicines (response rate, 88%); their mean age was 75.2 years (standard deviation, 4.3 years), and 8068 (55%) were women). A total of 10 961 respondents (74.3%) reported using them either daily or occasionally; fish oil (6563 of 14 757 respondents, 44.5%), vitamin D (4995, 33.8%), glucosamine (3940, 26.7%), and calcium supplements (3652, 24.7%) were the most frequently reported items (Supporting Information, table 1).
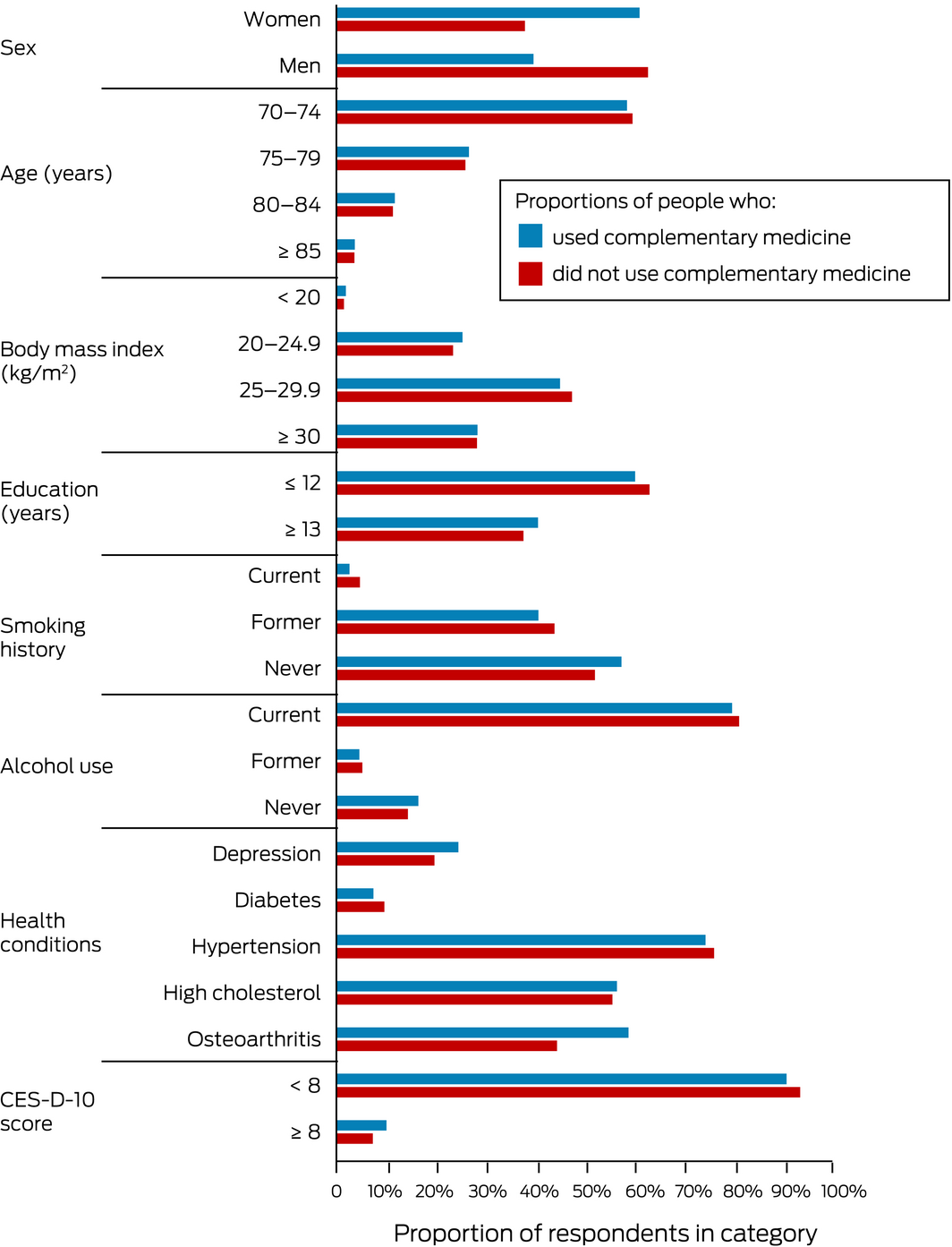
Complementary medicines were used by larger proportions of women (6637 of 8068, 82.3%) than of men (4324 of 6689, 64.6%; P < 0.001), and of people with more than 12 years of education (4418 of 5838, 75.7%) than of people with less education (6542 of 8918, 73.3%; P = 0.001). The proportions of complementary medicine users who reported a history of depression (987 of 4053, 24.4%) or osteoarthritis (3060 of 5240, 58.4%) were larger than for non‐users (depression, 264 of 1347, 19.6%; P = 0.002; osteoarthritis, 705 of 1598, 44.1%; P < 0.001); self‐reported diabetes was more common among non‐users (363 of 3790, 9.6%) than among complementary medicine users (815 of 10 944, 7.4%; P < 0.001) (Box; Supporting Information, tables 2 and 3).
Almost three‐quarters of people in our sample of community‐dwelling older adults in south‐eastern Australia used complementary medicines, with fish oil the most common product. While proprietary complementary medicines are generally regarded as safe, their widespread use by older people, who generally have a greater burden of disease, higher medical expenses, and low or fixed incomes, raises questions about their marketing and promotion.5
Our study population represents Australians over 70 who regularly visit general practitioners, and we included participants from geographically and socio‐economically diverse backgrounds.3 As we pre‐specified a limited number of products, our use estimates may be conservative. In our study, complementary medicine use was defined differently to some earlier studies; for example, the Australian Health Survey which asked about complementary medicine use in the previous 24‐hour period.6 This difference may account for our estimates being slightly higher. Our findings provide the most comprehensive information to date on complementary medicine use by Australians over 70 years of age.
Received 8 May 2020, accepted 17 August 2020
- 1. Complementary Medicines Australia. Australia’s complementary medicines industry audit 2019. http://www.cmaustralia.org.au/resources/CMA-INDUSTRY_AUDIT-V4.pdf (viewed July 2020).
- 2. Reid R, Steel A, Wardle J, et al. Complementary medicine use by the Australian population: a critical mixed studies systematic review of utilisation, perceptions and factors associated with use. BMC Complement Altern Med 2016; 16: 176.
- 3. McNeil JJ, Woods RL, Ward SA, et al. Cohort profile: the ASPREE Longitudinal Study of Older Persons (ALSOP). Int J Epidemiol 2019; 48: 1048–1049h.
- 4. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES‐D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med 1994; 10: 77–84.
- 5. Anlauf M, Hein L, Hense HW, et al. Complementary and alternative drug therapy versus science‐oriented medicine. Ger Med Sci 2015; 13: Doc05.
- 6. Australian Bureau of Statistics. Australian Health Survey: nutrition first results — foods and nutrients, 2011–12. May 2014. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/australian-health-survey-nutrition-first-results-foods-and-nutrients/latest-release (viewed July 2020).





* Robyn Woods, Michael Berk, Carlene Britt, Michael Ernst, Julia Gilmartin-Thomas, Jessica Lockery, Nigel Stocks.
The ASPREE study was funded by grants from the United States National Institute of Health, the National Health and Medical Research Council, Monash University, and the Victorian Cancer Agency. The ASPREE Longitudinal Study of Older Persons (ALSOP) was supported by a grant from the Wicking Trust.
No relevant disclosures.